Key Points
-
Highlights the differences between the NICE guideline for antibiotic prophylaxis against infective endocarditis and guidelines from other parts of the world.
-
Defines and describes the high risk cardiac patient group.
-
Highlights the legal implications applicable to the NICE guideline.
Abstract
Objective The National Institute for Health and Clinical Excellence (NICE) introduced the antibiotic prophylaxis guideline in 2008 for cardiac patients in the UK, which has led to a decrease in national prescription levels for antibiotic prophylaxis. Despite the introduction of the guideline there is still a discrepancy in levels of compliance among the dental community. The aims of this study were to determine the understanding of the NICE clinical guideline on antimicrobial prophylaxis against infective endocarditis (IE) and the difference in antibiotic prescription for high risk cardiac patients (HRCP) between dental trainers and trainees.
Methods A proforma was designed and distributed among dental trainers and trainees attending a conference at the London deanery. The trainers were GDPs responsible for training dental trainees allocated to them over a 12 month period based in a general dental practice. Dental trainees were recent graduates about to commence their vocational dental training. Eighty-five vocational dental trainees and 70 trainers completed the proforma on a voluntary basis.
Results The results of the study confirm that most trainers (95.7%) and trainees (94.1%) are aware of this guideline but only 62% of trainers and 69.7% of trainees have read the guideline. Compliancy with the guideline was low among trainers (55.7%) and trainees (77.6%). Compliance was high among those who had read the guideline. Trainers were more likely to prescribe prophylaxis antibiotics for HRCP. The majority (74-76%) would prescribe antibiotics on a specialist's request. Some trainers (54.9%) and trainees (48.2%) would want antibiotics themselves if they were HRCP.
Conclusion This study concludes that much needs to be done to improve the understanding and practice of NICE guideline among the dental trainers and trainees.
Similar content being viewed by others
Introduction
The National Institute for Health and Clinical Excellence (NICE) is an independent organisation providing guidance on the promotion of good health and prevention/treatment of ill health, in the United Kingdom. In March 2008, it produced guideline 64, stating that antibiotic prophylaxis against infective endocarditis (IE) is not recommended for people undergoing dental procedures.1 Antibiotic prophylaxis is an area of contention between regulatory bodies. It is universally accepted that there is no definitive proof that antibiotics are effective, merely evidence.2 Even among dental practitioners there is confusion as to what should be standard practice in relation to antibiotics and cardiac patients. After the initial implementation of the guideline there was a 78.6% reduction in the prescription of antibiotic prophylaxis with no notable effect on the identified cases of IE in England. However, there is still a baseline of 20% whom regularly prescribe prophylaxis.3
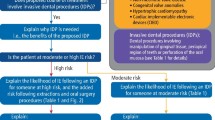
NICE stands at odds with other regulatory bodies such as the American Heart Association (AHA), European Society of Cardiology (ESC), and the Australian guidelines. It is agreed that the benefit of prophylaxis for dental treatment is unproven; NICE recommends no cover while the others state cover only for those deemed to be at high risk of developing IE.4 The Australian guidelines differ from the US and UK guidelines as antibiotic prophylaxis is recommended for indigenous Australians with rheumatic heart disease and shortlist patients considered to be high risk cardiac patients (HRCP). Furthermore, the Australian guideline has identified dental procedures that always require antibiotic prophylaxis for HRCP.5
This category of high risk cardiac patients (HRCP) is a source of contention between these organisations. They have been identified as patients with cardiac ailments who have the highest predisposition to IE. NICE have identified the following group of cardiac patients as HRCP. They include patients who have acquired valvular heart disease with stenosis or regurgitation, had valve replacement, structural congenital heart disease, previous IE and hypertrophic cardiomyopathy.1
Before the NICE guidelines, general dental practitioners (GDP) accounted for 91.9% of antibiotic prophylaxis prescriptions.3 The compliance and understanding of this change among dental practitioners has not been fully analysed previously, specifically in regards to the established GDPs who are trainers and vocational dental trainees.
In the UK, NICE is regarded as the major source of guidance for the medical/dental community for patient management. Hence it would be safe to assume that all dental practitioners would have read and implemented the guidelines for antibiotic prophylaxis for IE. This study's purpose was to determine the understanding of the NICE clinical guideline on antimicrobial prophylaxis against IE and the difference in antibiotic prescription for high risk cardiac patients (HRCP) between dental trainers and trainees.
Methods
A proforma was designed and distributed among dental trainers and trainees in the London deanery who were attending a conference. The trainers were GDPs who were responsible for the training of the dental trainee or trainees allocated to them over a 12 month period, based in a general dental practice. Dental trainees in this study had recently graduated from dental school and were about to commence their vocational dental training. Eighty-five vocational dental trainees and 70 trainers completed the proforma on a voluntary basis.
Results
Trainers
The average age of the trainers was 44 (29-62) years, with a male to female ratio of 4:1 noted. The majority (95.7%) had a postgraduate qualification and on average had been working for 19 (5-38) years. Most (97.1%) had heard of NICE guidelines but only 62% had read the guidelines. Only 55.7% trainers complied with the NICE guidelines by not prescribing antibiotic prophylaxis for HRCP. Of the group that had read the guidelines, 61.4% complied with the guidelines and for those that had not read the guidelines the compliance was lower at 48.1%. Most (90%) had prescribed antibiotics to cardiac patients in the past and amoxicillin 3 mg was the popular choice. Patients with a previous history of IE were more likely HRCP to be prescribed antibiotics by the trainers (32.8%). Although some trainers (27%) would consider prescribing prophylaxis antibiotics on patients' request, the majority (77.1%) would comply with the request if it was from a cardiologist/surgeon. Nearly half of the trainers (54.9%) who took part did want antibiotics if they were HRCP themselves. Even among those who did comply with the guidelines, 43.6% were keen to have prophylaxis antibiotics themselves (Table 1).
Trainees
Among the trainees the average age was 23.8 (22-35) years and the male to female ratio was 3:8. Only a few (15.3%) had a postgraduate qualification and the majority (94.1%) had heard of NICE guidelines but only 69.4% had read the guidelines. The majority of trainees (77.6%) would comply with the NICE guidelines regarding antibiotic prophylaxis in HRCP. The compliance was noted to be higher among the trainees who had read the guidelines (83%) over those who had not read them (65.4%). If antibiotics were to be prescribed, patients with a previous history of IE were most likely to be receiving it. Only a minority (3.5%) would adhere to patients' requests for antibiotics, while it was significantly higher if the request was made by a cardiologist/surgeon (74.1%). Nearly half of the trainees (48.2%) were keen to have antibiotic prophylaxis if they were HRCP themselves.
Discussion
The NICE guidelines have created a safer environment for the medical and dental professionals to work uninhibited and provide optimum patient care. The NICE committee guideline discouraging antibiotic prophylaxis for cardiac patients including HRCP was made on the basis of three findings: there is no correlation between having an interventional procedure and the development of IE, there is no clinical proof of the effectiveness of antibiotics and antibiotic prophylaxis may lead to an increase in the number of deaths from fatal anaphylaxis than a strategy of no antibiotic prophylaxis.2
Despite the wide dissemination of the existence of NICE guidelines for antibiotic prophylaxis for IE, results from this study confirm that much needs to be done to improve the understanding of this guideline among current dental trainers and trainees. Although majority of the trainers (95.7%) and trainees (94.1%) were aware of this guideline, only 62% of the trainers and 69.7% of the trainees had read the complete guideline or its summary.
A relatively low number of trainers (55.7%) and trainees (77.6%) complied with the NICE guideline by not prescribing antibiotics to HRCP; excluding external influences such as requests from specialists. The greater compliance observed among the trainees could be due to improved awareness having just completed their undergraduate training. This cannot be exploited to excuse the low compliance among the trainers, however, as they are meant to have implemented NICE changes since 2008 and should have a better understanding due to their teaching commitments.
It was interesting to note that the compliance among trainers and trainees who had read the guidelines were higher when compared to those who did not read it. Vocational trainees who had read the guideline had an increased compliancy rate of 83%. Among those who had not read it, 65.4% had an increased compliancy rate; a greater percentage than the complying trainers who had read the guideline (62.8%). Having come from a learning, university environment, the trainees could have been regularly reminded of the NICE guidelines and reinforced current practice of antibiotic prophylaxis through regular tutorials, lectures and examinations. This could have led to greater compliancy and understanding among trainees than trainers. A study by Thornhill et al.3 has identified that despite the introduction of the guideline in 2008, 20% of general dental practitioners (GDPs) routinely prescribe antibiotic prophylaxis for cardiac patients. Therefore this could also be a plausible explanation for the difference between the trainees and trainers' compliancy rate for both sub groups (those who have and have not read the guidelines) which stands at 20% (Table 2).
The results of the study also identified trainers to be susceptible to patient requests for prophylaxis antibiotics (26.8%). Soheilipur et al.6 who carried out a qualitative study of patient perspectives and understanding of the NICE guideline, confirm that in certain patient groups antibiotic prophylaxis was seen by some as an insurance against IE, with positive psychological effects. Prior history of receiving prophylaxis and long standing history with their GDP may cause the dental trainers to maintain good cordiality and hence prescribe antibiotics. It could be suggested that as trainees have no precedent with their patients, they are more likely to refuse the patient's request.
Within this study trainers were more likely to prescribe prophylaxis antibiotics for HRCP than the trainees except for patients with hypertrophic cardiomyopathy. It might be interpreted that the trainers are more set in their ways and are more comfortable prescribing. Despite this, both trainers and trainees should be made aware of the conclusion of the Cochrane Collaboration, which states that as long as dentists adhere to current published guidelines there is little course for redress and one is eminently defensible in a court of law. In the exacting criteria of their review paper, only a single study from The Netherlands was deemed suitable with 24 cases. The results of which were once again inconclusive with regard to the efficacy of antibiotic prophylaxis.7
The majority (74-76%) of dental trainers and trainees would equally prescribe antibiotics on the cardiologist/surgeon's request. Although such understanding among medical and dental professionals is paramount; individual beliefs and preferences should not undermine the existence of clearly stated guidelines and one should not shy away from questioning the validity for the variation from the set guideline.
According to the 'Bolam' principle under English law, a clinician cannot be found to be negligent if they have acted in accordance with a practice which is regarded as being appropriate by a responsible body of people working within their field. Therefore, it will be difficult to defend a dentist who does not adhere to the accepted guidelines. Even when requests are made in writing from medical or surgical clinicians, when it clearly conflicts with guidelines issued by NICE it may be difficult to defend. According to Dental Protection Limited (DPL); 'Dentists working within an NHS contract are required under the terms of their contract to observe the guidance of NICE when writing prescriptions. Clinicians working privately may not have a contractual obligation to follow this guidance, but they would need a very strong justification for choosing not to do so.'8 This conflict of opinion needs to be discussed with the clinician and the patient concerned to reach an amicable decision. Eminent medical associations and committees such as the AHA and ESC advise that antibiotics be prescribed for the HRCP. This could lead to the loss of autonomy and opinion of GDPs as the majority will defer to those who are more specialised.9. A significant proportion of both trainers (54.9%) and trainees (48.2%) would want antibiotics themselves if they were HRCP. This could be seen as basic self-interest and an assumption that positive psychological effects of antibiotic prophylaxis would ensure future good health. Should a dose be prescribed there is no universally accepted dose, the AHA suggests 2 mg amoxicillin, pre NICE it was 3 mg and the Australian guidelines suggest 2 mg 30-60 min pre procedure. The NICE committee quoted a risk of fatal anaphylaxis of approximately 20 per million administrations of penicillin, but the figure was mainly based on published 1960s data.10 The AHA reported it was unaware of any cases of fatal anaphylaxis resulting from the administration of penicillin in a 50 year period.11.
NICE is, however, a unique organisation in that it considers cost effectiveness. Due to this and the insufficient evidence of effectiveness or ineffectiveness of antibiotics it has been debated whether a cost effectiveness decision is beyond the remit of NICE. It is not a body constituted to undertake research.12 Ultimately what NICE presents are just guidelines, all cases must be assessed on their own merits. However, to make an informed and justifiable decision one must have at least read the guideline and understood the fundamentals behind them. It would be easier if GDPs had a more global consensus with regard to antibiotic prophylaxis, like that of the wisdom tooth guideline, but that is just an ideal.
Conclusion
This study confirms that dental trainers and trainees are well aware of the existence of the NICE guideline for antibiotic prophylaxis for IE. Despite this, a significant number of participants in both groups have not read the guideline. Reading the guideline has improved the understanding, which is reflected in their practice of antibiotic prophylaxis in HRCP. The majority would adhere to requests from medical professionals for antibiotic prophylaxis and would consider having it themselves if they were HRCP. Much needs to be done to formulate a universal guideline, which should be ethical, legal and easy to follow for both dental trainers and trainees alike.
References
National Institute of Clinical Excellence. Prophylaxis against infective endocarditis. London: NICE, 2008. Online guidelines available at http://www.nice.org.uk/nicemedia/pdf/CG64NICEguidance.pdf (accessed April 2012).
Chambers J B, Shanson D, Venn G, Pepper J . NICE v world on endocarditis prophylaxis. BMJ 2011; 342: d3531.
Thornhill M H, Dayer M J, Forde J M et al. Impact of the NICE guideline recommending cessation of antibiotic prophylaxis for prevention of infective endocarditis: before and after study: BMJ 2011; 342: d2392.
Rahman N, Roger S, Ryan D, Healy C, Flint S . Infective endocarditis prophylaxis and the current AHA, BSAC, NICE, Australian guidelines. J Ir Dent Assoc 2008; 54: 264–270.
Daly C G, Currie B J, Jeyasingham M S et al. A change of heart: the new infective endocarditis prophylaxis guidelines. Aust Dent J 2008; 53: 196–200.
Soheilipour S, Scambler S, Dickinson C et al. Antibiotic prophylaxis in dentistry: part II. A qualitative study of patient perspectives and understanding of the NICE guideline. Br Dent J 2011; 211: E2.
Oliver R, Roberts G J, Hooper L, Worthington H V . Antibiotics for the prophylaxis of bacterial endocarditis in dentistry. Cochrane Database Syst Rev 2008; 4: CD003813.
Dental Protection. Position statement: antibiotic prophylaxis. Issued 24 March 2008. Online statement available at http://www.dentalprotection.org/Default.aspx?DN=aea85b0b-f694-457e-8c09-61a4471cda8e (accessed July 2012).
Soheilipour S, Scambler S, Dickinson C et al. Antibiotic prophylaxis in dentistry: part I. A qualitative study of professionals' views on the NICE guideline. Br Dent J 2011; 211: E1.
Chambers J B, Shanson D, Hall R, Pepper J, Venn G, McGurk M . Antibiotic prophylaxis of endocarditis: the rest of the world and NICE. J R Soc Med 2011; 104: 138–40.
Wilson W, Taubert K A, Gewitz M et al. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anaesthesia and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc 2008; 139: 3–24.
Mohindra R K . A case of insufficient evidence equipoise: the NICE guidance on antibiotic prophylaxis for the prevention of infective endocarditis. J Med Ethics 2010; 36: 567–570.
Acknowledgements
We would like to thank Dr Elizabeth Jones, Dr Harish Patel and Dr Raj Rattan from the London Deanery for their kind advice and assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Farook, S., Davis, A., Khawaja, N. et al. NICE guideline and current practice of antibiotic prophylaxis for high risk cardiac patients (HRCP) among dental trainers and trainees in the United Kingdom (UK). Br Dent J 213, E6 (2012). https://doi.org/10.1038/sj.bdj.2012.723
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.723
This article is cited by
-
New dental graduates transition into UK professional practice; a longitudinal study of changes in perceptions and behaviours through the lens of evidence-based dentistry
BMC Medical Education (2024)
-
A longitudinal study of changes in new dental graduates' engagement with evidence-based practice during their transition to professional practice
British Dental Journal (2022)
-
Communicating new policy on antibiotic prophylaxis with patients: a randomised controlled trial
British Dental Journal (2013)
-
Lack of trainees
British Dental Journal (2012)