Abstract
Dobbs v. Jackson Women’s Health Organization (Dobbs decision) has already had profound impact on reproductive health care in the United States. Some studies have reported increased incidence of vasectomy after the Dobbs decision. The Military Health System (MHS) provides a unique opportunity to evaluate this relationship in a universally insured, geographically representative population. We conducted a retrospective cross-sectional study of vasectomies among all male beneficiaries in the MHS, ages 18 to 64, from 2018 to 2022. Beneficiaries receiving a vasectomy were identified via billing data extraction from the MHS Data Repository (MDR). Descriptive statistics of demographic factors of all those receiving a vasectomy in the study period were evaluated. Crude and multivariate logistic regression models were used to evaluate for differences in demographic variables in those receiving a vasectomy pre-Dobb’s decision as compared to after the Dobb’s decision. The total number of men receiving a vasectomy each month over the study period was analyzed, as were the numbers in a state immediately implementing abortion access restrictions (Texas), and one without any restrictions on abortion access (Virginia). Our analysis found that men receiving a vasectomy post-Dobbs decision were more likely to be younger, unmarried, and of junior military rank than prior to the Dobbs decision. In the months following the Dobbs decision in 2022 (June-December), there was a 22.1% increase in vasectomy utilization as compared to the averages of those months in 2018–2021. Further, it was found that the relative increase in vasectomy after the Dobbs decision was greater in Texas (29.3%) compared to Virginia (10.6%). Our findings highlight the impact of the Dobbs decision on reproductive health care utilization outside of abortion.
Similar content being viewed by others
Introduction
The Supreme Court ruling in the Dobbs decision delivered on June 24, 2022, has already had a profound impact on the delivery of reproductive health care in the United States [1]. The most visible of these has been the restriction on access to abortion and other reproductive health care services implemented by several states with the overturning of Roe v. Wade [2]. There have also been several important downstream effects from this decision on health systems and the delivery of contraceptive services including the utilization of vasectomy procedures throughout the United States [3].
Vasectomy is a safe, effective, reversible, relatively inexpensive contraceptive service that can be performed in an outpatient setting and requires minimal recovery time [4, 5]. It is associated with significantly fewer complications and shorter recovery times than female tubal ligation [6]. However, the prevalence of vasectomy has traditionally lagged that of tubal ligation [7]. Historically, motivations for men to request vasectomy have included previous unwanted pregnancy, completed family size, or dislike of other contraceptive options [8]. Other studies have shown vasectomy rates to be associated with multiple individual factors including knowledge of procedure, cultural and religious norms, insurance coverage status, and other socioeconomic indicators [9, 10]. In 2009, the reported prevalence of vasectomy in men aged 30–45 years was 11.4% [10]. In 2002, the reported incidence of vasectomy in the United States was 10.2 per 1 000 men aged 25–49 [11]. During the early 21st century, studies found a decline in the rates of vasectomy in the United States [12, 13]. However, more recently vasectomy rates increased in the United States in data from 2014 to 2021 [14].
In the wake of the Dobbs decision, however, studies have shown up to a 29% increase in vasectomy rates throughout the United States [15,16,17]. Larger increases have been seen in states with ‘trigger bans’ on abortion access as compared to those that did not immediately implement access restrictions to abortion services [15]. These more recent studies have also shown shifts in the demographics of men receiving vasectomies in the United States, with shifts towards younger and unmarried men increasingly utilizing this method of contraception [14, 16, 17]. The factors and motivations for these shifts in vasectomy demographics have not been rigorously studied, however stated reasons for seeking vasectomy amongst individuals motivated by the Dobbs decision included the high success rate of the procedure, concern that vasectomy may be outlawed next, or as an act of solidarity with women [15].
The Military Health System (MHS) provides health care to approximately 9.6 million beneficiaries comprising service members, retirees, and their families. The system is composed of 49 inpatient hospitals and medical centers and 465 ambulatory care clinics throughout the United States and internationally as well as over 500 000 network providers. Analysis of the MHS allows for a unique opportunity to examine the effects of health policies in a universally insured, geographically representative population [18]. Given the age and gender distribution in the military, the population provides a diverse sample of individuals of male reproductive capacity in which to study utilization of vasectomy services. Historically, the military has lagged the general population in vasectomy utilization, with an estimated incidence of 7.1 vasectomies per 1 000 male service members per year from 2000 to 2009 and 8.6 vasectomies per 1 000 male service members per year from 2000 to 2017 [13, 19]. Additionally, with the dispersion of the MHS throughout the United States, the system provides additional opportunity to study vasectomy rates between states implementing more onerous restrictions on abortion access post Dobbs decision (Texas) as compared to those not implementing restrictions on abortion access (Virginia). Aside from the differences in abortion policies between the two states, these states were chosen for further analysis due to having the second and third highest number of stationed active duty military servicemembers, and having sizable, representative populations from all military services present. The objective of this study was to retrospectively assess the utilization of vasectomy within the MHS with evaluation of the impact of the Dobbs decision, and differences amongst states with differing levels of restriction on abortion access.
Materials/subjects and methods
Data source and study population
We retrospectively evaluated administrative health care claims data extracted from the MHS Data Repository (MDR). The MDR holds administrative and healthcare claims for all service members and retirees of the United States Army, Air Force, Navy, Marine Corps and Coast Guard and their dependents. It includes data on care provided directly through Military Treatment Facilities (MTFs) as well as private sector care through the Department of Defense’s TRICARE benefit. It does not include care delivered in a deployed setting, or through the Veterans Health Administration.
Study population
Our study population included all male beneficiaries, ages 18 to 64, of the MHS during the time period of 2018 through 2022. Through query of the MDR we are able to achieve complete ascertainment of vasectomies covered by the MHS. We excluded service members (and their dependents) who were members of the National Guard or Military Reserves due to their inconsistent access to the MHS which may have resulted in bias of mis ascertainment of the outcome of interest by not fully capturing men receiving a vasectomy. There was minimal (< 2%) variation in total number of Active Duty men in the study population year to year, with a low of 1 261 768 in 2022 and a high of 1 285 952 in 2019. The consistency of the denominator indicates that the count of men receiving a vasectomy each year will provide an appropriate approximation of the vasectomy rate year over year.
Data extraction
We queried all encounter data for International Classification of Diseases 10 (ICD-10) codes Z30.2 and Z98.52 and Current Procedural Terminology (CPT) codes 55450 and 55250 to identify vasectomies performed within the MHS. For each unique individual identified, their first visit with one of these codes was counted as a vasectomy. Each unique individual could only be counted for one vasectomy during the study period.
Data analysis
We conducted a descriptive analysis on patient demographics and time period for individuals receiving a vasectomy. Descriptive analysis included patient demographics (age, race/ethnicity, military service branch, and rank), the month and year of their first vasectomy visit, and the state in which the visit occurred. Age was evaluated as a categorical variable by decade (ages 18 and 19 combined with 20 s, all over 60 combined). Rank has been utilized in a variety of military studies both as an indicator of socioeconomic status as well as educational attainment. We performed logistic regression analysis on the effect of these demographic covariates to determine if certain groups were more likely to receive a vasectomy after the Dobbs decision as compared to before the decision. We examined crude logistic regression models on each covariate, as well as a full logistic regression model adjusting for all covariates. We further evaluated numbers of individuals receiving a vasectomy in each month of each year under study to evaluate for general trends, and any potential deviation from these trends in 2022 following the release of the Dobbs decision in June of 2022. Additionally, we assessed the relative change in numbers of vasectomies in the months following the release of the Dobbs decision in 2022 as compared to those month’s average from 2018 through 2021 between a state immediately imposing restrictions on abortion access (Texas) and one that had no such immediate increase in abortion access restrictions (Virginia). All analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC). This study was considered exempt by the Institutional Review Board of the Uniformed Services University of the Health Sciences. This manuscript adheres to the STROBE reporting guidelines.
Results
A total of 96 617 men aged 18–64 received a vasectomy covered by the MHS from January 2018 to December 2022. The demographic breakdown of these men is presented in Table 1. The groups in which the largest number of vasectomies were performed was in those aged 30–39 (53.97%), White (73.82%), active duty service members (78.24%), in the Army (36.58%), of senior enlisted rank (64.11%), and married (85.37%). We evaluated these demographics in a logistic regression model to determine factors associated with higher odds of receiving a vasectomy after the Dobbs decision (Table 2). The results of our adjusted logistic regression model show that the odds of receiving a vasectomy post-Dobbs decision as compared to pre-Dobbs decision were the highest in MHS beneficiaries in ages 18–29 (aOR 1.11, 95% CI 1.07–1.15) as compared to the reference group of those aged 30–39, and in unmarried beneficiaries (aOR 1.06, 95% CI: 1.02–1.10). Dependent beneficiaries were more likely to receive a vasectomy (aOR 1.42, 95% CI: 1.27–1.58) as compared to active duty service members. Senior officers were the least likely of the formal military ranks to receive a vasectomy. No significant differences in odds of vasectomy by race were noted.
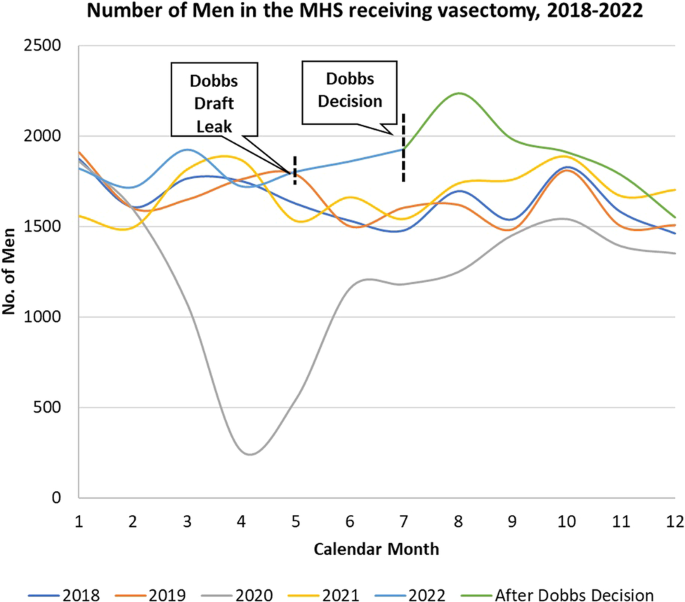
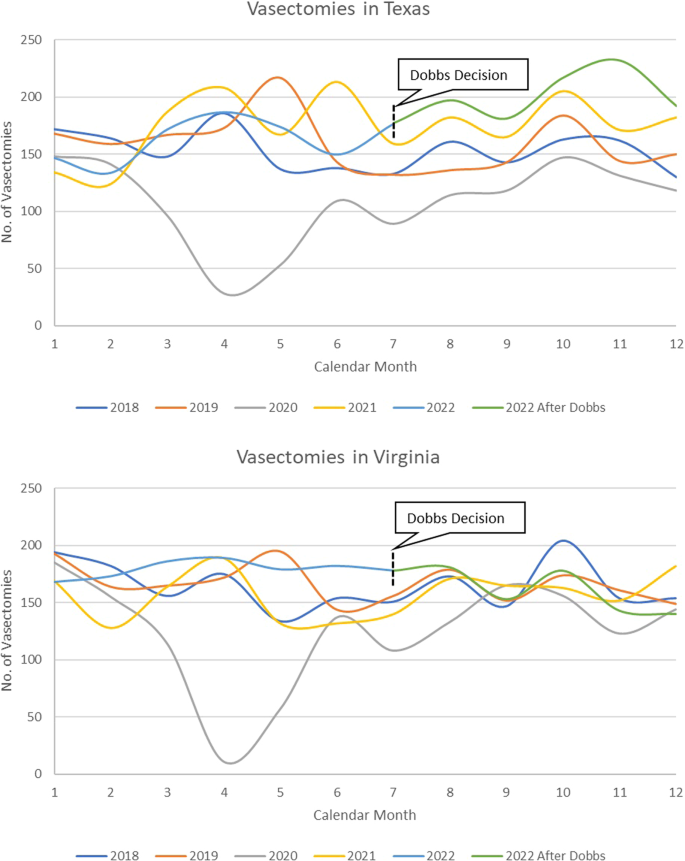
In the evaluation of the month during which men received vasectomies from January 2018 through December 2022 (Fig. 1) we observed fairly consistent levels between 1 500 and 2000 vasectomies per month during our study, with notable exceptions of large decreases seen during 2020, and a short increase seen immediately following the Dobbs decision in 2022. Overall, the year 2022 had the highest cumulative number of vasectomies performed among all calendar years (22 248) representing a 19.7% increase as compared to the average of 2018–2021. There was also a significant decrease in vasectomies performed in 2020, with only 14,642 men receiving a vasectomy. When discounting this significant decrease in 2020, we still observed an 11.8% increase in vasectomies in 2022 as compared to the average of 2018, 2019, and 2021. In the months following the Dobbs decision release, we observed a noticeable uptick in numbers of vasectomies performed, with a peak of 2236 in August 2022. In analysis of the average of the months June to December in each year, vasectomy incidence increased substantially after the release of the Dobbs decision in June of 2022, with a relative increase from June through December 2022 of 22.1% as compared to the average of the same months from 2018 to 2021. Analysis by state (Fig. 2) showed that the relative increase in vasectomy after the Dobbs decision from June through December 2022 as compared to the average of the same period in 2018–2021 was greater in a state immediately implementing a restriction on abortion access (Texas, 29.3%) as compared to a state with no such restriction (Virginia, 10.6%).
Discussion
Our findings demonstrate the striking changes in the incidence of vasectomy following the Dobbs decision in the MHS. Not only did 2022 have the highest number of men receiving a vasectomy, but monthly analysis showed a significant increase in vasectomy incidence in the months following the Dobbs decision release in 2022. Additionally, there was a notable difference in vasectomy incidence in Texas, which implemented a trigger restriction on abortion access after the reversal of Roe v. Wade, compared to Virginia, which had no such immediate restriction on abortion access. Texas had a substantially larger increase in vasectomy incidence from June to December 2022 as compared to expected rates from previous years. Further, our study provided interesting insight into the demographics of men receiving a vasectomy within the MHS, with unmarried and younger men having higher odds of receiving a vasectomy. Our analysis also indicated that there was a precipitous decrease in vasectomy incidence in 2020, during the height of the COVID-19 pandemic.
Increased incidence of vasectomy in the wake of the Dobbs decision has been noted in several other studies evaluating vasectomy incidence regional health centers and by insurance claims data [15, 16]. Our study shows that similar increases in vasectomy utilization were seen after the release of the Dobbs decision within the MHS as compared to the populations included in previous studies. However, in analysis of the monthly utilization of vasectomy within the MHS, there was a noticeable surge in vasectomies immediately following the Dobb’s decision with incidence largely returning to normal levels several months after the decision. This suggests that it may be possible that the release of the Dobbs decision acted as a ‘call to action’ in the short-term leading those already considering a vasectomy to receive one, but that the effect may be short lived, leading to vasectomy incidence returning to normal levels over time. Further study of the rate of incidence of vasectomy over the next several years could help to determine if this trend persists and vasectomy becomes a more mainstream and utilized form of contraceptive care.
Our findings highlight the potential importance of state-by-state level abortion access restrictions on the utilization of vasectomy, which has notable implications for the MHS. The legalities around providing access to abortion care within the MHS are muddied due to the Hyde Amendment of 1976, which restricts the use of federal funds to be used for abortion care. Typically, for MHS beneficiaries, these services were utilized as needed on an out-of-pocket basis. In some circumstances, beneficiaries were eligible for reimbursement for travel for the procedures due to the care not being available in network [20,21,22]. Our findings show that in our two comparator states (Texas and Virginia), the immediate implementation of abortion access restrictions was associated with higher rates of vasectomy utilization post Dobbs decision. This finding has been replicated in at least one other study; however no direct analysis on the effect of restrictions by differing gestational age, or other factors on the rate of vasectomy post Dobbs has been published to date [15]. Further research into the persistence of these effects, as well as analysis including differing levels of abortion access restrictions to better understand the effects these State level policies have on driving vasectomy utilization is important to better understand the issue and in the allocation of assets and resources for reproductive health care services.
Our demographic analysis indicated that younger (<30) and unmarried men had increased odds of utilizing vasectomy services post Dobbs decision as compared to pre-Dobbs. These findings suggest a significant shift in the demographics of vasectomy utilization, with previous studies typically showing older men at time of family completion were the most likely to utilize the service [10]. Other more recent studies have demonstrated these trends towards increased utilization of vasectomy services by younger men after the Dobbs decision, with Bole and colleagues showing a significant decline in median age of vasectomy utilization, and larger proportions of unmarried and childless men receiving vasectomy post Dobbs [16]. These findings suggest a shift in the landscape of perceptions and beliefs regarding vasectomy in younger generations, and further qualitative study of younger men receiving vasectomy to better characterize their attitudes regarding reproductive care could help provide greater insight into this trend. Additionally, longitudinal follow up of these younger and unmarried men receiving vasectomies may be indicated to assess if they are more likely to utilize procedures to reverse their vasectomy in the future. Substantially increased utilization of the more complex reversal procedures could drive significant requirements for resources and training for reproductive urologists and may further highlight the importance of evidence-based pre-vasectomy counseling [23, 24].
The impact of the COVID-19 pandemic on vasectomy utilization was an additional significant finding, with 2020 having the lowest number of vasectomies in our study. This finding continues to highlight the myriad impacts that the pandemic had on health care access and utilization, which may drive untold further healthcare needs in the future. Multiple studies have shown varying degrees of decreases in medical care access and utilization from cancer screenings to routine immunizations, and other reproductive services were all significantly impacted by the pandemic [25,26,27]. Further work on the downstream effects of these impacts could help to develop campaigns to ‘catch up’ on the immense amount of delayed care.
Our study had several key limitations. First, we were only able to capture vasectomies paid for (directly or indirectly) by the MHS, therefore any beneficiary receiving this service outside of the MHS would not be included. Additionally, we only utilized data back to 2018, which was primarily done to present data comparable to other studies that have been published on this issue [15, 16]. Further, as we only allowed for each individual to be counted for one vasectomy, it is possible that individuals received a vasectomy, had it reversed, and then received another vasectomy, in which case their second vasectomy would not be counted; however, we believe this to be rare, with only approximately 5% of men seeking an initial vasectomy reversal, and an even smaller proportion seeking re-vasectomy after a reversal [28].
Our analysis supports the hypothesis that the Dobbs decision had an immediate effect on vasectomy utilization within the MHS. We assess that the reversal of Roe v. Wade was a significant driver of a sizable increase in vasectomy incidence within the MHS, specifically amongst younger and unmarried men. Additionally, state level restrictions on abortion access may have mediated this effect; with more stringent restrictions resulting in higher rates of vasectomy utilization. These findings demonstrate the robustness of changes in the landscape of vasectomy utilization in a universally insured, geographically representative population. The MHS must be cognizant of the profound effect that the Dobbs decision has had on the state of reproductive health care access in America. It must be agile in appropriately allocating reproductive care assets and resources to those areas greatest effected by the reversal of Roe v. Wade to best support the needs of service members and their families.
Disclaimer
The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, assertions, opinions or policies of the Uniformed Services University of the Health Sciences (USUHS), the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. (HJF), the Department of Defense (DoD), or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the United States Government.
Data availability
The data that support the findings of this study are available from the United States Defense Health Agency. Restrictions apply to the availability of these data, which were used under federal Data User Agreements for the current study, and so are not publicly available.
References
Stein TB, Vasan A. Public health’s role in a Post-Dobbs World - The New York City abortion access hub. N Engl J Med. 2023;388:1926–9.
Kulczycki A. Dobbs: navigating the new quagmire and its impacts on abortion and reproductive health care. Health Educ Behav Off Publ Soc Public Health Educ. 2022;49:924–8.
Paltrow LM, Harris LH, Marshall MF. Beyond abortion: the consequences of overturning roe. Am J Bioeth AJOB. 2022;22:3–15.
Jamieson DJ, Costello C, Trussell J, Hillis SD, Marchbanks PA, Peterson HB, et al. The risk of pregnancy after vasectomy. Obstet Gynecol. 2004;103:848–50.
Schwingl PJ, Guess HA. Safety and effectiveness of vasectomy. Fertil Steril. 2000;73:923–36.
Bartz D, Greenberg JA. Sterilization in the United States. Rev Obstet Gynecol. 2008;1:23–32.
Mosher WD, Martinez GM, Chandra A, Abma JC, Willson SJ. Use of contraception and use of family planning services in the United States: 1982–2002. Adv Data. 2004:1–36.
Howard G. Motivation for vasectomy. Lancet Lond Engl. 1978;1:546–8.
Dejene Wolde Y, Ali M, Gebremeskel F, Ukke GG, Gebreselassie R, Demelash M, et al. Knowledge, attitude and associated factors towards vasectomy among married men in Arba Minch Town, Southern Ethiopia, 2021; A Cross-Sectional Study. Open Access J Contracept. 2023;14:1–13.
Eisenberg ML, Henderson JT, Amory JK, Smith JF, Walsh TJ. Racial differences in vasectomy utilization in the United States: data from the national survey of family growth. Urology. 2009;74:1020–4.
Barone MA, Hutchinson PL, Johnson CH, Hsia J, Wheeler J. Vasectomy in the United States, 2002. J Urol. 2006;176:232–6.
Punjani N, Goldstein M. Vasectomy: is the apparent decline real or not? Nat Rev Urol. 2022;19:69–70.
Zhang X, Eisenberg ML. Vasectomy utilization in men aged 18–45 declined between 2002 and 2017: Results from the United States National Survey for Family Growth data. Andrology. 2022;10:137–42.
Huang Z, Hyman MJ, Raheem OA. Trends in the vasectomy rate among privately insured men aged 18-64 in the United States Between 2014 and 2021. Urology. 2023;179:80–6.
Vasectomies rose by 29% in the three months after the end of Roe. Econ Lond. 2023.
Bole R, Lundy SD, Pei E, Bajic P, Parekh N, Vij SC. Rising vasectomy volume following reversal of federal protections for abortion rights in the United States. Int J Impot Res. [Internet]. 2023. Available from: https://doi.org/10.1038/s41443-023-00672-x
Zhang TR, Able C, Ramasamy R, Kohn TP. United States vasectomy incidence rises after the reversal of Roe v. Wade in a national clinical and claims database. Fertil Steril. 2023;120:196–7.
Tanielian T, Farmer C. The US military health system: promoting readiness and providing health care. Health Aff Proj Hope. 2019;38:1259–67.
Santomauro M, Masterson J, Marguet C, Crain D. Demographics of Men Receiving Vasectomies in the US Military 2000-2009. Curr Urol. 2012;6:15–20.
Rosoff JI. The Hyde Amendment and the future. Fam Plann Perspect. 1980;12:172.
Fix L, Seymour JW, Grossman D, Johnson DM, Aiken ARA, Gomperts R, et al. Abortion Need among U.S. Servicewomen: Evidence from an Internet Service. Womens Health Issues Off Publ Jacobs Inst Womens Health. 2020;30:161–6.
Grindlay K, Seymour JW, Fix L, Reiger S, Keefe-Oates B, Grossman D. Abortion knowledge and experiences among U.S. Servicewomen: a qualitative study. Perspect Sex Reprod Health. 2017;49:245–52.
Fantus RJ, Halpern JA. Vasovasostomy and vasoepididymostomy: indications, operative technique, and outcomes. Fertil Steril. 2021;115:1384–92.
Hyman MJ, Huang Z, Raheem OA The percentage of men counseled by urologists who received a vasectomy mildly increased after the publication of the AUA vasectomy guideline. Int J Impot Res. 2024. https://doi.org/10.1038/s41443-024-00829-2.
Becker NV, Moniz MH, Tipirneni R, Dalton VK, Ayanian JZ. Utilization of women’s preventive health services during the COVID-19 pandemic. JAMA Health Forum. 2021;2:e211408.
Mafi JN, Craff M, Vangala S, Pu T, Skinner D, Tabatabai-Yazdi C, et al. Trends in US ambulatory care patterns during the COVID-19 pandemic, 2019–2021. JAMA. 2022;327:237–47.
Steenland MW, Geiger CK, Chen L, Rokicki S, Gourevitch RA, Sinaiko AD, et al. Declines in contraceptive visits in the United States during the COVID-19 pandemic. Contraception. 2021;104:593–9.
Ramasamy R, Schlegel PN. Vasectomy and vasectomy reversal: an update. Indian J Urol IJU J Urol Soc India. 2011;27:92–7.
Acknowledgements
We acknowledge critical advice from the Center for Health Services Research and faculty of the Uniformed Services University Department of Preventive Medicine and Biostatistics. This study was funded by the Department of Defense, Defense Health Agency: Grant #HU0001–20–20035.
Author information
Authors and Affiliations
Contributions
Pierson – Conceived and designed work that led to submission, drafted and revised manuscript, approved final version of manuscript and is accountable for all aspects of the work. Banaag – Designed analysis plan, acquired and interpreted data, revised manuscript, approved final version and is accountable for all aspects of the work. Janvrin – Played an important role in interpreting results, revised manuscript, approved final version and is accountable for all aspects of the work. Koehlmoos – Conceived and designed work that lead to submission, revised manuscript, approved final version of manuscript and is accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Due to the secondary analysis of existing, de-identified data, this study was deemed exempt from human subjects review by the Institutional Review Board of the Uniformed Services University of the Health Sciences. Permission and conditions for use of these data were granted by the United States Defense Health Agency.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pierson, B.C., Banaag, A., Janvrin, M.L. et al. Vasectomy incidence in the military health system after the reversal of Roe v. Wade. Int J Impot Res (2024). https://doi.org/10.1038/s41443-024-00905-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-024-00905-7