Abstract
Ingestible electronics can potentially be used to track and treat gastrointestinal diseases in real time. In the past decade, substantial improvements have been made to ingestible electronic pills at the sensor, circuit and system levels, which has improved the clinical applicability of the technology by increasing device sensitivity, lifetime and location awareness. Here we explore the development of ingestible electronics and provide a step-by-step guide for the design of ingestible capsules at the system level. We consider the anatomical and physiological characteristics of gastrointestinal organs, which set requirements and constraints on ingestible electronics in terms of size, shape, topology and the materials used for packaging. We then examine the key design components: sensors and actuators, integrated circuits, communication, power, packaging, localization and locomotion. We also consider the challenges that must be addressed to realize the full application potential of ingestible electronics.
Similar content being viewed by others
Main
The first generation of ingestible electronic pills—which measured gastric pH, pressure and temperature—was reported in the 1960s1,2. However, it was the introduction of the PillCam capsule endoscope in 2000 that launched recent progress in the development of smart pills3. Modern capsules now incorporate different kinds of sensing, actuation, energy storage and communication components in a small form factor to diagnose and treat various gastrointestinal (GI) disorders. The minimally invasive nature of these devices allows physicians to monitor any organ of the GI tract, including the small intestine, which is not easily accessible by conventional endoscopy. Ingestible electronic devices are also of increasing interest in medical technology, with growth in both investments and the number of companies involved in the area4,5. The main factors for this growth are patient preference for minimally invasive procedures and the potential for healthcare providers to remotely monitor patients6. The ingestible capsules market is expected to be worth US$8.98 billion in 2024, with capsule endoscopy, remote patient monitoring and targeted drug delivery the key application areas7.
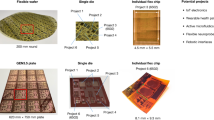
An ingestible pill is composed of various parts—including sensors, actuators, integrated circuits and power modules—that are chosen depending on the intended use4,8,9,10. There are numerous options for each of these components, with each option having distinct advantages and drawbacks, as well as varying sizes and power consumptions. This variety can make it challenging for both academic labs and companies to begin to construct their own ingestible pills. In this Review, we provide a step-by-step guide for designing ingestible electronic capsules. We first provide an overview of the anatomy, physiology and pathophysiology of the GI tract. We then examine the functional blocks of ingestibles, focusing on seven components of the design process (Fig. 1): sensors and actuators, integrated circuits, communication, power, packaging, localization and locomotion. The first five of these are essential for any ingestible; localization and locomotion are increasingly popular functionalities but not a requirement. We also highlight two electronic capsules—a camera-based ingestible pill with an onboard artificial intelligence (AI) accelerator and an optical-sensing ingestible pill with three-dimensional (3D) magnetic localization—to explore the design process and provide a more practical guide to the design of ingestible devices. Finally, we explore the issues that currently limit further progress in the field and the wider application of the technology.
The choice of (1) sensors and actuators, (2) integrated circuits, (3) communication, (4) power and (5) packaging drives the design process. The first five components are essential. (6) Localization and (7) locomotion are emerging functionalities that can be added to the design. The selection, pros and cons for the available choices of these seven components are described in detail in the main text.
Gastrointestinal organs
The main function of the GI tract is to digest and absorb nutrients and excrete waste products of digestion. Moreover, the GI tract has an extensive intrinsic nervous system, termed the enteric nervous system (ENS), that interacts with the central nervous system (CNS), regulates immune homoeostasis and maintains gut microbiota11,12. The GI tract comprises four concentric layers: mucosa, submucosa, muscularis, and serosa or adventitia. The mucosa, the innermost layer composed of simple epithelium cells, plays a role in absorbing, transforming and secreting nutrients, and protecting the body from resident bacterial flora and ingested pathogens by limiting their diffusion. The submucosa is a thick layer of loose connective tissue surrounding the mucosa, which contains blood vessels, lymphatics and nerves. The muscularis is responsible for segmental contractions, which enable mechanical digestion and peristaltic movements of the food along the GI tract. The serosa or adventitia is the outermost layer, whose primary function is to lubricate the body’s internal structures or to hold the internal structures together. The main organs comprising the GI tract are the oesophagus, stomach, small intestine and large intestine. The function, pH, transit times of food, pathologies and the types of sensing used in these organs are summarized in Fig. 2.
Oesophagus
Once the food is ingested, the oesophagus transports it to the stomach through peristaltic contractions, usually occurring in a few seconds. The common disorders associated with this organ are gastroesophageal reflux disease, achalasia, eosinophilic oesophagitis, oesophageal cancer, oesophageal spasms and oesophageal strictures, the symptoms of which include tissue irritation, inflammation, swelling and muscle spasms, resulting in a reduced diameter of the oesophagus. These conditions can be assessed with traditional endoscopes and imaging capsules.
Stomach
In the stomach, the ingested food undergoes mechanical and chemical disintegration. Mechanical contractions break down food particles into smaller pieces, while the secretion of gastric fluid and enzymes turns them into chyme. The typical transit time of food in the stomach ranges from 15 minutes to 4 hours, and may take longer if the patient suffers from gastroparesis, a medical condition associated with impaired motility of the stomach13. The most prevalent stomach disorders include peptic ulcers, gastritis and stomach cancer, for many of which the cause is Helicobacter pylori infection14. Biomarkers such as pH, metabolites, enzymes, gases, electrolytes, bacteria and overall integrity of mucosa layer are essential parameters of a healthy stomach that can be assessed through traditional and capsule endoscopy, tissue biopsy and gastric fluid sampling8.
Small intestine
The digestion and majority of nutrient absorption occur in the small intestine, composed of the duodenum, jejunum and ileum. The duodenum is the shortest section of the small intestine, where the acidic chyme produced in the stomach is exposed to pancreatic digestive enzymes and bile acids secreted by the gallbladder. Bicarbonate secretions from Brunner’s glands and the pancreas neutralize the highly acidic gastric juice, thus protecting the intestinal wall from degradation. Here, digestion enzymes break down proteins, carbohydrates, triglycerides and nucleic acids to smaller sizes13. Further along the small intestine is the jejunum, with a mucosa layer containing two levels of finger-like projections called villi and microvilli, which increase the surface area of tissue available to absorb nutrients. Most products of digestion, including amino acids, carbohydrates and fatty acids, are absorbed into the bloodstream here. The final segment of the small intestine is the ileum. It also contains villi and microvilli similar to the jejunum, and it mainly absorbs bile acids, vitamin B12 and other remaining nutrients, including small sugar units, glycerol and fatty acids8,15. Traditional endoscopy, colonoscopy and more convenient capsule endoscopy are used to diagnose these disorders. Another abnormality that mainly affects the small intestine is obstruction, which is a mechanical blockage of the bowel that hernias or intra-abdominal adhesions may cause. A complete bowel obstruction is an emergency that needs immediate surgery, which accounts for 20% of emergency surgical procedures16. For maintaining good health in the small intestine, it is essential to have balanced electrolyte levels, gases, metabolites and bacteria.
Large intestine
The large intestine is made up of the caecum, appendix, colon, rectum and anal canal. The colon absorbs water and other remaining absorbable nutrients from the processed food and then excretes the indigestible matter to the rectum in solid faeces. The colonic bacterial community is diverse (>1,000 species) and accounts for ~1.5 kg of the colon weight8,17. It is established that changing the diet alters the gut microbiota composition18. Furthermore, the gut microbiome interacts with the ENS and CNS (gut–brain axis), and its alteration has been observed in different neurodevelopmental and neurodegenerative disorders19,20. Colonoscopy is the gold standard in assessing the quality of the colon mucosa in search of inflammation and wounds that may further reveal different disorders such as colorectal cancer, colonic polyps and ulcerative colitis. Also, analysing stool samples may reveal abnormalities such as poor nutrient absorption and infections from parasites, viruses and bacteria21.
Sensors and actuators
Sensing
A variety of biomarkers present in the GI tract, such as bacteria22, metabolites23, physiological gases24, proteins25 and neurotransmitters26, can be sensed and leveraged to assess a patient’s health in real time. The connection of some of these biomarkers with different GI, neurodegenerative and neurodevelopmental diseases has been demonstrated by analysing patients’ stool samples or biopsy specimens collected from patients’ rectum through colonoscopy19,20,21. Ingestible pills with embedded optical, electrochemical, electrical, biological and mechanical sensors can be utilized for diagnostics of different diseases and abnormalities in a more convenient and time-efficient way, as described in the following paragraphs (Fig. 3).
a, AI-empowered wireless video endoscopic capsule30. b, Ingestible pill with haem-sensitive probiotic biosensor for diagnosis of GI bleeding64. c, Galvanically self-powered capsule for glucose detection54. d, Osmotic pill for in vivo sampling of gut microbiome79. e, Self-orienting millimetre-scale applicator capsule for drug delivery and electrical stimulation of the GI wall119. f, Ingestible pill with an intragastric balloon for obesity treatment113. g, Ingestible capsule for electrical stimulation of the GI wall194. Panels adapted with permission from: a, ref. 30, under a Creative Commons licence CC BY 4.0; b, ref. 64, AAAS; c, ref. 54, under a Creative Commons licence CC BY 4.0; d, ref. 79, under a Creative Commons licence CC BY 4.0; e, ref. 119, under a Creative Commons licence CC BY 4.0; f, ref. 113, IOP Publishing; g, ref. 194, IOP Publishing.
Imaging
Capsule endoscopes rely on visible wavelengths of light to perform optical imaging of the mucosal surface and detect GI pathologies using high-resolution cameras and light-emitting diodes (LEDs). Numerous capsule endoscopes are distributed by companies such as Medtronic, Intro-Medic, Jinshan, CapsoVision, RF System Lab, Olympus Medical, Sonopill Programme, AnX Robotica and Check-Cap, and have been extensively reviewed in past literature4,6. It must be noted that substantial progress has been made in the analysis of capsule endoscopy images by various AI algorithms. In particular, deep learning has been widely utilized for classifying different GI disorders including bleeding, ulcers, oesophagitis, polyps, hookworm, and coeliac and Crohn’s diseases with mostly >90% accuracy27,28,29. Although most of these research outcomes examined the pictures sent from the pill externally, it is also possible to have onboard deep neural network capabilities30,31. This allows the pill to classify the images locally and then transmit only the final results to the external reader. This approach reduces the amount of data sent from the pill, thus, relaxing the data-rate requirements of an onboard transmitter, but possibly at the cost of extra power consumption of an onboard microcontroller unit (MCU).
Capsule endoscopy shows only the mucosal surface, which does not reveal abnormalities within the GI wall. Submucosal ultrasound imaging with a tethered ingestible device can provide a transmural or cross-sectional image of the GI tract, achieving a 10 mm imaging depth and a resolution as high as 40 μm (ref. 32). X-ray-based ingestible electronic devices can also be used to evaluate the GI tract. Once the capsule reaches the colon, it generates a low dose of X-ray beams, which interact with the ingested contrast agents, tissue walls and the contents of the colon. The reflected X-ray fluorescence photons are then detected by the capsule to identify precancerous polyps33,34. The tethered ingestible capsule with confocal microscopy capability has been utilized to diagnose and monitor eosinophilic oesophagitis—an allergic condition that is characterized by eosinophils infiltrating the oesophageal wall35. The endomicroscope can also be implemented as a tethered ingestible capsule to capture cross-sectional microscopic images of the GI wall and generate 3D, microstructural images of the upper GI tract36.
In general, imaging techniques consume a substantial amount of power, which is why most of the methods mentioned above are tethered. To eliminate the need for wires and make the pill completely wireless, it it necessary to use batteries with high capacity or optimize the power consumption of these techniques.
Optical sensing
In cases when imaging is not necessary, ingestible capsules equipped with optical sensors can be utilized to record a target biomarker. Typically, ingestible pills use an LED to emit light and then measure the light absorption using a photodiode37. To detect internal bleeding, the commercially available HemoPill uses this phenomenon to measure the optical absorption at 415 nm between an LED and a photodetector38. Another example of spectrometric sensing is the capsule with laser diodes and photodiodes that can detect infrared fluorescence emitted by indocyanine green fluorophore dye, which is one of the infrared fluorescent-labelling contrast agents used for efficient early-stage cancer detection39. The fluorescence-based sensing systems can also detect microbiome nucleic acids in the GI fluid, which is suitable for detecting the gut microbiome distribution in vivo40. In a similar study, an ingestible pill was demonstrated that collects GI fluids into an internal sponge and then uses an integrated fluorescence-based assay to measure the sponge’s changing optical properties caused by viable bacteria41. Overall, optical systems can be very compact due to a variety of small microLEDs and photodiodes available on the market. In terms of power consumption, optical systems are power hungry—the LED itself typically requires tens of milliamperes while the analogue front end that interfaces with the photodiode can consume microampere-level current42 (Supplementary Table 1).
Electrochemical sensing
Various voltammetric techniques, such as cyclic, square-wave and differential pulse, can be implemented on the ingestible device with traditional three-electrode electrochemical sensors. One example is pH sensing, which is related to GI diseases such as gastric ulcers, functional dyspepsia, Crohn’s disease and ulcerative colitis43,44. Ingestible capsules have been used to measure GI pH in different studies for decades45. Yet, there are still many attempts to simplify the production, reduce the cost and minimize the size of pH-sensing electrodes46,47. The Bravo and SmartPill capsules distributed by Medtronic are commercially available products that measure pH in the GI tract. The SmartPill has been successfully utilized to measure gastric emptying time by indicating the passage from one organ to another with pH measurements, which has the potential to replace gamma camera scintigraphy—the current standard of care for diagnosing gastroparesis48. Ingestible platforms with traditional and aptamer-conjugated electrochemical sensors can also characterize the gut fluids to diagnose GI diseases such as Crohn’s and ulcerative colitis49,50. It is also possible to measure neurotransmitters in the GI tract, which play a big role in multiple GI disorders and the gut–brain axis bidirectional network51. Recently, several studies have presented completely food-based edible electrochemical sensors consisting of corn, olive oil, mushroom, horseradish and activated charcoal, which were characterized in voltammetric detection of catechol, uric acid, ascorbic acid, dopamine, acetaminophen and glucose in artificial saliva, gastric fluid and intestinal fluid52,53. It has also been demonstrated that an ingestible pill powered with a glucose biofuel cell can also be used to measure changing glucose concentrations from the extracted power itself. What makes this study unique is its elimination of the need for extra sensors to measure glucose levels. Instead, the glucose collected for self-powering directly modulates the carrier signal frequency of a radiofrequency (RF) transmitter, which can then be correlated with glucose concentration from the RF receiver side54.
When designing electrochemical sensors for ingestible devices, it is extremely important to take into account the highly acidic environment in the stomach. Sensors must have enhanced ability against low-pH environments or be protected with a temporal polymer coating that dissolves later in the intestine. To address non-adherence to drug treatment plans, a couple of ingestible devices that can be attached to medication pills to monitor adherence were proposed and commercialized—the Proteus Digital55 pill (2012) and the EtectRx56 pill (2019). Both pills operate in a similar way: once the medication tagged with the smart pill reaches the stomach, gastric juice dissolves the pill’s external coating and powers internal electronics by forming a galvanic coupling with two electrodes, and transmits a signal to the external reader, indicating successful drug administration57.
Apart from durability in the highly acidic environment of the stomach, other challenges associated with electrochemical sensors include selectivity and drift over time. During the sensor’s initial design and validation on the laboratory bench, it is important to ensure that the sensor is immune to interference due to several other substances present in the GI tract. In addition, the measurements from amperometric sensors tend to drift over time even if they were appropriately calibrated initially, which can be partially counteracted by either discontinuing sensor usage before the drift is expected to surpass a specific threshold or employing differential measurements to cancel background current58. When it comes to the analogue front end (for example, potentiostat), there are several off-the-shelf and custom solutions with small area and low power consumption (Supplementary Table 1). The availability, cost and development time should be considered when choosing the right sensor and analogue front-end electronics.
Electrical sensing
As a non-invasive and accurate alternative to the body core temperature measurements obtained from the pulmonary artery, oesophagus, tympanic membrane, nasopharynx and rectum, it has been shown that ingestible capsules can continuously monitor the internal body temperature of healthcare workers wearing personal protective equipment59, individuals during active heating and cooling60, firefighters during the work shift61, and individuals during sleep and exercise60,62. Ingestible temperature sensors can assist people to stay within safe levels of core temperature, and detect hypothermia and hyperthermia right away. Ingestible capsules for measuring body core temperature are commercially available and distributed by Medtronic, Philips and HQ. A human pilot trial of an ingestible electronic capsule revealed that it can successfully sense oxygen, hydrogen and carbon dioxide in the GI tract63. The capsule employed semiconducting metal–oxide-based and thermal conductivity sensors to measure the gas concentrations in the GI tract. Eventually, a research group founded Atmo Biosciences to commercialize their gas-sensing capsules, which can potentially reveal functional aspects of the intestine’s response to dietary changes and medical supplements, and can also replace breath tests—the most common method used to measure and assess gases in the gut. As of today, there are no commercially available gas sensors that can be directly integrated into the capsule form factor.
Biological sensing
It has been demonstrated that genetically modified, bacteria-based sensors can be integrated with ingestible electronics. In one study, a research group altered the genome of Escherichia coli to produce luminescence in the presence of haem64. A similar approach has been taken in another work to genetically encode E. coli to respond to nitric oxide and hydrogen sulfide—key signals and mediators of inflammatory bowel disease65. Both sensors have been integrated with a photodetector and custom readout chip, and the capsule efficacy has been successfully tested in pig intestine. A big advantage of this method is that it does not require an LED, which substantially reduces the power requirements. However, a major concern with these sensors is their ability to survive the challenging conditions of the GI tract, including the stomach’s highly acidic environment. Bacteria-based sensors, in particular, may be sensitive to these conditions and at risk of being washed out by GI fluids.
It is also possible to detect gut bacteria activity with sensors composed of edible materials such as guar gum, a dietary fibre that is decomposed by bifidobacteria. After integrating the sensor with an antenna made from rice paper and gold, it was confirmed that the proposed guar gum film was substantially degraded by bifidobacteria in benchtop experiments66. The primary challenge associated with these sensors is the ability to accurately quantify the concentration of a specific type of bacteria relative to the amount of edible material that has been decomposed.
Mechanical sensing
Ingestible capsules are capable of recording the pressure in the GI tract, an elevated value of which may lead to the development of pressure-induced organ dysfunction and failure46,67. In vivo measurement results in pigs were comparable to invasive gold-standard recordings via telemetry pressure probes68. Pressure-sensing ingestible pills were utilized to measure the internal pressure due to underwater or in-air blast exposure encountered by military divers, which can be helpful in unravelling the mechanisms of blast injury and the way blast energy interacts with all areas of the human body69. SmartPill is the only commercially available, US Food and Drug Administration (FDA)-approved intraluminal pressure-sensing pill, which is also capable of measuring pH and temperature in the GI tract. It utilizes a solid-state microelectromechanical-system pressure sensor to measure pressure changes as it travels through the GI tract70. To directly measure the motility and activity of GI muscles, an ingestible device with flexible piezoelectric components can be used to sense mechanical deformations within the gastric cavity, which has been successfully tested in both in vitro- and ex vivo-simulated gastric models71. Piezoelectric pressure sensors generate an electrical charge when subjected to mechanical stress or pressure. They are typically easier to fabricate, more robust and self-powered. Microelectromechanical-system pressure sensors, in contrast, rely on the piezoresistive principle—their resistance changes in response to mechanical stress. They typically achieve higher resolution and result in more compact dimensions, but require external power72.
Tissue biopsy and microbiota sampling
GI tissue and microbiota fluid biopsy are essential for diagnosing diseases of the GI tract. The gold standard for acquiring tissue samples from the upper and lower GI tract are endoscopy and colonoscopy, respectively. Although these methods allow the reliable collection of tissue samples, they are usually associated with major discomfort and sometimes requires sedation. To avoid these negative aspects, several ingestible capsules with external magnetic actuation and self-sustained robotic mechanisms have been proposed to collect samples at a target GI location. Some capsules with internal permanent magnets or external magnetic shells can be controlled with an external permanent magnet or electromagnet to navigate them to the target location. The device then performs tissue biopsy by using microneedles73,74, untethered microgrippers75 or rotating-blade mechanisms76. Similarly, magnetically actuated pills can be used to collect GI liquid by using brushes77, a hydrogel78, an osmotic sampler79 and a self-polymerizing reaction mixture80. Recently, a device that collects liquid samples from multiple regions of the gut was successfully evaluated by collecting 240 intestinal samples from 15 healthy individuals81. Bacterial populations recovered from ingestible devices closely resembled the bacterial population demographics collected from stool samples. The advantage of the external magnetic actuation method is that zero power is consumed by the pill; however, it requires a bulky and complex external system to control the device. To achieve self-sustained locomotion, a capsule equipped with an internal camera, after naturally reaching the target location in the GI tract, can align and attach itself to the GI wall by using shape-memory alloy springs, and perform the biopsy by using internal razors82. Although this method does not require external bulky components, it needs a lot of power for a camera and other electronic components.
One disadvantage of collecting tissue and GI liquid samples using ingestible pills is the necessity to retrieve them from the toilet and send them back to the lab for further analysis. This adds an extra hurdle for the patients to adopt this approach. Having an on-pill analysis platform would solve this issue, but it is still far from being implemented because the tools required for analysis may vary and it might be difficult to effectively miniaturize them into pill form factor. Another concern about utilizing ingestible devices for collecting GI samples is the risk of contamination. It must be ensured that the samples collected at specific sites remain uncontaminated due to accidental penetration of other fluids and tissues from different parts of the GI tract, which can be accomplished by ensuring the integrity of the encapsulation81. In addition, there are numerous unanswered questions on the efficacy of such pills in clinical conditions as well as risks of bleeding and perforations in the GI tract.
Actuation
Along with sensing and diagnosing abnormalities, ingestible pills can also perform therapeutic actions such as drug delivery, cancer therapy, chronic constipation, obesity and GI dysmotility treatment (Fig. 3).
Chemical actuation
Orally administered medications can be susceptible to enzymatic degradation, adverse pH conditions, microbiota, mucus barriers and difficulty in crossing the epithelial barriers83. To address these limitations, injecting the drug directly into the GI wall is preferred, which is a routine part of some treatments for conditions such as bleeding ulcers and polypectomy84,85. It has been demonstrated that GI injection shows a quicker pharmacokinetic response compared with subcutaneous injection86 and active pharmaceutical ingredient plasma levels delivered by the drug delivery pill are comparable to those achieved with subcutaneous administration87,88. Several drug-carrying ingestible devices have been presented that utilize internal springs89,90, gas91, magnets92, an osmotic pump93 and a stepper motor94,95 to expel the drug-containing needle into the GI wall or diffuse the drug into the GI environment96. Among these methods, pills that use springs and magnets to release the drug are easiest to implement because they do not require active electronic components, they consume no power and they occupy the least volume. However, using a miniature stepper motor has its advantages, such as precise control of drug release amount and time, but these motors are usually quite power hungry and still are not optimal in terms of size.
One of the main challenges associated with microneedle-based drug delivery capsules is properly orienting the pill with needles facing the GI wall. Pills equipped with magnets can be externally controlled and oriented with the help of external permanent magnets or electromagnets. However, integrating the magnet is not always a solution because the pill can contain other electronic parts that can be affected by the magnet (for example, RF transceiver and antenna). To solve this problem, a pill with a mono-monostatic body that automatically orients itself towards the mucus can be used. One such shape is similar to a weeble-wobble toy, the leopard tortoise with a shifted centre of mass and a high-curvature upper shell that enables self-orientation to the preferred upright position87,88.
When it comes to safety, although microneedles are a relatively safe way of penetrating the GI wall, it is still important to note that some microneedles may induce temporary and minimal inflammation around the injection site97. Moreover, the force at which the microneedle is inserted into the tissue must be carefully optimized to reduce the risk of tissue perforation89. Several diffusion and microneedle-based ingestible capsules are currently undergoing clinical and pre-clinical animal trials98,99.
Ultrasonic actuation
Low-frequency ultrasound applied to the GI wall can be beneficial for increasing the uptake of drugs and potentially accelerating the treatment of GI diseases100,101. Also, ultrasonic therapy can be utilized in GI cancer treatment, which accounts for 26% of the global cancer incidence and 35% of all cancer-related deaths102. Besides chemotherapy and surgery, high-intensity focused ultrasound therapy applied to colorectal cancer tumour cells may have both thermal and non-thermal effects and result in ablation or mechanical disruption of target tissues, as well as enhancing the anticancer immune responses103,104. It has already been demonstrated that miniature ultrasonic transducers can be integrated into capsule form, and in vivo experiments in pigs have shown that fluorescent markers can penetrate the mucus layer of the small intestine at low acoustic powers105. The next application could be a GI cancer treatment with ultrasound. The main question marks, for now, are whether these compact ultrasonic transducers can generate sufficient power and, if yes, what should be the battery capacity to accommodate this functionality. The main safety concern with ultrasonic therapy is to ensure that it does not heat and burn the GI wall tissue.
Mechanical actuation
Ingestible pills can be used to treat chronic constipation by inducing vibration to stimulate peristalsis in the large intestine. Two ingestible capsules with such functionality have been proposed: the VIBRANT capsule from Vibrant Ltd106,107,108 and the VibraBot capsule from AnX Robotica109. While some studies have confirmed the efficacy of these pills107,109, others have indicated no substantial difference in spontaneous bowel movements between ‘pill’ and sham groups106,108. Ingestible capsules can also be used to perform versatile clinical procedures such as patching a wound in the stomach110. An origami-based ingestible microrobot can locomote to a desired location in a phantom oesophagus and stomach using external magnetic manipulation, patch a wound, remove foreign objects, deliver drugs and biodegrade.
In recent years, intragastric balloons (saline-filled silicone balloons) have gained popularity in minimally invasive obesity treatment. They are designed to reduce the stomach volume and food consumption by occupying space in the stomach and inducing satiety111. As of today, a catheter or endoscope is used to place it in the stomach, introduce liquid into the balloon and remove it afterwards. To achieve endoscope assistance-free operation in inflating and deflating, and inserting and removing the balloon, several ingestible pills have been proposed to perform this task112,113. Once the pill containing the deflated balloon has been ingested and reached the stomach, the valve present in the pill is opened with an external permanent magnet, allowing for an acid–base reaction to release carbon dioxide for inflation of the balloon. In the end, when the balloon is degraded, it deflates itself and naturally leaves the body through self-excretion112,114,115,116.
Electrical actuation
Multiple studies have demonstrated that electrical stimulation of the GI wall can modulate GI motility and, therefore, may be a promising alternative or addition to pharmacological treatments of GI dysmotility disorders117,118. It has been shown that electrical stimulation of the GI wall can be performed with an ingestible device that attaches itself to the GI wall by inserting electrically conductive, hooked probes and stimulates the tissue via timed electrical pulses to induce acute muscular contractions119. Moreover, electrical stimulation of the GI wall offers another way of treating obesity. A stimulator with electrodes connected to the stomach can apply a train of short pulses that have almost no effect on gastric motility but alter hormonal signals in the hypothalamus, reduce appetite, and produce an early sensation of fullness and satiety120. A miniature, self-powered device for vagus nerve stimulation has been tested in rats, and it was shown that, by the end of 100 days, the average body weight of rats with implanted stimulators was 38% less than that of the rats in the control group121.
Integrated circuits
After choosing the sensors and actuators, the next step is to include the associated circuits to read out the sensor data or drive the actuator. Typically, most of the sensing elements for ingestible devices are custom-designed due to constraints associated with size and shape. As these are just sensing elements, analogue/mixed-signal processing electronics must be included in the design to amplify, filter and pre-process the sensor data. This readout circuitry, also known as analogue front end (AFE), mainly consists of an amplifier and analogue-to-digital converter (ADC). There are a variety of AFE circuits available off-the-shelf that can be directly used for ingestible devices. However, they are usually not optimized for power consumption and size. An alternative approach is to individually find an amplifier and an ADC with minimal power and size specifications, and then combine them at the system level. However, this method could potentially lead to a larger overall footprint compared with using an AFE that is integrated within a single chip or package. However, custom AFEs can be designed, but at the cost of time (several months to design and fabricate the chip), money (US$1,000 mm−2 in Taiwan Semiconductor Manufacturing Company 180 nm complementary metal–oxide–semiconductor for a small quantity production, which might be substantially cheaper if mass produced) and effort122. Supplementary Table 1 provides a comparative view of commercial and custom AFEs for ingestibles.
As an example from Supplementary Table 1, we can compare two electrochemical AFEs: commercial NJU9101 and custom123. The first two parameters that may capture the reader’s attention are power consumption and supply voltage—the custom chip consumes 100 times less power and requires a 2 times smaller supply voltage. Even though both AFEs have 16-bit ADCs, the drastic difference in sampling rate is the main reason for reduced power consumption in the custom chip. Such a high sampling rate used in NJU9101 might not even be needed for a target ingestible device, therefore, burning more unnecessary power and requiring a battery with a bigger capacity. When it comes to chip size, the custom AFE occupies 44 times less area—another advantage of custom design. The size of NJU9101 (4 mm × 4 mm) might seem to be small, which is true, but it plays a big role when integrating multiple electronic parts in a single ingestible platform. Given all these parameters, choosing the right approach (off-the-shelf or custom) is important when choosing an AFE for the target device.
Communications
The wireless transceiver (TRX) is the next essential block in an ingestible pill. It allows the user to send different commands to the pill and receive the data recorded by the capsule without manually retrieving it at the end of the measurements. Typically, the TRX is the most area- and power-hungry unit in the ingestible platform. RF communication is the dominant technology used for wireless communication with ingestible devices. The TRX generally consists of an antenna, a matching network, and transmitter (TX) and receiver (RX) circuits (Fig. 4a). The matching network, consisting of capacitors and inductors, matches the impedance between an antenna and TRX circuitry. It can be implemented either on a printed circuit board or directly on a TRX chip. The TX’s power amplifier is used to drive an antenna and typically has a programmable output power. The low-noise amplifier in the RX picks up the signal from the antenna and amplifies it for further processing. Crystal oscillators are often used as a reference to generate a precise carrier signal. The power amplifier and the low-noise amplifier usually consume most of the TRX power. The modulator and demodulator circuits vary depending on the communication protocol.
a, Block diagram of conventional sensor and transceiver circuits. LNA, low-noise amplifier; PA, power amplifier; LO, local oscillator; PLL, phase-locked loop; TIA, transimpedance amplifier; OpAmp, operational amplifier. b, Components used for sensing and communication. The sensing and actuating elements are interfaced with an AFE, and a custom/commercial circuit solution is used along with an MCU for the control and communication tasks of the ingestible.
Selecting the appropriate communication frequency is critical for ingestible devices. Numerous frequency bands have been allocated by the Federal Communications Commission for this purpose: Medical Device Radio Communications Service (MedRadio) (401–406, 413–419, 426–432, 438–444 and 451–457 MHz), Industrial, Scientific, and Medical bands (13.553–13.567, 433.05–434.79, 902–928 and 2,400–2,500–MHz) and Medical Body Area Networks (2,360–2,400 MHz)124. Factors such as tissue attenuation and antenna dimensions affect the frequency selection process. Ideally, the dimensions of the antenna must be at least one-fourth or greater than the wavelength for efficient communication. Body tissues propagate RF signals more efficiently at lower frequencies. For instance, in an implant that transmits the data with a carrier signal frequency of 400 MHz and 2.4 GHz from the small or large intestine, the in-body path loss is ~3 dB cm−1 and ~8 dB cm−1, respectively125,126. It makes the 13.553–13.567 MHz frequency range an attractive option, but it does not support a high data transfer rate and, as a result of a longer wavelength, requires large antennas for adequate communication. In contrast, higher-frequency bands (902–928 and 2,300–2,500 MHz) have the advantage of supporting a high data rate and require smaller antennas but result in high signal attenuation, which reduces the maximum communication distance and necessitates more power to be radiated to compensate for that path loss. In recent years, MedRadio and 433 MHz Industrial, Scientific, and Medical frequency bands have been most widely utilized for ingestible capsules, including the commercialized Atmo Biosciences gas pill, and Medtronic’s PillCam and SmartPill capsules, as this frequency range offers a compromise between the tissue attenuation, data rate and antenna dimensions6. Several miniature antenna topologies (Fig. 4b), such as helix127, conformal128,129, patch130,131 and loop132,133, have been proposed to efficiently utilize the total volume available in the capsule to maximize the radiation efficiency and achieve omnidirectional radiation for orientation-insensitive communication.
The TX and RX modules can be purchased directly off-the-shelf or custom-designed (Supplementary Table 2). Using commercially available chips with communication protocols such as Bluetooth low energy, Zigbee, long range radio and medical implant communication system allows compatibility with existing devices. Still, they are typically not optimized for a target application in terms of power consumption and area. Several custom integrated circuit topologies have been proposed in the literature that target minimizing the power consumption and area and maximizing the data rate and communication distance133,134,135,136,137. It is also essential to ensure the precise frequency tuning and stability over different process, voltage and temperature variations. One way of achieving this is by incorporating the crystal oscillator, which comes at the cost of extra area. A recently proposed crystal-less wireless transceiver for volume-constrained insertable pills tackles all these challenges by consuming only several milliwatts of power, achieving a 200 kb s−1 data rate at 5 m communication distance132.
An alternative way to communicate with the external reader is to rely on body channel communication, which utilizes the human body as a communication medium. Pills employing body channel communication offer many benefits including lower channel attenuation, higher data rates, lower power consumption and smaller form factor as it requires an electrode instead of an antenna for communication54,138,139. Owing to the low propagation of sound waves in soft tissues (~1 dB cm−1 MHz−1), the ultrasonic modality has also been utilized for communicating with ingestible devices with up to a 100 kb s−1 data rate at 8.5 cm depth while consuming less than 200 μW (refs. 140,141,142). The minor disadvantage of these methods is that the external electrode or ultrasonic transducer must be in contact with the skin, necessitating the patient to wear a patch with all the electronics constantly. Due to the transparency of the human body to magnetic fields, a static magnetic field generated by an electromagnet can be utilized to interact with ingestible devices133. In this modality, the communication range is not limited by the device’s location inside the body but rather by the sensitivity of the magnetic sensor and the magnitude of the applied magnetic field. Similarly, this method requires a patient to wear a compact patch with a planar electromagnet.
As an example from Supplementary Table 2, we can compare the commercial 400 MHz ZL70102 and custom 915 MHz TRX143. The power consumption of the custom TRX is approximately 75 times less than that of the ZL70102, largely because it radiates a signal with 24 dB lower strength (around 250 times lower in linear scale). This raises the question of whether radiating a power of −3 dBm is necessary. If we consider an ingestible device to be 10 cm deep in the body, the path loss for a 400 MHz carrier signal would be 30 dB, while for 915 MHz it would be 60 dB. This means that the ZL70102 would deliver a signal strength of −33 dBm, while the custom TRX would deliver −87 dBm to the base station that resides outside the body. As external receivers can typically detect signals as low as −100 dBm, the signal delivered by the custom TRX is sufficient for detection, and there is no need to waste more power to radiate signals with higher strength. Another factor to consider is the area, as the custom TRX occupies five times less area and requires only an external antenna to be connected to the circuitry, while the ZL70102 needs a matching network and crystal, which further increases the overall size of the TRX. The data rate required for a particular application depends heavily on the nature of that application. For example, capsule endoscopy typically requires a data rate above 1 Mb s−1, while pills equipped with electrochemical or optical sensors may only require a data rate in the tens of kilobits per second.
Power
The power source is one of the most crucial elements determining the operation life of the ingestible device. When choosing a power source for ingestibles, the primary considerations are (1) volumetric capacity (μAh mm−3), (2) size and (3) safety. Figure 5 and Supplementary Table 3 show various power sources, namely, batteries (silver oxide, lithium ion, flexible, solid state, and transient), wireless power transfer (acoustic and RF) and electrochemical galvanic cells, are compared. Usually, onboard batteries are utilized because most capsules require reliable, stable electrical power. However, batteries occupy a large volume and determine the device’s size, which increases the risk of its retention in the GI tract. Standard lithium-ion batteries have high electrical capacity but are susceptible to thermal runaway, explosion and toxic electrolyte leakage144. Silver-oxide batteries, which are not prone to thermal runaway but still contain toxic metals and caustic electrolytes, are preferred as an onboard power source and the only type of battery approved for clinical use to power capsules endoscopes145,146. Solid-state batteries are also attractive due to their reduced risk of thermal runaway, flammability and leakages147. Transient batteries made from biodegradable materials may eliminate the risks associated with toxicity and minimize GI obstruction through partial or complete decomposition. However, they have much lower capacity than traditional batteries, typically thousands of times smaller148,149,150. Similarly, flexible batteries made from biocompatible materials provide another option to minimize the capsule’s volume151,152. Ingestible devices can also benefit from new technologies such as fully 3D-printed batteries made from disposable papers153 and gel-based micro-batteries consisting of organic and organometallic molecules154. Most of the regular coin cells, and some solid-state and flexible batteries, can be easily purchased off-the-shelf. However, transient and most solid-state and flexible batteries remain part of ongoing research studies.
Batteries (silver oxide, lithium ion, flexible, solid state, and transient), wireless power transfer (acoustic and RF) and electrochemical galvanic cells are compared in terms of volumetric capacity (μAh mm−3), size and safety. Silver-oxide batteries are preferred as an onboard power source and the only type of battery approved for clinical use to power ingestibles.
Energy harvesting in the GI tract is another way of powering ingestible devices. For instance, flexible piezoelectric materials can be used to sense GI motility and power onboard electronics71. Triboelectric energy harvesting is another method demonstrated in ingestible devices121,155. Galvanic cells have also been used to power ingestible capsules using gastric acid as an electrolyte156, including clinically approved Proteus Digital (Mg–CuCl couple)55 and EtectRx (MgCl–AgCl couple)56 medication adherence capsules. Also, nutrients such as glucose54 and microorganisms in the gut157,158 can be exploited for submilliwatt-level power generation. The transducers for these energy-harvesting methods are typically custom-designed and optimized for the target pill specifications. The disadvantage of these energy-harvesting techniques is their unreliability as they may not be able to generate power continuously for long measurements due to a lack of glucose, gastric juice or GI muscle contractions.
Remote powering of ingestible devices is also possible using acoustic140,141,142,159 and RF96,160 power transfer. Due to the low propagation loss of sound waves, the first method can deliver several milliwatts of power with the implant placed under 6 cm of animal tissue. Regarding RF power transfer, in vivo experiments in pigs have shown the feasibility of this method delivering hundreds of microwatts to the implanted device. These numbers may be affected by frequency-dependent path loss, antenna size and orientation of the device in the GI tract. When utilizing this power delivery method, it is essential to ensure that the specific absorption rate values are lower than the standard provided by the Institute of Electrical and Electronics Engineers (the standard limit for 1 g of tissue is 1.6 W kg−1 for an input power of 1 W)161. The piezoelectric materials and circuits that convert an a.c. signal from the external station to the stable d.c. voltage rail are available off-the-shelf, and they can be integrated into the pill.
Packaging
The US FDA outlines health risks linked to ingestible electronic pills, emphasizing biocompatibility, electrical and mechanical safety, functional reliability, structural integrity, intestinal obstruction, and injury. To address these concerns, the FDA developed an act with a specific set of controls that would reasonably ensure the safety and effectiveness of these devices for experiments with animals and humans162,163. On the basis of the aforementioned risks, the packaging of such ingestible capsules becomes exceptionally vital. To adhere to regulations, the encapsulation of an ingestible pill must be made from biocompatible materials and remain sealed in the harsh environment of the GI tract. Also, it must be robust to retain its shape during the peristaltic movement of the GI passage. Polydimethylsiloxane and polyether ether ketone are most often utilized as the pill’s external coating due to their biocompatibility and sturdiness after being cured49,64,113,119. It is also possible to 3D-print the shell from biocompatible resin and directly use it as an encapsulation79,113. If there is a need to collect certain chemicals or gases in the GI tract, small openings that are isolated from toxic electronic parts or semi-permeable membranes are used to interface with the GI environment49,54,63.
The size and the shape are important parameters of an ingestible pill. The largest standard capsule (000) has a diameter of 9.91 mm and a length of 26 mm, considered the largest reference geometry when developing ingestible electronics4. Typically, big capsules allow more functional components but also cause device retention, which might result in obstruction of GI tract. Statistical analysis of 402 studies about capsule endoscopy (the size of which is typically close to 000 capsules) procedures revealed that retention occurred in 1,096 out of 86,742 cases (0.73%). The definite reasons for retention were reported in 610 procedures according to 119 studies, where Crohn’s disease accounts for most cases (216, 35.41%)164. Sometimes the capsule can be retrieved naturally with additional medical prescriptions165. However, depending on the retention site, endoscopic intervention and medical surgery may be required164,166.
Possible solutions to avoid retention risks include minimizing the capsule dimensions and using partially or fully biodegradable components. Because the former option may have specific limitations dictated by the size of the battery or other components, the second solution has been actively investigated in recent years, offering a variety of edible and biodegradable biosensors53,66, biodegradable66 and flexible167,168 antennas, transient148,153,169 and flexible152,170 batteries, and other structural parts96,110,171,172 of the ingestible device.
Localization
An accurate knowledge of the position and orientation of the ingestible pill along the GI tract is crucial because it would reveal the measurement location recorded by a sensing unit, which could indicate the site of a tumour, bleeding or other essential markers in the gut. Moreover, knowing the location and orientation of the pill would help in the case of wireless power transfer to the device as it allows tuning the location, orientation or power radiated by an external base station173,174. Several localization techniques have been developed, particularly for ingestible pills, and techniques have been proposed for general implantable devices that could be adopted for ingestibles as well. Figure 6 and Supplementary Table 4 provide a summary of reported localization techniques and their benefits and demerits.
a, Localization based on medical and radiological imaging such as MRI, CT, X-ray, fluoroscopy and ultrasound techniques. b, Localization based on environmental markers. GI tract organs have distinct oxygen and pH concentrations. Hence partial pressure of oxygen (\(p_{{{\mathrm{O}}_{2}}}\)) and pH can be used for localization. c, Triangulation by using RF, ultrasound or magnetic field generated by the ingestible. The signal strength received by external receivers is used calculated path loss from which the location can be inferred. d, The magnetic-field-based localization technique uses bidirectional communication and magnetic-field strength measured by the ingestible for triangulation.
The most straightforward approach to locating the ingestible inside the body is to use medical and radiological imaging, such as MRI, computerized tomography (CT), ultrasound, X-ray, fluoroscopy or gamma-ray techniques (Fig. 6a). Even though these methods can achieve high accuracy (as low as 100–200 μm; ref. 175), the imaging process can be time-consuming, requires bulky and expensive equipment, and can cause an undesired high level of radiation exposure to the patient. Another method to locate the ingestible device is by using the GI tract’s physical parameters that change from one region of the gut to another (Fig. 6b). For example, GI tract organs have different oxygen levels, temperature profiles and pH concentrations176. Therefore, oxygen and pH sensors can be embedded into capsules for accurately identifying the passage from one organ to another8. Even though this method does not require any external elements, it can only say in which organ the capsule is located at a particular moment.
The RF transmitter used to send the data from the pill to the external reader can also be utilized for localization purposes (Fig. 6c). One of the methods is to use the signal strength received by external antennas and to use path-loss models to estimate the ingestible’s location, achieving 5 cm accuracy177. A time-of-flight algorithm based on a zero transmission power backscatter communication can also be utilized to predict the ingestible’s location with 1.4 cm accuracy178. Overall, these RF-based methods suffer from uncertain signal propagation velocities, path-loss parameters and strong absorption of human tissue, which results in moderate centimetre-scale localization accuracy. An ultrasound-based method is another technique where the capsule’s position is estimated using the time-of-flight measurements between the ultrasonic signals transmitted from an external source mounted on the patient’s body and the signals reflected by the implant179,180. As ultrasound’s propagation loss is less than RF in soft tissues and internal organs, this approach can achieve submillimetre accuracy174. Another magnetic-field-based localization technique utilizes a permanent magnet placed with the capsule (Fig. 6c). An array of external magnetic sensors measure the magnetic field coming from the GI tract and decodes the capsule’s location181,182. The advantage of magnetic-field-based localization is that low-frequency magnetic fields can run through the body with reduced attenuation as the body’s tissues are non-magnetic. An accuracy of 1.8 mm can be achieved, but further improvements of this method are limited by environmental interference, such as Earth’s magnetic field182. Moreover, placing a magnet inside the human body may pose health risks. For example, multiple magnets on different sides can attach together and burrow through the tissue to create a perforation.
Another magnetic-field-based method relies on the magnetic fields generated by external electromagnets that uniquely encode each spatial point in the field of view183,184,185,186 (Fig. 6d). The magnetic sensor placed in the capsule measures the local magnetic field and then transmits its value wirelessly to the external reader. On the basis of that value and by exactly knowing the magnetic field at a given point, the location of the capsule can be decoded. The advantage of this method is its low-power implementation and small-area requirements of the capsule, while achieving 1.5 mm resolution186. The potential drawback of this method is the need for external power-hungry magnetic coils with sufficient field of view, which may also limit the patient’s movement. Another magnetic localization approach scales the frequency of the excitation coils up to 2 MHz, which allows them to be miniaturized and resonated with high quality factors, boosting the sensitivity and power efficiency of the system by several orders of magnitude, and achieving 920 μm resolution, the highest accuracy among all methods mentioned above184,185.
Locomotion
Typically, ingestible capsules do not have the functionality to independently control their movement, which limits their ability to target specific locations along the GI tract. Different steering approaches are being explored in mechanical, electrical and magnetic modalities to overcome this limitation. Mechanical techniques generally require an onboard motor to actuate parts such as a hydrodynamic propeller187,188, spring-type shape-memory alloys189,190 and robotic legs191,192, which produces propulsive, crawling or walking movements, respectively. Electrical stimulation of the intestinal wall can cause local muscular contraction and propel the capsule along the lumen. In vivo and ex vivo experiments in pigs have shown that, with stimulation current values exceeding a certain threshold (tens of milliamperes), the device could reliably move in both forwards and backwards directions193,194. These methods do not require sophisticated external components but only a wireless link with the capsule to control its motion. However, the power consumed by motors is in the order of hundreds of milliwatts, and electrical stimulation requires tens of milliamperes of current, necessitating the battery’s high capacity that subsequently increases the capsule’s size. Heat dissipation is another concern that must be considered with such power levels. Due to safety issues, none of these methods has been tested on human volunteers.
Ingestible capsules equipped with permanent magnets or a magnetic shell can be steered with external magnetic fields created by another permanent magnet or electromagnet such as a Helmholtz coil73,74,75,76,110. Three main advantages of magnetic locomotion are no onboard power consumption, complete control over capsule’s axial and rotational movements, and direct applicability to any capsule with no functional modifications. This method has been successfully tested in clinical trials with no adverse events reported by participants195,196.
Design guidelines
In this section, two examples of ingestible pills are discussed: a camera-based ingestible pill with an onboard AI accelerator and an optical-sensing ingestible pill with 3D magnetic localization. We delve deeper into the design process by discussing the rationale behind component selection for each of the two example pills. We explain how these component choices impact various aspects of the device, such as size, sensing capabilities, processing power and energy consumption. In addition, in Fig. 7, we provide a visual representation of the pill’s stack-up, listing the possible components that can be utilized in the prototype. To enhance clarity, the selected components in the given examples are highlighted in bold font. Here, we aim to provide a more practical and actionable guide to designing ingestible devices by offering step-by-step design guidance.
Camera-based ingestible pill with onboard AI accelerator
The application of this pill is the visual inspection of the GI tract with onboard image classification for detecting GI abnormalities such as bleeding or polyps30. The main components of the pill are a camera, an MCU with AI capabilities, a power management unit, a transceiver, batteries and encapsulation. The components that are selected first are the camera, MCU and transceiver as they will eventually define the dimension constraints and power consumption of the whole system. On the basis of existing off-the-shelf complementary metal–oxide–semiconductor cameras, multiple options are available, with OV7670 being the most compact and power-efficient option. This component consumes approximately 18 mA of current in the active state and requires 2.8 V and 1.8 V power rails. Similarly, MAX78000 from Maxim Integrated is a compact and low-power solution for an MCU with an AI accelerator, consuming 1 mA in active state with a power supply of 1.8 V. As this pill is similar to a capsule endoscope, a 400 MHz ZL70102 chip is selected as a transceiver, which consumes 5.3 mA of current during the data transfer, less than 1 μA in sleep mode, and requires a 2.8 V supply voltage. At this point, we conclude that 2 supply rails are required to power the components: 1.8 V and 2.8 V. To generate these power rails directly from a battery or d.c.–d.c. converter, we need a low dropout regulator (LDO). Among various LDOs available off-the-shelf, we selected two S-1318D LDOs from Ablic as this particular part consumes only 95 nA of quiescent current and has an area of 1 mm × 1 mm. Each LDO generates 1.8 V and 2.8 V, respectively. As this pill consumes tens of milliwatts during the measurements, a battery is used as a power source due to its capability to deliver this level of power. Three silver-oxide batteries (SR721) are connected in series resulting in 4.6 V of output voltage with 29 mAh of total capacitance. Although regulating 4.6 V down to 1.8 V and 2.8 V is not the most efficient solution, this approach eliminates the use of a d.c.–d.c. converter, thus, saving more power. If we assume that the camera performs measurement for 1 s at 30 frames per second, then the MCU analyses the data for the next 10 ms, and then the transceiver sends out the data for 10 ms and everything is repeated every 2 s, the average current consumption of the whole system would approximately be 6 mA. With the given battery capacitance, the total battery life would be 4.8 hours. To further improve the battery life without increasing the number of batteries, the frame rate of the camera and MCU clock frequency can be reduced, and the period of this measurement sequence can be increased. The encapsulation of this pill consists of two parts: a 3D-printed shell made from biocompatible resin and a transparent glass dome. The diameter of the pill is approximately 15 mm and the length is 30 mm. As of now, the prototype is bigger than the standard 000 capsules with the camera being the bottleneck for the pill’s diameter.
Optical-sensing ingestible pill with 3D magnetic localization
The goal of this pill is to sense different biomarkers present in the GI tract by exciting the sensing element with an LED and recording its reflection or sensing element’s luminescence with the photodiode37,38,39,197. Also, this pill employs a magnetic-field-gradient-based localization: it uses a 3D magnetic sensor to measure the magnetic field in its proximity and then transmits this information to the external reader that decodes its location based on these values186. The electronic components of the pill are an optical sensor with integrated LEDs and photodiode, an MCU, a magnetic sensor, a transceiver, a power management unit and a battery. Among commercially available optical sensors, MAX86916 from Maxim Integrated is one of the most appealing options as it integrates four different LEDs (blue, green, red, infrared) and a wideband photodiode in a single package. Moreover, it has built-in LED drivers and photodiode readout circuitry along with an ADC converter. It consumes 0.5 mA of current during the measurement, requires a supply voltage of 1.8 V for electronics and 5 V for LEDs, and comes in a compact 3.5 mm × 7.0 mm × 1.5 mm package. When it comes to the MCU and transceiver, nRF5340 (BMD-350) was selected as it integrates both of these elements in a single package, and has better specifications in terms of power compared with its alternatives (Supplementary Table 2). It utilizes Bluetooth low energy and the data can directly be transmitted to the mobile device. nRF5340 consumes 3.2 mA of current during the data transfer and uses a 1.8 V supply voltage. The 3D magnetic sensor selected for this pill is MMC5633NJL from MEMSIC, which occupies only 0.85 mm × 0.85 mm of area and consumes 7 μA per measurement. With the given components, 2 supply rails of 1.8 V and 5 V are needed. Instead of using two separate LDOs, the low-power S-1200 LDO with dual output (1.8 V and 5 V) from Ablic is selected. It consumes 18 μA of current and occupies 1.6 mm × 1.6 mm of area. Instead of stacking 4 silver-oxide batteries in series to output 6.2 V, it is better in terms of volume to use a d.c.–d.c. converter to boost the voltage of one or two batteries connected in series to 5.2 V and then regulate it to the desired 5 V and 1.8 V using LDOs. Among various d.c.–d.c. converter options, XCL100 from Torex is selected as it has a low quiescent current of 7 μA, incorporates an integrated inductor and has a volume of 2.5 mm × 2 mm × 1 mm. Two silver-oxide batteries (SR626) connected in series are utilized, resulting in 3.1 V output voltage and 28 mAh capacitance. As mentioned before, the battery is connected to the input of a d.c.–d.c. converter. Assuming that the optical sensor performs measurement for 1 ms and the LED consumes 10 mA during that time, then the magnetic sensor measures the magnetic field for the next 50 ms, nRF53 transmits the data during the next 0.1 ms and all these steps are repeated every second, it results in 1.75 mA of average current consumption. With the given battery capacitance, the pill would theoretically operate for 16 hours. Similar to the previous example, the pill is covered with a 3D-printed encapsulation made from biocompatible resin. The total dimensions of the pill are 9.8 mm × 26 mm, which is slightly smaller than the standard 000 pill.
Outlook
Ingestible electronics offer a non-invasive solution to diagnose and treat different diseases in the GI tract, and thus considerable growth in the technology can be expected in the coming years. However, several challenges lie ahead. Safety issues (such as GI obstruction), the complexity of clinical trials and cost are limitations that slow the wider application of the technology. Miniaturization and development of transient electronic components, including sensors and batteries, could solve device retention and GI obstruction issues. Furthermore, this would ease some patients’ hesitation and fear of swallowing an electronic device. The inter-person variability of GI tract physiology and disease pathophysiology requires careful planning and a broad spectrum of volunteer participants, making it more complex, expensive and time-consuming. As Otsuka Pharmaceutical and Atmo Biosciences have demonstrated, ingestible capsules offer remote monitoring capabilities, allowing autonomous data collection without the presence of a physician. Once the safety profiles of such devices are improved, the diagnostics and monitoring of the GI tract in real time would be possible from the comfort of home.
Currently, most ingestible capsules that are used for sensing focus on measuring general biomarkers (such as pH, temperature, pressure, bleeding and gases) and only a few sensors have been developed to detect specific bacteria present in the gut microbiome. However, the colonic bacterial community is diverse, so it is crucial to develop sensors capable of detecting different bacteria, which could provide valuable information. For example, individuals with neurodegenerative disorders such as Alzheimer’s and Parkinson’s diseases have been found to have lower levels of Bifidobacterium and Lactobacillus and higher levels of inflammatory bacteria such as Desulfovibrio198. Alternatively, higher levels of Bacteroides fragilis and Lactobacillus reuteri have been linked to improved symptoms of autism spectrum disorder199. Many other bacteria in the gut may be associated with different GI and CNS diseases, and thus it is essential to develop ingestible sensors that can record a variety of different bacteria present in the gut.
Sensing has been the main application of ingestible pills, but the technology can be used in a variety of therapeutic procedures, including targeted drug delivery, ultrasonic treatment of colorectal cancer and electrical stimulation-based treatment of GI motility disorders. In such applications, control over the pill’s movement with high precision is vital. Magnetic manipulation of ingestible capsules offers the most straightforward option to steer the device, but it requires bulky external components such as an electromagnet or permanent magnet. Self-sustained leg-based locomotion, which currently suffers from high power requirements (hundreds of milliwatts), would be the most convenient option for both patient and physician. Therefore, the therapeutic direction of ingestibles would directly benefit from miniature and ultralow power implementation of self-sustained locomotion.
Another important aspect of ingestible electronics is privacy. Ingestible pills transmit personal health data wirelessly, and there is a risk that these data could be intercepted or misused. Thus, it is important that distributors of ingestible electronic pills implement robust security measures to protect patient privacy. This includes secure data transmission, encryption and protection against unauthorized access. From the perspective of electronic hardware, it would also be beneficial to reduce the size and power consumption of some secondary components. For example, optimizing RF transceivers to achieve submilliwatt power consumption would increase battery life. Similarly, integrating the components used for reading out the sensor data, localization and power management in a single chip would reduce the area and, therefore, the overall volume of the capsules.
Ingestible electronic pills can potentially be used to unravel different phenomena underlying various GI, ENS and CNS disorders. The devices could also play a key role in the development of personalized medicine, as treatments can be customized according to an individual’s unique microbiome profile. With the possibility of scaling up production and reducing manufacturing costs, ingestible pills could serve as a more accessible alternative for people in various regions who do not have access to expensive clinical equipment used for diagnosis and treatment. But to achieve this application potential, continued advancements in various areas of pill design will be needed, including developing various sensors, decreasing power consumption, creating more reliable powering options, minimizing dimensions and enhancing safety measures.
References
Jacobson, B. & Mackay, R. S. A pH-endoradiosonde. Lancet 269, 1224 (1957).
Farrar, J. T., Zworykin, V. K. & Baum, J. Pressure-sensitive telemetering capsule for study of gastrointestinal motility. Science 126, 975–976 (1957).
Iddan, G., Meron, G., Glukhovsky, A. & Swain, P. Wireless capsule endoscopy. Nature 405, 417–417 (2000).
Steiger, C. et al. Ingestible electronics for diagnostics and therapy. Nat. Rev. Mater. 4, 83–98 (2019).
Litvinova, O. et al. Digital pills with ingestible sensors: patent landscape analysis. Pharmaceuticals 15, 1025 (2022).
Miley, D. et al. Video capsule endoscopy and ingestible electronics: emerging trends in sensors, circuits, materials, telemetry, optics, and rapid reading software. Adv. Devices Instrum. 2021, 9854040 (2021).
Smart Pills Market by Application (Capsule Endoscopy, Drug Delivery, Patient Monitoring), Target Area (Esophagus, Small Intestine, Large Intestine, Stomach), End User (Hospitals, Diagnostic Centers) & Region—Global Forecast to 2028 (Markets and Markets, 2023); https://www.marketsandmarkets.com/Market-Reports/smart-pill-technology-market-840.html
Kalantar-Zadeh, K., Ha, N., Ou, J. Z. & Berean, K. J. Ingestible sensors. ACS Sensors 2, 468–483 (2017).
Beardslee, L. A. et al. Ingestible sensors and sensing systems for minimally invasive diagnosis and monitoring: the next frontier in minimally invasive screening. ACS Sensors 5, 891–910 (2020).
Cummins, G. Smart pills for gastrointestinal diagnostics and therapy. Adv. Drug Deliv. Rev. 177, 113931 (2021).
Browning, K. N. & Travagli, R. A. Central nervous system control of gastrointestinal motility and secretion and modulation of gastrointestinal functions. Compr. Physiol. 4, 1339 (2014).
Dieterich, W., Schink, M. & Zopf, Y. Microbiota in the gastrointestinal tract. Med. Sci. 6, 116 (2018).
Sensoy, I. A review on the food digestion in the digestive tract and the used in vitro models. Curr. Res. Food Sci. 4, 308–319 (2021).
Tsang, K. W. & Lam, S.-K. Helicobacter pylori and extra-digestive diseases. J. Gastroenterol. Hepatol. 14, 844–850 (1999).
Montoro-Huguet, M. A., Belloc, B. & Domínguez-Cajal, M. Small and large intestine (I): malabsorption of nutrients. Nutrients 13, 1254 (2021).
Tong, J. W. V., Lingam, P. & Shelat, V. G. Adhesive small bowel obstruction—an update. Acute Med. Surg. 7, e587 (2020).
Qin, J. et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464, 59–65 (2010).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559–563 (2014).
Luna, R. A. et al. Distinct microbiome–neuroimmune signatures correlate with functional abdominal pain in children with autism spectrum disorder. Cell. Mol. Gastroenterol. Hepatol. 3, 218–230 (2017).
Chandra, S. et al. Healthy gut, healthy brain: the gut microbiome in neurodegenerative disorders. Curr. Top. Med. Chem. 20, 1142–1153 (2020).
Fan, Y. & Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 19, 55–71 (2021).
Stearns, J. et al. Bacterial biogeography of the human digestive tract. Sci. Rep. 1, 170 (2011).
Lavelle, A. & Sokol, H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 17, 223–237 (2020).
Kalantar-Zadeh, K., Berean, K. J., Burgell, R. E., Muir, J. G. & Gibson, P. R. Intestinal gases: influence on gut disorders and the role of dietary manipulations. Nat. Rev. Gastroenterol. Hepatol. 16, 733–747 (2019).
Dave, L. A., Montoya, C. A., Rutherfurd, S. M. & Moughan, P. J. Gastrointestinal endogenous proteins as a source of bioactive peptides-an in silico study. PLoS ONE 9, e98922 (2014).
Yang, X. et al. Pathophysiologic role of neurotransmitters in digestive diseases. Front. Physiol. 12, 567650 (2021).
Atsawarungruangkit, A., Elfanagely, Y., Asombang, A. W., Rupawala, A. & Rich, H. G. Understanding deep learning in capsule endoscopy: can artificial intelligence enhance clinical practice? Artif. Intell. Gastrointest. Endosc. 1, 33–43 (2020).
Nadimi, E. S. et al. Application of deep learning for autonomous detection and localization of colorectal polyps in wireless colon capsule endoscopy. Comput. Electr. Eng. 81, 106531 (2020).
Moen, S., Vuik, F. E., Kuipers, E. J. & Spaander, M. C. Artificial intelligence in colon capsule endoscopy—a systematic review. Diagnostics 12, 1994 (2022).
Sahafi, A. et al. Edge artificial intelligence wireless video capsule endoscopy. Sci. Rep. 12, 13723 (2022).
Raza, W. Gastroscopic image processing—OpenMV Cam H7. Edge Impulse https://docs.edgeimpulse.com/experts/prototype-and-concept-projects/tinyml-gastroscopic-image-processing (2023).
Qiu, Y. et al. Ultrasound capsule endoscopy with a mechanically scanning micro-ultrasound: a porcine study. Ultrasound Med. Biol. 46, 796–804 (2020).
Kimchy, Y. et al. Radiographic capsule-based system for non-cathartic colorectal cancer screening. Abdom. Radiol. 42, 1291–1297 (2016).
Gluck, N. et al. Novel prep-less X-ray imaging capsule for colon cancer screening: a feasibility study. Gut 68, 774–775 (2019).
Tabatabaei, N. et al. Tethered confocal endomicroscopy capsule for diagnosis and monitoring of eosinophilic esophagitis. Biomed. Opt. Express 5, 197–207 (2014).
Gora, M. J. et al. Tethered capsule endomicroscopy enables less invasive imaging of gastrointestinal tract microstructure. Nat. Med. 19, 238–240 (2013).
Qiao, P., Liu, H., Yan, X., Jia, Z. & Pi, X. A smart capsule system for automated detection of intestinal bleeding using HSL color recognition. PLoS ONE 11, e0166488 (2016).
Schostek, S. et al. Volunteer case series of a new telemetric sensor for blood detection in the upper gastrointestinal tract: the hemopill. Dig. Dis. Sci. 61, 2956–2962 (2016).
Demosthenous, P., Pitris, C. & Georgiou, J. Infrared fluorescence-based cancer screening capsule for the small intestine. IEEE Trans. Biomed. Circuits Syst. 10, 467–476 (2016).
Zhu, C., Wen, Y., Liu, T., Yang, H. & Sengupta, K. A packaged ingestible bio-pill with 15-pixel multiplexed fluorescence nucleic-acid sensor and bi-directional wireless interface for in-vivo bio-molecular sensing. In 2020 IEEE Symposium on VLSI Circuits 1–2 (IEEE, 2020).
Singh, S. et al. Sa1717—development of a swallowable diagnostic capsule to monitor gastrointestinal health. Gastroenterology 156, S-376 (2019).
Manickam, A. et al. A fully integrated CMOS fluorescence biochip for DNA and RNA testing. IEEE J. Solid State Circuits 52, 2857–2870 (2017).
Machida, T. A study of intragastric pH in patients with peptic ulcer—with special reference to the clinical significance of basal pH value. Gastroenterol. Jpn. 16, 447–458 (1981).
Press, A. et al. Gastrointestinal pH profiles in patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 12, 673–678 (1998).
Maurer, J. M. et al. Gastrointestinal ph and transit time profiling in healthy volunteers using the intellicap system confirms ileo-colonic release of colopulse tablets. PLoS ONE 10, e0129076 (2015).
Arefin, M. S., Redouté, J.-M. & Yuce, M. R. Integration of low-power ASIC and mems sensors for monitoring gastrointestinal tract using a wireless capsule system. IEEE J. Biomed. Health Inform. 22, 87–97 (2017).
Cheng, C. et al. A wireless, ingestible pH sensing capsule system based on iridium oxide for monitoring gastrointestinal health. Sens. Actuators B 349, 130781 (2021).
Hasler, W. L. The use of smartpill for gastric monitoring. Expert Rev. Gastroenterol. Hepatol. 8, 587–600 (2014).
Caffrey, C. M., Twomey, K. & Ogurtsov, V. Development of a wireless swallowable capsule with potentiostatic electrochemical sensor for gastrointestinal track investigation. Sens. Actuators B 218, 8–15 (2015).
Salama, R., Arshavsky-Graham, S., Sella-Tavor, O., Massad-Ivanir, N. & Segal, E. Design considerations of aptasensors for continuous monitoring of biomarkers in digestive tract fluids. Talanta 239, 123124 (2022).
Li, J. et al. A tissue-like neurotransmitter sensor for the brain and gut. Nature 606, 94–101 (2022).
Kim, J. et al. Edible electrochemistry: food materials based electrochemical sensors. Adv. Healthc. Mater. 6, 1700770 (2017).
Montiel, V. et al. Direct electrochemical biosensing in gastrointestinal fluids. Anal. Bioanal. Chem. 411, 4597–4604 (2019).
De la Paz, E. et al. A self-powered ingestible wireless biosensing system for real-time in situ monitoring of gastrointestinal tract metabolites. Nat. Commun. 13, 7405 (2022).
Hafezi, H. et al. An ingestible sensor for measuring medication adherence. IEEE Trans. Biomed. Eng. 62, 99–109 (2015).
Flores, G. P. et al. Performance, reliability, usability, and safety of the ID-Cap system for ingestion event monitoring in healthy volunteers: a pilot study. Innov. Clin. Neurosci. 13, 12–19 (2016).
Chai, P. R. et al. Ingestible electronic sensors to measure instantaneous medication adherence: a narrative review. Digit. Health 8, 20552076221083119 (2022).
Ghoreishizadeh, S. S., Taurino, I., De Micheli, G., Carrara, S. & Georgiou, P. A differential electrochemical readout asic with heterogeneous integration of bio-nano sensors for amperometric sensing. IEEE Trans. Biomed. Circuits Syst. 11, 1148–1159 (2017).
Herstein, J. J. et al. A pilot study of core body temperatures in healthcare workers wearing personal protective equipment in a high-level isolation unit. J. Occup. Environ. Hyg. 18, 430–435 (2021).
O’Brien, C., Hoyt, R. W., Buller, M. J., Castellani, J. W. & Young, A. J. Telemetry pill measurement of core temperature in humans during active heating and cooling. Med. Sci. Sports Exerc. 30, 468–472 (1998).
West, M. R., Costello, S., Sol, J. A. & Domitrovich, J. W. Risk for heat-related illness among wildland firefighters: job tasks and core body temperature change. Occup. Environ. Med. 77, 433–438 (2020).
Monnard, C. R. et al. Issues in continuous 24-h core body temperature monitoring in humans using an ingestible capsule telemetric sensor. Front. Endocrinol. 8, 130 (2017).
Kalantar-Zadeh, K. et al. A human pilot trial of ingestible electronic capsules capable of sensing different gases in the gut. Nat. Electron. 1, 79–87 (2018).
Mimee, M. et al. An ingestible bacterial-electronic system to monitor gastrointestinal health. Science 360, 915–918 (2018).
Inda-Webb, M. et al. Sub-1.4 cm3 capsule for detecting labile inflammatory biomarkers in situ. Nature 620, 386–392 (2023).
Inami, A., Kan, T. & Onoe, H. Ingestible wireless capsule sensor made from edible materials for gut bacteria monitoring. In 2022 IEEE 35th International Conference on Micro Electro Mechanical Systems Conference (MEMS) 110–113 (IEEE, 2022).
Guozheng, Y., Biao, H. & Peng, Z. Design of battery-less and real-time telemetry system for gastrointestinal applications. In 2007 IEEE International Conference on Control and Automation 245–249 (IEEE, 2007).
Liao, C.-H. et al. An ingestible electronics for continuous and real-time intraabdominal pressure monitoring. J. Pers. Med. 11, 12 (2020).
Beardslee, L. A. et al. Blast capsule: an embedded pressure sensing system for internal blast pressure measurement. IEEE Sens. Lett. 5, 1–4 (2021).
Yunus, N. A. M., Halin, I. A., Sulaiman, N., Ismail, N. F. & Sheng, O. K. Valuation on MEMS pressure sensors and device applications. Int. J. Electron. Commun. Eng. 9, 834–842 (2015).
Dagdeviren, C. et al. Flexible piezoelectric devices for gastrointestinal motility sensing. Nat. Biomed. Eng. 1, 807–817 (2017).
Dileena, L., Sreeja, S. B. & Sreekala, C. A comparative study on piezoelectric and piezoresistive pressure sensor using comsol simulation. Mater. Today Proc. 46, 3121–3126 (2021).
Hoang, M. C. et al. A robotic biopsy endoscope with magnetic 5-DOF locomotion and a retractable biopsy punch. Micromachines 11, 98 (2020).
Son, D., Gilbert, H. & Sitti, M. Magnetically actuated soft capsule endoscope for fine-needle biopsy. Soft Robot. 7, 10–21 (2020).
Yim, S., Gultepe, E., Gracias, D. H. & Sitti, M. Biopsy using a magnetic capsule endoscope carrying, releasing, and retrieving untethered microgrippers. IEEE Trans. Biomed. Eng. 61, 513–521 (2014).
Hoang, M. C. et al. Untethered robotic motion and rotating blade mechanism for actively locomotive biopsy capsule endoscope. IEEE Access 7, 93364–93374 (2019).
Finocchiaro, M. et al. Design of a magnetic actuation system for a microbiota-collection ingestible capsule. In 2021 IEEE International Conference on Robotics and Automation (ICRA) 6905–6911 (IEEE, 2021).
Waimin, J. F. et al. Smart capsule for non-invasive sampling and studying of the gastrointestinal microbiome. RSC Adv. 10, 16313–16322 (2020).
Rezaei Nejad, H. et al. Ingestible osmotic pill for in vivo sampling of gut microbiomes. Adv. Intell. Syst. 1, 1900053 (2019).
Chen, L., Gruzinskyte, L., Jørgensen, S. L., Boisen, A. & Srivastava, S. K. An ingestible self-polymerizing system for targeted sampling of gut microbiota and biomarkers. ACS Nano 14, 12072–12081 (2020).
Shalon, D. et al. Profiling the human intestinal environment under physiological conditions. Nature 617, 581–591 (2023).
Kong, K., Yim, S., Choi, S. & Jeon, D. A robotic biopsy device for capsule endoscopy. J. Med. Devices 6, 031004 (2012).
Durán-Lobato, M., Niu, Z. & Alonso, M. J. Oral delivery of biologics for precision medicine. Adv. Mater. 32, 1901935 (2020).
Castro, R., Libânio, D., Pita, I. & Dinis-Ribeiro, M. Solutions for submucosal injection: what to choose and how to do it. World J. Gastroenterol. 25, 777 (2019).
Yamaguchi, D. et al. Colorectal endoscopic mucosal resection with submucosal injection of epinephrine versus hypertonic saline in patients taking antithrombotic agents: propensity-score-matching analysis. BMC Gastroenterol. 19, 1 (2019).
Traverso, G. et al. Microneedles for drug delivery via the gastrointestinal tract. J. Pharm. Sci. 104, 362–367 (2015).
Abramson, A. et al. An ingestible self-orienting system for oral delivery of macromolecules. Science 363, 611–615 (2019).
Abramson, A. et al. Oral delivery of systemic monoclonal antibodies, peptides and small molecules using gastric auto-injectors. Nat. Biotechnol. 40, 103–109 (2022).
Abramson, A. et al. A luminal unfolding microneedle injector for oral delivery of macromolecules. Nat. Med. 25, 1512–1518 (2019).
Our technology. Biograil https://biograil.com/the-technology/(2023).
Aran, K. et al. An oral microjet vaccination system elicits antibody production in rabbits. Sci. Transl. Med. 9, eaaf6413 (2017).
Beccani, M. et al. A magnetic drug delivery capsule based on a coil actuation mechanism. Procedia Eng. 120, 53–56 (2015).
Sarker, S. et al. A novel capsule-delivered enteric drug-injection device for delivery of systemic biologics: a pilot study in a porcine model. IEEE Trans. Biomed. Eng. 69, 1870–1879 (2021).
Srinivasan, S. S. et al. Robocap: robotic mucus-clearing capsule for enhanced drug delivery in the gastrointestinal tract. Sci. Robot. 7, eabp9066 (2022).
Söderlind, E. et al. Validation of the IntelliCap® system as a tool to evaluate extended release profiles in human GI tract using metoprolol as model drug. J. Control. Release 217, 300–307 (2015).
Koo, J. et al. Wirelessly controlled, bioresorbable drug delivery device with active valves that exploit electrochemically triggered crevice corrosion. Sci. Adv. 6, eabb1093 (2020).
Bal, S. M., Caussin, J., Pavel, S. & Bouwstra, J. A. In vivo assessment of safety of microneedle arrays in human skin. Eur. J. Pharm. Sci. 35, 193–202 (2008).
Miller, D. & Niichel, R. Advancing high tech drug delivery systems for the treatment of Crohn’s disease. Gastroenterology 160, S2–S3 (2021).
Dhalla, A. K. et al. A robotic pill for oral delivery of biotherapeutics: safety, tolerability, and performance in healthy subjects. Drug Deliv. Transl. Res. 12, 294–305 (2022).
Schoellhammer, C. M. et al. Ultrasound-mediated gastrointestinal drug delivery. Sci. Transl. Med. 7, 310ra168 (2015).
Schoellhammer, C. M., Langer, R. & Traverso, G. Of microneedles and ultrasound: physical modes of gastrointestinal macromolecule delivery. Tissue Barriers 4, e1150235 (2016).
Arnold, M. et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159, 335–349 (2020).
A study of high intensity focused ultrasound for cancer of the rectum. Cancer Research UK https://www.cancerresearchuk.org/about-cancer/find-a-clinical-trial/a-study-of-high-intensity-focused-ultrasound-for-cancer-of-the-rectum#undefined (2019).
Li, M., Wan, G., Yu, H. & Xiong, W. High-intensity focused ultrasound inhibits invasion and metastasis of colon cancer cells by enhancing microrna-124-mediated suppression of stat3. FEBS Open Bio 9, 1128–1136 (2019).
Stewart, F. et al. Ultrasound mediated delivery of quantum dots from a proof of concept capsule endoscope to the gastrointestinal wall. Sci. Rep. 11, 2584 (2021).
Rao, S. S., Lembo, A., Chey, W. D., Friedenberg, K. & Quigley, E. M. Effects of the vibrating capsule on colonic circadian rhythm and bowel symptoms in chronic idiopathic constipation. Neurogastroenterol. Motil. 32, e13890 (2020).
Ron, Y. et al. Safety and efficacy of the vibrating capsule, an innovative non-pharmacological treatment modality for chronic constipation. Neurogastroenterol. Motil. 27, 99–104 (2015).
Nelson, A. D. et al. A single-center, prospective, double-blind, sham-controlled, randomized study of the effect of a vibrating capsule on colonic transit in patients with chronic constipation. Neurogastroenterol. Motil. 29, e13034 (2017).
Yu, J. et al. Safety and efficacy of a new smartphone-controlled vibrating capsule on defecation in beagles. Sci. Rep. 7, 2841 (2017).
Miyashita, S. et al. Ingestible, controllable, and degradable origami robot for patching stomach wounds. In 2016 IEEE International Conference on Robotics and Automation (ICRA) 909–916 (IEEE, 2016).
Ponce, J., Quebbemann, B. B. & Patterson, E. J. Prospective, randomized, multicenter study evaluating safety and efficacy of intragastric dual-balloon in obesity. Surg. Obes. Relat. Dis. 9, 290–295 (2013).
Kaan, H. L. et al. First-in-man feasibility study of a novel ingestible magnetically inflated balloon capsule for treatment of obesity. Endosc. Int. Open 8, E607–E610 (2020).
Freitas, R., Rodrigues, J., Puga, H. & Correia, J. Design, simulation, and fabrication of an ingestible capsule with gastric balloon for obesity treatment. Biomed. Phys. Eng. Express 7, 055024 (2021).
Do, T. N., Seah, T. E. T., Yu, H. K. & Phee, S. J. Development and testing of a magnetically actuated capsule endoscopy for obesity treatment. PLoS ONE 11, e0148035 (2016).
Do, T. N., Ho, K. Y. & Phee, S. J. A magnetic soft endoscopic capsule-inflated intragastric balloon for weight management. Sci. Rep. 6, 1–10 (2016).
Phan, P. T. et al. EndoPil: a magnetically actuated swallowable capsule for weight management: development and trials. Ann. Biomed. Eng. 49, 1391–1401 (2021).
Cutts, T., Luo, J., Starkebaum, W., Rashed, H. & Abell, T. Is gastric electrical stimulation superior to standard pharmacologic therapy in improving GI symptoms, healthcare resources, and long-term health care benefits? Neurogastroenterol. Motil. 17, 35–43 (2005).
Abell, T. L. et al. Effectiveness of gastric electrical stimulation in gastroparesis: results from a large prospectively collected database of national gastroparesis registries. Neurogastroenterol. Motil. 31, e13714 (2019).
Abramson, A. et al. Ingestible transiently anchoring electronics for microstimulation and conductive signaling. Sci. Adv. 6, eaaz0127 (2020).
Maisiyiti, A. & Chen, J. D. Systematic review on gastric electrical stimulation in obesity treatment. Expert Rev. Med. Devices 16, 855–861 (2019).
Yao, G. et al. Effective weight control via an implanted self-powered vagus nerve stimulation device. Nat. Commun. 9, 5349 (2018).
TSMC MPW full block tapeouts. MUSE SEMICONDUCTOR https://www.musesemi.com/full-block-tapeout-pricing (2022).
Liao, Y.-T., Yao, H., Lingley, A., Parviz, B. & Otis, B. P. A 3-μW CMOS glucose sensor for wireless contact-lens tear glucose monitoring. IEEE J. Solid State Circuits 47, 335–344 (2012).
FCC Online Table of Frequency Allocations Title 47, Ch. 2, Part 106 (Federal Communications Commission, 2021).
Khaleghi, A. & Balasingham, I. On selecting the frequency for wireless implant communications. In IEEE Loughborough Antennas & Propagation Conference (LAPC) 1–4 (IEEE, 2015).
Liu, Y. & Gitlin, R. D. A phenomenological path loss model of the in vivo wireless channel. In 2015 IEEE 16th Annual Wireless and Microwave Technology Conference (WAMICON) 1–3 (IEEE, 2015).
Faerber, J. et al. In vivo characterization of a wireless telemetry module for a capsule endoscopy system utilizing a conformal antenna. IEEE Trans. Biomed. Circuits Systems 12, 95–105 (2018).
Basir, A., Zada, M., Cho, Y. & Yoo, H. A dual-circular-polarized endoscopic antenna with wideband characteristics and wireless biotelemetric link characterization. IEEE Trans. Antennas Propag. 68, 6953–6963 (2020).
Christoe, M. J. et al. Meandering pattern 433 MHz antennas for ingestible capsules. IEEE Access 9, 91874–91882 (2021).
Suzan Miah, M., Khan, A. N., Icheln, C., Haneda, K. & Takizawa, K.-I. Antenna system design for improved wireless capsule endoscope links at 433 MHz. IEEE Trans. Antennas Propag. 67, 2687–2699 (2019).
Lei, W. & Guo, Y.-X. Design of a dual-polarized wideband conformal loop antenna for capsule endoscopy systems. IEEE Trans. Antennas Propag. 66, 5706–5715 (2018).
Song, M. et al. A millimeter-scale crystal-less MICS transceiver for insertable smart pills. IEEE Trans. Biomed. Circuits Syst. 14, 1218–1229 (2020).
Abdigazy, A. & Monge, M. A bimodal low-power transceiver featuring a ring oscillator-based transmitter and magnetic field-based receiver for insertable smart pills. IEEE Solid State Circuits Lett. 5, 154–157 (2022).
Mondal, S. & Hall, D. A. A 67-μW ultra-low power PVT-robust MedRadio transmitter. In 2020 IEEE Radio Frequency Integrated Circuits Symposium (RFIC) 327–330 (IEEE, 2020).
Shi, Y., Chen, X., Kim, H.-S., Blaauw, D. & Wentzloff, D. 28.3 a 606μW mm-scale bluetooth low-energy transmitter using co-designed 3.5 × 3.5 mm 2 loop antenna and transformer-boost power oscillator. In 2019 IEEE International Solid-State Circuits Conference (ISSCC) 442–444 (IEEE, 2019).
Shibata, K. et al. A 22nm 0.84 mm 2 BLE transceiver with self IQ-phase correction achieving 39dB image rejection and on-chip antenna impedance tuning. In 2022 IEEE International Solid-State Circuits Conference (ISSCC) Vol. 65, 398–400 (IEEE, 2022).
Ba, A. et al. A 0.33 nJ/bit IEEE802. 15.6/proprietary MICS/ISM wireless transceiver with scalable data rate for medical implantable applications. IEEE J. Biomed. Health Inform. 19, 920–929 (2015).
Jang, J., Bae, J. & Yoo, H.-J. Understanding body channel communication: a review: from history to the future applications. In 2019 IEEE Custom Integrated Circuits Conference (CICC) 1–8 (IEEE, 2019).
Jang, J. et al. A four-camera VGA-resolution capsule endoscope system with 80-mB/s body channel communication transceiver and sub-centimeter range capsule localization. IEEE J. Solid State Circuits 54, 538–549 (2018).
Chang, T. C., Wang, M. L., Charthad, J., Weber, M. J. & Arbabian, A. 27.7 A 30.5mm3 fully packaged implantable device with duplex ultrasonic data and power links achieving 95kb/s with <10−4 BER at 8.5cm depth. In 2017 IEEE International Solid-State Circuits Conference (ISSCC) 460–461 (IEEE, 2017).
Zhang, Y. & Shepard, K. L. A 0.6-mm2 powering and data telemetry system compatible with ultrasound B-mode imaging for freely moving biomedical sensor systems. In 2019 IEEE Custom Integrated Circuits Conference (CICC) 1–4 (IEEE, 2019).
Sonmezoglu, S. & Maharbiz, M. M. 34.4 A 4.5mm3 deep-tissue ultrasonic implantable luminescence oxygen sensor. In 2020 IEEE International Solid-State Circuits Conference (ISSCC) 454–456 (IEEE, 2020).
Chuo, L.-X. et al. 7.4 A 915MHz asymmetric radio using Q-enhanced amplifier for a fully integrated 3 × 3 × 3mm3 wireless sensor node with 20m non-line-of-sight communication. In 2017 IEEE International Solid-State Circuits Conference (ISSCC) 132–133 (IEEE, 2017).
Chen, Y. et al. A review of lithium-ion battery safety concerns: the issues, strategies, and testing standards. J. Energy Chem. 59, 83–99 (2021).
Le, S. et al. Status of zinc–silver battery. J. Electrochem. Soc. 166, A2980 (2019).
Ciuti, G., Menciassi, A. & Dario, P. Capsule endoscopy: from current achievements to open challenges. IEEE Rev. Biomed. Eng. 4, 59–72 (2011).
Li, C. et al. An advance review of solid-state battery: challenges, progress and prospects. Sustain. Mater. Technol. 29, e00297 (2021).
Kumar, P. et al. Melanin-based flexible supercapacitors. J. Mater. Chem. C 4, 9516–9525 (2016).
Mittal, N., Ojanguren, A., Niederberger, M. & Lizundia, E. Degradation behavior, biocompatibility, electrochemical performance, and circularity potential of transient batteries. Adv. Sci. 8, 2004814 (2021).
Chen, Y. et al. Physical–chemical hybrid transiency: a fully transient Li-ion battery based on insoluble active materials. J. Polym. Sci. B 54, 2021–2027 (2016).
Kutbee, A. T. et al. Flexible and biocompatible high-performance solid-state micro-battery for implantable orthodontic system. npj Flex. Electron. 1, 7 (2017).
Li, N., Chen, Z., Ren, W., Li, F. & Cheng, H.-M. Flexible graphene-based lithium ion batteries with ultrafast charge and discharge rates. Proc. Natl Acad. Sci. USA 109, 17360–17365 (2012).
Aeby, X., Poulin, A., Siqueira, G., Hausmann, M. K. & Nyström, G. Fully 3D printed and disposable paper supercapacitors. Adv. Mater. 33, 2101328 (2021).
Crespilho, F. N. et al. Non-corrosive, low-toxicity gel-based microbattery from organic and organometallic molecules. J. Mater. Chem. A 7, 24784–24787 (2019).
Liu, L., Towfighian, S. & Jin, Z. A cylindrical triboelectric energy harvester for capsule endoscopes. In 2015 IEEE Biomedical Circuits and Systems Conference (BioCAS) 1–4 (IEEE, 2015).
Yoshida, S., Miyaguchi, H. & Nakamura, T. Development of ingestible thermometer with built-in coil antenna charged by gastric acid battery and demonstration of long-time in vivo telemetry. IEEE Access 9, 102368–102377 (2021).
Dong, K. et al. Microbial fuel cell as power supply for implantable medical devices: a novel configuration design for simulating colonic environment. Biosens. Bioelectron. 41, 916–919 (2013).
Han, Y., Yu, C. & Liu, H. A microbial fuel cell as power supply for implantable medical devices. Biosens. Bioelectron. 25, 2156–2160 (2010).
Zhao, L., Annayev, M., Oralkan, Ö. & Jia, Y. An ultrasonic energy harvesting IC providing adjustable bias voltage for pre-charged CMUT. IEEE Trans. Biomed. Circuits Systems 16, 842–851 (2022).
Abid, A. et al. Wireless power transfer to millimeter-sized gastrointestinal electronics validated in a swine model. Sci. Rep. 7, 46745 (2017).
Iqbal, A., Sura, P. R., Al-Hasan, M., Mabrouk, I. B. & Denidni, T. A. Wireless power transfer system for deep-implanted biomedical devices. Sci. Rep. 12, 13689 (2022).
Ingestible Telemetric Gastrointestinal Capsule Imaging System—Final Class II Special Controls Guidance Document for Industry and FDA (US FDA, 2001); https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/ingestible-telemetric-gastrointestinal-capsule-imaging-system-final-class-ii-special-controls
General Considerations for Animal Studies Intended to Evaluate Medical Devices (US FDA, 2023); https://www.fda.gov/regulatory-information/search-fda-guidance-documents/general-considerations-animal-studies-intended-evaluate-medical-devices
Wang, Y.-C. et al. Adverse events of video capsule endoscopy over the past two decades: a systematic review and proportion meta-analysis. BMC Gastroenterol. 20, 364 (2020).
Lee, S. Y., Lee, J. Y., Lee, Y. J. & Park, K. S. Natural elimination of a video capsule after retention for 1 year in a patient with small bowel crohn disease: a case report. Medicine 98, e17580 (2019).
Saad, M. K., Fiani, E., El Hajj, I. & Saikaly, E. A rare complication of capsule endoscopy, retained in diverticula: a report of two cases. Int. J. Gastrointest. Interv. 10, 36–39 (2021).
Inui, T., Koga, H., Nogi, M., Komoda, N. & Suganuma, K. A miniaturized flexible antenna printed on a high dielectric constant nanopaper composite. Adv. Mater. 27, 1112–1116 (2015).
Rai, T., Dantes, P., Bahreyni, B. & Kim, W. S. A stretchable RF antenna with silver nanowires. IEEE Electron Device Lett. 34, 544–546 (2013).
Tsang, M. et al. A MEMS-enabled biodegradable battery for powering transient implantable devices. In 2014 IEEE 27th International Conference on Micro Electro Mechanical Systems (MEMS) 358–361 (IEEE, 2014).
Hu, L., Wu, H., La Mantia, F., Yang, Y. & Cui, Y. Thin, flexible secondary Li-ion paper batteries. ACS Nano 4, 5843–5848 (2010).
Bonacchini, G. E. et al. Tattoo-paper transfer as a versatile platform for all-printed organic edible electronics. Adv. Mater. 30, 1706091 (2018).
Kang, S.-K., Koo, J., Lee, Y. K. & Rogers, J. A. Advanced materials and devices for bioresorbable electronics. Acc. Chem. Res. 51, 988–998 (2018).
Umay, I., Fidan, B. & Barshan, B. Localization and tracking of implantable biomedical sensors. Sensors 17, 583 (2017).
Wang, M. L., Chang, T. C. & Arbabian, A. Ultrasonic implant localization for wireless power transfer: active uplink and harmonic backscatter. In 2019 IEEE International Ultrasonics Symposium (IUS) 818–821 (IEEE, 2019).
Chen, H., Rogalski, M. M. & Anker, J. N. Advances in functional X-ray imaging techniques and contrast agents. Phys. Chem. Chem. Phys. 14, 13469–13486 (2012).
Koziolek, M. et al. Investigation of pH and temperature profiles in the GI tract of fasted human subjects using the IntelliCap® system. J. Pharm. Sci. 104, 2855–2863 (2015).
Ye, Y., Khan, U. & Pahlavan, K. Accuracy bounds for RSS and TOA based RF localization in capsule endoscopy. In Proc. 33rd IEEE Annual International Conference of Engineering in Medicine and Biology Society (EMBC) 5602–5607 (IEEE, 2011).
Vasisht, D. et al. In-body backscatter communication and localization. In Proc. 2018 Conference of the ACM Special Interest Group on Data Communication 132–146 (ACM, 2018).
Chen, F., Liu, J. & Liao, H. 3D catheter shape determination for endovascular navigation using a two-step particle filter and ultrasound scanning. IEEE Trans. Med. Imaging 36, 685–695 (2017).
Parent, F. et al. Intra-arterial image guidance with optical frequency domain reflectometry shape sensing. IEEE Trans. Med. Imaging 38, 482–492 (2019).
Hu, C., Meng, M.-H. & Mandal, M. Efficient linear algorithm for magnetic localization and orientation in capsule endoscopy. In 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference 7143–7146 (IEEE, 2005).
Hu, C. et al. A cubic 3-axis magnetic sensor array for wirelessly tracking magnet position and orientation. IEEE Sens. J. 10, 903–913 (2010).
Gao, H., Lin, Y. & Monge, M. Towards magnetic field gradient-based imaging and control of in-body devices. In 2021 IEEE Biomedical Circuits and Systems Conference (BioCAS) 1–4 (IEEE, 2021).
Rustom, M. & Sideris, C. Wireless frequency-division multiplexed 3D magnetic localization for low power sub-mm precision capsule endoscopy. In 2022 IEEE Custom Integrated Circuits Conference (CICC) 01–02 (IEEE, 2022).
Rustom, M. & Sideris, C. Design and implementation of a low power wireless frequency-division multiplexed magnetic 3D localization scheme with sub-mm precision for capsule endoscopy applications. IEEE Solid State Circuits Lett. 6, 37–40 (2023).
Sharma, S. et al. Location-aware ingestible microdevices for wireless monitoring of gastrointestinal dynamics. Nat. Electron. 6, 242–256 (2023).
Carta, R. et al. Wireless powering for a self-propelled and steerable endoscopic capsule for stomach inspection. Biosens. Bioelectron. 25, 845–851 (2009).
Liang, H., Guan, Y., Xiao, Z., Hu, C. & Liu, Z. A screw propelling capsule robot. In 2011 IEEE International Conference on Information and Automation 786–791 (IEEE, 2011).
Wang, K., Yan, G., Ma, G. & Ye, D. An earthworm-like robotic endoscope system for human intestine: design, analysis, and experiment. Ann. Biomed. Eng. 37, 210–221 (2009).
Chen, Z., Liu, J., Wang, S. & Zuo, S. A bio-inspired self-propelling endoscopic device for inspecting the large intestine. Bioinspir. Biomim. 14, 066013 (2019).
Kim, H. M. et al. Active locomotion of a paddling-based capsule endoscope in an in vitro and in vivo experiment (with videos). Gastrointest. Endosc. 72, 381–387 (2010).
Valdastri, P. et al. A new mechanism for mesoscale legged locomotion in compliant tubular environments. IEEE Trans. Robot. 25, 1047–1057 (2009).
Mosse, C., Mills, T. N., Appleyard, M. N., Kadirkamanathan, S. S. & Swain, C. Electrical stimulation for propelling endoscopes. Gastrointest. Endosc. 54, 79–83 (2001).
Woo, S. H., Kim, T. W., Mohy-Ud-Din, Z., Park, I. Y. & Cho, J.-H. Small intestinal model for electrically propelled capsule endoscopy. Biomed. Eng. Online 10, 108 (2011).
Keller, J. et al. Inspection of the human stomach using remote-controlled capsule endoscopy: a feasibility study in healthy volunteers (with videos). Gastrointest. Endosc. 73, 22–28 (2011).
Rey, J.-F. et al. Blinded nonrandomized comparative study of gastric examination with a magnetically guided capsule endoscope and standard videoendoscope. Gastrointest. Endosc. 75, 373–381 (2012).
Schostek, S. et al. Telemetric real-time sensor for the detection of acute upper gastrointestinal bleeding. Biosens. Bioelectron. 78, 524–529 (2016).
Zhuang, Z. et al. Alterations of the gut microbiota and plasma biomarkers in Parkinson’s disease. Parkinsonism Relat. Disord. 81, 179–184 (2020).
Kang, D.-W. et al. Microbiota transfer therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome 7, 10 (2019).
Acknowledgements
Y.K. acknowledges support from USC Viterbi School of Engineering.
Author information
Authors and Affiliations
Contributions
A. Abdigazy, M.A. and Y.K. conceptualized and wrote the review paper. G.L., C.S. and A. Abramson provided feedback and suggestions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Electronics thanks Azita Emami, Santosh Pandey and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–4.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdigazy, A., Arfan, M., Lazzi, G. et al. End-to-end design of ingestible electronics. Nat Electron 7, 102–118 (2024). https://doi.org/10.1038/s41928-024-01122-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41928-024-01122-2