Abstract
Objective:
To report and discuss the case of an incomplete paraplegic patient who died of pulmonary embolism (PE) aggravated by manual muscle testing.
Setting:
Acute spinal ward, Maharaj Hospital, Chiang Mai, Thailand.
Case report:
A 79-year-old man suffering from chest trauma, fractured ribs and a fracture of T11 with incomplete paraplegia, American Spinal Injury Association impairment scale D. Intercostal tubes were inserted at both sides due to haemothorax. Ten days after onset, T9 to L2 posterior instrumentation was successfully completed. A week after the operation, he was allowed to stand on a tilt-table and a rehabilitation specialist was consulted to assess and plan to encourage ambulation. After manual muscle testing of the right hip flexors and knee extensors, the patient suffered from a short period of unconsciousness and breathlessness. Electrocardiography showed right bundle branch block and a drop in oxygen saturation from 98 to 70%. After oxygenation with mask and bag, oxygen saturation increased to 90%. PE or acute myocardial infarction was suspected. After insertion of an endotracheal tube, the patient went into cardiac arrest. Cardiopulmonary resuscitation failed. The autopsy revealed large and small thromboemboli in both lungs, particularly in the pulmonary artery.
Conclusion:
Strong hip and knee muscle contractions during manual muscle testing were suspected of triggering massive pulmonary emboli from the proximal vein of the right leg of a paraplegic patient who had functional motor movements and did not receive any thromboembolic prophylaxis which caused unexpected fatal pulmonary emboli. Screening of venous thromboembolism risks and its symptoms/signs before mobilisation is mandatory.
Similar content being viewed by others
Introduction
The incidence of venous thromboembolism (VTE)—deep vein thrombosis (DVT) and pulmonary embolism (PE)—is low among Thai populations. According to our hospital statistical data in 2013, of all 27 383 patients discharged, only 18 cases (0.066%) developed DVT in the lower extremities during admission and out of 91 new traumatic spinal cord injury (SCI) patients, there was only 1 case (1.098%) diagnosed with PE. We are therefore reporting this fatal PE case that was aggravated due to manual muscle testing (MMT), and also discussing guidelines for screening and thromboprophylaxis for a population with low incidence of VTE.
Case report
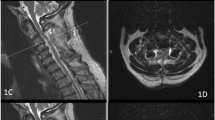
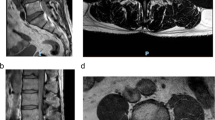
Fifteen minutes after a car accident, a 79-year-old man was transferred to a hospital. He had severe back pain with mild weakness of the left lower extremity due to a chance fracture of T11 and cord compression; and a mild traumatic brain injury (TBI). Hip flexors and knee extensors were graded 4 on the right and 2 on the left, other leg muscles were graded 5. No spasticity was detected. Electrocardiography (ECG) was normal on admission. Two days following admission, a chest X-ray revealed haemothorax on both sides that needed insertion of intercostal drainage (ICD) tubes and oxygen at 6 l min−1 was given to maintain oxygen saturation (O2sat) above 95%.
On day 10 of admission, posterior instrumentation was successfully completed and back pain was reduced. A week after the operation, ICD tubes were removed and the patient underwent mobilisation on a tilt-table for the first time. A day later, a rehabilitation specialist was consulted to advice on a programme for ambulation. Immediately after MMT of the right hip flexors and knee extensors (grade 5), the patient developed a short period of breathlessness and unconsciousness. O2sat dropped from 98 to 70% but increased to 90% after oxygenation with a mask and bag. ECG showed right bundle branch block (RBBB). PE or acute myocardial infarction (AMI) was suspected.
An endotracheal tube was inserted and then a few minutes after insertion the patient went into cardiac arrest. Cardiopulmonary resuscitation failed. An autopsy revealed large and multiple small thromboemboli in both lungs, particularly in the right pulmonary artery; but there was no evidence of AMI. To be noted, interventions against thrombosis or screening for possible VTE were not conducted due to the low incidence of VTE and nearly normal muscle power of both legs.
Discussion
This was the first case of fatal PE aggravated by MMT ever reported. We suspected that strong proximal leg muscle contractions during MMT dislodged thrombi from the veins in the right leg and/or pelvis and triggered the onset of PE. Unfortunately, our suspicion was not proven due to the lack of exploration of such vessels. Retrospectively, this case had multiple risks of VTE such as male gender, old age, chest trauma and TBI.1, 2 In addition, the fall of O2sat3 and the ECG showing RBBB4 were also associated with PE.
We agree with the NICE guidelines1 that the risks of VTE and bleeding should be assessed in all newly diagnosed SCI cases, and repeat assessment regularly carried out by observing symptoms/signs of DVT—pain, tenderness, swelling, warmth and discolouration of the affected leg.1, 2 Doppler ultrasonography should be requested to confirm the diagnosis. For early detection of PE, observe dyspnoea, pleuritic chest pain, hypotension, hypoxia and oxygen desaturation.1, 3 In addition, ECG is another useful screening test as RBBB is associated with PE.4
If there are the risks of VTE, the advice must be to follow the guidelines: offer combined VTE prophylaxis with mechanical and pharmacological methods—low-molecular-weight heparin is preferable.1 For less well-resourced countries with a low VTE prevalence, recommended mechanical methods such as anti-embolic stockings and intermittent pneumatic compression devices1 are usually not available. Range of motion exercises (ROMEs) and elastic bandaging should be started as early as possible. In addition, staff should be aware of the possibility of an unexpected thromboembolic event when patients start weight-bearing. Calf girth and any signs of DVT should be re-checked before doing MMT and ROMEs.
In conclusion, this case reminds us that MMT of the lower extremities with strong muscle power could aggravate pulmonary emboli. In a population with a low incidence of VTE, risk factors should be assessed. Anticoagulant prophylaxis should be prescribed for those at risk. Mechanical methods such as exercises and elastic bandaging should be started as early as possible. Regular re-assessment of symptoms/signs of VTE and bleeding for early diagnosis and proper management must be carried out.
References
National Clinical Guideline Centre-Acute and Chronic Conditions (UK). Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital. Royal College of Physicians (UK): London, UK. 2010.
Maung AA, Schuster KM, Kaplan LJ, Maerz LL, Davis KA . Risk of venous thromboembolism after spinal cord injury: not all levels are the same. J Trauma 2011; 71: 1241–1245.
Pulido L, Grossman S, Smith EB, Joshi A, Purtill JJ, Parvizi J et al. Clinical presentation of pulmonary embolus after total joint arthroplasty: do size and location of embolus matter? Am J Orthop (Belle Mead NJ) 2010; 39: 185–189.
Frisbie JH, Sharma GV . Right bundle branch block as a screening test for pulmonary embolism in chronic spinal cord injury. Arch Phys Med Rehabil 2009; 90: 1241–1244.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kovindha, A., Kammuang-lue, P. Pulmonary embolism after manual muscle testing in an incomplete paraplegic patient: a case report. Spinal Cord 52 (Suppl 3), S6–S7 (2014). https://doi.org/10.1038/sc.2014.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.121