Abstract
The aim of the study was to investigate the prognostic significance of the advanced lung cancer inflammation index (ALI) in patients with limited-stage small-cell lung cancer (LS-SCLC) undergoing definite chemo-radiotherapy (CRT). We included 87 patients with LS-SCLC from South Korea, treated between 2005 and 2019 with definite CRT. ALI was calculated using body mass index, serum albumin, and neutrophil–lymphocyte ratio. We categorized 38 patients into the high ALI group (ALI ≥ 44.3) and 48 into the low ALI group (ALI < 44.3). Patients in the high ALI group exhibited longer overall survival (OS) than patients in the low ALI group. In multivariate analysis, prophylactic cranial irradiation (hazard ratio [HR] = 0.366, 95% confidence interval [CI] 0.20–0.66, P = 0.0008), and high ALI (HR = 0.475, 95% CI 0.27–0.84, P = 0.0103) were identified as independent prognostic factors for predicting better OS. Notably, a high ALI score was particularly indicative of longer survival in patients treated with the combination of etoposide and cisplatin. In conclusion, this study demonstrated that a high pretreatment ALI was significantly associated with better OS in patients with LS-SCLC undergoing definite CRT. This suggests that ALI could be a useful tool for predicting prognosis and guiding chemotherapy regimen selections in clinical practice for LS-SCLC.
Similar content being viewed by others
Introduction
Lung cancer remains a leading cause of death world-wide, holding the highest mortality rate among all cancers in South Korea1. Small cell lung cancer (SCLC) constitutes approximately about 15% of all lung cancer types, characterized by aggressive features such as rapid doubling time, a high growth fraction, and early extensive metastasis2. Prior to treatment, approximately 30–40% of SCLC patients present with limited-stage small cell lung cancer (LS-SCLC), qualifying them as suitable candidates for radiotherapy. The standard treatment for LS-SCLC involves concurrent chemotherapy and thoracic radiotherapy (TRT). While LS-SCLC exhibits high sensitivity to chemotherapy and radiotherapy, it is prone to relapse, with median survival ranging 15 to 20 months, from the time of diagnosis3. Therefore, identifying accurate prognostic indicators for LS-SCLC is crucial.
Various clinical parameters, including cancer staging, performance stage, age, and smoking status, have been suggested to be related to prognosis4,5. Notably, inflammation has emerged as a hallmark characteristic in cancer development and metastasis6. Various laboratory markers of systemic inflammation, such as C-reactive protein (CRP), albumin, and lactate dehydrogenase (LDH) levels, have been proposed for prognostication. The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) have demonstrated prognostic value in various malignancies, such as gastric cancer, head and neck cancer, melanoma, and lung cancer7,8,9,10,11. Recently, a new prognostic marker, the advanced lung cancer inflammation index (ALI), based on height, weight, serum albumin, and NLR, has been suggested for patients with lung cancer12,13,14. In SCLC research, earlier studies have proposed ALI as a prognostic indicator13,15, but the limited sample sizes of patients with LS-SCLC have hindered comprehensive research.
This study aimed to investigate the prognostic significance of ALI in the peripheral blood of patients with LS-SCLC undergoing chemoradiotherapy (CRT), focusing on overall survival (OS). Additionally, we aimed to identify other factors that may modify the prognostic utility of ALI.
Results
In total of 87 patients with LS-SCLC were analyzed, encompassing comprehensive clinical information and baseline laboratory parameters. The baseline characteristics of the study population are summarized in Table 1. The mean age of the study population was 64.7 (SD, 8.9) years, which included 75 (86.2%) male patients. A significant majority, including 85 (97.7%) patients were ever-smokers. The performance status (PS) was generally good, with 43 (49.4%) patients scoring 0, 40 (46%) scoring 1, and only 4 (4.6%) scoring 2. Underlying comorbidities included chronic obstructive pulmonary disease in 42 (48.3%), diabetes mellitus in 30 (34.5%), hypertension in 36 (41.4%), and chronic kidney disease (CKD) in 17 (19.5%) patients. Most patients received platinum-based chemotherapy concurrently during the course of RT, with 11 (12.6%) patients receiving RT sequentially. In terms of chemotherapeutic regimen, 83 (95.4%) patients received etoposide-based combination chemotherapy, while the remaining four (4.6%) received irinotecan-based combination chemotherapy. Consolidation chemotherapy was administered in 30 (40.2%) patients and prophylactic cranial irradiation (PCI) was performed in 35 (34.5%) patients.
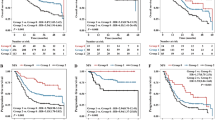
Using the biostatistical tool Cutoff Finder16, the optimal cutoff point of ALI for layering OS in LS-SCLC was determined to be 44.3 (Fig. 1). Based on this cutoff value, excluding one patient whose albumin level was not measured, patients were divided into two groups: ALI < 44.3 (n = 48) and ≥ 44.3 (n = 38). Both groups demonstrated no statistical differences in terms of sex, age, smoking history, PS, underlying diseases, TNM stage, radiation dosage, schedule of radiotherapy, chemotherapy regimen, and PCI.
Hazard ratio for overall survival based on the cutoff-point for the advanced lung cancer inflammation index in patients with limited-stage small-cell lung cancer. The vertical line designates the optimal cutoff-point with the most significant (Log-Rank Test) split. The plot is generated using the Biostatistical Tool, Cutoff Finder.
The median OS of all patients was 21.5 (18.6–31.9) months. Univariate and multivariate analyses of OS were performed for clinical and laboratory factors. Several prognostic factors identified through the univariate analysis included higher radiotherapy dosage (≥ 60 Gy; hazard ratio [HR] = 0.532, 95% confidence interval [CI] 0.32–0.90, P = 0.0185 vs. 45–60 Gy), advanced TNM stage (IIIB/IIIC; HR = 2.786, 95% CI 1.27–6.09, P = 0.0103 vs. stage I/II), the presence of PCI (HR = 0.366, 95% CI 0.20–0.66, P = 0.0008), and high ALI (HR = 0.475, 95% CI 0.27–0.84, P = 0.0098). However, in multivariate analysis, advanced TNM stage of IIIB/IIIC (HR = 2.786, 95% CI 1.27–6.09, P = 0.0103 vs. stage I/II) was related to worse survival, though the difference did not reach statistical significance (HR = 2.117, 95% CI 0.95–4.70, P = 0.0656) (Table 2). Additionally, patients who received PCI (P = 0.005) or had a high ALI score (P = 0.006) exhibited statistically better survival rates (Fig. 2).
Within the patients receiving etoposide and cisplatin (EP) regimen, ALI score emerged as an independent prognostic factor in patients with LS-SCLC treated with EP regimen in multivariate analysis. A high ALI value was significantly associated with improved long-term survival outcomes (HR = 0.388, 95% CI 0.20–0.75, P = 0.0045) (Table 3). Among patients with high ALI score, those treated with etoposide and carboplatin (EC) regimen exhibited a higher mortality risk compared to EP regimen, although the difference did not reach statistical significance (HR = 3.211, 95% CI 1.00–10.32, P = 0.0501) according to Cox proportional hazard analysis (Table 4).
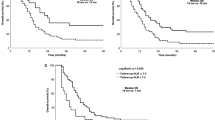
The difference in OS was not statistically significant when comparing patients treated with EP to those treated with EC or other regimens (P = 0.519) (Fig. 3A). In subgroup analysis among patients in the EP regimen-treated group, the high-ALI group had a significantly longer OS time compared to the low ALI-group (P = 0.007). However, in the EC regimen-treated group, no difference in OS time was observed between the high and low ALI groups (P = 0.784) (Fig. 3B,C).
Kaplan–Meier curves for overall survival (OS) of patients with limited-stage small-cell lung cancer treated with etoposide and cisplatin (EP) and etoposide and carboplatin (EC). (A) No difference in OS time is observed among chemotherapy regimens (EP, EC and others; P = 0.519). (B) In the EP regimen‑treated group, the high ALI group exhibit a significantly longer OS time than that of the low ALI group (P = 0.007). (C) In the EC regimen‑treated group, no difference in OS time is observed between the high and low ALI groups (P = 0.784).
Discussion
In this retrospective study, we established that the pre-treatment ALI serves as a significant prognostic indicator for predicting OS in patients with LS-SCLC undergoing definite CRT. Multivariate analysis revealed that a high ALI score, using a cut-off value of 44.3, was associated with better survival. Furthermore, subgroup analysis within the EP regimen-treated group demonstrated that a high-ALI score was associated with an extended OS time. Interestingly, another subgroup analysis within the high-ALI group suggested that patients receiving the EC regimen may have worse survival compared to those on the EP regimen, although this observation did not achieve statistical significance.
This finding aligns with those of earlier studies, particularly the findings of Jafri et al., who initially developed ALI as a prognostic marker for non-small cell lung cancer (NSCLC), highlighting that a low ALI score (< 18), indicating significant systemic inflammation, was associated with poor progression free survival (PFS) and OS12. Similarly, Xiaobo He et al. reported ALI as an independent prognostic marker in SCLC13. Following these studies, numerous research has reinforced the prognostic value of various inflammatory biomarkers in the field of lung cancer17,18, with NLR and ALI emerging as simple and cost-effective tools for evaluating systemic inflammation. Although not fully understood, the negative correlation of a high NLR with worse OS, observed consistently across various cancer types, may be attributed to the immunological effects of neutrophils and lymphocytes19. Neutrophils, through the secretion of tumor growth factors, including vascular endothelial growth factor, IL-6, IL-8, matrix metalloproteinase, and elastase, contribute to the stimulation of the tumor microenvironment, while also suppressing the cytotoxic activity of lymphocytes, activated T cells, and natural killer cells, which are crucial elements in the prognosis and cytotoxic treatment of cancer patients20,21,22. Conversely, lymphocytes play a fundamental role in cytotoxic cell death and cytokine production in tumor cell destruction, making lymphocyte count a recognized predictor of survival in patients with advanced cancer treated with chemotherapy23,24. This immunologic effect is heightened in radiotherapy, where radiation induces tumor cell death by directly inducing DNA damage, producing tumor-associated antigens, enhancing antigen presentation, and increasing immune cell infiltration25,26. While the prognostic value of inflammatory indices in radiotherapy is documented in multiple studies27,28, previous research has predominantly focused on NSCLC or advanced stages treated with systemic chemotherapy. Although some recent studies reported the use of NLR as a prognostic value in NSCLC patients treated with CCRT29,30,31, patients with LS-SCLC were overlooked due to the limited number of patients. Our study exclusively focuses on patients with LS-SCLC treated with definite chemo-radiotherapy, broadening the utility of ALI as a prognostic factor.
An etoposide and platinum combination regimen is the first choice for SCLC treatment, and in multiple randomized controlled trials, the combination of carboplatin or cisplatin with etoposide resulted in no significant difference in PFS or OS32,33, making the choice of treatment challenging. Pan et al. initially proposed the potential consideration of pre-treatment NLR for optimizing the choice of treatment in SCLC. Their findings suggested that patients with high NLR exhibited significantly longer PFS when treated with the EP regimen, than that of patients treated with the EC regimen34. Liu et al. reported contradicting results, as in the low-NLR group, the treatment with the EP regimen resulted in better OS time than that of the EC regimen treatment, and in the high-NLR group, the EC regimen treatment conferred better OS outcomes than that of the EP regimen treatment35. This observation is in line with the results of our study, which incorporated the ALI score, supporting the notion that inflammatory biomarkers can play a role in the selection of chemotherapy regimens in patients with LS-SCLC.
As the understanding of lung cancer biology and the inflammatory effects of cancer development advances, the introduction of immune checkpoint inhibitors (ICIs) has shifted the treatment paradigm. For patients without driver mutation, ICIs such as PD-1 inhibitors are now integral in the treatment of NSCLC36. In SCLC, ICIs conventionally have been limited to extensive-stage cases due to the lack of correlating immune biomarkers for treatment response, making patient selection difficult37,38. However, recent investigations have explored expanding the role of ICIs to LS-SCLC. Welsh et al. presented a phase I/II study of concurrent pembrolizumab combining CRT in LS-SCLC, showing favorable outcome39. Such promising results emphasizes the need for development of prognostic biomarkers. Although PD-L1 expression is recommended biomarker in NSCLC by National Comprehensive Cancer Network (NCCN) guideline, it has shown insufficient in SCLC patients40. Inflammatory biomarkers drawn from peripheral blood, such as NLR and/or PLR are showing prognostic value in patients treated with ICIs in NSCLC, as low NLR and PLR are associated with better survival outcomes41,42,43. Shiroyama et al. first demonstrated the relationship between ALI and the survival outcome of NSCLC patients treated with immunotherapy, as a low ALI score is associated with poor prognosis and patients may benefit from continued nivolumab treatment44. Mountzio et al. conducted a large comparative study showing the prognostic value of ALI for patients with advanced NSCLC treated with PD-L1 inhibitors alone45. As shown by our study, ALI may help broaden patient selection in patients with LS-SCLC for immunotherapy; however, further investigation is needed.
Despite these insights, out study has several limitations. The retrospective design and a relatively small number of patients constrain generalization and introduce selection bias. The cut-off value for defining high and low ALI groups needs further validation. As previously mentioned, Jafri et al. drew cutoff value at 18 which was around 50th percentile mark to divide high and low ALI group12. In study of prognostic value of ALI in SCLC following surgical resection, Hu et al. drew cut off value at 48.2 using ROC curve analysis15. As such, standardizing program for ALI and its cutoff value needs further discussion. Furthermore, other inflammatory blood parameters such as CRP, monocyte, platelet, hemoglobin counts are not included in calculating ALI. As previous studies have shown prognostic value of lymphocyte-to-CRP ratio (LCR), systemic immune-inflammation index (SII), systemic inflammation response index (SIRI), and hemoglobin-to-red-cell-distribution-width ratio (HRR), further investigation is needed to supplement the ALI formula46. Additionally, our study did not investigate baseline conditions that could affect NLR such as sepsis, pneumonia or cardiovascular disease due to limited data. Therefore, we are unable to provide additional information on this aspect.
In conclusion, this study is the first to indicate the potential use of ALI values for predicting survival in patients with LS-SCLC undergoing definite CRT. Moreover, our data imply that pre-treatment ALI score, as a blood-based biomarker, could be useful to identify specific subgroup of LS-SCLC likely to benefit from definite CRT. Additionally, it offers valuable guidance for selecting appropriate chemotherapy regimen in those patients, providing a basis for further investigations.
Methods
Study population and data collection
A retrospective study was conducted including patients with LS-SCLC treated with definite CRT at four university-affiliated hospitals in South Korea: Hanyang University Hospital, Hanyang Guri University Hospital, Kyeonghi University Hospital, and Kangdong Kyeonghi University hospital, spanning from January 2005 to December 2019. Inclusion criteria comprised a pathologically proven diagnosis of SCLC, confirmed as LS-SCLC (confined to one hemithorax, mediastinum, contralateral hilus, and supraclavicular regions), and completion of combined chemotherapy and TRT as planned. Patients confirmed as having extensive stage small-cell lung cancer were excluded.
The study included 87 patients with LS-SCLC, and survival was defined as period from the date of diagnosis to death from any other cause or the last follow-up.
Data on demographic factors associated with mortality were collected, including sex, body mass index (BMI), age at the time of SCLC diagnosis, calendar year of SCLC diagnosis, smoking status, years of initiation for radiotherapy, radiation dosage, PS, underlying diseases including CKD, TNM stage for lung cancer, schedule of radiotherapy, chemotherapy regimen, status of PCI, and consolidation chemotherapy. Pretreatment blood samples were collected for white blood cell counts, absolute lymphocyte counts, absolute neutrophil counts, platelet counts, serum albumin, LDH, and CRP.
ALI, proposed as a potential prognostic biomarker, was calculated using the formula: BMI × serum albumin/NLR, with NLR representing the proportion of neutrophil counts to lymphocyte counts in peripheral blood.
Patients eligible for the study underwent baseline staging computed tomography, irradiation of all pathological upon completion of TRT, and at least one course of chemotherapy. All enrolled patients received thoracic radiotherapy of at least 45 Gy in once-daily doses of 2 Gy administered over 6 weeks using involved-field TRT. Administration of PCI was optional for those responding well to CRT, and the decision to add consolidation chemotherapy was made individually, considering the patient’s preference and performance status.
Statistical analysis
SAS software (version 9.4; SAS Institute, Cary, NC, USA) was used for patient matching, and R software (version 3.4.2; R Development Core Team, Vienna, Austria) for all other statistical analyses, following an assessment of the data distribution’s normality using the Shapiro–Wilk test. Continuous variables were compared using the Student’s t-test or Mann–Whitney U test, and categorical variables using the χ2 or Fisher’s exact tests. Nominal variables are expressed as frequencies and percentages, while continuous variables are presented as means ± SD if normally distributed, and as medians with quartile range if non-normally distributed. Follow-up began at the time of cancer diagnosis and ended at the time of death or the last follow-up visit for patients without an event (whichever occurred first).
Survival curves were estimated using the Kaplan–Meier method, and differences in survival among groups were assessed using a two-sided log-rank test. Univariate associations of mortality with clinicopathological variables of interest were analyzed using a Cox proportional hazards regression model. The best subset selection method was then applied to build multivariate models, including variables significant in the univariate analysis, using the backward stepwise selection method. The Akaike information criterion (AIC) was computed to select the model with the smallest AIC value.
The years of treatment initiation were categorized into 2005–2009, 2010–2014, and 2015–2019, with a difference in radiation dose in 2015–2019 compared to 2005–2014 (mean 62.02 vs 51.69 Gy). Although the optimal radiation dose and schedule has not been established, it is widely recognized that increasing radiation dose is associate with better survival outcomes47,48. Therefore, we used radiation dose rather than years of initiation for radiotherapy as a variable in the final multivariable analysis.
The prognostic value of ALI was determined using the Biostatistical Tool, Cutoff Finder, to obtain the cut-off point. Subgroup analysis was performed for the low-ALI (ALI < 44.3) and high‑ALI (ALI ≥ 44.3) groups using Cox proportional hazards regression analysis, estimating HRs and calculating P-values for various prognostic factors. Additional subgroup analysis based on the chemotherapy regimen provided to patients was conducted, considering previous research showing relevant yet contradicting results with NLR and EP, EC regimens34,35. Thus, we hypothesized that ALI could be a relevant prognostic factor in selecting a chemotherapy-regimen.
Survival curves were generated using the Kaplan–Meier method. All tests were two-sided, and P-values < 0.05 were considered statistically significant.
Ethics statement
The study protocol received approval from the Institutional Review Board (IRB) of Hanyang University Hospital, Seoul, South Korea (IRB No.–2023-01-002), in accordance with the principles outlined in the Declaration of Helsinki. All data were anonymized before analysis, and the IRB at Hanyang University Hospital waived the requirement for informed consent from the study participants due to the retrospective nature of the study.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kang, M. J. et al. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2019. Cancer Res. Treat. 54, 330–344. https://doi.org/10.4143/crt.2022.128 (2022).
Rudin, C. M., Brambilla, E., Faivre-Finn, C. & Sage, J. Small-cell lung cancer. Nat. Rev. Dis. Primers 7, 3. https://doi.org/10.1038/s41572-020-00235-0 (2021).
Bogart, J. A., Waqar, S. N. & Mix, M. D. Radiation and systemic therapy for limited-stage small-cell lung cancer. J. Clin. Oncol. 40, 661–670. https://doi.org/10.1200/jco.21.01639 (2022).
Woodard, G. A., Jones, K. D. & Jablons, D. M. Lung cancer staging and prognosis. Cancer Treat. Res. 170, 47–75. https://doi.org/10.1007/978-3-319-40389-2_3 (2016).
Nasim, F., Sabath, B. F. & Eapen, G. A. Lung cancer. Med. Clin. North Am. 103, 463–473. https://doi.org/10.1016/j.mcna.2018.12.006 (2019).
Mantovani, A., Allavena, P., Sica, A. & Balkwill, F. Cancer-related inflammation. Nature 454, 436–444. https://doi.org/10.1038/nature07205 (2008).
Kao, D. D. et al. Neutrophil-to-lymphocyte ratio as a predictor of surgical outcomes in head and neck cancer. Head Neck 45, 1903–1912. https://doi.org/10.1002/hed.27402 (2023).
Li, P., Li, H., Ding, S. & Zhou, J. NLR, PLR, LMR and MWR as diagnostic and prognostic markers for laryngeal carcinoma. Am. J. Transl. Res. 14, 3017–3027 (2022).
Hirahara, T. et al. Combined neutrophil-lymphocyte ratio and platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with advanced gastric cancer. BMC Cancer 19, 672. https://doi.org/10.1186/s12885-019-5903-y (2019).
Xia, W. K. et al. Prognostic performance of pre-treatment NLR and PLR in patients suffering from osteosarcoma. World J. Surg. Oncol. 14, 127. https://doi.org/10.1186/s12957-016-0889-2 (2016).
Ma, J. et al. Neutrophil-to-lymphocyte Ratio (NLR) as a predictor for recurrence in patients with stage III melanoma. Sci. Rep. 8, 4044. https://doi.org/10.1038/s41598-018-22425-3 (2018).
Jafri, S. H., Shi, R. & Mills, G. Advance lung cancer inflammation index (ALI) at diagnosis is a prognostic marker in patients with metastatic non-small cell lung cancer (NSCLC): A retrospective review. BMC Cancer 13, 158. https://doi.org/10.1186/1471-2407-13-158 (2013).
He, X. et al. Advanced lung cancer inflammation index, a new prognostic score, predicts outcome in patients with small-cell lung cancer. Clin. Lung Cancer 16, e165-171. https://doi.org/10.1016/j.cllc.2015.03.005 (2015).
Zhang, X., Wang, D., Sun, T., Li, W. & Dang, C. Advanced lung cancer inflammation index (ALI) predicts prognosis of patients with gastric cancer after surgical resection. BMC Cancer 22, 684. https://doi.org/10.1186/s12885-022-09774-z (2022).
Hu, Z. et al. Advanced lung cancer inflammation index is a prognostic factor of patients with small-cell lung cancer following surgical resection. Cancer Manag. Res. 13, 2047–2055. https://doi.org/10.2147/cmar.S295952 (2021).
Budczies, J. et al. Cutoff Finder: A comprehensive and straightforward Web application enabling rapid biomarker cutoff optimization. PLoS ONE 7, e51862. https://doi.org/10.1371/journal.pone.0051862 (2012).
Sumiyoshi, I. et al. High lymphocyte population-related predictive factors for a long-term response in non-small cell lung cancer patients treated with pemetrexed: A retrospective observational study. J. Transl. Med. 19, 92. https://doi.org/10.1186/s12967-021-02761-1 (2021).
Song, M. et al. The advanced lung cancer inflammation index is the optimal inflammatory biomarker of overall survival in patients with lung cancer. J. Cachexia Sarcopenia Muscle 13, 2504–2514. https://doi.org/10.1002/jcsm.13032 (2022).
Diakos, C. I., Charles, K. A., McMillan, D. C. & Clarke, S. J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 15, e493-503. https://doi.org/10.1016/s1470-2045(14)70263-3 (2014).
Shamamian, P. et al. Activation of progelatinase A (MMP-2) by neutrophil elastase, cathepsin G, and proteinase-3: A role for inflammatory cells in tumor invasion and angiogenesis. J. Cell Physiol 189, 197–206. https://doi.org/10.1002/jcp.10014 (2001).
Balkwill, F. & Mantovani, A. Inflammation and cancer: Back to Virchow?. Lancet 357, 539–545. https://doi.org/10.1016/s0140-6736(00)04046-0 (2001).
Jabłońska, E. et al. TNF-alpha, IL-6 and their soluble receptor serum levels and secretion by neutrophils in cancer patients. Arch. Immunol. Ther. Exp. (Warsz) 49, 63–69 (2001).
Lissoni, P. et al. Efficacy of cancer chemotherapy in relation to the pretreatment number of lymphocytes in patients with metastatic solid tumors. Int. J. Biol. Markers 19, 135–140. https://doi.org/10.1177/172460080401900208 (2004).
Eerola, A. K., Soini, Y. & Pääkkö, P. A high number of tumor-infiltrating lymphocytes are associated with a small tumor size, low tumor stage, and a favorable prognosis in operated small cell lung carcinoma. Clin. Cancer Res. 6, 1875–1881 (2000).
Arina, A., Gutiontov, S. I. & Weichselbaum, R. R. Radiotherapy and immunotherapy for cancer: From “systemic” to “multisite”. Clin. Cancer Res. 26, 2777–2782. https://doi.org/10.1158/1078-0432.Ccr-19-2034 (2020).
Jeong, H., Bok, S., Hong, B. J., Choi, H. S. & Ahn, G. O. Radiation-induced immune responses: Mechanisms and therapeutic perspectives. Blood Res. 51, 157–163. https://doi.org/10.5045/br.2016.51.3.157 (2016).
Chen, D. et al. Pre-radiotherapy systemic immune inflammation index associated with overall survival in patients with advanced EGFR mutant non-small cell lung cancer receiving thoracic radiotherapy. Clin. Transl. Oncol. 25, 226–235. https://doi.org/10.1007/s12094-022-02936-2 (2023).
Luo, H. et al. Systemic inflammation biomarkers predict survival in patients of early stage non-small cell lung cancer treated with stereotactic ablative radiotherapy—a single center experience. J. Cancer 9, 182–188. https://doi.org/10.7150/jca.21703 (2018).
Park, E. Y. et al. Prognostic value of neutrophil-to-lymphocyte ratio in locally advanced non-small cell lung cancer treated with concurrent chemoradiotherapy. Radiat. Oncol. J. 37, 166–175. https://doi.org/10.3857/roj.2019.00220 (2019).
Tong, Y. S., Tan, J., Zhou, X. L., Song, Y. Q. & Song, Y. J. Systemic immune-inflammation index predicting chemoradiation resistance and poor outcome in patients with stage III non-small cell lung cancer. J. Transl. Med. 15, 221. https://doi.org/10.1186/s12967-017-1326-1 (2017).
Scilla, K. A. et al. Neutrophil-lymphocyte ratio is a prognostic marker in patients with locally advanced (Stage IIIA and IIIB) non-small cell lung cancer treated with combined modality therapy. Oncologist 22, 737–742. https://doi.org/10.1634/theoncologist.2016-0443 (2017).
Rossi, A. et al. Carboplatin- or cisplatin-based chemotherapy in first-line treatment of small-cell lung cancer: The COCIS meta-analysis of individual patient data. J. Clin. Oncol. 30, 1692–1698. https://doi.org/10.1200/jco.2011.40.4905 (2012).
Skarlos, D. V. et al. Randomized comparison of etoposide-cisplatin vs. etoposide-carboplatin and irradiation in small-cell lung cancer. A Hellenic Co-operative Oncology Group study. Ann. Oncol. 5, 601–607. https://doi.org/10.1093/oxfordjournals.annonc.a058931 (1994).
Pan, Z. et al. Cisplatin or carboplatin? Neutrophil to lymphocyte ratio may serve as a useful factor in small cell lung cancer therapy selection. Oncol. Lett. 18, 1513–1520. https://doi.org/10.3892/ol.2019.10459 (2019).
Liu, F., Zhou, S., Tan, L., Jiang, H. & Huang, Y. A retrospective cohort study on pretreated neutrophil-to-lymphocyte ratio and prognosis of small cell lung cancer: Evidence of effect modification by chemotherapy regimen. Cancer Manag. Res. 12, 10341–10352. https://doi.org/10.2147/cmar.S263863 (2020).
Mamdani, H., Matosevic, S., Khalid, A. B., Durm, G. & Jalal, S. I. Immunotherapy in lung cancer: Current landscape and future directions. Front. Immunol. 13, 823618. https://doi.org/10.3389/fimmu.2022.823618 (2022).
Esposito, G. et al. Immunotherapy in small cell lung cancer. Cancers https://doi.org/10.3390/cancers12092522 (2020).
El Sayed, R. & Blais, N. Immunotherapy in extensive-stage small cell lung cancer. Curr. Oncol. 28, 4093–4108. https://doi.org/10.3390/curroncol28050347 (2021).
Welsh, J. W. et al. Phase 1/2 trial of pembrolizumab and concurrent chemoradiation therapy for limited-stage SCLC. J. Thorac. Oncol. 15, 1919–1927. https://doi.org/10.1016/j.jtho.2020.08.022 (2020).
Liu, S. V. et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133). J. Clin. Oncol. 39, 619–630. https://doi.org/10.1200/jco.20.01055 (2021).
Liu, J. et al. Systemic immune-inflammation index, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio can predict clinical outcomes in patients with metastatic non-small-cell lung cancer treated with nivolumab. J. Clin. Lab. Anal. 33, e22964. https://doi.org/10.1002/jcla.22964 (2019).
Ksienski, D. et al. Prognostic significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio for advanced non-small cell lung cancer patients with high PD-L1 tumor expression receiving pembrolizumab. Transl. Lung Cancer Res. 10, 355–367. https://doi.org/10.21037/tlcr-20-541 (2021).
Hasegawa, T. et al. Association of high neutrophil-to-lymphocyte ratio with poor outcomes of pembrolizumab therapy in high-PD-L1-expressing non-small cell lung cancer. Anticancer Res. 39, 6851–6857. https://doi.org/10.21873/anticanres.13902 (2019).
Shiroyama, T. et al. Pretreatment advanced lung cancer inflammation index (ALI) for predicting early progression in nivolumab-treated patients with advanced non-small cell lung cancer. Cancer Med. 7, 13–20. https://doi.org/10.1002/cam4.1234 (2018).
Mountzios, G. et al. Association of the advanced lung cancer inflammation index (ALI) with immune checkpoint inhibitor efficacy in patients with advanced non-small-cell lung cancer. ESMO Open 6, 100254. https://doi.org/10.1016/j.esmoop.2021.100254 (2021).
Yilmaz, H. & Yersal, Ö. Prognostic significance of novel inflammatory markers in extensive-stage small-cell lung cancer. J. Cancer Res. Ther. 18, 691–696. https://doi.org/10.4103/jcrt.jcrt_1937_21 (2022).
Miller, K. L. et al. Routine use of approximately 60 Gy once-daily thoracic irradiation for patients with limited-stage small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 56, 355–359. https://doi.org/10.1016/s0360-3016(02)04493-0 (2003).
Roof, K. S., Fidias, P., Lynch, T. J., Ancukiewicz, M. & Choi, N. C. Radiation dose escalation in limited-stage small-cell lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 57, 701–708. https://doi.org/10.1016/s0360-3016(03)00715-6 (2003).
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT)(No.2019M3E5D1A01069361).
Author information
Authors and Affiliations
Contributions
DWP, SHL conceived the study and had a major role in the coordination of the study. DWP, SHL, JC, SC, BGK, TSP, HL, JYM, SJY, HJP and SHK managed the data collection and DWP, SHL, JC, THK and HJY performed statistical analysis and participated in data interpretation. DWP, SHL, JC, BGK, HL and JWS drafted the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seo, B.M., Choi, J., Chang, B. et al. Clinical significance of the advanced lung cancer inflammation index in patients with limited-stage small cell lung cancer treated with chemoradiotherapy. Sci Rep 14, 10347 (2024). https://doi.org/10.1038/s41598-024-61145-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61145-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.