Abstract
Inhibition of the protein kinase mechanistic target of rapamycin (mTOR) with the Food and Drug Administration (FDA)-approved therapeutic rapamycin promotes health and longevity in diverse model organisms. More recently, specific inhibition of mTORC1 to treat aging-related conditions has become the goal of basic and translational scientists, clinicians and biotechnology companies. Here, we review the effects of rapamycin on the longevity and survival of both wild-type mice and mouse models of human diseases. We discuss recent clinical trials that have explored whether existing mTOR inhibitors can safely prevent, delay or treat multiple diseases of aging. Finally, we discuss how new molecules may provide routes to the safer and more selective inhibition of mTOR complex 1 (mTORC1) in the decade ahead. We conclude by discussing what work remains to be done and the questions that will need to be addressed to make mTOR inhibitors part of the standard of care for diseases of aging.
Similar content being viewed by others
Main
mTOR is an evolutionarily conserved serine–threonine protein kinase found in diverse species including mice and humans. The mTOR kinase forms the catalytic core of two distinct protein complexes, mTORC1 and mTORC2, each of which are composed of shared as well as unique protein subunits and phosphorylate different substrates. mTORC1 is regulated by a wide range of nutrients and hormonal cues, most notably by the availability of amino acids, but also glucose, oxygen and cholesterol1,2,3. mTORC1 activity drives a wide variety of anabolic processes through phosphorylation of substrates including ribosomal protein S6 kinase (S6K) β1 (S6K1) and eukaryotic translation-initiation factor 4E-binding proteins (4E-BPs). mTORC1 activity also inhibits autophagy via phosphorylation of substrates including Unc-51-like autophagy-activating kinase (ULK1)4. In contrast to mTORC1, which is responsive to many different environmental cues, mTORC2 primarily acts as an effector of phosphoinositide 3-kinase (PI3K) signaling by tuning the activity of substrates including the kinase AKT, serum–glucocorticoid-regulated kinase (SGK) and protein kinase Cα (PKCα).
Beginning 20 years ago, researchers discovered a role for mTORC1 signaling in the aging process. Studies in yeast, worms and flies found that genetic inhibition of mTORC1 or signaling pathways downstream of mTORC1, including S6K and translation-initiation factors, extends lifespan5,6,7,8,9,10,11. mTORC1 signaling was also observed to be lower in long-lived Ames dwarf mice than in wild-type controls12. Studies in mice have likewise shown that genetic depletion of mTORC1 subunits, deletion of S6K1 (also known as Rps6kb1) or downstream substrates or expression of dominant negative 4E-BP1 in specific tissues extends the lifespan and healthspan of mice13,14,15,16. Even partial inhibition of mTORC1 in genetic mouse models (for example, S6K1−/−, Mtor+/−, Mlst8+/−, MtorΔ/Δ and Tsc1tg) can extend lifespan and healthspan in mice13,17,18,19.
These results quite logically spurred substantial interest in the possibility that a potent chemical inhibitor of mTORC1, rapamycin, could extend lifespan. This was indeed the case, and there are now numerous studies showing that rapamycin can extend the lifespan not only of model organisms including yeast, worms and flies20,21,22 but also, as we detail below, of both wild-type mice and in many disease models. In this Review, we will discuss the results of these studies, as well as the possible mechanism by which reduced mTORC1 signaling via both dietary and pharmacological means may improve healthspan23,24,25.
Many of the side effects of rapamycin, which include immunosuppression, hyperlipidemia and hyperglycemia, have raised concerns about the feasibility of using rapamycin to promote healthy longevity in humans and have slowed clinical evaluation of mTOR inhibitors for diseases of aging26. In this Review, we will discuss data generated over the past decade suggesting that the beneficial effects of rapamycin on healthspan and lifespan are mediated by inhibition of mTORC1, whereas the negative effects of rapamycin on glucose and lipid metabolism are mediated by inhibition of mTORC2.
Importantly, these data predict that interventions that more selectively target mTORC1, by limiting the amount of mTOR inhibitor used and the time of the exposure, will have reduced side effects as compared to chronic treatment. Here we discuss preclinical animal data and clinical human data exploring the use of intermittent and low-dose mTOR-inhibitor-treatment regimens, the results of which suggest that rapamycin analogs (rapalogs) and other mTOR inhibitors may be able to be dosed in a way that is safer as well as geroprotective. Finally, we discuss future studies and the quest for mTORC1-selective molecules derived in part through recent discoveries about the molecular machinery through which mTORC1 senses nutrients and hormonal cues.
Extension of lifespan with the mTOR inhibitor rapamycin in mice
Rapamycin is a macrolide first discovered in soil from Easter Island almost 50 years ago27. Rapamycin is an acute inhibitor of mTORC1 but not of mTORC2 (ref. 28). The reason for this difference in rapamycin sensitivity is structural; the mTOR-interacting protein RICTOR, which is present in mTORC2 but not in mTORC1, masks the rapamycin-interacting domain of mTOR29,30,31. Although mTORC2 is not acutely inhibited by rapamycin, subsequent studies have shown that mTORC2 is inhibited in cell culture as well as in vivo in mice when exposed to high concentrations of rapamycin for a prolonged period of time, most probably due to the sequestration of free mTOR by rapamycin so that it is unavailable for incorporation into mTORC2 (refs. 17,32). Rapamycin and rapalogs inhibit T cell activation and are approved to prevent organ transplant rejection. In addition, rapalogs inhibit tumor cell growth and are approved for the treatment of a subset of tumors. Finally, rapalogs are approved for the treatment of specific genetic disorders that result in hyperactive mTOR signaling.
Multiple groups have studied the effect of rapamycin on the longevity of mice, starting with a landmark study by the National Institute on Aging Interventions Testing Program (NIA ITP) published in 2009, which demonstrated that rapamycin extended the lifespan of genetically heterogeneous mice33. Since that time, additional studies of rapamycin on mouse lifespan have been conducted not only by the NIA ITP but by at least ten other groups across the globe (Table 1). A number of lessons can be drawn from this set of studies, primarily that rapamycin is an extraordinarily robust geroprotective intervention, extending lifespan in multiple wild-type mouse strains handled by multiple teams and including inbred, outbred and genetically heterogeneous male and female mice. Every study observed an extension of lifespan in one or more dosing groups, with females typically benefiting more than males at equivalent doses of rapamycin. Importantly, unlike caloric restriction, another well-validated longevity intervention, which is less efficacious when begun later in life34, rapamycin robustly extended lifespan when dosing was not initiated until late in life when the mice were 20 months of age (equivalent to about a 60-year-old human)33,35. Dosing regimens for rapamycin are very flexible, and beneficial effects of rapamycin on longevity are observed even when rapamycin is dosed intermittently, when it is given for only a short period of time immediately postnatally or when it is administered to older mice already past middle age36,37,38,39,40,41,42,43. Finally, rapamycin may be effective when combined with other geroprotectors, including metformin and acarbose44,45.
Rapamycin has also been tested in a wide number of disease models, including multiple different cancers, mitochondrial disease and progeria (Table 2). Here, the beneficial effects of rapamycin have been more varied than in wild-type mice. As might be expected, rapamycin has shown significant benefits in mouse models of mTORopathies46, diseases resulting from genetic activation of mTOR, including tuberous sclerosis complex (TSC) and some epilepsies. Rapamycin also has substantial positive effects on the survival of mouse cancer models. Finally, rapamycin extends the lifespan of several progeroid mouse models quite effectively, suggesting that progeria mouse models, while not perfect models of aging, may have utility for rapidly assessing the potential benefits of geroprotectors.
While by far the most work on rapamycin and aging has been done in mice, there is substantial interest in exploring the use of rapamycin in primates. A total of 66 middle-aged marmosets (Callithrix jacchus) have been fed either rapamycin- or vehicle-containing diets, with the lifespan and healthspan of the animals followed longitudinally. Both sexes are being examined in this study, which is still underway. A limitation of these studies is both the relatively small number of animals studied (less than 20 per sex and treatment) and the range of ages and the genetic heterogeneity of the population. Initial studies suggested that rapamycin, dosed at ~1 mg per kg of body weight via the diet, was well tolerated, with only minor effects of rapamycin on hematological parameters and no statistically significant changes in blood glucose, cholesterol or triglyceride levels47. In the subset of six animals treated with rapamycin or vehicle for 9 months, two rapamycin-treated animals showed an increase in fasting blood glucose and two rapamycin-treated animals showed an increase in triglycerides, suggesting the possibility of some inhibition of TORC2 at this dose level47. However, a definitive examination of the metabolic impact of rapamycin in marmosets will require studies in a larger number of animals, conducted over a longer period of time.
The second major study of rapamycin done outside of the rodent context is examining the effect of rapamycin on the aging of dogs. As companion animals, dogs share the human environment, receive regular medical care similar to humans and develop many of the same age-related diseases that humans do. Furthermore, many dog owners have shown interest in enrolling their dogs in studies to promote healthy aging. The short lifespan of dogs, particularly that of large dog breeds, allows for studies of shorter duration than for humans. A small pilot study found that treatment with 0.05 mg per kg or 0.1 mg per kg rapamycin three times per week did not cause statistically significant side effects but did improve measurements of cardiac function (fractional shortening and diastolic function)48. A larger study in which middle-aged, large-breed dogs will be treated with rapamycin or vehicle for 1 year will complete enrollment during 2023 (ref. 49).
Mechanisms underlying the effects of rapamycin on healthspan and lifespan
There are many possible mechanisms underlying the geroprotective effects of rapamycin. In this section, we will discuss the effects of mTORC1 inhibition on both specific disease processes and the molecular mechanisms that may contribute to the beneficial effects of rapamycin on lifespan and healthspan.
Protein translation
mTORC1, via S6K1 and 4E-BPs, has a central role in the regulation of translation, and defects in translation have long been theorized to contribute to aging. The error catastrophe theory suggests that errors in protein translation could lead to increasingly inaccurate protein synthesis and functional decline50. Conceptually, slowing protein translation by treatment with rapamycin might allow mRNA to be translated into protein with higher fidelity or to fold more accurately. In agreement with such a model, experiments in model organisms have shown that deletion or knockdown of genes encoding ribosomal subunits, S6K1 or translation-initiation factors results in increased lifespan6,10.
However, modern measurement techniques have not found evidence that protein translation errors increase with age51. Furthermore, neither mTOR inhibition by rapamycin nor deletion of S6K1 significantly slows protein translation in mice or cells52,53,54. Studies in Caenorhabditis elegans have shown that the lifespan of worms lacking eukaryotic translation-initiation factor 4E (eIF4E), which are long lived and have a global reduction in protein synthesis, can be still further increased by knockdown of the gene encoding TOR10. These results strongly suggest that rapamycin does not regulate longevity solely by downregulating protein translation.
There may be a more subtle effect of rapamycin on protein translation, namely, that rapamycin may alter the translation of specific mRNA species. Both rapamycin and complete mTOR inhibition preferentially inhibit translation of mRNA with 5′ terminal oligopyrimidine motifs, suggesting a potential role for these genes in longevity55,56. In yeast, the deletion of genes encoding ribosomal subunits can extend lifespan; this is partially dependent upon inducing translation of the mRNA encoding the transcription factor general control nondepressible 4 (Gcn4)57. Expression of the Gcn4 protein is limited by multiple upstream open reading frames that normally sequester ribosomes that bind to the mRNA. Under conditions of large ribosomal subunit abundance, the upstream open reading frames are more frequently bypassed to initiate translation of GCN4. It is not clear whether this system is conserved in mammals because, in mammals, mTORC1 inhibition decreases translation of the mammalian homolog of Gcn4, ATF4 (refs. 58,59). ATF4 instead may act as a brake on mTORC1 in response to mitochondrial distress, with ATF4 inhibiting mTORC1 activity by upregulating the mTORC1 inhibitors sestrin 2 and REDD1 (ref. 60). Despite these differences, it is possible that changes in translation of specific mRNA species may contribute to the beneficial effects of rapamycin on healthspan and lifespan.
One potential example of this is that mice expressing a constitutively active (dephosphorylated) form of 4E-BP1 in skeletal muscle are protected from age- and diet-induced declines in insulin sensitivity and metabolic rate15. These effects may be mediated in a non-cell-autonomous manner via increased production of fibroblast growth factor 21 (FGF21) by skeletal muscle, activating brown adipose tissue. Interestingly, whole-body overexpression of 4E-BP1 also has positive effects on healthspan, protecting male mice from diet-induced obesity16. These mice also have increased levels of FGF21, in this case due to upregulation of hepatic Fgf21 expression. Notably, expression of Fgf21 is regulated in part by ATF4 (refs. 61,62). A recently described downstream effector of mTORC1 and S6K1 is glutamyl-prolyl tRNA synthetase (EPRS), which is phosphorylated by S6K1 (ref. 14). When phosphorylated, EPRS functions to inhibit the translation of select mRNA species by forming an interferon γ (IFNγ)-activated inhibitor of translation (GAIT) complex, which selectively inhibits mRNA containing GAIT elements63. Mice expressing EPRSS999A, which cannot be phosphorylated, have reduced body weight and adipose mass and increased lifespan, similar to mice lacking S6K1 (ref. 14). Other aminoacyl-tRNA synthetases may similarly have non-canonical functions64 that may play a part in the response to rapamycin.
Autophagy
Autophagy is a process by which cells recycle their proteins and organelles, which not only allows cells to survive nutrient-limited conditions but is also a central mechanism by which damaged protein and subcellular organelles are removed. While autophagy thus seems to be very important from this description alone, studies in yeast, worms and flies have shown that inactivation of autophagy shortens lifespan, while promotion of autophagy extends lifespan65,66,67. Importantly, autophagy has also been shown to be required for the extension of lifespan by reduced mTOR signaling in both yeast and worms65,68. In mammals, autophagy is reportedly upregulated in calorie-restricted mice and in the cells of long-lived Snell dwarf mice and is required for some of the beneficial effects of a calorie-restricted diet on the heart, kidney and liver69,70,71,72.
When nutrients are abundant, mTORC1 activity acts as a brake on autophagy by phosphorylating the autophagy-initiating kinase ULK1 and autophagy-related protein 13 (ATG13) as well as other components downstream of autophagy initiation and is reviewed in detail elsewhere73,74,75. Conversely, when nutrients are low, autophagy is active as a result of AMP-activated protein kinase (AMPK) activation and reduced mTORC1 activity. Autophagy is normally impaired with age in multiple types of mouse cells, and genetic activation of autophagy in the aged mouse liver rejuvenates the liver histologically and improves function76,77,78. While rapamycin itself is not a strong inducer of autophagy compared to mTOR kinase inhibitors53, the effects of rapamycin on the pathology of mouse models of Alzheimer’s disease have been attributed in part to increased autophagy79,80.
Improvement in immune function
Premature aging of the immune system has been shown to drive aging of multiple other organ systems in mice81. These findings suggest that therapies that improve immune aging may have more systemic healthspan and lifespan benefits. mTOR inhibition has been shown to improve the function of the aging immune system in both mice and humans. Specifically, a short 6-week course of rapamycin has been shown to rejuvenate the function of hematopoietic stem cells (HSCs), increase production of naive lymphocytes and improve the response to influenza vaccination in old mice39. Of interest, rapamycin treatment extended lifespan in this study even though it was only administered for 6 weeks when mice were already old (26 months). In older humans, 6 weeks of mTOR-inhibitor treatment (a rapalog alone or in combination with a catalytic site mTOR inhibitor) also improved the response to influenza vaccination and was associated with a decrease in the percentage of exhausted PD-1+ T cells in peripheral blood82,83. In addition, mTOR inhibition has been shown to upregulate antiviral immunity in older adults83,84. These clinical studies will be discussed in more detail below.
However, it is worth noting that rapamycin is approved by the FDA as an immunosuppressant, and infections are common, particularly in humans taking high doses of rapalogs for a long period of time. In mice, rapamycin has been shown to be immunomodulatory, improving CD8+ T cell immunological memory while at the same time impairing defenses against acute viral and bacterial infections85. A recent meta-analysis suggests that mice treated with rapamycin have increased survival following an acute pathogenic challenge86. Thus, there may be tradeoffs, with rapalogs improving some aspects of immune function while impairing others.
Cancer
Cancer is the most common cause of death for laboratory mice, and rapamycin and its derivatives (rapalogs) inhibit the proliferation of cancer cell lines. Rapalogs are approved for use in certain oncology indications, and, as shown in Table 2, rapamycin is very effective at extending the lifespan of mouse models of cancer. A study by Neff and colleagues found that rapamycin significantly reduced the proportion of 16-month-old mice with cancer and/or precancerous lesions87 and suggested that this indicated that the effects of rapamycin on lifespan were driven by its anti-cancer effects. This effect on cancerous and precancerous lesions was not observed in animals killed at 25 months of age, although the interpretation of these results was confounded by the fact that cancer was not assessed in animals that died of natural causes. By contrast, the NIA ITP has shown that the overall prevalence of cancer at death, as well as the spectrum of cancers observed, was very similar between rapamycin-treated mice and controls36. While cancer prevention clearly has a role in the benefits of rapamycin in mice, cancer is itself an age-related disease, and thus prevention of cancer is an expected consequence of geroprotective therapies.
Cancer cells often express pluripotency markers, and rapamycin reduces cell size and proliferation and enhances the differentiation of mouse and human embryonic stem cells88,89,90. Rapamycin may be particularly beneficial against cancer stem cells and has been shown to deplete leukemia-initiating cells and inhibit both self-renewal and differentiation of stem cells derived from infantile hemangioma91,92. Rapamycin inhibits cell proliferation, the epithelial–mesenchymal transition and cancer stem cell characteristics of lung cancer stem cells and colorectal cancer stem cells93,94.
Stem cells
In contrast to its actions on cancer stems cells, rapamycin has been shown to have beneficial effects on self-renewal and function in normal stem cells, which may contribute to the benefits of rapamycin on tissue function. Several studies have been conducted on HSCs; aged mice have elevated mTORC1 activity in their HSCs as well as functional deficits similar to those observed in a mouse model of hyperactive mTORC1 activity39. Treatment of aged mice with rapamycin restored the functional capacity of their HSCs and boosted the immune response to influenza virus. In a separate study, rapamycin was shown to restore self-renewal capacity to a subpopulation of mouse HSCs with spontaneously high oxidative stress and reduced functional capacity95. Rapamycin also increases the self-renewal capacity of mouse intestinal stem cells via a non-cell-autonomous mechanism mediated by inhibition of mTORC1 in the adjacent Paneth cells96.
Reduction of hyperactive mTOR in aging tissues
One reason that mTOR inhibition may have health benefits in older organisms is because mTOR activity may become inappropriately high with age. Higher mTORC1–S6K activity in muscle of older mice, rats and humans is associated with sarcopenia97,98,99,100,101 and, in the brain, is associated with Alzheimer’s disease101,102,103,104,105. Altered mTORC1 signaling with age has also been reported in other tissues of mice, with most studies reporting increased mTORC1 activity with age39,97,106,107,108. The ability of rapamycin to promote longevity is consistent with the idea that mTOR activity is an example of antagonistic pleiotropy, with high mTOR signaling being beneficial for development and reproduction but harmful during a post-reproductive old age109. Under such a model, the benefits of mTOR inhibition may arise less from specific benefits on processes such as translation and more from avoiding negative effects of hyperactive mTOR on processes such as cellular senescence. Indeed, rapamycin has been shown to inhibit the accumulation of senescent cells in mice as well as to suppress the senescence-associated secretory phenotype110.
Inhibition of mTORC2
In sharp contrast to mTORC1, inhibition of mTORC2 has mostly negative effects on lifespan. In worms, mTORC2 inhibition has most often been associated with reduced lifespan, while, in flies, increasing mTORC2 activity through overexpression of rictor extends lifespan21,111,112,113. Whole-body deficiency of mTORC2 signaling or tissue-specific inhibition of mTORC2 signaling in the brain, liver or adipose tissue reduces lifespan in C57BL/6J mice114,115,116,117. Conversely, the lifespan of male mice is extended by acarbose and 17α estradiol, and these compounds increased hepatic mTORC2 activity118. mTORC2 activity is also elevated in long-lived Snell dwarf mice and Ghr−/− mice119.
Inhibition of mTORC2 also results in negative effects on metabolism and immunity. Genetic inhibition of mTORC2 in one or more tissues of a mouse can result in frailty, hyperphagia, insulin resistance, hyperlipidemia, hypercholesterolemia, hyperglycemia, kyphosis and/or obesity depending upon the specific tissues in which mTORC2 is inhibited68,114,115,116,117. Specific inhibition of mTORC1 in mice using an mTORC1-specific inhibitor did not result in hyperglycemia, impaired glucose tolerance, hyperlipidemia or hypercholesterolemia, again demonstrating that these negative effects are mediated at least in part by inhibition of mTORC2 (ref. 120). Finally, mTORC2 has been shown in a number of studies to have a key role in immunity and wound repair121,122,123,124,125,126,127, and, in accordance with this important role for mTORC2, compounds that selectively inhibit mTORC1 have a reduced effect on the immune system compared to rapamycin120. Thus, lower or intermittent doses of rapamycin or treatment with rapalogs that more specifically target mTORC1 are predicted to reduce mTORC2-associated side effects such as hyperlipidemia and hyperglycemia without impairing the lifespan-extending benefits of mTORC1 inhibition.
This is not to say that there may not be benefits of inhibiting mTORC2 in specific settings. Inhibition of mTORC2 signaling extends the lifespan of C. elegans under certain temperatures and dietary conditions111,112, has anti-tumor effects128,129,130,131, is beneficial in mouse models of mitochondrial disease132,133 and has been shown to inhibit or reverse senescence in human cells134,135. Certain side effects, whether mediated by mTORC1 or mTORC2, may potentially even be a consequence of ‘on-target’ action of rapamycin and rapalogs, and avoiding these side effects may limit the benefits of such drugs for healthy aging. However, given the balance of the evidence, particularly the genetic studies showing that mTORC2 activity is associated with lifespan and that inhibition of mTORC1 alone can extend lifespan, we believe that inhibition of mTORC2 is ‘off-target’ with respect to the beneficial effects of rapamycin and rapalogs on healthspan and longevity.
Clinical trials of mTOR inhibitors for diseases of aging
Given the extensive preclinical data confirming that mTOR inhibition extends lifespan and healthspan, there is great interest in determining whether mTOR inhibitors will have benefits for human aging. As highlighted in Fig. 1, based on mouse studies, rapamycin and rapalogs may have benefits in many different systems, including the brain, the heart, the immune system, the intestine, the liver, senescent skin cells, skeletal muscle and tendons. Rapalogs are approved for use in patients with transplantation and patients with cancer at high doses that strongly suppress mTORC1 activity136 and have substantial side effects including mouth ulcers similar to canker sores, gastrointestinal side effects, hyperlipidemia and hyperglycemia and impaired wound healing. The approved doses of rapalogs also inhibit immune function, and therefore the FDA approved prescribing information notes that taking rapalogs may increase the risk of infection and certain cancers associated with immunosuppression137,138. The risk of infectious diseases associated with higher doses of rapalogs in humans may not be adequately modeled in preclinical mouse experiments, as mice are usually housed in specific pathogen-free barrier facilities.
Based on studies in rodents and humans, rapamycin and rapalogs may have potential benefits for ameliorating or slowing age-related conditions associated with the brain105,245,246,247, the heart25,248,249, the liver25, skeletal muscle100, tendons25,250, the immune system39,82,83,84, the skin135 and the intestine96,251. Me, methyl.
Chronic treatment of humans with high doses of rapalogs is also associated with deleterious metabolic consequences including hyperlipidemia, hypercholesterolemia, hypertriglyceridemia, insulin resistance and glucose intolerance139,140,141,142,143. Hyperlipidemia and hyperglycemia have also been observed in rodents treated with rapamycin or rapalogs, although mice are less susceptible to developing hyperlipidemia-induced cardiovascular disease than humans. Trelinska and colleagues observed hyperlipidemia in 66% of patients with TSC taking high daily doses of everolimus for 15 months; hyperglycemia was observed in 22% of participants139. Another side effect of rapamycin at doses that extend lifespan in mice is testicular degeneration25,144, and reduced male fertility has been observed in humans treated with rapalogs145,146. Finally, rapamycin at lifespan-extending doses in mice also promotes the formation of cataracts25, although cataracts have not been associated with rapalog treatment in humans.
Recent studies have explored the safety and efficacy of lower or intermittent dosing regimens of mTOR inhibitors in older adults. Preliminary results from these studies suggest that lower or intermittent dosing regimens of mTOR inhibitors that turn down mTOR activity to ‘younger’ levels rather than turn off mTOR activity have the potential to safely improve the function of aging organ systems or ameliorate aging-related diseases in humans. Of interest, clinical trials to date suggest that low or intermittent doses of mTOR inhibitors enhance rather than suppress immune function and decrease infection risk in older adults. Table 3 summarizes the clinical trials published to date of mTOR inhibitors for aging-related conditions; we discuss each of these briefly below.
mTOR inhibition and the immune system
The largest clinical trials to date have investigated whether mTOR inhibition can improve the function of the aging immune system. The first clinical trial was done with 218 adults aged ≥65 years without unstable medical conditions to determine whether the rapalog everolimus improved the function of the aging immune system as assessed by response to influenza vaccination82. The rationale for the trial was a preclinical study demonstrating that 6 weeks of rapamycin treatment improved the immune response of old mice to influenza vaccination39.
Safety was a key concern when designing this trial. Therefore, very low daily or intermittent doses of everolimus were used in the vaccination trial (1/6th–1/20th lower than the approved doses for patients with transplantation and oncological conditions) that were predicted to minimize adverse events and to lower rather than completely inhibit mTORC1 activity. The clinical trial demonstrated that 6 weeks of treatment with everolimus at either 0.5 mg once daily or 5 mg once weekly was well tolerated and significantly improved the response of older adults to influenza vaccination. Immunophenotyping revealed that everolimus at low or intermittent doses decreased the percentage of PD-1+ exhausted T cells in the peripheral blood of older adults, and this may have been a mechanism underlying their improved immune function. This was the first study to demonstrate that mTOR inhibition may improve the function of an aging organ system in humans82.
A subsequent clinical trial was done with 264 adults aged ≥65 years to extend these findings and determine whether low-dose mTOR-inhibitor treatment with either everolimus and/or or the catalytic site mTOR inhibitor BEZ235 improved the function of the aging immune system sufficiently to improve not only influenza vaccination response but also to decrease total infection rates in older adults83. The study confirmed that 6 weeks of treatment with mTOR inhibitors at a low dose was safe and was associated with a dose-dependent significant improvement in influenza vaccination response. In addition, low-dose mTOR-inhibitor treatment significantly decreased the rate of infections, the majority of which were respiratory tract infections (RTIs). Exploratory transcriptional profiling found that the older adults receiving mTOR inhibitors at low doses had significant upregulation of genes in type 1 interferon-induced antiviral pathways. This upregulation of antiviral gene expression may underlie the reduction in RTIs observed in older adults treated with mTOR inhibitors, as most RTIs are viral in origin147,148.
Large follow-up phase 2b (n = 652) and phase 3 (n = 1,051) trials were done to confirm whether 16 weeks of treatment with mTOR inhibitor at a low dose upregulated antiviral immunity and decreased the incidence of viral RTIs in older adults84. Low doses of the mTOR inhibitor BEZ235 were observed to be well tolerated and to decrease the incidence of laboratory-confirmed RTIs (the phase 2b primary endpoint; odds ratio, 0.601 (90% confidence interval CI: 0.39, 0.92); P value, 0.025) but not the incidence of clinically symptomatic respiratory illness, which was defined as symptoms consistent with an RTI irrespective of whether an infection was laboratory confirmed (the phase 3 primary endpoint; odds ratio, 1.07 (90% confidence interval: 0.80, 1.42); P value, 0.65). In both trials, significantly more interferon-induced antiviral genes were upregulated in individuals treated with BEZ235 than in those treated with the placebo. Lessons learned from the combined phase 2b and 3 trial results suggest that upregulation of antiviral immunity by low-dose mTOR-inhibitor therapy may have a greater impact on (1) severity than incidence of viral RTIs, (2) RTIs caused by coronaviruses, rhinoviruses and influenza viruses as opposed to other respiratory viruses, and (3) the incidence and severity of viral RTIs in older adults ≥75 years of age as opposed to those 65–74 years of age. Based on these findings, it will be important to determine in future clinical trials whether mTOR inhibitors decrease the severity of specific viral RTIs in people ≥75 years of age.
Rapamycin in older adults
In contrast to the participants in the above trials, who tolerated everolimus or BEZ235 quite well, a small, 8-week long randomized clinical trial of 25 older adults between 70 and 95 years of age treated with rapamycin at 1 mg per day experienced more side effects than those treated with placebo, including a small increase in glycated hemoglobin (A1C) (within-group P = 0.03) and a 40% increase in triglyceride levels (within-group P = 0.05)149. While these results tend to align with our expectation that chronic rapamycin treatment may cause hyperglycemia and hyperlipidemia, a caution in interpreting these results is the small group size and the failure of the between-group comparisons to reach statistical significance (P = 0.07 and 0.12 for A1C and triglyceride changes, respectively). In addition, other parameters of glucose metabolism including insulin sensitivity and pancreatic beta cell function were not affected. It is possible that lower doses of rapamycin, intermittent treatment with rapamycin or treatment with everolimus would be better tolerated than the daily dose of 1 mg per day examined here, but this has not been directly tested.
Rapamycin in skin
Local administration of rapamycin with negligible systemic exposure poses fewer safety risks than systemic administration. In a randomized placebo-controlled study of participants aged ≥40 years with signs of skin aging, 36 participants topically applied cream containing rapamycin (10 µM) to one hand and a matching placebo cream to their other hand for 8 months135. A total of 17 participants completed the study, 13 participants had skin biopsies, and eight participants had sufficient biopsy material for analysis of p16 expression levels, the primary endpoint of the study. Rapamycin-treated as compared to placebo-treated participants were observed to have a significant decrease in senescent cells as assessed by p16 expression, increased collagen VII protein expression and clinical and histologically assessed improvements in skin appearance. Treated participants did not have detectable levels of rapamycin in their blood, and there were no treatment-related adverse events.
Forthcoming clinical trials
A number of small clinical trials focused on geroprotective outcomes have been proposed in the USA, the UK and New Zealand over the past 2 years, and many have obtained funding and/or began enrolling participants. While the details of each study differ, most are testing low or intermittent doses of rapamycin or everolimus in participants over the age of 50 years in the range of 0.5–1 mg per day to 5–6 mg per week. These studies are testing a range of outcomes for a range of age-related diseases, including Alzheimer’s disease, diabetes and sarcopenia; primary outcomes include disease-specific outcomes, including effects on cognitive performance, changes in insulin sensitivity and changes in physical performance. Secondary outcomes for most planned studies include biomarkers of aging, including analysis of the DNA-methylation clock; most studies are also assessing safety-related endpoints, including infections and metabolic disruption. A weakness of these planned studies is that even the largest will be studying a maximum of only 150 participants, and the longest planned study is 18 months. Thus, while these studies are critical to gather data on the safety and effectiveness of these compounds as geroprotectors in humans and interesting new data will probably become available over the next few years, comprehensive follow-up with well-powered double-blind placebo-controlled randomized clinical trials will still be necessary.
New ways to inhibit mTORC1
Given the drawbacks of rapamycin and commercially available rapalogs, most notably, the side effects and the narrowness of any potential therapeutic window, there is intense interest in identifying new ways to selectively inhibit mTORC1. In the short term, some dietary interventions have shown potential promise. In particular, because mTORC1 activity is regulated by amino acids, while mTORC2 activity is not, reducing the content of dietary protein or specific dietary amino acids that normally stimulate mTORC1 activity has been explored as a way to promote healthy aging. Several studies have shown that restriction of protein or specific restriction of either methionine or one or more of the branched-chain amino acids (leucine, isoleucine and valine) reduces mTORC1 activity and extends lifespan in preclinical species24,150,151,152. Intriguingly, low blood levels of isoleucine are also associated with reduced mortality in humans153. Other potentially mTORC1-lowering diets include a ketogenic diet, which has been shown to extend the lifespan of mice while reducing mTORC1 activity154.
Of course, any dietary intervention will have issues with adherence, and pharmaceutical interventions can take mTOR inhibition to a much broader swath of the population. High-resolution structures of mTORC1 have provided a previously unprecedented look at how mTORC1 is activated by nutrients and how it is inhibited by rapamycin155,156,157. High-resolution structures have also been generated of the complexes that regulate mTORC1 activity, including the TSC complex158, Rag GTPases in complex with mTORC1 and Ragulator159,160,161 and the binding of leucine by sestrin 2 (ref. 162). As discussed below, this has led to potential new approaches and the development of new molecules to target mTORC1 selectively.
mTORC1 is able to phosphorylate its substrates only after allosteric interaction with Ras homolog enriched in brain (RHEB)–GTP, which activates mTORC1 by promoting the alignment of kinase-site residues163,164. To bring mTORC1 and RHEB–GTP together, two signaling pathways converge at the surface of the lysosome. The first of these pathways brings mTORC1 to the lysosomal surface, while a second pathway controls the GTP–GDP binding status of RHEB. The recruitment of mTORC1 to the lysosomal surface has been studied for over a decade and has been reviewed in detail elsewhere3; we have outlined the major regulator mechanisms in Fig. 2. In brief, mTORC1 is recruited to the lysosome by interacting with heterodimeric pairs of the Rag family of small GTPases165,166. In the presence of amino acids, RagA or RagB binds GTP and RagC or RagD binds GDP (for example, RagAGTP–RagCGDP), permitting the Rag proteins to interact with mTORC1 and localize it to the lysosome. The nucleotide-binding status of Rag GTPases is controlled by several different protein complexes with guanine nucleotide exchange factor (GEF) or GTPase-activating protein (GAP) activity for Rag GTPases.
Negative regulators (CASTOR1, GATOR1, SAMTOR, sestrin 2, TSC) and positive regulators (FLCN–FNIP2, GATOR2, KICKSTOR, LRS, Rag GTPases, Ragulator, RHEB, SLC38A9, vacuolar-type ATPase (V-ATPase)) are shown. Potential mechanisms for the development of mTORC1-specific inhibitors include: identifying small molecules that block the ability of amino acid sensors upstream of mTORC1 to sense the availability of leucine, arginine or SAM (a–d); developing compounds such as BC-LI-0186 that inhibit the GAP or GEF activities of FLCN–FNIP2, LRS, Ragulator or TARS2 (e–g); inhibiting the interaction of mTORC1 and RHEB, the mechanism of action of NR1 (h); identifying small molecules that block the ability of LYCHOS and SLC38A9 to sense the availability of cholesterol (i); and identifying rapamycin derivatives such as DL001 that specifically inhibit mTORC1 (j). TNF, tumor necrosis factor-α. Select downstream substrates of mTORC1 and processes mediated by them are also shown. The figure was adapted with permission from ref. 252, Oxford University Press.
One of the best described systems for regulating the nucleotide-binding status of Rag GTPases is the activity of the GATOR complexes. GATOR1 functions as a GAP for RagA and RagB, while GATOR2 acts to inhibit the activity of GATOR1 (refs. 167,168). The GATOR complexes are regulated by levels of amino acids, cholesterol and glycolytic intermediates, thus linking mTORC1 activity with nutrient availability. Three different amino acid sensors have been found that regulate mTORC1 activity by controlling GATOR1 or GATOR2 activity. The sestrin and CASTOR families of proteins link the availability of leucine and arginine, respectively, to the recruitment of mTORC1 to the lysosomal surface. Specifically, the sestrin family of proteins binds to and inhibits the action of GATOR2 when leucine levels are low, permitting GATOR1 to inhibit the recruitment of mTORC1 to the lysosome. Binding of leucine by the sestrins, particularly sestrin 2, relieves this inhibition of GATOR2, resulting in inhibition of GATOR1 GAP activity and allowing mTORC1 to be recruited to the lysosome162,169.
The CASTOR proteins function similarly; when arginine levels are low, CASTOR proteins bind to and inhibit GATOR2. When arginine levels are high, CASTOR proteins bind to arginine and release GATOR2, which allows the recruitment of mTORC1 to the lysosome170,171. The SAMTOR protein acts as an indirect sensor of methionine levels, inhibiting GATOR1 when levels of the methionine metabolite S-adenosylmethionine (SAM) are low128. As SAM is extremely responsive to methionine levels, SAMTOR essentially functions as a sensor of methionine levels172. It was recently shown that cholesterol signals through a G protein-coupled receptor, LYCHOS, which links cholesterol levels to mTORC1 activity by sequestering GATOR1 in the presence of cholesterol173. Finally, while glucose is not directly sensed by mTORC1, the glycolytic intermediate dihydroxyacetone phosphate (DHAP) is sensed via a GATOR-dependent mechanism2.
The regulation of RagC and RagD is somewhat less well understood, but the folliculin (FLCN) complex has been shown to act as a GAP for these GTPases174,175,176,177. Leucyl-tRNA synthetase (LRS) has been shown to function as a leucine sensor for mTORC1, acting as a GAP for RagD178. The mitochondrial threonyl-tRNA synthetase TARS2 functions as a threonine sensor, interacting with GTP–RagC to promote GTP loading of RagA, probably via recruitment of an unidentified RagA GEF179.
At the lysosomal surface, mTORC1 activity depends upon the interaction of the mTOR protein kinase with GTP-bound RHEB. Cryo-electron microscopy has revealed that RHEB–GTP binds allosterically to mTOR, resulting in a global conformational change that allosterically realigns the active-site residues to enable substrate phosphorylation157. At the lysosomal surface, TSC inhibits mTORC1 activity by acting as a GAP for RHEB. A number of different factors have been reported to control the lysosomal localization of TSC, most notably, insulin–PI3K–AKT signaling, which acts to phosphorylates TSC on multiple residues, causing TSC to depart from the lysosome and permitting RHEB to be loaded by GTP180. The localization of TSC has also been reported to be sensitive to amino acids, including arginine, although the mechanism by which this takes place is unclear181. Rag GTPases have also been reported to recruit TSC to lysosomes in response to amino acid restriction, possibly via a GATOR2- or sestrin 2-dependent mechanism182.
Researchers are capitalizing on this knowledge to develop new but still early-stage mTORC1-selective drugs based on molecular and structural information about mTORC1 activation (Fig. 2). One of the best examples of these is the compound is NR1, which binds the mTORC1 activator RHEB and prevents it from allosterically activating mTORC1 (ref. 164). LRS has been proposed to function as a leucine sensor for mTORC1, acting as a GAP for RagD, and several recent compounds, for example, (S)-4-isobutyloxazolidin-2-one and BC-LI-0186, have been identified that inhibit mTORC1 by interfering with LRS sensing or activity178,183,184,185,186. BC-LI-0186 inhibits mTORC1 activity in vivo in mice and slows tumor growth in a mouse model of non-small-cell lung cancer187. As outlined in Fig. 2, small molecules that interfere with amino acid sensors or cholesterol sensors that normally signal nutrient availability could potentially be developed as mTORC1-selective inhibitors.
Newer rapalogs have been discovered that are more selective for mTORC1 than rapamycin. One company that screened a library of modified rapalogs identified a compound, DL001, with significantly greater selectivity for mTORC1 than rapamycin120. As expected, mice treated with DL001 had reduced glucose intolerance, dyslipidemia and immune disruption as compared to mice treated in parallel with rapamycin120. Multiple other companies are also working to bring more mTORC1-selective rapalogs to the clinic188. Preclinical trials of one such compound, NV-20494, have reportedly shown efficacy in a mouse model of polycystic kidney disease and in vitro in human three-dimensional cell culture189. Finally, Rapalink-1, a compound in which an mTOR kinase inhibitor is linked to rapamycin and delivered at a low dose, has shown the ability to inhibit mTORC1 kinase activity selectively190. A potential issue with this approach for diseases of aging is that mTOR kinase inhibitors result in broader mTORC1 inhibition than rapamycin53, and it remains to be determined whether mTOR kinase inhibitors recapitulate the lifespan benefits of rapamycin in preclinical species.
Conclusions
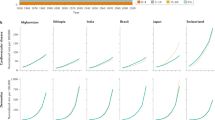
There is rapidly growing interest in using mTOR inhibitors to promote healthy aging and to treat, delay or reverse numerous age-related diseases. While there is incredibly strong preclinical evidence in mice that rapamycin can extend lifespan and healthspan, excitement about rapamycin has outpaced rigorous evidence that rapalogs are both safe and efficacious for diseases of aging in humans. There are many unanswered questions from the trials that have been conducted thus far, but a few general lessons can be taken from the clinical trials of mTOR inhibitors that have been performed thus far. As highlighted in Fig. 3, in both humans and mice, treatment with low or intermittent doses of rapamycin or everolimus or treatment of mice with the mTORC1-selective inhibitor DL001, is much better tolerated than the high doses of mTOR inhibitors currently approved for organ transplant and oncology indications, with fewer metabolic side effects and less immunosuppression. In addition, low doses of mTOR inhibitors have been shown to have some beneficial effects on the function of aging human organ systems, in particular, the immune system.
Chronic (daily) dosing of rapamycin is associated with impaired blood glucose regulation and hyperlipidemia in humans and mice, while everolimus in mice has somewhat reduced effects on glucose homeostasis. Intermittent or low-dose regimens of rapamycin or everolimus are associated with reduced side effects, while the mTORC1-selective rapalog DL001 does not impair blood glucose control or alter circulating lipid levels. Blue up arrow, improvement; red down arrow, impairment; dash indicates no change; question mark indicates unknown.
There remains much work ahead to bring mTOR inhibitors into the clinic for age-related conditions, and, as highlighted in Fig. 3, many open questions remain. While the safety profile of low-dose rapamycin and rapalogs in humans appears promising, the long-term safety and efficacy of low-dose regimens remain to be determined. A much better understanding is needed of the specific dose and duration of mTOR inhibitors that both maximize efficacy and minimize risk. In humans, higher doses (for example, 3 mg per day) of mTOR inhibitors such as everolimus inhibit T cell function and are therefore are used to suppress immune-mediated organ transplant rejection in patients. By contrast, a sixfold lower dose of everolimus for 6 weeks was associated with improved immune function as assessed by vaccination response. Thus, both dose and duration may contribute to whether mTOR inhibition has positive or negative effects on healthy aging, but, generally speaking, the lower the dose of a drug, the fewer expected side effects. Moreover, animal dosing regimens that extend lifespan cannot be directly translated to human doses due to differences between species in factors such as bioavailability, half-life, metabolism, plasma protein binding and tissue distribution. These factors need to be taken into consideration when estimating the human doses that may extend healthspan or lifespan.
There is also a need to identify both the specific aging population and the specific aging-related conditions that show the greatest benefit from a safe mTOR-inhibitor regimen. An important question for future research is discovering why mTOR inhibitors have sex-specific or sex-biased benefits, as pharmacological treatment with rapamycin or genetic inhibition of insulin–insulin-like growth factor 1 (IGF1)–PI3K–AKT–mTOR–S6K1 signaling typically (but not always) extends the lifespan of female mice a greater amount than it extends the lifespan of male mice191,192,193. We also need to define new regulatory paths for aging-related conditions such as frailty and sarcopenia and to develop new mTOR inhibitors that improve on the safety and efficacy of currently approved mTOR inhibitors. Over the next 5 years, we expect results from a rapidly expanding list of human clinical trials as well as work in canines and non-human primates to shed light on the viability of mTOR inhibition as a therapy for aging-related conditions. New mTORC1-specific molecules may help to widen the therapeutic window for rapalogs, limiting undesirable side effects resulting in whole or in part from inhibition of mTORC2. Collectively, we expect that researchers will soon be able to determine whether clinicians can safely and effectively bring mTOR inhibitors to the geriatric bedside.
References
Castellano, B. M. et al. Lysosomal cholesterol activates mTORC1 via an SLC38A9–Niemann–Pick C1 signaling complex. Science 355, 1306–1311 (2017).
Orozco, J. M. et al. Dihydroxyacetone phosphate signals glucose availability to mTORC1. Nat. Metab. 2, 893–901 (2020).
Lamming, D. W. & Bar-Peled, L. Lysosome: the metabolic signaling hub. Traffic 20, 27–38 (2019).
Simcox, J. & Lamming, D. W. The central moTOR of metabolism. Dev. Cell 57, 691–706 (2022).
Kaeberlein, M. et al. Regulation of yeast replicative life span by TOR and Sch9 in response to nutrients. Science 310, 1193–1196 (2005).
Kapahi, P. et al. Regulation of lifespan in Drosophila by modulation of genes in the TOR signaling pathway. Curr. Biol. 14, 885–890 (2004).
Powers, R. W. 3rd, Kaeberlein, M., Caldwell, S. D., Kennedy, B. K. & Fields, S. Extension of chronological life span in yeast by decreased TOR pathway signaling. Genes Dev. 20, 174–184 (2006).
Vellai, T. et al. Genetics: influence of TOR kinase on lifespan in C. elegans. Nature 426, 620 (2003).
Hansen, M. et al. Lifespan extension by conditions that inhibit translation in Caenorhabditis elegans. Aging Cell 6, 95–110 (2007).
Syntichaki, P., Troulinaki, K. & Tavernarakis, N. eIF4E function in somatic cells modulates ageing in Caenorhabditis elegans. Nature 445, 922–926 (2007).
Medvedik, O., Lamming, D. W., Kim, K. D. & Sinclair, D. A. MSN2 and MSN4 link calorie restriction and TOR to sirtuin-mediated lifespan extension in Saccharomyces cerevisiae. PLoS Biol. 5, e261 (2007).
Sharp, Z. D. & Bartke, A. Evidence for down-regulation of phosphoinositide 3-kinase/Akt/mammalian target of rapamycin (PI3K/Akt/mTOR)-dependent translation regulatory signaling pathways in Ames dwarf mice. J. Gerontol. A Biol. Sci. Med. Sci. 60, 293–300 (2005).
Selman, C. et al. Ribosomal protein S6 kinase 1 signaling regulates mammalian life span. Science 326, 140–144 (2009).
Arif, A. et al. EPRS is a critical mTORC1–S6K1 effector that influences adiposity in mice. Nature 542, 357–361 (2017).
Tsai, S. et al. Muscle-specific 4E-BP1 signaling activation improves metabolic parameters during aging and obesity. J. Clin. Invest. 125, 2952–2964 (2015).
Tsai, S. Y. et al. Increased 4E-BP1 expression protects against diet-induced obesity and insulin resistance in male mice. Cell Rep. 16, 1903–1914 (2016).
Lamming, D. W. et al. Rapamycin-induced insulin resistance is mediated by mTORC2 loss and uncoupled from longevity. Science 335, 1638–1643 (2012).
Wu, J. J. et al. Increased mammalian lifespan and a segmental and tissue-specific slowing of aging after genetic reduction of mTOR expression. Cell Rep. 4, 913–920 (2013).
Zhang, H. M., Diaz, V., Walsh, M. E. & Zhang, Y. Moderate lifelong overexpression of tuberous sclerosis complex 1 (TSC1) improves health and survival in mice. Sci. Rep. 7, 834 (2017).
Powolny, A. A., Singh, S. V., Melov, S., Hubbard, A. & Fisher, A. L. The garlic constituent diallyl trisulfide increases the lifespan of C. elegans via skn-1 activation. Exp. Gerontol. 46, 441–452 (2011).
Robida-Stubbs, S. et al. TOR signaling and rapamycin influence longevity by regulating SKN-1/Nrf and DAF-16/FoxO. Cell Metab. 15, 713–724 (2012).
Bjedov, I. et al. Mechanisms of life span extension by rapamycin in the fruit fly Drosophila melanogaster. Cell Metab. 11, 35–46 (2010).
Rice, K. M., Kinnard, R. S., Wright, G. L. & Blough, E. R. Aging alters vascular mechanotransduction: pressure-induced regulation of p70S6k in the rat aorta. Mech. Ageing Dev. 126, 1213–1222 (2005).
Solon-Biet, S. M. et al. The ratio of macronutrients, not caloric intake, dictates cardiometabolic health, aging, and longevity in ad libitum-fed mice. Cell Metab. 19, 418–430 (2014).
Wilkinson, J. E. et al. Rapamycin slows aging in mice. Aging Cell 11, 675–682 (2012).
Lamming, D. W., Ye, L., Sabatini, D. M. & Baur, J. A. Rapalogs and mTOR inhibitors as anti-aging therapeutics. J. Clin. Invest. 123, 980–989 (2013).
Vezina, C., Kudelski, A. & Sehgal, S. N. Rapamycin (AY-22,989), a new antifungal antibiotic. I. Taxonomy of the producing streptomycete and isolation of the active principle. J. Antibiot. 28, 721–726 (1975).
Sarbassov, D. D. et al. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr. Biol. 14, 1296–1302 (2004).
Scaiola, A. et al. The 3.2-Å resolution structure of human mTORC2. Sci. Adv. 6, eabc1251 (2020).
Gaubitz, C. et al. Molecular basis of the rapamycin insensitivity of target of rapamycin complex 2. Mol. Cell 58, 977–988 (2015).
Yip, C. K., Murata, K., Walz, T., Sabatini, D. M. & Kang, S. A. Structure of the human mTOR complex I and its implications for rapamycin inhibition. Mol. Cell 38, 768–774 (2010).
Sarbassov, D. D. et al. Prolonged rapamycin treatment inhibits mTORC2 assembly and Akt/PKB. Mol. Cell 22, 159–168 (2006).
Harrison, D. E. et al. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature 460, 392–395 (2009).
Hahn, O. et al. A nutritional memory effect counteracts benefits of dietary restriction in old mice. Nat. Metab. 1, 1059–1073 (2019).
Flurkey, K., Astle, C. M. & Harrison, D. E. Life extension by diet restriction and N-acetyl-l-cysteine in genetically heterogeneous mice. J. Gerontol. A Biol. Sci. Med. Sci. 65, 1275–1284 (2010).
Miller, R. A. et al. Rapamycin, but not resveratrol or simvastatin, extends life span of genetically heterogeneous mice. J. Gerontol. A Biol. Sci. Med. Sci. 66, 191–201 (2011).
Arriola Apelo, S. I., Pumper, C. P., Baar, E. L., Cummings, N. E. & Lamming, D. W. Intermittent administration of rapamycin extends the life span of female C57BL/6J mice. J. Gerontol. A Biol. Sci. Med. Sci. 71, 876–881 (2016).
Bitto, A. et al. Transient rapamycin treatment can increase lifespan and healthspan in middle-aged mice. eLife 5, e16351 (2016).
Chen, C., Liu, Y., Liu, Y. & Zheng, P. mTOR regulation and therapeutic rejuvenation of aging hematopoietic stem cells. Sci. Signal. 2, ra75 (2009).
Anisimov, V. N. et al. Rapamycin extends maximal lifespan in cancer-prone mice. Am. J. Pathol. 176, 2092–2097 (2010).
Anisimov, V. N. et al. Rapamycin increases lifespan and inhibits spontaneous tumorigenesis in inbred female mice. Cell Cycle 10, 4230–4236 (2011).
Shindyapina, A. V. et al. Rapamycin treatment during development extends life span and health span of male mice and Daphnia magna. Sci. Adv. 8, eabo5482 (2022).
Aiello, G. et al. Transient rapamycin treatment during developmental stage extends lifespan in Mus musculus and Drosophila melanogaster. EMBO Rep. 23, e55299 (2022).
Strong, R. et al. Longer lifespan in male mice treated with a weakly estrogenic agonist, an antioxidant, an α-glucosidase inhibitor or a Nrf2-inducer. Aging Cell 15, 872–884 (2016).
Strong, R. et al. Lifespan benefits for the combination of rapamycin plus acarbose and for captopril in genetically heterogeneous mice. Aging Cell 21, e13724 (2022).
Moloney, P. B., Cavalleri, G. L. & Delanty, N. Epilepsy in the mTORopathies: opportunities for precision medicine. Brain Commun. 3, fcab222 (2021).
Sills, A. M., Artavia, J. M., DeRosa, B. D., Ross, C. N. & Salmon, A. B. Long-term treatment with the mTOR inhibitor rapamycin has minor effect on clinical laboratory markers in middle-aged marmosets. Am. J. Primatol. 81, e22927 (2019).
Urfer, S. R. et al. A randomized controlled trial to establish effects of short-term rapamycin treatment in 24 middle-aged companion dogs. GeroScience 39, 117–127 (2017).
Creevy, K. E., Akey, J. M., Kaeberlein, M., Promislow, D. E. L. & Dog Aging Project, C. An open science study of ageing in companion dogs. Nature 602, 51–57 (2022).
Orgel, L. E. The maintenance of the accuracy of protein synthesis and its relevance to ageing. Proc. Natl Acad. Sci. USA 49, 517–521 (1963).
Ke, Z. et al. Translation fidelity coevolves with longevity. Aging Cell 16, 988–993 (2017).
Mieulet, V. et al. S6 kinase inactivation impairs growth and translational target phosphorylation in muscle cells maintaining proper regulation of protein turnover. Am. J. Physiol. Cell Physiol. 293, C712–C722 (2007).
Thoreen, C. C. et al. An ATP-competitive mammalian target of rapamycin inhibitor reveals rapamycin-resistant functions of mTORC1. J. Biol. Chem. 284, 8023–8032 (2009).
Pedersen, S., Celis, J. E., Nielsen, J., Christiansen, J. & Nielsen, F. C. Distinct repression of translation by wortmannin and rapamycin. Eur. J. Biochem. 247, 449–456 (1997).
Thoreen, C. C. et al. A unifying model for mTORC1-mediated regulation of mRNA translation. Nature 485, 109–113 (2012).
Jefferies, H. B. et al. Rapamycin suppresses 5′TOP mRNA translation through inhibition of p70s6k. EMBO J. 16, 3693–3704 (1997).
Steffen, K. K. et al. Yeast life span extension by depletion of 60S ribosomal subunits is mediated by Gcn4. Cell 133, 292–302 (2008).
Park, Y., Reyna-Neyra, A., Philippe, L. & Thoreen, C. C. mTORC1 balances cellular amino acid supply with demand for protein synthesis through post-transcriptional control of ATF4. Cell Rep. 19, 1083–1090 (2017).
Byles, V. et al. Hepatic mTORC1 signaling activates ATF4 as part of its metabolic response to feeding and insulin. Mol. Metab. 53, 101309 (2021).
Condon, K. J. et al. Genome-wide CRISPR screens reveal multitiered mechanisms through which mTORC1 senses mitochondrial dysfunction. Proc. Natl Acad. Sci. USA 118, e2022120118 (2021).
De Sousa-Coelho, A. L., Marrero, P. F. & Haro, D. Activating transcription factor 4-dependent induction of FGF21 during amino acid deprivation. Biochem. J. 443, 165–171 (2012).
Kim, K. H. et al. Autophagy deficiency leads to protection from obesity and insulin resistance by inducing Fgf21 as a mitokine. Nat. Med. 19, 83–92 (2013).
Arif, A. et al. Two-site phosphorylation of EPRS coordinates multimodal regulation of noncanonical translational control activity. Mol. Cell 35, 164–180 (2009).
Guo, M., Yang, X. L. & Schimmel, P. New functions of aminoacyl-tRNA synthetases beyond translation. Nat. Rev. Mol. Cell Biol. 11, 668–674 (2010).
Alvers, A. L. et al. Autophagy is required for extension of yeast chronological life span by rapamycin. Autophagy 5, 847–849 (2009).
Hars, E. S. et al. Autophagy regulates ageing in C. elegans. Autophagy 3, 93–95 (2007).
Lionaki, E., Markaki, M. & Tavernarakis, N. Autophagy and ageing: insights from invertebrate model organisms. Ageing Res. Rev. 12, 413–428 (2012).
Hansen, M. et al. A role for autophagy in the extension of lifespan by dietary restriction in C. elegans. PLoS Genet. 4, e24 (2008).
Cuervo, A. M. et al. Autophagy and aging: the importance of maintaining “clean” cells. Autophagy 1, 131–140 (2005).
Han, X. et al. Influence of long-term caloric restriction on myocardial and cardiomyocyte contractile function and autophagy in mice. J. Nutr. Biochem. 23, 1592–1599 (2012).
Kume, S. et al. Calorie restriction enhances cell adaptation to hypoxia through Sirt1-dependent mitochondrial autophagy in mouse aged kidney. J. Clin. Invest. 120, 1043–1055 (2010).
Wang, M. & Miller, R. A. Fibroblasts from long-lived mutant mice exhibit increased autophagy and lower TOR activity after nutrient deprivation or oxidative stress. Aging Cell 11, 668–674 (2012).
Kim, J., Kundu, M., Viollet, B. & Guan, K. L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat. Cell Biol. 13, 132–141 (2011).
Hosokawa, N. et al. Nutrient-dependent mTORC1 association with the ULK1–Atg13–FIP200 complex required for autophagy. Mol. Biol. Cell 20, 1981–1991 (2009).
Dossou, A. S. & Basu, A. The emerging roles of mTORC1 in macromanaging autophagy. Cancers 11, 1422 (2019).
Zhang, C. & Cuervo, A. M. Restoration of chaperone-mediated autophagy in aging liver improves cellular maintenance and hepatic function. Nat. Med. 14, 959–965 (2008).
Hua, Y. et al. Chronic Akt activation accentuates aging-induced cardiac hypertrophy and myocardial contractile dysfunction: role of autophagy. Basic Res. Cardiol. 106, 1173–1191 (2011).
Brandhorst, S. et al. A periodic diet that mimics fasting promotes multi-system regeneration, enhanced cognitive performance, and healthspan. Cell Metab. 22, 86–99 (2015).
Majumder, S., Richardson, A., Strong, R. & Oddo, S. Inducing autophagy by rapamycin before, but not after, the formation of plaques and tangles ameliorates cognitive deficits. PLoS ONE 6, e25416 (2011).
Spilman, P. et al. Inhibition of mTOR by rapamycin abolishes cognitive deficits and reduces amyloid-β levels in a mouse model of Alzheimer’s disease. PLoS ONE 5, e9979 (2010).
Yousefzadeh, M. J. et al. An aged immune system drives senescence and ageing of solid organs. Nature 594, 100–105 (2021).
Mannick, J. B. et al. mTOR inhibition improves immune function in the elderly. Sci. Transl. Med. 6, 268ra179 (2014).
Mannick, J. B. et al. TORC1 inhibition enhances immune function and reduces infections in the elderly. Sci. Transl. Med. 10, eaaq1564 (2018).
Mannick, J. B. et al. Targeting the biology of ageing with mTOR inhibitors to improve immune function in older adults: phase 2b and phase 3 randomised trials. Lancet Healthy Longev. 2, e250–e262 (2021).
Goldberg, E. L., Smithey, M. J., Lutes, L. K., Uhrlaub, J. L. & Nikolich-Zugich, J. Immune memory-boosting dose of rapamycin impairs macrophage vesicle acidification and curtails glycolysis in effector CD8 cells, impairing defense against acute infections. J. Immunol. 193, 757–763 (2014).
Phillips, E. J. & Simons, M. J. P. Rapamycin not dietary restriction improves resilience against pathogens: a meta-analysis. GeroScience 45, 1263–1270 (2023).
Neff, F. et al. Rapamycin extends murine lifespan but has limited effects on aging. J. Clin. Invest. 123, 3272–3291 (2013).
Zhou, J. et al. mTOR supports long-term self-renewal and suppresses mesoderm and endoderm activities of human embryonic stem cells. Proc. Natl Acad. Sci. USA 106, 7840–7845 (2009).
Murakami, M. et al. mTOR is essential for growth and proliferation in early mouse embryos and embryonic stem cells. Mol. Cell. Biol. 24, 6710–6718 (2004).
Lee, K. W. et al. Rapamycin promotes the osteoblastic differentiation of human embryonic stem cells by blocking the mTOR pathway and stimulating the BMP/Smad pathway. Stem Cells Dev. 19, 557–568 (2010).
Yilmaz, O. H. et al. Pten dependence distinguishes haematopoietic stem cells from leukaemia-initiating cells. Nature 441, 475–482 (2006).
Greenberger, S. et al. Rapamycin suppresses self-renewal and vasculogenic potential of stem cells isolated from infantile hemangioma. J. Invest. Dermatol. 131, 2467–2476 (2011).
Xie, L. X. et al. Rapamycin inhibited the function of lung CSCs via SOX2. Tumour Biol. 37, 4929–4937 (2016).
Wang, Y. et al. Rapamycin inhibits FBXW7 loss-induced epithelial–mesenchymal transition and cancer stem cell-like characteristics in colorectal cancer cells. Biochem. Biophys. Res. Commun. 434, 352–356 (2013).
Jang, Y. Y. & Sharkis, S. J. A low level of reactive oxygen species selects for primitive hematopoietic stem cells that may reside in the low-oxygenic niche. Blood 110, 3056–3063 (2007).
Yilmaz, O. H. et al. mTORC1 in the Paneth cell niche couples intestinal stem-cell function to calorie intake. Nature 486, 490–495 (2012).
Baar, E. L., Carbajal, K. A., Ong, I. M. & Lamming, D. W. Sex- and tissue-specific changes in mTOR signaling with age in C57BL/6J mice. Aging Cell 15, 155–166 (2016).
Markofski, M. M. et al. Effect of age on basal muscle protein synthesis and mTORC1 signaling in a large cohort of young and older men and women. Exp. Gerontol. 65, 1–7 (2015).
White, Z., White, R. B., McMahon, C., Grounds, M. D. & Shavlakadze, T. High mTORC1 signaling is maintained, while protein degradation pathways are perturbed in old murine skeletal muscles in the fasted state. Int. J. Biochem. Cell Biol. 78, 10–21 (2016).
Joseph, G. A. et al. Partial inhibition of mTORC1 in aged rats counteracts the decline in muscle mass and reverses molecular signaling associated with sarcopenia. Mol. Cell. Biol. 39, e00141-19 (2019).
Ham, D. J. et al. The neuromuscular junction is a focal point of mTORC1 signaling in sarcopenia. Nat. Commun. 11, 4510 (2020).
An, W. L. et al. Up-regulation of phosphorylated/activated p70 S6 kinase and its relationship to neurofibrillary pathology in Alzheimer’s disease. Am. J. Pathol. 163, 591–607 (2003).
Perluigi, M. et al. Neuropathological role of PI3K/Akt/mTOR axis in Down syndrome brain. Biochim. Biophys. Acta 1842, 1144–1153 (2014).
Tramutola, A. et al. Alteration of mTOR signaling occurs early in the progression of Alzheimer disease (AD): analysis of brain from subjects with pre-clinical AD, amnestic mild cognitive impairment and late-stage AD. J. Neurochem. 133, 739–749 (2015).
Caccamo, A., Majumder, S., Richardson, A., Strong, R. & Oddo, S. Molecular interplay between mammalian target of rapamycin (mTOR), amyloid-β, and tau: effects on cognitive impairments. J. Biol. Chem. 285, 13107–13120 (2010).
Houtkooper, R. H. et al. The metabolic footprint of aging in mice. Sci. Rep. 1, 134 (2011).
Leontieva, O. V., Paszkiewicz, G. M. & Blagosklonny, M. V. Fasting levels of hepatic p-S6 are increased in old mice. Cell Cycle 13, 2656–2659 (2014).
Calhoun, C. et al. Senescent cells contribute to the physiological remodeling of aged lungs. J. Gerontol. A Biol. Sci. Med. Sci. 71, 153–160 (2016).
Blagosklonny, M. V. Rapamycin treatment early in life reprograms aging: hyperfunction theory and clinical practice. Aging 14, 8140–8149 (2022).
Wang, R. et al. Rapamycin inhibits the secretory phenotype of senescent cells by a Nrf2-independent mechanism. Aging Cell 16, 564–574 (2017).
Soukas, A. A., Kane, E. A., Carr, C. E., Melo, J. A. & Ruvkun, G. Rictor/TORC2 regulates fat metabolism, feeding, growth, and life span in Caenorhabditis elegans. Genes Dev. 23, 496–511 (2009).
Mizunuma, M., Neumann-Haefelin, E., Moroz, N., Li, Y. & Blackwell, T. K. mTORC2–SGK-1 acts in two environmentally responsive pathways with opposing effects on longevity. Aging Cell 13, 869–878 (2014).
Chang, K. et al. TGFB–INHB/activin signaling regulates age-dependent autophagy and cardiac health through inhibition of MTORC2. Autophagy 16, 1807–1822 (2020).
Yu, D. et al. Calorie-restriction-induced insulin sensitivity is mediated by adipose mTORC2 and not required for lifespan extension. Cell Rep. 29, 236–248 (2019).
Chellappa, K. et al. Hypothalamic mTORC2 is essential for metabolic health and longevity. Aging Cell 18, e13014 (2019).
Arriola Apelo, S. I. et al. Ovariectomy uncouples lifespan from metabolic health and reveals a sex-hormone-dependent role of hepatic mTORC2 in aging. eLife 9, e56177 (2020).
Lamming, D. W. et al. Depletion of Rictor, an essential protein component of mTORC2, decreases male lifespan. Aging Cell 13, 911–917 (2014).
Garratt, M. et al. Male lifespan extension with 17-α estradiol is linked to a sex-specific metabolomic response modulated by gonadal hormones in mice. Aging Cell 17, e12786 (2018).
Dominick, G. et al. Regulation of mTOR activity in Snell dwarf and GH receptor gene-disrupted mice. Endocrinology 156, 565–575 (2015).
Schreiber, K. H. et al. A novel rapamycin analog is highly selective for mTORC1 in vivo. Nat. Commun. 10, 3194 (2019).
Sadtler, K. et al. Developing a pro-regenerative biomaterial scaffold microenvironment requires T helper 2 cells. Science 352, 366–370 (2016).
Festuccia, W. T., Pouliot, P., Bakan, I., Sabatini, D. M. & Laplante, M. Myeloid-specific Rictor deletion induces M1 macrophage polarization and potentiates in vivo pro-inflammatory response to lipopolysaccharide. PLoS ONE 9, e95432 (2014).
Katholnig, K. et al. Inactivation of mTORC2 in macrophages is a signature of colorectal cancer that promotes tumorigenesis. JCI Insight 4, e124164 (2019).
Yang, C. et al. mTORC1 and mTORC2 differentially promote natural killer cell development. eLife 7, e35619 (2018).
Hallowell, R. W. et al. mTORC2 signalling regulates M2 macrophage differentiation in response to helminth infection and adaptive thermogenesis. Nat. Commun. 8, 14208 (2017).
Zhang, L. et al. Mammalian target of rapamycin complex 2 controls CD8 T cell memory differentiation in a Foxo1-dependent manner. Cell Rep. 14, 1206–1217 (2016).
Powell, J. D., Pollizzi, K. N., Heikamp, E. B. & Horton, M. R. Regulation of immune responses by mTOR. Annu. Rev. Immunol. 30, 39–68 (2012).
Guertin, D. A. et al. mTOR complex 2 is required for the development of prostate cancer induced by Pten loss in mice. Cancer Cell 15, 148–159 (2009).
Fang, X. et al. LINC00998 functions as a novel tumor suppressor in acute myeloid leukemia via regulating the ZFP36 ring finger protein/mammalian target of rapamycin complex 2 axis. Bioengineered 12, 10363–10372 (2021).
Tian, L. et al. mTORC2 regulates ribonucleotide reductase to promote DNA replication and gemcitabine resistance in non-small cell lung cancer. Neoplasia 23, 643–652 (2021).
Ding, Y. et al. Vimentin loss promotes cancer proliferation through up-regulating Rictor/AKT/β-catenin signaling pathway. Exp. Cell Res. 405, 112666 (2021).
Johnson, S. C. et al. mTOR inhibition alleviates mitochondrial disease in a mouse model of Leigh syndrome. Science 342, 1524–1528 (2013).
Martin-Perez, M. et al. PKC downregulation upon rapamycin treatment attenuates mitochondrial disease. Nat. Metab. 2, 1472–1481 (2020).
Walters, H. E., Deneka-Hannemann, S. & Cox, L. S. Reversal of phenotypes of cellular senescence by pan-mTOR inhibition. Aging 8, 231–244 (2016).
Chung, C. L. et al. Topical rapamycin reduces markers of senescence and aging in human skin: an exploratory, prospective, randomized trial. GeroScience 41, 861–869 (2019).
Tabernero, J. et al. Dose- and schedule-dependent inhibition of the mammalian target of rapamycin pathway with everolimus: a phase I tumor pharmacodynamic study in patients with advanced solid tumors. J. Clin. Oncol. 26, 1603–1610 (2008).
Novartis. Full Prescribing Information Zortress https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021560s000lbl.pdf (2010).
Pfizer. Full Prescribing Information Rapamune https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021083s059,021110s076lbl.pdf (2017).
Trelinska, J. et al. Complications of mammalian target of rapamycin inhibitor anticancer treatment among patients with tuberous sclerosis complex are common and occasionally life-threatening. Anticancer Drugs 26, 437–442 (2015).
Krueger, D. A. et al. Long-term treatment of epilepsy with everolimus in tuberous sclerosis. Neurology 87, 2408–2415 (2016).
Johnston, O., Rose, C. L., Webster, A. C. & Gill, J. S. Sirolimus is associated with new-onset diabetes in kidney transplant recipients. J. Am. Soc. Nephrol. 19, 1411–1418 (2008).
Firpi, R. J. et al. Sirolimus-induced hyperlipidaemia in liver transplant recipients is not dose-dependent. Aliment. Pharmacol. Ther. 19, 1033–1039 (2004).
Bissler, J. J. et al. Everolimus long-term use in patients with tuberous sclerosis complex: four-year update of the EXIST-2 study. PLoS ONE 12, e0180939 (2017).
Arriola Apelo, S. I. et al. Alternative rapamycin treatment regimens mitigate the impact of rapamycin on glucose homeostasis and the immune system. Aging Cell 15, 28–38 (2016).
Zuber, J. et al. Sirolimus may reduce fertility in male renal transplant recipients. Am. J. Transplant. 8, 1471–1479 (2008).
Huyghe, E. et al. Gonadal impact of target of rapamycin inhibitors (sirolimus and everolimus) in male patients: an overview. Transpl. Int. 20, 305–311 (2007).
File, T. M. Viral respiratory tract infections: increasing importance and a new pathogen. Curr. Opin. Infect. Dis. 16, 125–127 (2003).
Jain, S. et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N. Engl. J. Med. 373, 415–427 (2015).
Kraig, E. et al. A randomized control trial to establish the feasibility and safety of rapamycin treatment in an older human cohort: immunological, physical performance, and cognitive effects. Exp. Gerontol. 105, 53–69 (2018).
Miller, R. A. et al. Methionine-deficient diet extends mouse lifespan, slows immune and lens aging, alters glucose, T4, IGF-I and insulin levels, and increases hepatocyte MIF levels and stress resistance. Aging Cell 4, 119–125 (2005).
Green, C. L. et al. Dietary restriction of isoleucine increases healthspan and lifespan of genetically heterogeneous mice. Preprint at https://doi.org/10.1101/2022.10.06.511051 (2022).
Richardson, N. E. et al. Lifelong restriction of dietary branched-chain amino acids has sex-specific benefits for frailty and lifespan in mice. Nat. Aging 1, 73–86 (2021).
Deelen, J. et al. A metabolic profile of all-cause mortality risk identified in an observational study of 44,168 individuals. Nat. Commun. 10, 3346 (2019).
Roberts, M. N. et al. A ketogenic diet extends longevity and healthspan in adult mice. Cell Metab. 26, 539–546 (2017).
Aylett, C. H. et al. Architecture of human mTOR complex 1. Science 351, 48–52 (2016).
Yang, H. et al. 4.4 Å resolution cryo-EM structure of human mTOR complex 1. Protein Cell 7, 878–887 (2016).
Yang, H. et al. Mechanisms of mTORC1 activation by RHEB and inhibition by PRAS40. Nature 552, 368–373 (2017).
Ramlaul, K. et al. Architecture of the tuberous sclerosis protein complex. J. Mol. Biol. 433, 166743 (2021).
Shen, K. et al. Architecture of the human GATOR1 and GATOR1–Rag GTPases complexes. Nature 556, 64–69 (2018).
Anandapadamanaban, M. et al. Architecture of human Rag GTPase heterodimers and their complex with mTORC1. Science 366, 203–210 (2019).
Rogala, K. B. et al. Structural basis for the docking of mTORC1 on the lysosomal surface. Science 366, 468–475 (2019).
Saxton, R. A. et al. Structural basis for leucine sensing by the sestrin2–mTORC1 pathway. Science 351, 53–58 (2016).
Long, X., Lin, Y., Ortiz-Vega, S., Yonezawa, K. & Avruch, J. Rheb binds and regulates the mTOR kinase. Curr. Biol. 15, 702–713 (2005).
Mahoney, S. J. et al. A small molecule inhibitor of Rheb selectively targets mTORC1 signaling. Nat. Commun. 9, 548 (2018).
Sancak, Y. et al. The Rag GTPases bind raptor and mediate amino acid signaling to mTORC1. Science 320, 1496–1501 (2008).
Kim, E., Goraksha-Hicks, P., Li, L., Neufeld, T. P. & Guan, K. L. Regulation of TORC1 by Rag GTPases in nutrient response. Nat. Cell Biol. 10, 935–945 (2008).
Panchaud, N., Peli-Gulli, M. P. & De Virgilio, C. Amino acid deprivation inhibits TORC1 through a GTPase-activating protein complex for the Rag family GTPase Gtr1. Sci. Signal. 6, ra42 (2013).
Bar-Peled, L. et al. A tumor suppressor complex with GAP activity for the Rag GTPases that signal amino acid sufficiency to mTORC1. Science 340, 1100–1106 (2013).
Wolfson, R. L. et al. Sestrin2 is a leucine sensor for the mTORC1 pathway. Science 351, 43–48 (2016).
Saxton, R. A., Chantranupong, L., Knockenhauer, K. E., Schwartz, T. U. & Sabatini, D. M. Mechanism of arginine sensing by CASTOR1 upstream of mTORC1. Nature 536, 229–233 (2016).
Chantranupong, L. et al. The CASTOR proteins are arginine sensors for the mTORC1 pathway. Cell 165, 153–164 (2016).
Haws, S. A. et al. Methyl-metabolite depletion elicits adaptive responses to support heterochromatin stability and epigenetic persistence. Mol. Cell 78, 210–223 (2020).
Shin, H. R. et al. Lysosomal GPCR-like protein LYCHOS signals cholesterol sufficiency to mTORC1. Science 377, 1290–1298 (2022).
Tsun, Z. Y. et al. The folliculin tumor suppressor is a GAP for the RagC/D GTPases that signal amino acid levels to mTORC1. Mol. Cell 52, 495–505 (2013).
Meng, J. & Ferguson, S. M. GATOR1-dependent recruitment of FLCN–FNIP to lysosomes coordinates Rag GTPase heterodimer nucleotide status in response to amino acids. J. Cell Biol. 217, 2765–2776 (2018).
Martinez-Carreres, L. et al. CDK4 regulates lysosomal function and mTORC1 activation to promote cancer cell survival. Cancer Res. 79, 5245–5259 (2019).
Jansen, R. M. et al. Structural basis for FLCN RagC GAP activation in MiT-TFE substrate-selective mTORC1 regulation. Sci. Adv. 8, eadd2926 (2022).
Han, J. M. et al. Leucyl-tRNA synthetase is an intracellular leucine sensor for the mTORC1-signaling pathway. Cell 149, 410–424 (2012).
Kim, S. H. et al. Mitochondrial threonyl-tRNA synthetase TARS2 is required for threonine-sensitive mTORC1 activation. Mol. Cell 81, 398–407 (2021).
Menon, S. et al. Spatial control of the TSC complex integrates insulin and nutrient regulation of mTORC1 at the lysosome. Cell 156, 771–785 (2014).
Carroll, B. et al. Control of TSC2–Rheb signaling axis by arginine regulates mTORC1 activity. eLife 5, e11058 (2016).
Yang, S. et al. The Rag GTPase regulates the dynamic behavior of TSC downstream of both amino acid and growth factor restriction. Dev. Cell 55, 272–288 (2020).
Yoon, S. et al. Discovery of leucyladenylate sulfamates as novel leucyl-tRNA synthetase (LRS)-targeted mammalian target of rapamycin complex 1 (mTORC1) inhibitors. J. Med. Chem. 59, 10322–10328 (2016).
Yoon, S. et al. Discovery of (S)-4-isobutyloxazolidin-2-one as a novel leucyl-tRNA synthetase (LRS)-targeted mTORC1 inhibitor. Bioorg. Med. Chem. Lett. 26, 3038–3041 (2016).
Yoon, S. et al. Discovery of simplified leucyladenylate sulfamates as novel leucyl-tRNA synthetase (LRS)-targeted mammalian target of rapamycin complex 1 (mTORC1) inhibitors. Bioorg. Med. Chem. 25, 4145–4152 (2017).
Kim, J. H. et al. Control of leucine-dependent mTORC1 pathway through chemical intervention of leucyl-tRNA synthetase and RagD interaction. Nat. Commun. 8, 732 (2017).
Kim, E. Y. et al. Therapeutic effects of the novel leucyl-tRNA synthetase inhibitor BC-LI-0186 in non-small cell lung cancer. Ther. Adv. Med. Oncol. 11, 1758835919846798 (2019).
Sullivan, D. New mTOR Player Storms into Longevity https://longevity.technology/news/new-mtor-player-storms-into-longevity/ (2022).
Mazin, A. Lessons from Longevity Therapeutics 2021—Part 4 https://www.lifespan.io/news/lessons-from-longevity-therapeutics-2021-part-4/ (2021).
Fan, Q. et al. A kinase inhibitor targeted to mTORC1 drives regression in glioblastoma. Cancer Cell 31, 424–435 (2017).
Lamming, D. W. Diminished mTOR signaling: a common mode of action for endocrine longevity factors. SpringerPlus 3, 735 (2014).
Mao, K. et al. Late-life targeting of the IGF-1 receptor improves healthspan and lifespan in female mice. Nat. Commun. 9, 2394 (2018).
Strong, R. et al. Rapamycin-mediated mouse lifespan extension: late-life dosage regimes with sex-specific effects. Aging Cell 19, e13269 (2020).
Zhang, Y. et al. Rapamycin extends life and health in C57BL/6 mice. J. Gerontol. A Biol. Sci. Med. Sci. 69, 119–130 (2014).
Miller, R. A. et al. Rapamycin-mediated lifespan increase in mice is dose and sex dependent and metabolically distinct from dietary restriction. Aging Cell 13, 468–477 (2014).
Fok, W. C. et al. Mice fed rapamycin have an increase in lifespan associated with major changes in the liver transcriptome. PLoS ONE 9, e83988 (2014).
Ferrara-Romeo, I. et al. The mTOR pathway is necessary for survival of mice with short telomeres. Nat. Commun. 11, 1168 (2020).
Fang, Y. et al. Effects of rapamycin on growth hormone receptor knockout mice. Proc. Natl Acad. Sci. USA 115, E1495–E1503 (2018).
Arriola Apelo, S. I. & Lamming, D. W. Rapamycin: an inhibiTOR of aging emerges from the soil of Easter Island. J. Gerontol. A Biol. Sci. Med. Sci. 71, 841–849 (2016).
Li, A. et al. Rapamycin treatment dose-dependently improves the cystic kidney in a new ADPKD mouse model via the mTORC1 and cell-cycle-associated CDK1/cyclin axis. J. Cell. Mol. Med. 21, 1619–1635 (2017).
Zhang, X. et al. Rapamycin treatment augments motor neuron degeneration in SOD1G93A mouse model of amyotrophic lateral sclerosis. Autophagy 7, 412–425 (2011).
Bhattacharya, A. et al. Dietary restriction but not rapamycin extends disease onset and survival of the H46R/H48Q mouse model of ALS. Neurobiol. Aging 33, 1829–1832 (2012).
Hernando, E. et al. The AKT–mTOR pathway plays a critical role in the development of leiomyosarcomas. Nat. Med. 13, 748–753 (2007).
Squarize, C. H., Castilho, R. M. & Gutkind, J. S. Chemoprevention and treatment of experimental Cowden’s disease by mTOR inhibition with rapamycin. Cancer Res. 68, 7066–7072 (2008).
Koehl, G. E. et al. Rapamycin inhibits oncogenic intestinal ion channels and neoplasia in APCMin/+ mice. Oncogene 29, 1553–1560 (2010).
Alexander, A. et al. ATM signals to TSC2 in the cytoplasm to regulate mTORC1 in response to ROS. Proc. Natl Acad. Sci. USA 107, 4153–4158 (2010).
Ohara, T. et al. Inhibition of mTOR by temsirolimus contributes to prolonged survival of mice with pleural dissemination of non-small-cell lung cancer cells. Cancer Sci. 102, 1344–1349 (2011).
Comas, M. et al. New nanoformulation of rapamycin Rapatar extends lifespan in homozygous p53−/− mice by delaying carcinogenesis. Aging 4, 715–722 (2012).
Hussein, O., Tiedemann, K., Murshed, M. & Komarova, S. V. Rapamycin inhibits osteolysis and improves survival in a model of experimental bone metastases. Cancer Lett. 314, 176–184 (2012).
Komarova, E. A. et al. Rapamycin extends lifespan and delays tumorigenesis in heterozygous p53+/− mice. Aging 4, 709–714 (2012).
Maude, S. L. et al. Targeting JAK1/2 and mTOR in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood 120, 3510–3518 (2012).
Livi, C. B. et al. Rapamycin extends life span of Rb1+/− mice by inhibiting neuroendocrine tumors. Aging 5, 100–110 (2013).
Hasty, P. et al. eRapa restores a normal life span in a FAP mouse model. Cancer Prev. Res. 7, 169–178 (2014).
Morran, D. C. et al. Targeting mTOR dependency in pancreatic cancer. Gut 63, 1481–1489 (2014).
Popovich, I. G. et al. Lifespan extension and cancer prevention in HER-2/neu transgenic mice treated with low intermittent doses of rapamycin. Cancer Biol. Ther. 15, 586–592 (2014).
Christy, B. et al. p53 and rapamycin are additive. Oncotarget 6, 15802–15813 (2015).
Ando, T. et al. Gemcitabine and rapamycin exhibit additive effect against osteosarcoma by targeting autophagy and apoptosis. Cancers 12, 3097 (2020).
Kon, N. et al. mTOR inhibition acts as an unexpected checkpoint in p53-mediated tumor suppression. Genes Dev. 35, 59–64 (2021).
Parihar, M. et al. Sex-dependent lifespan extension of ApcMin/+ FAP mice by chronic mTOR inhibition. Aging Pathobiol. Ther. 2, 187–194 (2020).
Parihar, M. et al. Rapamycin extends life span in ApcMin/+ colon cancer FAP model. Clin. Colorectal Cancer 20, e61–e70 (2021).
Tibarewal, P. et al. Long-term treatment of cancer-prone germline PTEN mutant mice with low-dose rapamycin extends lifespan and delays tumour development. J. Pathol. 258, 382–394 (2022).
Khapre, R. V. et al. BMAL1-dependent regulation of the mTOR signaling pathway delays aging. Aging 6, 48–57 (2014).
Leontieva, O. V., Paszkiewicz, G. M. & Blagosklonny, M. V. Weekly administration of rapamycin improves survival and biomarkers in obese male mice on high-fat diet. Aging Cell 13, 616–622 (2014).
Sataranatarajan, K. et al. Rapamycin increases mortality in db/db mice, a mouse model of type 2 diabetes. J. Gerontol. A Biol. Sci. Med. Sci. 71, 850–857 (2016).
Yuskaitis, C. J. et al. Chronic mTORC1 inhibition rescues behavioral and biochemical deficits resulting from neuronal Depdc5 loss in mice. Hum. Mol. Genet. 28, 2952–2964 (2019).
Klofas, L. K., Short, B. P., Zhou, C. & Carson, R. P. Prevention of premature death and seizures in a Depdc5 mouse epilepsy model through inhibition of mTORC1. Hum. Mol. Genet. 29, 1365–1377 (2020).
Hurez, V. et al. Chronic mTOR inhibition in mice with rapamycin alters T, B, myeloid, and innate lymphoid cells and gut flora and prolongs life of immune-deficient mice. Aging Cell 14, 945–956 (2015).
Feng, X. et al. Rapamycin is highly effective in murine models of immune-mediated bone marrow failure. Haematologica 102, 1691–1703 (2017).
Correia-Melo, C. et al. Rapamycin improves healthspan but not inflammaging in nfκb1−/− mice. Aging Cell 18, e12882 (2019).
Warner, L. M., Adams, L. M. & Sehgal, S. N. Rapamycin prolongs survival and arrests pathophysiologic changes in murine systemic lupus erythematosus. Arthritis Rheum. 37, 289–297 (1994).
Zaradzki, M. et al. Short-term rapamycin treatment increases life span and attenuates aortic aneurysm in a murine model of Marfan-syndrome. Biochem. Pharmacol. 205, 115280 (2022).
Johnson, S. C. et al. Dose-dependent effects of mTOR inhibition on weight and mitochondrial disease in mice. Front. Genet. 6, 247 (2015).
Siegmund, S. E. et al. Low-dose rapamycin extends lifespan in a mouse model of mtDNA depletion syndrome. Hum. Mol. Genet. 26, 4588–4605 (2017).
Cortes, C. J., Qin, K., Cook, J., Solanki, A. & Mastrianni, J. A. Rapamycin delays disease onset and prevents PrP plaque deposition in a mouse model of Gerstmann–Straussler–Scheinker disease. J. Neurosci. 32, 12396–12405 (2012).
Ramos, F. J. et al. Rapamycin reverses elevated mTORC1 signaling in lamin A/C-deficient mice, rescues cardiac and skeletal muscle function, and extends survival. Sci. Transl. Med. 4, 144ra103 (2012).
Liao, C. Y. et al. Rapamycin reverses metabolic deficits in lamin A/C-deficient mice. Cell Rep. 17, 2542–2552 (2016).
Birkisdottir, M. B. et al. Unlike dietary restriction, rapamycin fails to extend lifespan and reduce transcription stress in progeroid DNA repair-deficient mice. Aging Cell 20, e13302 (2021).
Zeng, L. H., Xu, L., Gutmann, D. H. & Wong, M. Rapamycin prevents epilepsy in a mouse model of tuberous sclerosis complex. Ann. Neurol. 63, 444–453 (2008).
Lee, N. et al. Rapamycin weekly maintenance dosing and the potential efficacy of combination sorafenib plus rapamycin but not atorvastatin or doxycycline in tuberous sclerosis preclinical models. BMC Pharmacol. 9, 8 (2009).
Liang, M. C. et al. TSC1 loss synergizes with KRAS activation in lung cancer development in the mouse and confers rapamycin sensitivity. Oncogene 29, 1588–1597 (2010).
Woodrum, C., Nobil, A. & Dabora, S. L. Comparison of three rapamycin dosing schedules in A/J Tsc2+/− mice and improved survival with angiogenesis inhibitor or asparaginase treatment in mice with subcutaneous tuberous sclerosis related tumors. J. Transl. Med. 8, 14 (2010).
Malhowski, A. J. et al. Smooth muscle protein-22-mediated deletion of Tsc1 results in cardiac hypertrophy that is mTORC1-mediated and reversed by rapamycin. Hum. Mol. Genet. 20, 1290–1305 (2011).
Nechama, M., Makayes, Y., Resnick, E., Meir, K. & Volovelsky, O. Rapamycin and dexamethasone during pregnancy prevent tuberous sclerosis complex-associated cystic kidney disease. JCI Insight 5, e136857 (2020).
Iwata, W. et al. Podocyte-specific deletion of tubular sclerosis complex 2 promotes focal segmental glomerulosclerosis and progressive renal failure. PLoS ONE 15, e0229397 (2020).
Halloran, J. et al. Chronic inhibition of mammalian target of rapamycin by rapamycin modulates cognitive and non-cognitive components of behavior throughout lifespan in mice. Neuroscience 223, 102–113 (2012).
Lin, A. L. et al. Rapamycin rescues vascular, metabolic and learning deficits in apolipoprotein E4 transgenic mice with pre-symptomatic Alzheimer’s disease. J. Cereb. Blood Flow Metab. 37, 217–226 (2017).
Van Skike, C. E. et al. mTOR drives cerebrovascular, synaptic, and cognitive dysfunction in normative aging. Aging Cell 19, e13057 (2020).
Dai, D. F. et al. Altered proteome turnover and remodeling by short-term caloric restriction or rapamycin rejuvenate the aging heart. Aging Cell 13, 529–539 (2014).
Flynn, J. M. et al. Late-life rapamycin treatment reverses age-related heart dysfunction. Aging Cell 12, 851–862 (2013).
Zaseck, L. W., Miller, R. A. & Brooks, S. V. Rapamycin attenuates age-associated changes in tibialis anterior tendon viscoelastic properties. J. Gerontol. A Biol. Sci. Med. Sci. 71, 858–865 (2016).
Liang, S. J., Zhou, J. Y. & Wang, X. Q. Signaling network centered on mTORC1 dominates mammalian intestinal stem cell ageing. Stem Cell Rev. Rep. 17, 842–849 (2021).
Dumas, S. N. & Lamming, D. W. Next generation strategies for geroprotection via mTORC1 inhibition. J. Gerontol. A Biol. Sci. Med. Sci. 75, 14–23 (2020).
Acknowledgements
We thank M. Simons for suggesting additional references to include in our tables of rapamycin lifespan and survival studies, A. Salmon for sharing information about his in-progress studies and many of our colleagues for providing additional information about their published studies and current and future plans. The Lamming laboratory is supported in part by the NIH–NIA (AG056771, AG062328, AG061635 and AG076941), the NIH–NIDDK (DK125859) and startup and other funds from the University of Wisconsin—Madison School of Medicine and Public Health and the Department of Medicine to D.W.L. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
J.B.M. and D.W.L. wrote the manuscript and prepared the figures.
Corresponding author
Ethics declarations
Competing interests
J.B.M. is CEO and cofounder of Tornado Therapeutics, which is developing safer, more effective mTOR inhibitors to extend human healthspan, and a former CMO of resTORbio. D.W.L. has received funding from and is a scientific advisory board member of Aeovian Pharmaceuticals, which seeks to develop new, selective mTOR inhibitors for the treatment of various diseases.
Peer review
Peer review information
Nature Aging thanks Troy Merry and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mannick, J.B., Lamming, D.W. Targeting the biology of aging with mTOR inhibitors. Nat Aging 3, 642–660 (2023). https://doi.org/10.1038/s43587-023-00416-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-023-00416-y
This article is cited by
-
Evaluating the effect of rapamycin treatment in Alzheimer’s disease and aging using in vivo imaging: the ERAP phase IIa clinical study protocol
BMC Neurology (2024)
-
Molecular mechanisms of aging and anti-aging strategies
Cell Communication and Signaling (2024)
-
mTORC1 in energy expenditure: consequences for obesity
Nature Reviews Endocrinology (2024)
-
Lysosomes as coordinators of cellular catabolism, metabolic signalling and organ physiology
Nature Reviews Molecular Cell Biology (2024)
-
Everolimus alleviates CD4+ T cell inflammation by regulating autophagy and cellular redox homeostasis
GeroScience (2024)