Abstract
Study Design:
A 6-month retrospective study.
Objectives:
To investigate incidence and factors associated with falls in independent ambulatory patients with spinal cord injury (SCI), and to compare levels of ability in those with and without a history of falls.
Setting:
A tertiary rehabilitation center and community hospitals.
Methods:
Seventy-seven independent ambulatory subjects with SCI were interviewed for fall data during 6 months before participation in the study. Subjects were also assessed for their functional ability using the timed up and go test (TUGT) and the 6-min walk test (6MinWT).
Results:
Twenty-six subjects (34%) reported falls during 6 months (range 1–6 times). After falls, two subjects required medical attention due to wrist joint fracture and back pain. Walking without a walking device significantly increased the risk of fall, whereas using a walker significantly reduced the risk of fall (P<0.05). Moreover, faller subjects showed significantly better levels of ability than the non-faller subjects (P<0.005 for the TUGT and P<0.05 for the 6MinWT).
Conclusion:
Approximately one-third of the independent ambulatory subjects with SCI experienced falls. Notably, faller subjects had better functional ability than the non-faller subjects. Thus, apart from emphasizing the ability to walk independently, rehabilitation professionals may need to seek strategies that improve balance and safety.
Similar content being viewed by others
Introduction
Patients with spinal cord injury (SCI) encounter sensorimotor dysfunctions that reduce ability of movement control and subsequently increased risk of falls.1, 2, 3, 4 Previous studies have reported that independent ambulatory patients with SCI encounter a high-risk of falls (74–75%).2, 5 The incidence is clearly higher than that reported in the elderly (33%)6, 7 and patients with other neurological disorders such as stroke (37–73%)8, 9 and Parkinson’s diseases (51–68%).10, 11 After falls, 18% of subjects with SCI reported fracture and 45% had restricted ability to get out into communities and engage in a productive activity.2 Amatachaya et al.5 also found that, among 17 faller subjects, seven of them had bruises, one reported muscular pain and one experienced metatarsal bone fracture that required medical attention and readmission with limitation of weight bearing for 14 days. Subjects in these studies indicated the reduction of balance control and muscle weakness as major factors relating to falls.2, 5
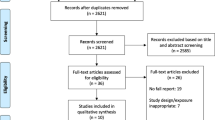
Until now, there is only little evidence on falls in individuals with SCI. Brotherton et al.2 retrospectively surveyed falls in independent ambulatory patients with SCI in 1 year. However, a retrospective design using a long follow-up period and self-reported data may have an increased chance of recall bias.12, 13 In addition, there were a large number of non-responders in which selective attrition/response could affect findings of the study.14 Amatachaya et al.5 prospectively assessed falls over 6 months after discharge. Nonetheless, the study recruited only 23 independent ambulatory subjects with SCI. The factors associated with falls were also subjectively reported by the subjects, which might not reflect actual impairments.5 Therefore, this study further explored incidence and factors associated with falls in independent ambulatory patients with SCI over 6 months before participation in the study. Furthermore, the study compared functional ability between patients with and without a history of falls.
Materials and methods
Subjects
The researchers invited independent ambulatory patients with SCI who visited an outpatient and inpatient department in a tertiary rehabilitation center and community hospitals in Thailand. The inclusion criteria were age at least 18 years, having an SCI from either traumatic or non-traumatic causes, and ability of independent walking with or without a walking device over at least 17 m continuously (functional independent measure locomotor (FIM-L) scores 5–7). The patients were excluded if they had an SCI from progressive diseases, and other medical conditions or complications that might affect/limit mobility, such as pain in the musculoskeletal system with a pain scale more than 5 out of 10 on a visual analog scale, leg length discrepancy, deformities in the joints of extremities, urinary tract infection or pressure ulcer that required bed rest. The eligible subjects needed to provide a written informed consent approved by the local ethics committee before taking part in the study.
Protocols of the study
Subjects were interviewed for their baseline demographics and SCI characteristics, and underwent screening tests to ensure levels and severity of SCI (American Spinal Injury Association Impairment Scale or AIS classification). Subsequently, they were interviewed for fall data during the 6 months before participation in the study using a questionnaire (Supplementary appendix). The questionnaire was developed through consolidation of data from previous studies2, 15 and with the assistance of four experts (two physical therapists, a nurse and a physician) who had good clinical experience in patients with neurological conditions. Then the questionnaire was preliminarily tested in 10 independent ambulatory patients with SCI. Thereafter, some items were deleted, modified or rearranged in order to improve the clarity and completeness of the questionnaire. After revision, the questionnaire contained both closed-end and opened-end questions that were divided into three parts, including baseline demographics, SCI characteristics and fall information (see appendix), and required approximately 20–30 min to complete.
For the objective of this study, a fall was defined as an unplanned, unexpected or unintentional event that resulted in a person coming to rest on the ground, or any other lower or supporting surface during standing, walking or changing posture.2, 5 Data for each fall were verified by asking the date, time, place and consequences of the fall. The findings were further confirmed by their relatives or a care giver.
Furthermore, subjects were assessed for their functional ability using the timed up and go test (TUGT) and the 6-min walk test (6MinWT). The TUGT recorded the time required to accomplish the tasks of standing up from a standard arm chair, walking at a fast and safe pace along a 3-m walkway and returning to sit down on the chair. The 6MinWT measured the longest distance walk in 6 min along a smooth rectangular walkway in order to minimize the effects of turning on the outcomes.16, 17, 18 Results of the test were also used to confirm baseline walking ability (FIM-L scores). In order to minimize the effects of routine treatments on the outcomes, inpatient subjects needed to complete the study within 2–3 days after admission.
Statistical analyses
Descriptive statistics were applied to explain baseline demographics, SCI characteristics and findings of the study. Multiple logistic regression analysis was used to determine factors relating to falls. The independent-samples t-test was utilized to compare the data of the TUGT and 6MinWT between faller and non-faller subjects. Levels of significant differences were set at P<0.05.
Results
Eighty-two independent ambulatory patients with SCI completed the study. However, data for five subjects were excluded because their functional ability data were outliers and extreme. (This refers to the data that were more than 1.5 times of the interquartile range below the first quartile or above the third quartile. The interquartile range is the difference between the third and first quartiles or Q3—Q1. Thus, the data (x) were considered as outliers and extreme, and subsequently excluded if they were less than Q1−(1.5*interquartile range) or more than Q3+(1.5*interquartile range)).19 As a result, the study analyzed data from 77 subjects. Most of these subjects were males at a chronic stage of injury, and had an SCI from non-traumatic causes. Two subjects could walk with a walker independently less than 50 m (FIM-L 5, the longest distance walk=24 and 38 m, respectively), 40 subjects were able to walk independently with a walking device at least 50 m (FIM-L 6, the average longest distance walk in 6 min (mean±s.d.)=110.23±41.60 m (range 82.34–142.13 m)), and the rest of them could walk independently at least 50 m without using any walking device (FIM-L 7, the average longest distance in 6 min (mean±s.d.)=284.68±63.48 m (range 235.82–332.38 m)). Other baseline demographics and SCI characteristics of subjects are given in Tables 1 and 2.
Twenty-six subjects (34%) experienced falls during 6 months before participation in the study (range 1–6 times/subject). Thus, the total number of falls was 55, in which 36 falls occurred while walking, 6 falls happened during standing and the rest occurred while changing posture. The falls happened only in subjects with FIM-L 6 (n=9) and FIM-L 7 (n=17), but not in subjects with FIM-L 5. After falls, two subjects required medical attention due to wrist joint fracture and back pain. The consequences reduced their ability to conduct daily activities and participate in a community. There were no significant differences of age, body mass index and postinjury time between faller and non-faller subjects (P>0.05, Table 1). However, the TUGT and 6MinWT data of the faller subjects significantly differed from those of the non-faller subjects (Table 1). The multiple logistic regression analysis suggested that walking without a walking device significantly increased the risk of fall whereas using a walker significantly decreased the risk of fall (P<0.05, Table 2).
Discussion
This study explored falls and compared functional ability in 77 independent ambulatory SCI subjects with and without a history of falls. The findings showed that 26 subjects (34%) experienced at least one fall during 6 months before taking part in the study (range 1–6 times/subject). Most falls happened during walking. After falls, two subjects suffered from serious medical consequences that affected mobility. Walking without an ambulatory device significantly increased the risk of falls, whereas walking with a walker significantly reduced the risk of fall (P<0.05, Table 2). Findings of the TUGT and the 6MinWT also emphasized that the faller subjects had better levels of functioning than the non-faller subjects (P<0.05, Table 1).
The study applied the TUGT and the 6MinWT to assess the functional ability of the subjects because the previous studies2, 5, 20 indicated that the impairments of balance control and muscle strength were the major causes of falls in subjects with SCI. Apart from standard walking, the TUGT also incorporates functional elements of sit-to-stand and balance control.17 Van Hedel et al.16, 18 suggest that the 6MinWT is one of the best thorough investigations that the results correlate with other walking ability tests, that is, the walking index for SCI II and the 10-m walk test. Results of the test also associate with strength of the hip flexors and abductor muscles, which are the key determinants for walking ability.21 Unexpectedly, the data suggested that subjects with good functional ability (walked without a walking device, required less time to complete the TUGT and achieved longer-distance walk in 6 min) encountered a risk of falls. The findings differed from those reported in elderly and other groups of patients where faller subjects had less functional ability than non-faller subjects.22, 23 A possible explanation for the findings may be that better functional ability may increase the integration of walking into daily activities and be less wheelchair dependence. High ability levels may also accompany greater confidence and less attention to movements. Therefore, these subjects have increased exposure to fall opportunities and have a high risk of falls.
Moreover, the findings indicated that using a walker reduced the risk of falls. Bateni and Maki24 indicate that a walker greatly enlarges the body base of support. Subjects could advance the device during a double support phase, which obviously increased postural stability and therefore decreased the risk of fall of the subjects. However, long-lasting use of a walker poses negative impacts on the patients, such as induced abnormal posture and musculoskeletal pain, requiring high-attention demand and energy expenditure, and increased risk of fall due to limited forward and lateral movements of the legs.24, 25 Thus, the findings may imply that, apart from levels of functioning (ability of independent walking), rehabilitation professionals may need to explore treatment strategies to improve safety issues for patients. For example, instead of training in an empty room without disturbing factors, physical therapists may need to incorporate contextual conditions that the patients may encounter at home and community in order to optimize their balance and subsequently minimize the risk of fall. However, there is a need of evidence to support this assumption.
The findings of this study reflect those of Brotherton et al.,20 who found that using more supportive walking devices, that is, walkers, decreased the risk of fall, whereas walking with a less supportive device, that is, cane, increased the risk of fall. Simpson et al.26 also demonstrated that faller subjects with stroke required significantly less time to complete the TUGT than the non-faller subjects. The different incidence of falls found in this study and the previous reports2, 5, 20 may relate to study design, follow-up period and the sample size. Although the data in this study were retrospectively gathered, the researchers attempted to minimize recall bias by decreasing the time interval to 6 months5 and interviewing for associated data such as time, place and consequences of each fall with confirmation from their relatives or a care giver. The subjects were recruited mainly from a tertiary rehabilitation center that limited the number of sample size. However, this rehabilitation center captures a large number of patients with SCI in the northeast area of Thailand. In order to increase the number of sample size, the researchers recruited both inpatient and outpatient subjects and those from community hospitals. However, admission in a hospital may increase the effects of other confounding factors, that is, regular treatments, on the outcomes. Therefore, inpatient subjects who were eligible as per the inclusion criteria needed to complete the study within 2–3 days after admission.
In addition, there are some other noteworthy limitations of the study. The ability of walking with or without a walking device was classified according to the subjects’ preference in order to represent their usual lifestyle. Nonetheless, using such criteria might influence the findings; for example, subjects might actually need a walking device but they may refuse to use any, which will increase the risk of fall. However, the baseline walking ability (the longest distance walk) may support the classification, that is, subjects who walked without a walking device could walk obviously longer than those who walked with a walking device. Nevertheless, a further study using a prospective design in a larger number of subjects with the information of medical prescription on the use of a walking device is needed to confirm the findings. Moreover, the incorporation of additional measures (for example, Berg Balance Scale) might help to clarify factors relating to falls following SCI.
Data archiving
There were no data to deposit.
References
Amatachaya S, Thaweewannakij T, Adirek-udomrat J, Siritaratiwat W . Factors related to obstacle crossing in independent ambulatory patients with spinal cord injury. J Spinal Cord Med 2010; 33: 144–149.
Brotherton SS, Krause JS, Nietert PJ . Falls in individuals with incomplete spinal cord injury. Spinal Cord 2007; 45: 45–37.
Crozier KS, Graziani V, Ditunno JF, Herbison GJ . Spinal cord injury: prognosis for ambulation based on sensory examination in patients who are initially motor complete. Arch Phys Med Rehabil 1991; 72: 119–121.
van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, Bergen MP et al A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil 2008; 89: 2094–2101.
Amatachaya S, Wannapakhe J, Arrayawichanon P, Siritarathiwat W, Wattanapun P . Functional abilities, incidences of complications and falls of patients with spinal cord injury 6 months after discharge. Spinal Cord 2011; 49: 520–524.
Tood C, Skeltion D . What are the Main Risk Factors for Falls among Older People and What are the Most Effective Interventions to Prevent These Falls, . WHO Regional Office for Europe, 2004.
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J . Prevention of falls and consequent injuries in elderly people. Lancet 2005; 336: 1885–1893.
Forster A, Young J . Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ 1995; 311: 83–86.
Teasell R, McRae M, Foley N, Bhardwaj A . The incidence and consequences of falls in stroke patients during inpatient rehabilitation: factors associated with high risk. Arch Phys Med Rehabil 2002; 83: 329–233.
Bloem BR, Grimbergen YA, Cramer M, Willemsen M, Zwinderman AH . Prospective assessment of falls in Parkinson's disease. J Neurol 2001; 248: 950–958.
Wood BH, Bilclough JA, Bowron A, Walker RW . Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry 2002; 72: 721–725.
Hassan E . Recall bias can be a threat to retrospective and prospective research designs. Internet J Epidemiol 2006; 3: 1–8.
Bradburn NM, Ripa LJ, Shevell SK . Answering autobiographical questions: The impact of memory and inferrence on surveys. Science 1987; 236: 157–161.
Earl RB . The practice of social research. Belmont, CA: : Wadsworth Publishing Company. 2007.
Wannapakhe J . Physical abilities, quality of life, incidences of complications and falls in patients with spinal cord injury after discharge. Master Thesis. Faculty of Associated Medical Sciences, Khon Kaen University: Khon Kaen, Thailand. 2009.
van Hedel HJ, Wirz M, Dietz V . Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil 2005; 86: 190–196.
Read MS, Sisto SA, Ditunno JF . Standardized ambulation assessments following spinal cord injury. Top Spinal Cord Inj Rehabil 2008; 14: 39–60.
van Hedel HJ, Wirz M, Dietz V . Standardized assessment of walking capacity after spinal cord injury: the European network approach. Neurol Res 2008; 30: 61–73.
Jones J Stats: measures of position. 2012 [cited 27 September 2012]; Available from http://people.richland.edu/james/lecture/m170/ch03-pos.html.
Brotherton SS, Krause JS, Nietert PJ . A pilot study of factors associated with fall in individuals with incomplete spinal cord injury. J Spinal Cord Med 2007; 30: 243–250.
Kim CM, Eng JJ, Whittaker MW . Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord 2004; 42: 156–162.
Shumway-Cook A, Brauer S, Woollacott M . Predicting the probability for falls in community-dwelling older adults using the timed up & go test. J Am Phys Ther Assoc 2000; 80: 896–903.
Dibble LE, Lange M . Predicting falls in individuals with parkinson disease: a reconsideration of clinical balance measures. J Neurol Phys Ther 2006; 30: 60–67.
Bateni H, Maki BE . Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil 2005; 86: 134–145.
Koh ES, Williams AJ, Povlsen B . Upper-limb pain in long-term poliomyelitis. QJM 2002; 95: 389–395.
Simpson LA, Miller WC, Eng JJ . Effect of stroke on fall rate, location and predictors: a prospective comparison of older adults with and without stroke. PLoS One 2011; 6: 1–6.
Acknowledgements
This study was supported by funding from the Faculty of Associated Medical Sciences, and the Improvement of Physical Performance and Quality of Life (IPQ) research group, Khon Kaen University, Khon Kaen, Thailand. The researchers would like to thank Mr Ian Thomas for his help in manuscript preparation. This study was presented in part at the 1st Singapore Rehabilitation Conference, 10–11 February 2012, Singapore.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
Phonthee, S., Saengsuwan, J. & Amatachaya, S. Falls in independent ambulatory patients with spinal cord injury: incidence, associated factors and levels of ability. Spinal Cord 51, 365–368 (2013). https://doi.org/10.1038/sc.2012.147
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.147
Keywords
This article is cited by
-
Feasibility and tolerance of a robotic postural training to improve standing in a person with ambulatory spinal cord injury
Spinal Cord Series and Cases (2021)
-
The association between participation and quality of life indicators with hospitalizations in ambulatory adults with spinal cord injury
Spinal Cord (2020)
-
Falls after spinal cord injury: a systematic review and meta-analysis of incidence proportion and contributing factors
Spinal Cord (2019)
-
Do clinical balance measures have the ability to predict falls among ambulatory individuals with spinal cord injury? A systematic review and meta-analysis
Spinal Cord (2019)
-
Various surfaces challenge gait characteristics of ambulatory patients with spinal cord injury
Spinal Cord (2019)