Key Points
-
Provides an overview of dental prescribing pattern in Wales.
-
Highlights the potential inappropriate prescribing of antibiotics by dentists.
-
Highlights the limited use of systemic antibiotics in dentistry and the need for education for dentists and the public.
-
Argues for a surveillance system of dental prescribing at practice/practitioner level so that inappropriate prescribing can be managed.
Abstract
Dental prescribing data in Wales have not been studied in detail previously. The analysis of national data available from Health Solutions Wales showed that dental prescribing in Wales accounted for 9% of total antibacterial prescribing in primary care in 2008. Penicillin and metronidazole constituted the bulk of antibiotics prescribed by dentists. Since the publication of National Institute for Health and Clinical Excellence (NICE) guidance (March 2008) on prophylaxis against infective endocarditis, dental prescriptions for amoxicillin 3g sachets and clindamycin capsules have decreased. Dental prescriptions for fluoride preparations increased in number from 2007 to 2008. Dental prescribing of controlled drugs raises no concern. The figure for antibiotic prescribing in Wales is similar to that of England. Nevertheless, the figure seems a little high, indicating potential inappropriate prescribing behaviour among dentists. Antibiotic resistance is a major public health issue and many patients each year die from infections from bacterial strains that are resistant to one or more antibiotics. Inappropriate use of antibiotics is a major cause of antibiotic resistance and every effort should be made to reduce the number of inappropriate antibiotic prescriptions in dental practice.
Similar content being viewed by others
Introduction
Dentists can only prescribe a limited number of drugs through the National Health Service (NHS). Dentists may only prescribe medicines through the NHS if they are listed in the Dental Practitioners' Formulary (DPF). However, the Act and Regulations in the UK do not limit the number and variety of drugs a dentist may administer to patients in the surgery and/or may order by private prescription, as long as they are needed for the clinical situation.
The NHS database in Wales captures and records all items prescribed by the dentists via the NHS form WP10D. However, it does not include any drugs, except controlled drugs, prescribed by the dentists on private prescriptions.
Analysis of dental prescribing data provides useful information on important public health issues such as antibiotic prescribing patterns and trends, the use of fluoride preparations for the prevention of decay and also the prescribing of controlled drugs. At the time of writing this paper, unlike in England, there is no charge for prescription items for patients in Wales.1
A report on dental prescribing in England was recently published by the NHS Information Centre.2 However, no such report exists for Wales. This paper provides an overview of dental prescribing in Wales and discusses some important public health issues.
Methods
Prescribing data for 2007 and 2008 were analysed using the Comparative Analysis System for Prescribing Audit (CASPA) software version 3.3.2, produced by Health Solutions Wales (HSW) and all figures shown in this report represent calendar years, that is, January–December. This data does not include the drugs prescribed and dispensed within hospitals in Wales. This data does not include drugs prescribed privately, with the exception of controlled drugs.
Dental prescribing data is only available at a national (Wales) level because, unlike General Medical Practitioners' (GPs') prescriptions, the prescription forms for dental practitioners do not identify their specific practice locations or their associated Local Health Board (LHB).
Results
The majority of dental items prescribed on the NHS are within British National Formulary (BNF) Chapter 5: Infections. Table 1 shows the dental prescriptions from the leading BNF chapters in 2007 and 2008.
Table 2 identifies how dental prescribing compares with all-community prescribing for the major BNF sections. A total of 481,031 items of antibiotics were prescribed by dentists from January 2007 to December 2008. Table 2 also shows that 9% of all antibacterials prescribed annually in primary care were prescribed by dentists. In 2008, dentists prescribed 36% of all items prescribed under the mineral section and 32% of the drugs acting on the oropharynx. Very few analgesics from BNF Chapter 4.7 (4,404 items in 2007 and 4,872 in 2008) were prescribed by dentists. Overall, there was a slight increase (1.3%) in prescriptions for anti-bacterial drugs from 2007 to 2008.
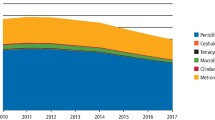
Penicillins and metronidazoles were the two most commonly prescribed antibiotics by primary care dentists in Wales (Table 3). During 2007 and 2008, penicillins accounted for 67% of antibacterial drugs prescribed by dentists in Wales. While there was a slight (0.4%) increase in the items of penicillin prescribed by dentists from 2007 to 2008, prescriptions for clindamycin, macrolides and tetracycline decreased by 23.7%, 0.9% and 12.1% respectively (Table 3).
There was a 43.7% decrease in the prescription of amoxicillin 3 g sachets from 2007 to 2008. Data indicate that there was a decrease in the prescriptions of amoxicillin 3 g sachets and clindamycin capsules following the publication of the NICE guidance on prophylaxis against infective endocarditis (Fig. 1).3
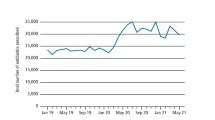
Within the Minerals section of the BNF, preparations containing fluoride were the only items prescribed by dentists. Primary care dentists in Wales prescribed a total of 19,441 and 30,252 fluoride preparation items in 2007 and 2008 respectively (Table 2), which represents an increase of 56%. Table 4 shows the three key prescribed product groups that have been the main drivers for this increase. Dental prescribing of fluoride items accounted for 91% of all prescribed fluoride items in 2007 and 86% in 2008. The remaining fluoride items were prescribed by the GPs and other independent prescribers.
The number of controlled drugs prescribed by dentists in Wales was minimal. A total of 2,171 and 2,052 items of controlled drugs were prescribed by dentists in Wales in 2007 and 2008. Table 5 shows the various controlled drugs prescribed by the dentists in Wales in 2007 and 2008. In 2008, the majority (60%) of the controlled drugs prescribed by the dentists consisted of the Schedule 5 drug dihydrocodeine.
Discussion
Analysis of data on dental prescribing in primary care has shed light on the prescribing pattern of NHS dentists in Wales. There are no local or national systems in place to capture private prescribing, except controlled drugs, by dentists and other professionals working in primary care. Hence, the level of prescribing under private arrangements for drugs other than controlled drugs is unknown.
During the 24 months ending 31 December 2008, 1,630,493 patients were seen or treated4 and 481,031 items of antibiotics were prescribed by NHS dentists in Wales. This equals to one item of antibiotic for every 3.4 dental patients. However, it must be noted that the same patient may have received multiple items of antibiotics. Considering the limited indications for use of antibiotics in dentistry, the antibiotic figure in Wales suggests the potential inappropriate use of antibiotics by dentists working in primary care. Previous studies have found inappropriate antibiotic prescribing by dentists in England and Wales.5,6
The figure of dental antibiotic prescriptions in Wales raises some concerns. Inappropriate use of antibiotics contributes towards antimicrobial resistance and concomitant costs to the NHS. In addition, there are potential side effects to antibiotic use such as sensitisation, skin rashes and, on rare occasions, anaphylactic shock and even death.
With the wide and injudicious use of antibiotics, there have emerged many strains of bacteria that are resistant to common antibiotics. The widely publicised and known strain called Methicillin Resistant Staphylococcus Aureus (MRSA) is associated with many deaths in hospitals.7,8 Many oral bacteria are resistant to commonly used penicillin.8,9
There is a limited role for antibiotics in dentistry. Local surgical interventions should be the first-choice treatment.10 The majority of patients with dental pain can be managed without the use of antibiotics. Systematic reviews have shown that systemic antibiotics do not have a role in the management of irreversible pulpitis and acute apical periodontitis.11,12 Further research is required to find out what dental conditions dentists prescribe antibacterial drugs for and their reasoning behind the prescriptions. Similarly, non-clinical factors that influence dentists' antibiotic prescribing behaviour should also be explored.
There seems to be a need to educate primary care dentists as well as the public about the limited role of systemic antibiotics in the management of dental conditions. Since the publication of the NICE guidance on prophylaxis against infective endocarditis3, the dental prescribing of amoxicillin 3 g sachets and clindamycin 150 mg capsules have decreased. Similar publication of guidance on the use of antibiotics in dentistry by NICE could also decrease the overall prescription of antibiotics.
The LHBs could monitor the number of dental prescriptions for antibacterial drugs in their area. Currently this can be done through monitoring of the number of dental claims for payment (FP17s) with prescriptions and carrying out an audit on antibiotic prescriptions. However, for better accuracy, a system will need to be developed where national dental prescribing patterns can be analysed at dental practitioner or practice level. The Prescribing Services Unit (PSU) within Health Solutions Wales is currently scoping for the development of such a system in Wales. Similarly, the proposed inclusion of antibiotic prescriptions on dental claim forms, FP17s, should also facilitate such monitoring at practice or practitioner level. However, data obtained via FP17s will be reliable if the details required in these forms are completed by all dentists. In the meantime, the LHBs should consider monitoring the number of antibacterial prescriptions issued at out-of-hours dental services. Audit in combination with guideline and education has been successfully used to reduce the number of inappropriate antibiotics prescriptions in dentistry.13
There are no local dental formularies or national prescribing guidelines for dentists in Wales. A randomised controlled trial carried out in Wales14 found that provision of educational material or guidelines did not result in a significant reduction in the inappropriate prescribing of antibiotics by dentists in Wales. However, the postage of educational material followed by an academic detailing visit by a trained pharmacist was successful in reducing the number of inappropriate antibiotic prescriptions.14 The employment of such academic detailers for all dental practitioners in Wales would require a considerable amount of resources. However, once the system of data analysis at practitioner level is established, a targeted approach of academic detailing could be employed.
Supplemental fluorides are effective in preventing dental decay.15,16,17,18,19 Dentists can prescribe fluoride in various forms such as high concentration fluoride toothpastes, mouthwashes and fluoride tablets. In the absence of water fluoridation in Wales, it was encouraging to see, from the prescription data, the increase in prescriptions for fluoride in primary care. There is a high level of dental decay in many deprived areas in Wales. Dentists practising in these areas can play a crucial role in the prevention of dental decay in the population.
The Welsh Assembly Government recently rolled out Designed to Smile, the national fluoride supplementation programme which aims to increase the exposure of topical fluoride to children's teeth in Wales. The core of this programme includes supervised toothbrushing and is mainly delivered from the school/nursery setting. LHBs should work with the dentists in their area to maximise the impact of this programme with complementary increase in fluoride exposure via practice setting, especially in the most deprived areas. Similarly, the use of supplemental fluoride on patients could be included in the basket of indicators used for monitoring dental contracts. Effective oral health prevention programmes are required to decrease the prevalence of dental decay, which in turn should result in a decrease in dental infections and the use of antibiotics.
Controlled drug prescribing by the dentists in Wales during 2007 and 2008 does not show any alarming pattern. The data captured here includes privately prescribed controlled drugs. A dentist can prescribe privately any Schedule 2 or 3-controlled drug on a WP10PCD form, as long as it meets the dental needs of the patient.
There is a limited role of controlled drugs in dentistry. Opioids are not effective analgesics and their use should remain low. Temazepam, diazepam and nitrazepam are occasionally used on some dentally anxious patients in addition to other management techniques. Midazolam is used for sedation by some dentists in the dental surgery but can not be prescribed for patients' use outside the dental practice. Pethidine was removed from the NHS dental formulary in April 2009.
The Controlled Drugs (Supervision of Management and Use) (Wales) Regulations 200820 came into force in Wales in January 2009. Local Health Boards now have a statutory responsibility to monitor the use and management of controlled drugs by all healthcare professionals including dentists. An accountable officer within each LHB is responsible for discharging these functions. The LHBs should ensure that any audit on use of controlled drugs is linked to their dental clinical governance framework. All dentists who store and use controlled drugs are required to have standard operating procedures on management of controlled drugs.
Conclusion
While the fluoride prescribing pattern in Wales is encouraging, antibiotic prescription figures raise some concern. Antibiotic resistance can lead to increased mortality and morbidity and imposes significant costs on the NHS, patients and society. Hence, the introduction of surveillance and management systems for the dental prescribing pattern is important. Regardless of the control systems in place, every dentist should think about the potential implications of their actions when they prescribe antibiotics to those patients who can be managed without.
References
National Health Service, Wales. National Health Service (Free Prescriptions and Charges for Drugs and Appliances) (Wales) Regulations 2007. Cardiff: National Health Service, Wales, 2007. Accessed online at http://opsi.gov.uk/legislation/wales/wsi2007/wsi_20070121_en_1.
The NHS Information Centre, Prescribing Support and Primary Care Services. Prescribing by dentists 2007: England. London: The Health and Social Care Information Centre, Prescribing Support Unit, 2009. Accessed online at http://www.ic.nhs.uk/webfiles/publications/PrescribingDentists07/Prescribing%20by%20Dentists%202007.pdf.
National Institute for Health and Clinical Excellence. Prophylaxis against infective endocarditis: antimicrobial prophylaxis against infective endocarditis in adults and children undergoing interventional procedures. London: National Institute for Health and Clinical Excellence, 2008. Accessed online at http://guidance.nice.org.uk/CG64/Guidance/pdf/English.
Welsh Assembly Government, Health and Health care Statistics, StatsWales, Accessed online at http://www.statswales.wales.gov.uk/TableViewer/tableView.aspx?ReportId=3486.
Dailey Y M, Martin M V . Are antibiotics being used appropriately for emergency dental treatment? Br Dent J 2001; 191: 391–393.
Thomas D W, Satterthwaite J, Absi E G, Lewis M A, Shepherd J P . Antibiotic prescription for acute dental conditions in the primary care setting. Br Dent J 1996; 181: 401–404.
Office for National Statistics. Deaths involving MRSA: England and Wales, 2008. Newport: Office for National Statistics, 2009.
Lewis M A O . Why we must reduce dental prescription of antibiotics: European Union Antibiotic Awareness Day. Br Dent J 2008; 205: 537–538.
Sweeney L C, Dave J, Chambers P A, Heritage J . Antibiotic resistance in general dental practice - a cause for concern? J. Antimicrob Chemother, 2004; 53: 567–576.
Scottish Dental Clinical Effectiveness Programme. Drug prescribing for dentistry: dental clinical guidance. Dundee: Scottish Dental Clinical Effectiveness Programme, 2008. Accessed online at http://www.sdcep.org.uk/?o=2334.
Keenan J V, Farman A G, Fedorowicz Z, Newton J T . Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev 2005; (2): CD004969.
Sutherland S E, Matthews D C . Emergency management of acute apical periodontitis in the permanent dentition: a systematic review of the literature. J Can Dent Assoc 2003; 69(3):160–160L.
Palmer N A O, Dailey Y M, Martin M V . Can audit improve antibiotic prescribing in general dental practice? Br Dent J 2001; 191: 253–255.
Seager J M, Howell- Jones R S, Dunstan F D, Lewis M A, Richmond S, Thomas D W . A randomised clinical trial of clinical outreach education to rationalise antibiotic prescribing for acute dental pain in the primary care setting. Br Dent J 2006; 201: 217–222.
Marinho V C, Higgins J P, Logan S, Sheiham A . Fluoride gels for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2002; (2): CD002280.
Marinho V C, Higgins J P, Logan S, Sheiham A . Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003; (3): CD002284.
Marinho V C, Higgins J P, Logan S, Sheiham A . Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003; (1): CD002278.
Marinho V C, Higgins J P, Logan S, Sheiham A . Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2002; (3): CD002279.
Marinho V C, Higgins J P, Logan S, Sheiham A . Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003; (4): CD002782.
The Controlled Drugs (Supervision of Management and Use) (Wales) Regulations 2008. Welsh Statutory Instruments 2008; No. 3239 (W 286). Accessed online at http://www.opsi.gov.uk/legislation/wales/wsi2008/wsi_20083239_en_2.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Karki, A., Holyfield, G. & Thomas, D. Dental prescribing in Wales and associated public health issues. Br Dent J 210, E21 (2011). https://doi.org/10.1038/sj.bdj.2010.1179
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2010.1179
This article is cited by
-
Higher antibiotic prescribing propensity of dentists in deprived areas and those with greater access to care in the North East and Cumbria, UK
British Dental Journal (2018)
-
Dentists, antibiotics and Clostridium difficile-associated disease
British Dental Journal (2015)
-
General dental practitioners' perceptions of antimicrobial use and resistance: a qualitative interview study
British Dental Journal (2014)
-
Local operative measures
British Dental Journal (2013)
-
Antibiotics and oral contraceptives: new considerations for dental practice
British Dental Journal (2012)