Abstract
Right-sided infective endocarditis (RSIE) is less common than left-sided infective endocarditis (LSIE) and exhibits distinct epidemiological, clinical, and microbiological characteristics. Previous studies have focused primarily on RSIE in patients with intravenous drug use. We investigated the characteristics and risk factors for RSIE in an area where intravenous drug use is uncommon. A retrospective cohort study was conducted at a tertiary hospital in South Korea. Patients diagnosed with infective endocarditis between November 2005 and August 2017 were categorized into LSIE and RSIE groups. Of the 406 patients, 365 (89.9%) had LSIE and 41 (10.1%) had RSIE. The mortality rates were 31.7% in the RSIE group and 31.5% in the LSIE group (P = 0.860). Patients with RSIE had a higher prevalence of infection with Staphylococcus aureus (29.3% vs. 13.7%, P = 0.016), coagulase-negative staphylococci (17.1% vs. 6.0%, P = 0.022), and gram-negative bacilli other than HACEK (12.2% vs. 2.2%, P = 0.003). Younger age (adjusted odds ratio [aOR] 0.97, 95% confidence interval [CI] 0.95–0.99, P = 0.006), implanted cardiac devices (aOR 37.75, 95% CI 11.63–141.64, P ≤ 0.001), and central venous catheterization (aOR 4.25, 95% CI 1.14–15.55, P = 0.029) were independent risk factors for RSIE. Treatment strategies that consider the epidemiologic and microbiologic characteristics of RSIE are warranted.
Similar content being viewed by others
Introduction
Right-sided infective endocarditis (RSIE) constitutes approximately 5–10% of all cases of infective endocarditis (IE) and has distinct epidemiologic, clinical, and microbiological characteristics compared with those of left-sided infective endocarditis (LSIE)1,2,3. However, most previous studies of RSIE have focused on patients with intravenous drug use (IVDU), and limited information is available on the characteristics of RSIE in populations in which IVDU is uncommon2,4.
A study conducted in South Korea, where IVDU is not prevalent, revealed differences in the clinical features of RSIE compared with studies conducted in countries with a higher prevalence of IVDU5. These differences were attributed to a lower proportion of Staphylococcus aureus, and patients with RSIE and LSIE had similar mortality rates6,7,8. Risk factors for RSIE include central venous catheterization, intracardiac devices, congenital heart disease, and IVDU2.
As the population ages and underlying diseases increase, the number of patients with these risk factors is expected to rise. However, few studies have examined risk factors for RSIE in populations in which IVDU is uncommon. Therefore, our study aimed to investigate the clinical characteristics and risk factors of RSIE in South Korea, where IVDU is infrequent.
Methods
Study population
We retrospectively analyzed adult patients with IE who were admitted to Severance Hospital, a large tertiary care teaching hospital with 2,400 beds in South Korea, between November 2005 and August 2017. Patients with IE involving both sides were excluded from the study. The study received approval from the Institutional Review Board of Yonsei University Health System Clinical Trial Center (4–2018-0248), and the need for patient consent was waived due to the retrospective nature of the study. All methods were performed in accordance with the relevant guideline (STROBE checklist) and regulations.
IE was defined as definite or possible based on the Duke criteria, which were modified in 2000, and patients meeting these criteria were included in the study9. A multidisciplinary team comprising cardiologists, cardiovascular surgeons, and infectious disease specialists managed patients admitted for suspicion of IE. Surgery was performed in accordance with the guidelines of the American Heart Association and South Korea's national guidelines10,11. The appropriate surgical approach was determined through agreement among cardiologists, cardiovascular surgeons, and the advice of infectious disease specialists. Transesophageal echocardiography was conducted in most patients, including those with negative transthoracic echocardiographic findings.
Follow-up visits to the outpatient clinic were scheduled at 1 week and at 1, 3, 6, and 12 months after discharge. During each visit, patients underwent a systematic review and physical examination to assess evidence of heart failure and IE relapse. At the 6-month follow-up, echocardiography was performed to evaluate valvular and ventricular function. Subsequently, follow-up visits to the outpatient clinic were conducted every 6 months.
Variables and definitions
Nosocomial infection was defined as an infection occurring more than 48 h after hospitalization, with no evidence of infection at admission. It was also diagnosed if IE occurred within 60 days after hospital discharge when a high-risk procedure for bacteremia was performed or when any predisposing factor for IE was present during hospitalization, including dental manipulation, gastrointestinal manipulation, gynecological procedures, urological manipulation, and invasive intravascular techniques (intravascular device implantation, pacemaker insertion, and cardiac catheterization)12,13,14. Cardiac devices were defined as implantable pacemakers or defibrillators15.
The Charlson Comorbidity Index was used to categorize patients based on comorbidities identified on hospital admission16. The Sequential Organ Failure Assessment was used to stratify disease severity. Causative microorganisms were defined as those present in blood or tissue samples (valves and/or vegetation).
Mortality referred to all-cause mortality. Mortality data were obtained from the Ministry of the Interior and Safety of South Korea, which compiles mortality records of all Korean citizens. Mortality data were collected through September 2019.
Microbiological tests
Identification testing was performed using the VITEK 2 automated analyzer system (bioMérieux, Marcy-l’Étoile, France) until 2013. From 2013 onward, the Bruker Biotyper matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) system was used for identification testing (Bruker Daltonics, Bremen, Germany). Susceptibility tests were performed using the VITEK 2 automated analyzer system with a VITEK AST2 N212 card (bioMérieux). The results of antibiotic susceptibility testing were interpreted using the criteria of the Clinical and Laboratory Standards Institute17.
Statistical analysis
We evaluated the clinical and microbiological characteristics of LSIE and RSIE. Continuous variables were compared using the independent samples t-test or Mann–Whitney U-test, depending on the normality of distribution. Pearson’s chi-squared test was used to compare two categorical variables, and Fisher's exact test was used when the expected value of at least one cell was < 5. Kaplan–Meier survival analysis was performed to assess the long-term prognosis. Variables with a P-value of < 0.05 in the univariable analysis were included in the multivariable logistic regression model to identify independent risk factors for RSIE. The variance inflation factor (VIF) was used to assess multicollinearity, with a VIF value greater than 10 indicating multicollinearity. The goodness-of-fit was tested using the Hosmer–Lemeshow test. P-values < 0.05 were considered statistically significant. All statistical analyses were performed using R V.4.2.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Ethics approval and informed consent statement
This study was approved by the Institutional Review Board of Yonsei University Health System Clinical Trial Center (4–2018-0248). The requirement for patient consent was waived owing to the retrospective nature of the study.
Results
Study population and characteristics
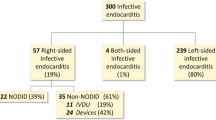
A total of 414 patients who met the inclusion criteria were initially enrolled in the study (Fig. 1). Of these patients, eight with involvement of both sides were excluded. The final analysis included 406 patients, of whom 365 and 41 were diagnosed with LSIE and RSIE, respectively.
The median age of patients with RSIE was 49 years (interquartile range [IQR]: 32–66 years), whereas that of patients with LSIE was 57 years (IQR: 44–68 years) (Table 1). Sex distribution did not differ significantly between the two groups (men: 67.1% vs. 53.7%, P = 0.121). A history of previous valve surgery was more prevalent in the RSIE group than in the LSIE group (18.1% vs. 34.1%, P = 0.025). The number of patients who had undergone cardiac device implantation was also higher in the RSIE group than in the LSIE group (1.4% vs. 31.7%, P < 0.001).
Among the patients with RSIE, 26 (63.4%) had tricuspid valve involvement, whereas 15 (36.6%) had pulmonary valve involvement. Transthoracic echocardiography was performed in most of the patients, with no difference in frequency between those with RSIE and LSIE. Transesophageal echocardiography was performed more frequently in patients with LSIE than in those with RSIE (73.4% of LSIE cases and 43.9% of RSIE cases; P < 0.001). The presence of large vegetations, > 2 cm in diameter, was more commonly observed in the RSIE group than in the LSIE group (22.0% vs. 10.1%, P = 0.045).
Patients with RSIE involving the pulmonary valve and those with RSIE involving the tricuspid valve were compared (Supplementary Table S1). Patients with pulmonary valve IE were younger than those with tricuspid valve IE (44 vs. 58 years, P = 0.010). In the pulmonary valve IE group, a higher proportion of patients had predisposing factors for IE, including 11 (73.3%) with a history of valve surgery and 4 (26.7%) with cardiac devices. In the tricuspid valve IE group, only 3 patients (11.5%) had a history of undergoing valve surgery. Of the 15 pulmonary valve IE cases, 13 (86.7%) had congenital heart disease, including patent ductus arteriosus, tetralogy of Fallot, pulmonary atresia, and ventricular septal defect.
Clinical outcomes
In the RSIE group, 21 patients (51.2%) underwent surgery; in the LSIE group, 243 patients (66.6%) underwent surgical intervention (P = 0.075). In the RSIE group, embolism prevention was the most common surgical indication (n = 13; 31.7%), followed by heart failure (n = 12; 29.3%). Heart failure (65.8% vs. 29.3%, P < 0.001) and paravalvular complications (17.3% vs. 0.0%, P = 0.008), as surgical indications, were observed more frequently in the LSIE group than in the RSIE group.
Overall, the outcomes of the two groups were similar (Table 2). In the RSIE group, four patients (9.8%) died during their hospital stay, which did not differ significantly from the mortality rate in the LSIE group (n = 53, 14.5%, P = 0.551). The overall mortality rates were 31.7% in patients with RSIE and 31.5% in patients with LSIE. Kaplan–Meier curves showed that the overall survival rates of the two groups did not differ significantly (P = 0.860, log-rank test) (Fig. 2). The median follow-up duration was 1,829 days (IQR: 558.75–3104.25 days).
Microbiological characteristics
Microbiological analyses revealed several differences in the distribution of microorganisms between the LSIE and RSIE groups. Patients with RSIE showed higher prevalence of infection with S. aureus (LSIE: 13.7% vs. RSIE: 29.3%, P = 0.016), coagulase-negative staphylococci (CoNS) (LSIE: 6.0% vs. RSIE: 17.1%, P = 0.022), and gram-negative bacilli (GNB) other than HACEK (Haemophilus parainfluenzae, Haemophilus aphrophilus, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae) (LSIE: 2.2% vs. RSIE: 12.2%, P = 0.003) (Table 3). In contrast, streptococcal infections were more common in the LSIE group than in the RSIE group (LSIE: 38.1% vs. RSIE: 14.6%, P = 0.005).
Methicillin-resistant staphylococci were more common in patients with RSIE. Methicillin-resistant S. aureus (MRSA) and methicillin-resistant CoNS were found in 12.2% of patients with RSIE, and 5.8% and 3.8% of patients with LSIE, respectively. Methicillin resistance was observed in 41.7% of patients with RSIE and 42.0% of patients with LSIE infected with S. aureus, and in 71.4% of patients with RSIE and 63.6% of patients with LSIE infected with CoNS. Overall, methicillin-resistant staphylococci accounted for 24.4% and 9.6% of all cases of RSIE and LSIE, respectively.
Risk factors for right-sided infective endocarditis
Univariate analysis revealed that younger age, history of valve surgery, implanted cardiac devices, recent antibiotic use, and central venous catheterization were associated with RSIE (Table 4). The multivariable model identified that RSIE was independently associated with age (aOR: 0.97, 95% CI: 0.95–0.99, P = 0.006), implanted cardiac devices (aOR: 37.75, 95% CI: 11.63–141.64; P < 0.001), and central venous catheters (aOR: 4.25, 95% CI: 1.14–15.55, P = 0.029; Table 4).
Discussion
This study revealed the distinct bacterial causes and clinical manifestations of RSIE and LSIE. Patients with RSIE are more likely to have predisposing factors such as a history of valve surgery, implanted cardiac devices, and central venous catheter placement. Patients with RSIE also tended to have larger vegetations and a higher prevalence of infection with S. aureus, CoNS, and GNB other than HACEK, compared with patients with LSIE. The risk of death did not differ significantly between the two groups. The risk factors for RSIE were younger age, implanted cardiac devices, and central venous catheterization.
The risk factors for RSIE identified in this study align with those reported in previous studies, although the presence of congenital heart disease was not investigated2. Currently, commonly used implantable cardiac devices include pacemakers, implantable cardioverter defibrillators, and cardiac resynchronization therapy implants18. The leads of these cardiac devices’ are primarily positioned in the right heart, and this anatomical arrangement appears to be associated with the occurrence of IE. In patients with pacemakers, approximately two-thirds show valvular involvement, with tricuspid valve involvement19. observed in about 60% of pacemaker-lead IE cases.
Central venous catheter insertion is also a common risk factor. The potential mechanism is believed to involve the abrasion of the tricuspid leaflet and endocardium because of the close proximity to the tricuspid valve and the forceful and rapid jet of injections through the catheter20. Several studies have compared the infection risk between central venous catheters and peripherally inserted central catheters (PICCs), with discrepancies in their findings21,22,23. According to a previous meta-analysis, the degree of infection risk associated with PICCs was found to be similar to that with central venous catheters in inpatient settings but lower in outpatient settings24.
In addition, young age was found to be a risk factor for RSIE in this study. This finding is attributable to the increased involvement of the pulmonary valve observed in patients with RSIE. The median age of patients with tricuspid valve involvement was 58 years, which was comparable to that of patients with LSIE (57 years). In patients with pulmonary valve IE, the median age was 44 years, which was significantly lower. Although previous studies on RSIE associated with IVDU have reported tricuspid valve involvement in a high percentage of patients and considered pulmonary valve involvement to be rare, this study showed a substantial proportion (36.6%) of patients with RSIE with pulmonary valve involvement6,25,26. This age difference in pulmonary valve IE and the higher incidence of pulmonary valve involvement probably contribute to the higher occurrence of RSIE at a younger age.
Regarding microbiology, this study showed a higher prevalence of S. aureus, CoNS, and GNB other than HACEK infections in RSIE compared with LSIE. S. aureus is the most common causative pathogen in RSIE, accounting for 60%–90% of cases2. In our study, S. aureus was the most common causative microorganism, constituting 29.3% of RSIE cases, which is substantially lower than the previous study. This discrepancy is likely attributable to the regional characteristics of the lower IVDU in our study population. When comparing our study with previous research conducted in the same region, the prevalence of S. aureus infections was similar5.
We also observed a relatively high prevalence of CoNS infection and a relatively low prevalence of streptococcal infection. These differences in microbiology are likely to be associated with the increased incidence of RSIE in patients with implanted cardiac devices and central catheters. Staphylococcal species are the major causative microorganisms of pacemaker infections, accounting for 70–95% of cases27. The most common causative organisms of catheter-related bloodstream infections are CoNS, S. aureus, Candida species, and enteric GNB28. In RSIEs not associated with IVDUs, the microbiology is related to that of pacemaker and catheter-related infections—infections associated with these conditions are common in RSIE.
Infections caused by non-HACEK GNBs are infrequent in IE. The International Collaboration on Endocarditis reported that only 1.8% of IE cases were non-HACEK GNB infections29. Similarly, in this study, infections caused by GNB accounted for only 2.2% of cases of LSIE. However, 12.2% of cases of RSIE were GNB infections, a significantly higher proportion than that in LSIE cases. The current guidelines for empiric treatment of IE do not differentiate between RSIE and LSIE and focus mainly on infections caused by gram-positive organisms2. Based on the results of this study, about 10% of RSIE patients may receive inappropriate empirical antibiotics if treated according to the guidelines. Therefore, further research is needed on risk factors and treatment strategies for GNB infection in RSIE, and further consideration of empirical treatment may be warranted based on the epidemiologic and microbiologic characteristics of RSIE.
Methicillin-resistant staphylococcal infections accounted for approximately 25% of all patients with RSIE. Among cases of staphylococcal infection, methicillin resistance was observed in 41.7% of patients with S. aureus infection and 71.4% of patients with CoNS infection. This finding indicates a notably high rate of methicillin resistance. Additionally, when considering nosocomial infections alone, methicillin resistance was observed in 58.3% of all patients with RSIE. Community-acquired infections exhibited a lower resistance rate, with 10.3% of the patients showing methicillin resistance. Therefore, methicillin resistance should be considered in RSIE, particularly in patients with nosocomial infections.
Furthermore, this study revealed a higher incidence of large vegetations (≥ 2 cm) in patients with RSIE, with 22% of patients with RSIE having large vegetations. A study conducted in the same region also reported a high prevalence of large vegetations (33.3%)5. In both studies, the incidence of large vegetations in LSIE was approximately 10%, which is significantly lower than the rates observed in patients with RSIE. In a study on IVDU-related IE, 15.3% of individuals with IE had large vegetations. This finding suggests that large vegetation is more common in patients with RSIE in regions where IVDU is less common30. Given the previous findings that large vegetation is a poor prognostic factor for in-hospital mortality in RSIE, identifying the presence of these large vegetation types in RSIE is important owing to its potential association with unfavorable patient outcomes30. Therefore, conducting further research to establish early diagnostic strategies for RSIE may help improve the patient’s prognosis.
This study also showed no significant difference in long-term mortality between the RSIE and LSIE groups. The overall mortality rates for LSIE and RSIE were 31.5% and 31.7%, respectively, with no significant difference. A study conducted in countries with low IVDU rates also found no difference in in-hospital mortality between the two groups, whereas a study on IVDU-related IE showed favorable long-term survival of patients with RSIE5,31. The median age of patients with IVDU-related IE was 39 years, significantly younger than those without non-IVDU-related IE31. However, in this study, the median age of patients with RSIE was 49 years, suggesting enrolment of older patients than the previous study. Additionally, there were no significant differences in comorbidities between the RSIE and LSIE groups, which may have contributed to the lack of significant differences in long-term outcomes. Therefore, we hypothesize that the better prognosis of RSIE compared to LSIE is a result of inter-study differences in patient age and comorbidities rather than the nature of the disease.
Several limitations should be considered when interpreting the results of this study. It was a retrospective cohort study conducted in a single large tertiary hospital in South Korea, potentially introducing selection bias and limiting its ability to fully represent the entire population of individuals with IE. Additionally, the small number of patients with RSIE may pose a challenge when interpreting the data. Detailed information on IVDU may not have been thoroughly investigated owing to the regional characteristics in which IVDU is less common.
Despite the limitations, our findings are meaningful because RSIE is rare in areas of low IVDU prevalence. One study has evaluated the characteristics of RSIE in areas of low IVDU prevalence, and it included 39 cases of RSIE5, a similar number of RSIE cases to this work. Considering the low incidence of RSIE, a multicenter prospective cohort study may be warranted to provide a more comprehensive description of the disease characteristics.
Conclusion
In regions with a low IVDU prevalence, RSIE demonstrated a higher incidence of infection with S. aureus, CoNS, and GNB other than HACEK. Methicillin resistance can be considered in RSIE, particularly in patients who developed nosocomial infections. Overall mortality did not differ between the RSIE and LSIE groups. Younger age, implanted cardiac devices, and central venous catheterization were identified as the risk factors for RSIE. With the increased use of cardiac devices and central venous catheters, the increasing incidence of RSIE is a potential concern and treatment strategies that consider epidemiologic and microbiologic characteristics of RSIE is warranted.
Data availability
The datasets used for the current study are available from the corresponding author upon reasonable request.
References
Frontera, J. A. & Gradon, J. D. Right-side endocarditis in injection drug users: Review of proposed mechanisms of pathogenesis. Clin. Infect. Dis. 30, 374–379 (2000).
Habib, G. et al. ESC guidelines for the management of infective endocarditis: The task force for the management of infective endocarditis of the European society of cardiology (ESC). Endorsed by: European association for cardio-thoracic surgery (EACTS), the European association of nuclear medicine (EANM). Eur. Heart J. 36, 3075–3128 (2015).
Wilson, L. E., Thomas, D. L., Astemborski, J., Freedman, T. L. & Vlahov, D. Prospective study of infective endocarditis among injection drug users. J. Infect. Dis. 185, 1761–1766 (2002).
Akinosoglou, K., Apostolakis, E., Marangos, M. & Pasvol, G. Native valve right sided infective endocarditis. Eur. J. Intern. Med. 24, 510–519 (2013).
Lee, M. R. et al. Clinical features of right-sided infective endocarditis occurring in non-drug users. J. Korean Med. Sci. 29, 776–781 (2014).
Mathew, J. et al. Clinical features, site of involvement, bacteriologic findings, and outcome of infective endocarditis in intravenous drug users. Arch. Intern. Med. 155, 1641–1648 (1995).
Gray, M. E., Rogawski McQuade, E. T., Scheld, W. M. & Dillingham, R. A. Rising rates of injection drug use associated infective endocarditis in Virginia with missed opportunities for addiction treatment referral: A retrospective cohort study. BMC Infect. Dis. 18, 532 (2018).
Hecht, S. R. & Berger, M. Right-sided endocarditis in intravenous drug users. prognostic features in 102 episodes. Ann. Intern. Med. 117, 560–566 (1992).
Li, J. S. et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin. Infect. Dis. 30, 633–638 (2000).
Baddour, L. M. et al. Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the American heart association. Circulation 132, 1435–1486 (2015).
The Korean Society for Thoracic and Cardiovascular Surgery. Clinical guideline for the diagnosis and treatment of cardiovascular infections. Infect. Chemother. 43, 129–177 (2011).
Chirio, D. et al. Factors associated with unfavorable outcome in a multicenter audit of 100 infective endocarditis. Eur. J. Clin. Microbiol. Infect. Dis. 38, 109–115 (2019).
Martín-Dávila, P. et al. Nosocomial endocarditis in a tertiary hospital: An increasing trend in native valve cases. Chest 128, 772–779 (2005).
Hwang, J. W. et al. Risk factors for poor prognosis in nosocomial infective endocarditis. Korean J. Intern. Med. 33, 102–112 (2018).
Sy, R. W., Chawantanpipat, C., Richmond, D. R. & Kritharides, L. Development and validation of a time-dependent risk model for predicting mortality in infective endocarditis. Eur. Heart J. 32, 2016–2026 (2011).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 40, 373–383 (1987).
P, W. USA: Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: 26th Informational Supplement. CLSI document M100S (ISBN 1–56238–923–8) (2016).
Gadler, F., Valzania, C. & Linde, C. Current use of implantable electrical devices in Sweden: Data from the Swedish pacemaker and implantable cardioverter-defibrillator registry. Europace 17, 69–77 (2015).
Duval, X. et al. Endocarditis in patients with a permanent pacemaker: A 1-year epidemiological survey on infective endocarditis due to valvular and/or pacemaker infection. Clin. Infect. Dis. 39, 68–74 (2004).
Kale, S. B. & Raghavan, J. Tricuspid valve endocarditis following central venous cannulation: The increasing problem of catheter related infection. Indian J. Anaesth. 57, 390–393 (2013).
Gunst, M. et al. Peripherally inserted central catheters may lower the incidence of catheter-related blood stream infections in patients in surgical intensive care units. Surg. Infect. Larchmt. 12, 279–282 (2011).
Pitiriga, V. et al. Lower risk of bloodstream infections for peripherally inserted central catheters compared to central venous catheters in critically ill patients. Antimicrob. Resist. Infect. Control 11, 137 (2022).
Al Raiy, B. et al. Peripherally inserted central venous catheters in the acute care setting: A safe alternative to high-risk short-term central venous catheters. Am. J. Infect. Control 38, 149–153 (2010).
Chopra, V., O’Horo, J. C., Rogers, M. A., Maki, D. G. & Safdar, N. The risk of bloodstream infection associated with peripherally inserted central catheters compared with central venous catheters in adults: A systematic review and meta-analysis. Infect. Control Hosp. Epidemiol. 34, 908–918 (2013).
Weber, C. et al. Characteristics and outcomes of patients with right-sided endocarditis undergoing cardiac surgery. Ann. Cardiothorac. Surg. 8, 645–653 (2019).
Hussain, S. T. et al. Rarity of invasiveness in right-sided infective endocarditis. J. Thorac. Cardiovasc. Surg. 155, 54-61.e51 (2018).
Chambers, S. T. Diagnosis and management of staphylococcal infections of pacemakers and cardiac defibrillators. Intern. Med. J. 35(Suppl 2), S63-71 (2005).
Mermel, L. A. et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the infectious diseases society of America. Clin. Infect. Dis 49, 1–45 (2009).
Morpeth, S. et al. Non-HACEK gram-negative bacillus endocarditis. Ann. Intern Med. 147, 829–835 (2007).
Martín-Dávila, P. et al. Analysis of mortality and risk factors associated with native valve endocarditis in drug users: The importance of vegetation size. Am. Heart J. 150, 1099–1106 (2005).
Thalme, A., Westling, K. & Julander, I. In-hospital and long-term mortality in infective endocarditis in injecting drug users compared to non-drug users: A retrospective study of 192 episodes. Scand. J. Infect. Dis. 39, 197–204 (2007).
Acknowledgements
We appreciate the Medical Illustration & Design(MID) team, a member of Medical Research Support Services of Yonsei University College of Medicine, for their excellent support with medical illustration.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Science and ICT) (No. 2022R1C1C1010012) (N.S.K) and a faculty research grant of Yonsei University College of Medicine (6–2023-0084).
Author information
Authors and Affiliations
Contributions
Conceptualization Y.L. Data curation J.H.K. Formal analysis and investigation Y.L. Writing—original draft Y.L. and J.H.K. Writing—review and editing: all authors; Funding acquisition: N.S.K. Supervision J.H.K., J.Y.A., S.J.J., J.Y.C., J.S.Y., S.H.L., and N.S.K.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, Y., Kim, J.H., Lee, J.A. et al. Clinical characteristics and risk factors for right-sided infective endocarditis in Korea: a 12-year retrospective cohort study. Sci Rep 14, 10466 (2024). https://doi.org/10.1038/s41598-024-60638-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60638-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.