Abstract
The benefits of intravascular ultrasonography (IVUS)-guided percutaneous coronary intervention (PCI) in the clinical context of cardiogenic shock (CS) complicating acute myocardial infarction are lacking. We aimed to investigate the impact of IVUS-guided PCI in patients with AMI and CS. From the pooled data based on a series of Korean AMI registries during 2011–2020, we identified 1418 consecutive patients who underwent PCI with second generation drug-eluting stent (DES) for AMI and CS. The primary endpoint was the 1-year rate of target lesion failure (TLF), defined as the composite of cardiac death, target vessel myocardial infarction, and ischemic-driven target lesion revascularization. In total, 294 (20.7%) and 1124 (79.3%) underwent IVUS-guided and angiography-guided PCI with second generation DES implantation, respectively. The 1-year TLF was not significantly different between groups after IPTW analysis (hazard ratio 0.93, 95% confidence interval 0.65–1.34, p = 0.70). Additionally, the adjusted landmark analysis for TLF at 30 days and between 30 days and 1 year after PCI demonstrated no significant difference between the groups. In conclusion, in patients with AMI and CS who underwent PCI with second-generation DES, IVUS-guided PCI did not improve the 1-year TLF compared with angiography-guided PCI.
Registration: URL: http://cris.nih.go.kr. KCT0000863 and KCT0008355.
Similar content being viewed by others
Introduction
Cardiogenic shock (CS) accompanies 3–10% of acute myocardial infarctions (AMIs), with combined AMI and CS showing worse short- and long-term clinical outcomes than AMI without CS1 Despite mortality reduction by 40–50% from early revascularization2, AMI complicated by CS remains a leading cause of death3. This is further evidenced by a recent increase in mortality rates owing to an increase in comorbidities in the aging population4. Therefore, an early invasive strategy with appropriate revascularization is crucial for successful treatment in this population2, along with critical care including fluid administration and inotropic supports5.
Intravascular ultrasonography (IVUS) offers critical insights on lesion characteristics, enabling optimal stent deployment. IVUS also plays a pivotal role in detecting suboptimal stent results and improving percutaneous coronary intervention (PCI) outcomes6. Therefore, it has been widely used in the contemporary PCI era7. Two recent AMI registries demonstrated that IVUS-guidance improved the long-term clinical outcomes of PCI8,9.
However, data regarding the benefits of IVUS-guided PCI in the clinical context of CS complicating AMI are lacking. Therefore, this study aimed to investigate the clinical impact of IVUS-guided versus angiography-guided PCI in patients with AMI and CS.
Methods
Patients
The Korean Acute Myocardial Infarction Registry (KAMIR) registry was designated to evaluate real-world long-term clinical outcomes of patients with AMI. The KAMIR-National Institute of Health (NIH) (KCT-0000863) includes patients with AMI between November 2011 and December 201510, whereas the KAMIR-V (KCT-0008355) includes patients with AMI between January 2016 and June 202011. These registries encompass nationwide, multicenter and prospective observational cohorts supported by the Korean Working Group of Acute Myocardial Infarction. The 20 and 43 centers that participated in the KAMIR-NIH and KAMIR-V, respectively, were equipped for primary PCI and on-site cardiac surgery. The ethics committees of each participating center approved the study protocol. This study complied with the tenets of the Declaration of Helsinki. All patients provided written informed consent upon enrollment.
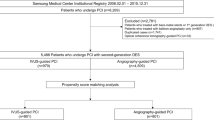
Among 28,949 consecutive patients with AMI between 2011 and 2020, we selected 2,095 patients with AMI and CS (Fig. 1). CS was defined as systolic blood pressure < 90 mmHg for > 30 min or the need for supportive management to maintain systolic blood pressure > 90 mmHg; clinical signs of pulmonary congestion; and evidence of impaired end-organ perfusion with at least one of the following: cool extremities, decreased urine output, increased lactic acid level, or altered mental status2. The exclusion criteria were no CS; out-of-hospital cardiac arrest; thrombolysis; no PCI or history of PCI without stenting; treatment with a bare metal stent, first-generation DES, or bioresorbable vascular scaffold; history of optical coherence tomography guidance; missing data for IVUS use; and loss to follow-up. Patients who were discharged but never visited the outpatient department again were considered lost to follow-up.
Treatment
Patients diagnosed with AMI were treated according to contemporary guidelines12,13. The strategy for revascularization, techniques, vascular access, selection of devices, and adjunctive antithrombotic therapy including glycoprotein IIb/IIIa inhibitor were left to the discretion of each physician. All procedures were performed in accordance with standard interventional techniques. The decision to use IVUS was at the operator’s discretion. Patients were recommended to receive optimal pharmacological therapy after PCI according to standard guidelines. For cardiogenic shock management, the use of intra-aortic balloon pump (IABP), extracorporeal membrane oxygenation (ECMO), and inotropic agents was also determined at the operator’s discretion.
Endpoints
The primary endpoint was target lesion failure (TLF), defined as the composite of cardiac death, target vessel myocardial infarction (TV-MI), and ischemia-driven target lesion revascularization (ID-TLR) at 1 year after the index procedure. The secondary endpoints included all-cause mortality; individual components of TLF; definite/probable stent thrombosis as defined by the Academic Research Consortium14; and major adverse cardiovascular events (MACEs), including death from any cause, myocardial infarction (MI), and revascularization. Clinical outcomes at 30 days and between 30 days and 1 year were also compared. All-cause mortality was regarded as cardiac death unless a definite noncardiac cause was identified. TV-MI was defined as MI with evidence of myocardial necrosis in the vascular territory of a previously treated target vessel. Target lesion revascularization was considered ischemia-driven if any revascularization including PCI or bypass surgery for the target lesion was performed in ≥ 50% angiographic diameter stenosis with ischemic symptoms, positive results on a functional study, or ≥ 70% angiographic diameter stenosis with or without documented ischemia.
Statistical analysis
Data are presented as the mean ± standard deviation (SD) for continuous variables and frequency (percentage) for categorical variables. Between-group comparisons were performed using the independent two sample t-test for continuous variables and the chi‐squared or Fisher’s exact test for categorical variables as appropriate. The mean imputation for missing value of laboratory findings was performed to minimize the sample size loss. The cumulative incidence rate of clinical endpoints was estimated using the Kaplan–Meier method and compared between groups using the log-rank test. Cox proportional hazard regression analyses were performed to calculate hazard ratio (HR) with 95% confidence interval (CI) for each clinical endpoint associated with IVUS- or angiography-guided PCI. Landmark analysis was conducted at 30 days after PCI. Inverse probability of treatment weighting (IPTW) was used to adjust for confounding factors. The propensity score (PS) was estimated using multiple logistic regression analysis with all covariates. The standardized mean difference (SMD) was used to assess the balance of covariate distribution between the groups. Covariates with an SMD < 0.1 were considered balanced. The cumulative incidence rate of clinical endpoints was calculated using the IPTW-adjusted Kaplan–Meier estimators and compared between groups using IPTW-adjusted log-rank test. We also conducted sensitivity analyses using PS matching to enhance the validity of our results. The IVUS and angiography groups were matched in a 1:2 ratio without replacement using the nearest-neighbor method based on a PS with a 0.1-caliper width. Additionally, we performed univariable and multivariable logistic regression analyses to identify the determinants for IVUS use. Significant variables (i.e., P < 0.10) in the univariable analysis were included in the multivariable analysis. All statistical analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC, USA) and R software (version 4.1.1; R Foundation for Statistical Computing, Vienna, Austria). P < 0.05 was considered significant.
Results
Baseline characteristics
The baseline characteristics are summarized in Tables 1 and 2. Overall, 1418 patients were evaluated: 294 (20.7%) underwent IVUS-guided PCI, and 1124 (79.3%) underwent angiography-guided PCI with second-generation DES implantation. The mean age was 66.6 ± 12.3 years, and 75.1% of the patients were men. In total, 1138 patients (80.3%) presented with ST-segment elevation myocardial infarction (STEMI). The IVUS-guided PCI group was younger and had a higher frequency of prior MI history. The left ventricular ejection fraction was similar between the groups. Although the proportion of multivessel disease was higher in the IVUS-guided PCI group, the proportion of patients treated with culprit-only PCI strategy among patients with multivessel disease was not significantly different. Regarding the lesion profiles, the proportion of culprit vessels located in the left main artery and prevalence of type B2/C lesion were higher in the IVUS-guided PCI group. During the procedure, 18.2% of patients required hemodynamic support devices. The proportion of transradial approach and use of glycoprotein IIb/IIIa inhibitors were higher in the IVUS-guided PCI group. The IVUS-guided PCI group showed a higher number of implanted stents (1.33 ± 0.55 vs. 1.16 ± 0.40; p < 0.01), larger implanted stent diameter (3.27 ± 0.51 mm vs. 3.16 ± 0.43 mm; p < 0.01), and longer implanted stent (34.9 ± 18.7 mm vs. 30.3 ± 14.2 mm; p < 0.01). After PS matching and IPTW adjustment, the standardized differences between the groups were < 10.0% for all variables, indicating appropriate matching (Supplementary Tables S1 and S2).
One-year clinical outcomes
Fig. 2, Table 3, and Supplementary Fig. S3 present the comparison of 1-year clinical outcomes between the IVUS- and angiography-guided PCI groups. The median follow-up duration was 360 days (interquartile range, 284–382 days). Overall, 311 TLFs (21.9%; 286 cardiac deaths, 7 TV-MI, and 27 ID-TLRs) occurred during the 1-year follow-up. The risk of TLF at 1 year was significantly lower in the IVUS-guided PCI group, but there was no difference after multiple sensitivity analyses (multivariable adjusted HR: 0.74; 95% CI 0.54–1.05; p = 0.10, PS-matched HR: 0.86; 95% CI 0.57–1.29; p = 0.47, and IPTW-adjusted HR: 0.93; 95% CI 0.65–1.34; p = 0.70). Regarding the secondary outcomes, risk of MACE, all-cause death, and cardiac death did not significantly differ between the two groups after adjustment, although the unadjusted analyses showed significantly lower rates in the IVUS‐guided PCI group. There was no significant between-group difference in the risk of any MI, TV-MI, any revascularization, ID-TLR, and definite/probable stent thrombosis. The risk of TLF and MACE were comparable between the groups in both patients with STEMI and with NSTEMI (Supplementary Tables S3 and S4). No significant interaction was observed in the subgroup analyses (Supplementary Fig. S4).
Thirty-day outcome and landmark analysis
Supplementary Tables S5 and S6, and Fig. 3 present the clinical outcomes at 30 days and between 30 days and 1 year of follow-up in the IVUS- and angiography-guided PCI groups. Regarding short-term clinical outcomes, although the unadjusted rates for 30-day TLF and MACE were significantly lower in the IVUS‐guided PCI group, multivariable, PS matching, and IPTW adjustment revealed that the risks of 30-day TLF and MACE, all-cause death, and cardiac death did not differ significantly between the two groups. TLF and MACE also did not differ before and after multiple sensitivity analyses.
Major factors influencing IVUS usage
In total, 7.2% (2095/28,949) patients were treated for CS complicating AMI between 2011 and 2020. Among them, 18.6% (354/1907) of patients underwent PCI with IVUS guidance, and the remaining 81.4% (1553) underwent PCI with angiography guidance. Among patients with AMI accompanied by CS, the rate of IVUS utilization has consistently remained over 10% (Fig. 4) in patients who underwent PCI. The primary factors for IVUS usage were younger patients (aged < 65 years), prior MI, left main disease, and multiple stent implantation (Table 4). Although not significant, there was a trend towards higher IVUS utilization in patients with NSTEMI than in patients with STEMI.
Discussion
The main findings of the present study were as follows (Central Illustration). First, there was no difference in 1-year TLF risk between the IVUS- and angiography-guided PCI groups after adjustment for confounding factors. Second, the adjusted landmark analysis for TLF and MACE showed no significant differences between the two groups at within 30 days and between 30 days and 1 year. Third, the major factors for IVUS usage were younger patients, prior MI, left main disease, and multiple stent implantation.
IVUS-guided PCI is associated with better clinical outcomes than angiography-guided PCI in the second-generation DES era15,16. However, previous studies excluded patients with CS. Two AMI registries demonstrated that IVUS-guided PCI improved long-term clinical outcomes compared with angiography-guided PCI in real-world practice. However, one study using the KAMIR-NIH registry excluded patients with CS, whereas in another AMI registry, only approximately 8.7% (855/9846) of the patients had CS. Furthermore, no further subgroup analysis was conducted for patients with CS8,9. The role of intravascular imaging during revascularization is also not mentioned in the current guideline for the management of CS complicating MI17. Therefore, the importance of this study lies in its primary focus on comparing clinical outcomes between IVUS and angiography guidance in patients with CS derived from a dedicated AMI registry.
In this study, IVUS was consistently utilized in PCI procedures for 13–25% of all patients diagnosed with AMI and CS. The unusually high rate of IVUS penetration in the clinical context of AMI and CS might be attributed to several factors. First, the positive outcomes observed in randomized trials and dedicated AMI registries with IVUS guidance may have influenced the operators to choose PCI optimization even in patients with AMI and CS. Furthermore, the presence of left main disease was associated with IVUS utilization in the current study. Because current guidelines recommend IVUS guidance for left main-PCI, the operators may have faithfully adhered to this guideline in cases of CS complicating AMI18. Second, IVUS guidance was selected for patients with a history of MI and those undergoing multiple stent implantation, as they are considered as having high risk for subsequent ischemic events. Therefore, IVUS for these patients is aimed to minimize the risk of future ischemic events. Third, physicians seemed to favor IVUS-guided PCI among relatively young patients (age < 65 years), anticipating its long-term benefits in reducing the risk of ischemic event. Indeed, IVUS-guided PCI consistently reduced ischemic risks even beyond the 1-year follow up19. However, IVUS-guided PCI in patients with AMI and CS in the present study did not improve TLF reflecting ischemic events compared with angiography-guided PCI in the same population. In the landmark analysis, IVUS-guided PCI also did not reduce ischemic risk between 30 days and 1 year after the index procedure compared with angiography-guided PCI. Notably, the IVUS group showed an equal TLR rate to that of angiography alone despite the greater complexity of the PCI procedure. These results may offer valuable insights for physicians in prioritizing treatment strategies in the challenging scenario of CS complicating AMI. Nevertheless, the benefit of IVUS use in particular patients, such as those with distal lesions of the left main artery of with confusing angiographic findings, cannot be excluded.
Given the substantial predictive value of CS in relation to stent thrombosis20, physicians have made efforts to optimize stent deployment under IVUS guidance, aiming to minimize acute or subacute ischemic events. However, adjusted landmark analysis from the present study showed no difference in 30-day clinical outcomes between the IVUS- and angiography-guided PCI groups. In the future, a well-designed, large scale randomized trial is needed to identify a specific patient subgroup in whom IVUS-guided PCI could enhance the clinical outcomes for individuals with AMI and CS.
Limitations
First, the non-randomized observational design introduced inherent selection and information biases. Using physician discretion to determine treatment strategy inevitably introduced the possibility of selection bias. Furthermore, the number of patients was largely different between the groups. Although, extensive sensitivity analyses were conducted to adjust for the measured or unmeasured confounding factors to minimize the bias from different baseline characteristics, the possibility of unmeasured confounders influencing the findings cannot be excluded. Second, despite the pooled analyses, differences between centers and operator’s experiences on IVUS may affect the findings. Third, the decision to use IVUS was made at the operator’s discretion. Fourth, detailed procedural data were missing. Additionally, we did not have the timing of intravascular imaging relative to the PCI procedure. Therefore, the use of IVUS-guided PCI did not guarantee the optimization of PCI, and the findings should be interpreted cautiously. Fifth, detailed procedural data procedure time, and total amount of contrast media were unavailable. Finally, procedure-related risks were not evaluated.
In conclusion, IVUS-guidance did not improve the 1-year TLF compared with angiography-guidance in patients with AMI and CS who underwent PCI with second-generation DES. Further, risk of TLF at 30 days and between 30 days and 1 year after PCI were also comparable between the two groups. The factors for IVUS usage were younger age, prior MI, LM coronary artery disease, and multiple stent implantation.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Goldberg, R. J. et al. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: A population-based perspective. Circulation 119(9), 1211–1219. https://doi.org/10.1161/CIRCULATIONAHA.108.814947 (2009).
Hochman, J. S. et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. N. Engl. J. Med. 341(9), 625–634. https://doi.org/10.1056/NEJM199908263410901 (1999).
Thiele, H. et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N. Engl. J. Med. 377(25), 2419–2432. https://doi.org/10.1056/NEJMoa1710261 (2017).
Wayangankar, S. A. et al. Temporal trends and outcomes of patients undergoing percutaneous coronary interventions for cardiogenic shock in the setting of acute myocardial infarction: A report from the CathPCI Registry. JACC Cardiovasc. Interv. 9(4), 341–351. https://doi.org/10.1016/j.jcin.2015.10.039 (2016).
Van Diepen, S. et al. Contemporary management of cardiogenic shock: A scientific statement from the American Heart Association. Circulation 136(16), e232–e268. https://doi.org/10.1161/CIR.0000000000000525 (2017).
Maehara, A. et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents. Circ. Cardiovasc. Interv. 11(11), e006243. https://doi.org/10.1161/CIRCINTERVENTIONS.117.006243 (2018).
Members, W. C. et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 79(2), e21–e129. https://doi.org/10.1016/j.jacc.2021.09.006 (2022).
Choi, I. J. et al. Impact of intravascular ultrasound on long-term clinical outcomes in patients with acute myocardial infarction. JACC Cardiovasc. Interv. 14(22), 2431–2443. https://doi.org/10.1016/j.jcin.2021.08.021 (2021).
Kim, Y. et al. Role of intravascular ultrasound-guided percutaneous coronary intervention in optimizing outcomes in acute myocardial infarction. J. Am. Heart Assoc. 11(5), e023481. https://doi.org/10.1161/JAHA.121.023481 (2022).
Kim, J. H. et al. Multicenter cohort study of acute myocardial infarction in Korea–interim analysis of the Korea acute myocardial infarction registry-national institutes of health registry. Circ. J. 80(6), 1427–1436. https://doi.org/10.1253/circj.CJ-16-0061 (2016).
Kim, M. H. et al. Clinical outcomes of calcium-channel blocker vs beta-blocker: From the Korean Acute Myocardial Infarction Registry. JACC Asia 3(3), 446–454. https://doi.org/10.1016/j.jacasi.2023.02.006 (2023).
Ibanez, B. et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 39(2), 119–177. https://doi.org/10.1093/eurheartj/ehx393 (2018).
O’gara, P. T. et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 61(4), e78–e140. https://doi.org/10.1016/j.jacc.2012.11.019 (2013).
Cutlip, D. E. et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 115(17), 2344–2351. https://doi.org/10.1161/CIRCULATIONAHA.106.685313 (2007).
Hong, S. J. et al. Effect of intravascular ultrasound–guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA 314(20), 2155–2163. https://doi.org/10.1001/jama.2015.15454 (2015).
Zhang, J. et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: The ULTIMATE trial. J. Am. Coll. Cardiol. 72(24), 3126–3137. https://doi.org/10.1016/j.jacc.2018.09.013 (2018).
Thiele, H. et al. Management of cardiogenic shock complicating myocardial infarction: An update 2019. Eur. Heart J. 40(32), 2671–2683. https://doi.org/10.1093/eurheartj/ehz363 (2019).
Neumann, F.-J. et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 40(2), 87–165. https://doi.org/10.1093/eurheartj/ehy394 (2019).
Hong, S. J. et al. Effect of intravascular ultrasound–guided drug-eluting stent implantation: 5-year follow-up of the IVUS-XPL randomized trial. JACC Cardiovasc. Interv. 13(1), 62–71. https://doi.org/10.1016/j.jcin.2019.09.033 (2020).
Iqbal, J. Incidence and predictors of stent thrombosis: A single-centre study of 5833 consecutive patients undergoing coronary artery stenting. EuroIntervention 9(1), 62–69. https://doi.org/10.4244/EIJV9I1A10 (2013).
Acknowledgements
The authors would like to thank the clinical investigators of the Korea Acute Myocardial Infarction Registry. The authors wish to thank Medical Illustration and Design, a part of the Medical Research Support Services of Yonsei University College of Medicine, for all artistic support related to this work.
Funding
This research was supported by a fund (2016-ER6304-02) conferred by Research of Korea Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Consortia
Contributions
O-HL and YK: study concept and design and drafting for the manuscript. D-KC, J-SK, B-KK, DC, M-KH, YJ and MHJ: acquired the data. YK and MHJ: supervised the progress of the study. O-HL, S-JH and YK: acquisition, analysis, and interpretation of data. O-HL, S-JH, YK, and MHJ : critical revision of the manuscript for important intellectual content. All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, OH., Heo, SJ., Johnson, T.W. et al. Intravascular ultrasound-guided versus angiography-guided percutaneous coronary intervention for acute myocardial infarction with cardiogenic shock. Sci Rep 14, 10028 (2024). https://doi.org/10.1038/s41598-024-59723-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59723-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.