Key Points
-
Apex locators are valid tools for use in root length determination in general dental practice.
-
The use of apex locators may help reduce ionisation radiation exposure for patients undergoing root canal treatment.
-
This study highlights the importance of randomised controlled trials in primary dental care settings.
Abstract
Objective To evaluate the ability of apex locators as a tool in determining working length in comparison to traditional working length radiographs in general dental practice.
Design Randomised controlled clinical trial.
Setting General dental practices in the North West of England.
Subjects Adults requiring root canal treatment of at least one tooth with minimal or moderate difficulty.
Intervention Root canal treatment was carried out with the working length determined by apex locator in the treatment group (AL), and periapical radiograph in the control group (PA).
Outcome measure The acceptability of the master cone gutta percha measured from a radiograph before obturation was used as the primary outcome.
Results Twenty-one of 23 fillings in the AL group were judged as acceptable, compared to 17 of 23 fillings in the PA group. This difference was not statistically significant.
Conclusion In general dental practice, no significant difference was found in working length determined using apex locator combined with a master cone GP radiograph or using the conventional method. There is a need for larger trials to investigate these methods further.
Similar content being viewed by others
Introduction
Cleaning and shaping of the root canal system is an essential part of root canal treatment in order to remove the inflamed or necrotic pulp and associated micro-organisms. Root canal working length determination is an important aspect of the root canal treatment process, as it has been shown that a better long-term outcome can be predicted if the root filling is confined to the root canal system.1,2,3
The objective of determining the working length is to enable the root canal to be prepared as close to the apical constriction (AC) as possible. The apical constriction is considered the area of the root canal with the narrowest diameter; it effectively reflects the junction point between the pulpal and the periodontal tissue. The position of the AC normally varies between 0.5 and 2 mm from the radiographic apex (RA). The RA is the apical-most part of the root viewed on a radiographic image.4,5
Traditionally, the working length has been determined using intraoral periapical radiographs. However, a radiograph is a two dimensional image of a three dimensional object.6 A study on extracted teeth found when placing files to the radiographic apex, only 82% appeared to be at the actual apical foramen (AF) where the root canal terminates and communicates with the apical periodontal ligament fibres.7 Dense bone and anatomical structures can make the radiographic visualisation of root canal files unfeasible by obscuring the apex. In addition, the superimposition of the zygomatic arch has been shown to interfere radiographically with 20% of maxillary first molar and 42% of maxillary second molar apices.8
Electronic apex locators (EAL) were first described in 1962.9 The recent generation of EALs have become a reliable tool for working length determination and are clinically utilised in combination with radiographs.10,11,12 EALs were reported to have an accuracy of 90% to within 0.5 mm of the apical cemento-dentinal junction, with reports of 100% accuracy to within 1.0 mm.13 Although the accuracy of apex locators has been evaluated in the dental literature, they are still not widely used in general dental practice.14,15,16,17
There are a substantial number of teeth that receive root canal treatment in any given year within the National Health general dental service (GDS) in England and Wales. For example, in the year ending March 2004, 1,001,675 root canal fillings were placed within the GDS, at a cost of £50.5 million.18
A survey of 350 dentists in England showed that 44.5% of general dental practitioners use EALs for endodontic treatment.19 Of those using EALs, confirmatory working length radiographs were either never or occasionally taken by 48% of the respondents.
The combined use of an apex locator alongside radiographic confirmation is recommended by the Royal College of General Dental Practitioners' guidelines and the European consensus on this issue.20,21 The sole use of EALs could reduce the exposure to ionising radiation to the patient and the operator and save clinical time during root canal treatment.22,23 However, the evidence available to advocate the sole use of EAL is lacking.
The aim of this study was to evaluate the ability of apex locators in determining working length compared with a traditional working length radiograph in general dental practice, and to investigate the potential for a larger scale randomised controlled trial. The trial was set to test the null hypothesis that there is no difference between EALs or periapical radiographs in determining working length from the radiographic apex to the master cone gutta percha.
Materials and methods
Setting and subjects
This study was a pilot randomised controlled trial in general dental practices in the North West of England, with two parallel groups randomised in a 1:1 ratio. Three general dental practitioners were invited to take part. The dentists were given a training session which included didactic lectures, standardised protocols for root canal treatment and the use of apex locator. Ethical approval was gained from the National Research Ethics Service/England.
Adult patients who required root canal treatment of at least one tooth were invited to participate in the study. If a patient had multiple teeth requiring treatment, only one was included in the study. Preoperative radiographs were taken to confirm that the teeth chosen complied with the following inclusion criteria:
-
Minimal and moderate difficulty of proposed teeth required root canal treatments according to the American Association of Endodontists: Endodontic Case Difficulty Assessment Criteria.24
Following informed consent, the patients were randomised into one of the two study groups: apex locater (AL) treatment group and periapical (PA) radiograph control group.
Randomisation
Randomisation lists were produced by an independent statistician using computer-generated random numbers with random variable block size stratified for the dentists and the degree of difficulty (minimum or moderate). Allocation concealment was by sealed serially-numbered opaque envelopes. Each dentist stored their envelopes in a secure place and determined the type of treatment allocated for each patient by opening the next envelope in the sequence.
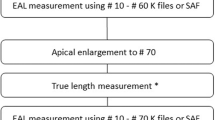
Root canal treatment
All teeth were isolated with dental dam and a standardised root canal treatment procedure was followed:
-
1
Access preparation to the root canal system, followed by chemo-mechanical preparation using the modified double-flare technique
-
2
Radicular access and initial enlargement with size 4, 3, and 2 Gates-Glidden burs (DENTSPLY, UK)
-
3
Working length determination: this was carried out using an apex locator (Ray-pex® 5, DENTSPLY, UK) in the AL group and measured as 0.5 mm from the apex locator 'zero' reading. In the PA group, radiographs were taken using standardisation holder (Endo Bite, Kerr, US) to ensure a paralleling technique and with an endodontic file in situ. The file was adjusted to 0.5mm short of the radiographic apex. The files used for working length determination were either size 10 or 15 (K-flexofiles, DENTSPLY, Switzerland)
-
4
Apical preparation: the root canal preparation was completed by hand instrumentation (K-flexofiles, DENTSPLY, Switzerland) and irrigated with 2% sodium hypochlorite (Melton, UK), 17% EDTA solution ((PulpDent, US) for 1 min and a final rinse with 0.2% chlorhexidine (GSK, UK) before being dried with paper points
-
5
A master cone gutta percha (GP) (DENTSPLY, UK) was measured to the working length determined by each method and inserted into the root canal, and a 'master cone' radiograph was taken for all teeth in both groups
-
6
Obturation was completed by the cold lateral compaction technique using gutta percha and a zinc oxide-eugenol sealer (Tubliseal EWT, Kerr, USA). This was followed by post-obturation radiographs for both groups.
The appointment time was recorded in minutes from the start of the root canal treatment procedure (placement of dental dam) to completion following the post-obturation radiograph.
Assessment of radiographs
A standard millimetre rule was placed onto the post-obturation radiograph adjacent to the image of the master cone and then both rule and radiograph were digitally scanned. This was repeated for all the radiographs. The digital images were then calibrated and assessed using SigmaScan Pro software (Systat, USA). The images were sent to a central location for assessment by two examiners who were not involved in the treatment of any participants. Inter- and intra-examiner reliability were assessed. Where any discrepancy existed between the two examiners a consensus was reached. For multi-rooted teeth, the palatal root of the maxillary molars and the distal root of the mandibular molars were assessed.
The distance between the master cone GP and the radiographic apex was measured in millimetres and recorded. The master cone GP was then classified as acceptable or not acceptable depending on the position of GP in relation to the radiographical apex. 'Acceptable' was recorded when the master cone GP was at or less than 2 mm away from the radiographic apex. However, 'not acceptable' was recorded when the master cone GP was under-extended by more than 2 mm, or over-extended by greater than 0.5 mm and therefore adjustment was required before obturation.1,2
Outcome measures
The acceptability of the master cone GP, as defined above, was used as the primary outcome. Further outcome measures were the distance between the master cone GP and the root apex, and the total time taken for the procedure.
Sample size
The sample size for this pilot was set at 50 patients.
Data analysis
The mean differences between groups in the acceptability of the master cone GP, distance from filling to apex, and in total reported time taken to complete the treatment was calculated, with 95% confidence intervals. Due to the skewed distribution observed for the treatment time variable, the total reported time taken to complete the treatment was compared between groups using the Mann Whitney U test.
Results
A total of 51 patients were recruited. Assessment of the primary outcome data for five cases was excluded due to inadequate clarity for radiographic software assessment. Therefore, a total of 46 cases were acceptable for use in the study. Participant flow through the trial is shown in Figure 1. Table 1 shows age, gender, and degree of difficulty for the two randomisation groups.
The assessed inter- and intra-examiner reliability revealed good agreement (kappa = 0.8 and 0.89, respectively).
Twenty-one of the 23 fillings in the AL group were judged to be acceptable (91%), compared to 17 of 23 in the PA group (74%). This is an observed difference in proportions of 17% (95% confidence interval −4% to 39%), and corresponds to a relative risk of an unacceptable filling in the PA group of 3.0 (95% confidence interval 0.7 to 13.3).
The mean length from the tip of the master cone GP to the radiographic apex was 1.06 mm (SD = 0.67) for the AL group, compared to 1.23 mm (SD = 0.72) in the PA group (mean difference −0.18 mm, 95% confidence interval −0.60 to 0.25).
The median reported time taken for treatment in each group was 90 minutes (interquartile range 45).None of the observed differences were statistically significant at the 5% level.
Discussion
The difficulties in accurately determining the apical point to which a root filling should extend are well recognised, with differences observed between the position of the anatomical apex and the radiographic apex.25 Nevertheless, it is widely accepted that placement of the root filling within 2 mm of the radiographic apex significantly affects the success of root treated teeth.1,2,3,26 Although until now no studies have investigated working length determination methods in relation to the clinical outcomes, there is available evidence to support the association between clinical outcome and root canal filling within 2 mm from the radiographic apex.26
Apex locators have become a valuable clinical tool for assessing root canal length and may have the capacity to improve clinical outcomes, decrease radiation dose and decrease clinical time. However, at present there is no high level evidence to confirm whether apex locators are as reliable as periapical radiographs in ascertaining the root canal length. The current study found similar results to recent reports which found no difference when comparing the use of apex locator and length determining radiograph.27,28,29 However, this randomised controlled clinical trial evaluated the effectiveness of apex locator in the hands of general dental practitioners, who undertake the majority of routine root canal treatments, in contrast to previous reports which were performed in more controlled specialist environments.
In this study, all dentists were trained to ensure that they used a standardised, recognised endodontic technique and that the primary variable would be the use of an apex locator or a working length radiograph. However, with the provision of dental treatment, there is always inherent variability such as number of root canals present, differences in root canal shape, the age of the patient and amount of sclerotic dentine. This has been addressed by the inclusion criteria which involved only teeth with mild to moderated endodontic difficulty and measurements of palatal roots of maxillary molars and distal roots for mandibular molars. The measurements were also made comparable by ensuring that working length recording using both techniques was standardised to take place before apical preparation.
The Ray-pex® 5 (DENTSPLY, UK) apex locator, which is a 4th generation apex locator, was chosen as it is easy to use even in wet canals, and has a high level of accuracy.30 Although Stoll et al.31 reported that the interpretation of the colour-coded zones as to the foramen might lead to erroneous interpretations, this did not seem to affect the results of this study. This could be due to the protocol adopted in this study where the zero point was identified from EAL screen and then half a millimeter distance was subtracted from the file length.
In this study the root canal length was determined by two methods and verified using master cone GP radiographs, where the master cone GP was placed to the recorded working length. The radiographic assessment is only capable of determining the relationship of the master cone to the radiographic apex and not to the anatomical apical foramen or constriction. However, this method of radiographic assessment is widely used in clinical studies in the literature as a method of determining satisfactory root canal treatment.1,2,3,26
If the outcome measure is deemed acceptable, this does not necessarily mean that the root canal filling is actually within the root canal system, because the anatomical foramen may be 2 or 3 mm away from the radiographic apex. This problem may affect the PA group more than the AL group. On the other hand, when using the apex locator, a root canal filling may appear to be short on a radiograph (more that 2 mm) but in fact it is at or close to the apical foramen. The available assessment technique does not allow the operator to assess if the root filling is confined to the root canal system. Cone beam CT may provide a new standard for assessment of root canal success, however the high radiographic dose, low resolution and expense may hinder its use.32
In this study, the apex locator was only used once to measure root canal length. This single use method was used to simulate the most common practice by general dental practitioners. However, this can lead to inaccuracies due to changes in length of the canals after preparation, especially in curved roots. In addition, other factors such as the presence of vital tissue, irrigants in the canals, metal restorations or caries can lead to inaccurate readings.10 Therefore, a more reliable method to confirm the working length may be to utilise the apex locators throughout the root canal treatment.
Although using the apex locator to determine the working length gave a higher proportion of acceptable GP master cones, this pilot study was not powered to detect a statistically significant difference between the two groups.
Conclusions
In general dental practice, no significant difference was observed in working lengths when determined using an apex locator combined with a master cone GP radiograph or using the conventional method. There is a need for further studies to assess the effectiveness of different methods of working length determination and their effect on the clinical outcome of root canal treated teeth in general dental practice.
References
Sjogren U, Hagglund B, Sundqvist G, Wing K . Factors affecting the long-term results of endodontic treatment. J Endod 1990; 16: 498–504.
Farzaneh M, Abitbol S, Lawrence H P, Friedman S . Treatment outcome in endodontics – the Toronto Study. Phase II: initial treatment. J Endod 2004; 30: 302–309.
Schaeffer M A, White R R, Walton R E . Determining the optimal obturation length: a meta-analysis of literature. J Endod 2005; 31: 271–274.
Kuttler Y . Microscopic investigation of root apexes. J Am Dent Assoc 1955; 50: 544–552.
Dummer P M, McGinn J H, Rees D G . The position and topography of the apical canal constriction and apical foramen. Int Endod J 1984; 17: 192–198.
Simon S, Machtou P, Adams N, Tomson P, Lumley P . Apical limit and working length in endodontics. Dent Update 2006; 36: 146–153.
Olson A K, Goerig A C, Cavataio R E, Luciano J . The ability of the radiograph to determine the location of the apical foramen. Int Endod J 1991; 24: 28–35.
Tamse A, Kaffe I, Fishel D . Zygomatic arch interference with correct radiographic diagnosis in maxillary molar endodontics. Oral Surg Oral Med Oral Pathol 1980; 50: 563–566.
Sunada I . New method for measuring the length of the root canal. J Dent Res 1962; 41: 375–387.
Gordon M P, Chandler N P . Electronic apex locators. Int Endod J 2004; 37: 425–437.
Kim E, Lee S J . Electronic apex locator. Dent Clin N Am 2004; 48: 35–54.
ElAyouti A, Dima E, Ohmer J, Sperl K, Von Ohle C, Löst C . Consistency of apex locator function: a clinical study. J Endod 2009; 35: 179–181.
Pagavino G, Pace R, Baccetti T . A SEM study of in vivo accuracy of the Root ZX electronic apex locator. J Endod 1998; 24: 438–441.
Hoer D, Attin T . The accuracy of electronic working length determination. Int Endod J 2004; 37: 125–131.
Tselnik M, Baumgartner J C, Marshall J G . An evaluation of Root ZX and Elements diagnostic apex locators. J Endod 2005; 31: 507–509.
Haffner C, Folwaczny M, Galler K, Hickel R . Accuracy of electronic apex locators in comparison to actual length – an in vivo study. J Dent 2005; 33: 619–625.
Goldberg F, Marroquin B B, Frajlich S, Dreyer C . In vitro evaluation of the ability of three apex locators to determine the working length during retreatment. J Endod 2005; 31: 676–678.
Dental Practice Board. DPB digest of statistics. Eastbourne, UK: Dental Practice Board, 2004.
Molyneux L, Mccullough C, Preston A J, Jarad F D . Apex locator use by general dental practitioners in Merseyside. J Dent Res 2008; 87(Spec Iss C): Abstract number 0166 (PEF IADR). Available from: http://iadr.confex.com/iadr/pef08/techprogram/abstract_111422.htm.
Faculty of General Dental Practice (UK) of the Royal College of Surgeon of England. Selection criteria for dental radiography. London: FGDP(UK), 2004.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921–930.
Saad A Y, al-Nazhan S. Radiation dose reduction during endodontic therapy: a new technique combining an apex locator (Root ZX) and a digital imaging system (RadioVisioGraphy). J Endod 2000; 26: 144–147.
Brunton P A, Abdeen D, MacFarlane T V . The effect of an apex locator on exposure to radiation during endodontic therapy. J Endod 2002; 28: 524–526.
American Association of Endodontists. AAE endodontic case difficulty assessment form and guidelines. Endodontics: Colleagues for Excellence 2005; Spring/Summer: 6–7. Available from: http://www.aae.org/uploadedFiles/Publications_and_Research/Endodontics_Colleagues_for_Excellence_Newsletter/ss05ecfe.pdf.
Williams C B, Joyce A P, Roberts S . A comparison between in vivo radiographic working length determination and measurement after extraction. J Endod 2006; 32: 624–627.
Ng Y L, Mann V, Rahbaran S, Lewsey J, Gulabivala K . Outcome of primary root canal treatment: systematic review of the literature – part 2. Influence of clinical factors. Int J Endod 2008; 41: 6–31.
Smadi L . Comparison between two methods of working length determination and its effect on radiographic extent of root canal filling; a clinical study. BMC Oral Health 2006; 6: 4.
Kim E, Marmo M, Lee C-Y, Oh N-S, Kim I-K. An in vivo comparison of working length determination by only Root-ZX apex locator versus combining Root-ZX apex locator with radiographs using a new impression technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105: e79–e83.
D'Assunção F L, Albuquerque D S, Salazar-Silva J R, Dos Santos V C, Sousa J C . Ex vivo evaluation of the accuracy and coefficient of repeatability of three electronic apex locators using a simple mounting model: a preliminary report. Int Endod J 2010; 43: 269–274.
Wrbas K T, Ziegler A A, Altenburger M J, Schirrmeister J F . In vivo comparison of working length determination with two electronic apex locators. Int Endod J 2006; 40: 133–138.
Stoll R, Urban-Klein B, Roggendorf M J, Jablonski-Momeni A, Strauch K, Frankenberger R . Effectiveness of four electronic apex locators to determine distance from the apical foramen. Int Endod J 2010; 43: 808–817.
Patel S, Kanagasingam S, Mannocci F . Cone beam computed tomography (CBCT) in endodontics. Dent Update 2010; 37: 373–379.
Acknowledgements
This study was funded by the NHS Research and Development Fund, Royal Liverpool and Broadgreen University Hospitals Trust, England. The authors acknowledge the contribution of Mr Ashley Jones in carrying out the randomisation procedure.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Jarad, F., Albadri, S., Gamble, C. et al. Working length determination in general dental practice: a randomised controlled trial. Br Dent J 211, 595–598 (2011). https://doi.org/10.1038/sj.bdj.2011.1052
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2011.1052