Abstract
Pulmonary tuberculosis (TB) can result in irreversible damage and lead to tuberculous destructive lung (TDL), a severe chronic lung disease that is associated with a high mortality rate. Additionally, pulmonary hypertension (PH) is a hemodynamic disorder that can be caused by lung diseases. The objective of this study is to investigate the risk factors associated with PH in active TB patients diagnosed with TDL. We conducted a retrospective review of the medical records of 237 patients who were diagnosed with TDL, active pulmonary tuberculosis, and underwent echocardiography at the Third People’ Hospital of Shenzhen from January 1, 2016, to June 30, 2023. Univariate and multivariate logistic regression analyses were performed to identify factors that correlated with the development of pulmonary hypertension. Univariate and multivariate logistic regression analyses revealed that several factors were associated with an increased risk of pulmonary hypertension (PH) in individuals with tuberculosis destroyed lung (TDL). These factors included age (OR = 1.055), dyspnea (OR = 10.728), D-dimer (OR = 1.27), PaCO2 (OR = 1.040), number of destroyed lung lobes (OR = 5.584), bronchiectasis (OR = 3.205), and chronic pleuritis (OR = 2.841). When age, D-dimer, PaCO2, and number of destroyed lung lobes were combined, the predictive value for PH in patients with TDL was found to be 80.6% (95% CI 0.739–0.873),with a sensitivity of 76.6% and specificity of 73.2%. Advanced age, elevated D-dimer levels, hypercapnia, and severe lung damage were strongly correlated with the onset of PH in individuals with active pulmonary tuberculosis (PTB) and TDL. Furthermore, a model incorporating age, D-dimer, PaCO2, and the number of destroyed lung lobes might be valuable in predicting the occurrence of PH in patients with active PTB and TDL.
Similar content being viewed by others
Introduction
Tuberculosis (TB) remains a significant global public health threat, with 10.6 million new cases and 1.6 million deaths reported in 20211. Among the different types of TB, pulmonary TB is the most commonly observed, and it can cause irreversible damage to the lung parenchyma, bronchi, and lymph nodes, leading to a condition known as tuberculous destructive lung (TDL)2. TDL is characterized by a decrease in lung and airway volume, progressive airflow limitation, and recurrent exacerbations. It is a severe complication of pulmonary TB and is associated with high mortality3. Pulmonary hypertension (PH) is a hemodynamic disorder defined by a mean pulmonary arterial pressure of 25 mm Hg (1 mmHg = 0.133 kPa) or higher at rest during the Right-sided Heart Catheterization (RHC). Non-invasive transthoracic echocardiography is commonly used clinically to estimate the probability of PH4. PH due to chronic lung diseases is classified as Group 3 according to clinical practice guidelines5. Although TB is not commonly recognized as a cause of PH, previous studies have demonstrated the onset of PH in TB survivors6,7. As one of the complications of TDL, PH frequently complicates the clinical course of lung disease, reduces functional ability, impairs quality of life, causes right ventricular dysfunction and heart failure, thereby worsening the prognosis of patients with TDL8,9,10. However, the prevalence and clinical implications of PH in active pulmonary TB patients with TDL have not been well understood, and the risk factors for the development of PH have not been clearly identified11. Therefore, in this study, we aim to analyze clinical data, imaging characteristics, and echocardiography findings to explore the risk factors for PH in active TB patients with TDL.
Methods
Methods and materials
Study design and participants
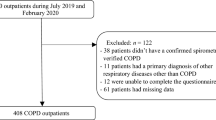
We conducted a retrospective study to investigate the relationship between tuberculous destructive lung (TDL) and pulmonary hypertension (PH). We reviewed the medical records of 662 patients who were diagnosed with active pulmonary TB and TDL at the Third People’s Hospital of Shenzhen from January 1, 2016, to June 30, 2023. The inclusion and exclusion criteria were as follows: (1) Inclusion criteria: active tuberculosis and TDL patients who underwent echocardiography. (2) Exclusion criteria: non-active pulmonary TB; non-tuberculous mycobacterial lung diseases; PH associated with left heart diseases, chronic obstructive lung diseases or emphysema, restrictive lung disease, connective tissue disease, chronic pulmonary embolism, pulmonary artery obstructions and idiopathic PH. Among them, we excluded 191 cases of non-active pulmonary tuberculosis, 20 cases of old pulmonary tuberculosis complicated with aspergillosis, and 45 cases of non-tuberculous mycobacterial lung disease. We included 406 cases of active pulmonary tuberculosis complicated with TDL. Furthermore, we excluded 144 cases with no echocardiography and 25 cases with PH caused by left-sided heart diseases and chronic thromboembolic PH. Ultimately, we included 237 cases in the analysis (Fig. 1). This study was approved by the Ethical Committee of the Third People’ Hospital of Shenzhen (IRB number: 2021-014-02). Written informed consent of patients was waived by the ethics committee (Ethical Committee of the Third People’ Hospital of Shenzhen) as all clinical data were extracted from the medical system and personal information of any patient was masked. The hospital ensured that no personal information of any patients was involved in using these data, and they adhered to the Declaration of Helsinki regarding confidentiality and ethical standards.
Definitions
Active pulmonary tuberculosis is defined according to the diagnostic criteria issued by the World Health Organization12. The detailed diagnosis criteria of active tuberculosis were as below: ① tuberculosis pathogenicity testing (positive fast-acid bacilli smear or culture results or molecular test) ② a comprehensive assessment based on the patient's clinical manifestations, laboratory testing, and radiological findings.
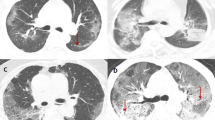
Tuberculosis destroyed lung (TDL) refers to extensive structural damage of the lung caused by Mycobacterium tuberculosis infection. This damage is manifested by widespread bronchial distortion, bronchiectasis, pulmonary fibrosis, cavitation, caseous necrosis, lymph node necrosis, and lymphatic obstruction, resulting in the loss of normal lung function. The assessment of TDL was conducted by one radiologist and one pulmonary tuberculosis specialist. In case of disagreement, another senior radiologist was consulted. Doppler echocardiography was used in our study to estimate the pulmonary artery systolic pressure (PASP) and assess the presence of pulmonary hypertension (PH) in the patients. A PASP measurement above 35 mmHg indicated PH in our study4. Right atrium (RA) pressure was also used in the determination of PASP. Estimation of RA pressure is based on inferior vena cava (IVC) size and collapse. IVC diameter > 2.1 cm that collapses < 50% with a sniff suggests high RA pressure of 15 mm Hg, which indicates the onset of PH13,14.
Data collection
For all eligible patients, the recorded information included demographics, medical history, underlying comorbidities, laboratory findings, Chest CT images, and cardiac ultrasound reports were obtained. Laboratory findings included white blood cell (WBC) count, neutrophilic granulocyte (GRA), lymphocyte (LYN), hemoglobin (HGB), monocyte (MONO), C-reactive protein (CRP), procalcitonin (PCT), D-Dimer, liver, and kidney function. All these clinical data were within 1 week of admission. A trained team of physicians and imaging specialists at The Third People's Hospital of Shenzhen reviewed the Chest CT images and cardiac ultrasound reports. The occurrence of destructive lung, pleural effusion, bronchiectasis, and PH were documented.
Statistical analyses
All statistical analyses were conducted using SPSS 26.0 (IBM, USA). Normal distribution data were expressed as mean ± standard deviation (SD), while skewed distribution data were presented as median and quantile. The significance of continuous data was determined using either a student's t-test or a Mann Whitney U test. Comparisons between two groups were performed using either a One-way Anova or a K-W test. Categorical features were presented as frequency (%) and compared using the chi-squared test. Differences in non-normally distributed data between two groups were assessed using the Mann–Whitney U test. Univariate and multivariate linear regression analyses were performed to identify factors correlated with PH. The association of variables with pulmonary arterial hypertension was evaluated using the receiver operating characteristic curve (ROC) and the area under the curve (AUC). Statistical significance was defined as a p-value < 0.05, and all reported p-values were two-sided.
Results
Clinical characteristics between TDL patients with and without PH
According to the measurement of pulmonary artery systolic pressure (PASP) through Doppler echocardiography, a total of 237 patients with tuberculous destroyed lung (TDL) were divided into two groups: TDL with PH group (47 cases) and TDL without PH group (190 cases). The mean age of the enrolled patients was 50.5 ± 17.1 years. Within the TDL with PH group, the mean age was 58.5 ± 15.8 years, while within the TDL without PH group, the mean age was 48.5 ± 16.9 years. The difference in age between the two groups was statistically significant (P < 0.001). Among the patients, 59 females (24.9%) were identified, with 19 in the TDL with PH group and 46 in the TDL without PH group. There was no statistically significant difference in gender composition between the two groups. Moreover, no statistically significant differences were observed between the two groups of patients in terms of body mass index (BMI), duration of symptoms, smoking history, diabetes, malnutrition, treatment history, and drug resistance. However, the incidence of hypertension was higher in the TDL with PH group (14.9%) compared to the TDL without PH group (5.3%), and this difference was statistically significant (P = 0.022). Regarding clinical symptoms, patients in the TDL with PH group had a higher incidence of dyspnea and bilateral lower extremity edema compared to the TDL without PH group (93.6% vs. 66.8%, P < 0.001; 19.1% vs. 8.4%, P = 0.032, respectively). However, there were no significant differences between the two groups in terms of cough, sputum, and hemoptysis (P > 0.05). Furthermore, the partial pressure of carbon dioxide (PaCO2) in the TDL with PH group was higher than that in the TDL group (P = 0.001), while the arterial/alveolar oxygen ratio was lower in the TDL with PH group compared to the TDL without PH group (P = 0.005). Both differences showed statistical significance (Table 1).
Imaging characteristics between TDL patients with and without PH
There was also no significant difference in cardiac ejection fraction between the two groups (P = 0.171). The median number of destroyed lung lobes on CT images in the TDL with PH group was 2, which was significantly different those in the TDL without PH group (P < 0.001). The incidence of bronchiectasis, pleural effusion, and atelectasis in the TDL with PH group were 53.2% vs. 31.1% (P = 0.004), 70.2% vs. 43.7% (P = 0.001), and 10.5% vs. 3.2% (P = 0.029), respectively, all with significant statistical differences.
Univariate and logistic regression analysis of factors correlated with PH
Using pulmonary hypertension (0 = no, 1 = yes) as the dependent variable, binary logistic regression analysis was conducted with the indicators (age, dyspnea, d-dimer, Number of destroyed lung lobe, bronchiectasis, chronic pleuritis) that showed statistical significance in the univariate analysis serving as the independent variables. The results indicated that the above indicators had beta values greater than 0, which were independent risk factors of pulmonary hypertension in individuals with tuberculosis-related lung damage. What’s more, the higher the OR, the higher the hazard correlation coefficient. The study proved that risk factors included age (OR = 1.055), dyspnoea (OR = 10.728), D-dimer (OR = 1.27), PaCO2 (OR = 1.040), number of destroyed lobes (OR = 5.584), bronchiectasis (OR = 3.205) and chronic pleurisy (OR = 2.841). All of the above variables were statistically significant (Table 2).
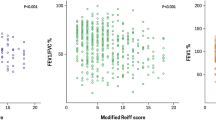
Diagnostic efficacy of a prediction model for PH in patients with active PTB with TDL
The diagnostic efficacy of age, D-dimer, PaCO2,the number of destroyed lung lobes, and a combined model based on these four variables were evaluated for the diagnosis of pulmonary hypertension (PH) in patients with TDL.The diagnostic efficacy of the combined model based on these four variables for the diagnosis of pulmonary hypertension (PH) in patients with TDL was assessed using the cut-off value, sensitivity, specificity, Youden's index, and AUC, which was 0.806 (95% CI 0.805–0.871), with a sensitivity of 76.6% and a specificity of 73.2% (Table 3). The optimal cutoff point was 0.2, resulting in a Youden index of 0.498 (Fig. 2).
Discussion
In our study, we demonstrated that active PTB patients with both TDL and PH were older and exhibited more severe clinical symptoms and extensive lung damage compared to those with TDL alone. Additionally, our study revealed that elevated levels of D-Dimer and hypercapnia were commonly observed in patients with both TDL and PH.
TDL mainly affected elderly patients, the mean age in this study was about 50 years old. TDL patients with PH were about ten years older than those without PH. This aligned with previous research indicating that older COPD patients are more likely to develop PH, implying that the prevalence of PH may increase with age in individuals with lung structural damage15,16. Furthermore, our study found that a higher proportion of patients with PH reported experiencing dyspnea compared to those without PH. While dyspnea is not a typical symptom of patients with PH, it can be indicative of impaired gas exchange. This highlights the importance of conducting cardiac ultrasounds and screening for the possible onset of PH in patients with TDL who present with dyspnea. Early diagnosis and management of PH may have the potential to enhance the quality of life and slow disease progression for these individuals.
In our study, we found out that patients with PH exhibited variable lung damage, including increased numbers of destroyed lung lobes, bronchiectasis, and chronic pleuritis. A retrospective study conducted in South Korea also revealed that patients with PH associated with tuberculous destroyed lung (TDL) experienced more severe lung damage17. TDL may lead to airflow limitation and the loss of the capillary network, thus contributing to the development of PH18. It has been observed in a study conducted by Li et al. that patients with active TB and elevated PASP frequently presented with lung cavities and extensive lung destruction. PaO2 levels were inversely correlated with PASP values in these patients19. But in our study, we didn’t found correlation between PaO2 level and PH. We contributed the possible reasons to different study population in two study. In our study, the enrolled patients were those with active PTB and TDL, while in Li’s study, the participants were all active PTB patients. Our study focused more on patients with severely damaged lung structures, who may basically have lower PaO2 level. However, the underlying pathophysiological mechanisms behind the development of PH in PTB patients remain unclear. Hypoxemia caused by chronic lung disease might be a contributor to PH, as it induces pulmonary vasoconstriction and increases PASP20. But recent studies have revealed that chronic hypercapnia, resulting from the direct effect of carbon dioxide on muscular pulmonary arteries, may also contribute to PH by causing recurring contraction and remodeling of pulmonary vessels. Hypercapnia is an important pathogenic factor in the development of PH21. In our study, we observed a correlation between severe lung destruction, elevated PaCO2 levels, and the development of PH in patients with TDL. We propose that the elevated PaCO2 levels are a result of impaired gas exchange due to lung destruction. Furthermore, the elevated PaCO2 levels contribute to increased vascular resistance, ultimately leading to PH.
Moreover, we observed that patients with TDL and PH had a higher level of D-dimer compared to patients with TDL alone. Univariate and logistic regression analyses revealed that elevated D-dimer was a risk factor for TDL with PH. This suggests that hypercoagulability may play a role in the development of PH22. Elevated levels of D-dimer, a byproduct of fibrin degradation, indicate a state of hypercoagulation in the body. Various inflammatory mediators, triggered by factors such as hypoxia, hypercapnia, infection, and others, can increase the production of fibrinogen and D-dimer. This creates a hypercoagulable state that can increase pulmonary artery pressure23. Previous studies have also reported higher levels of D-dimer in patients with pulmonary tuberculosis (PTB) and elevated PASP19. Additionally, recent research has demonstrated the benefits of oral anticoagulant therapy for patients with chronic obstructive pulmonary disease and PH24. Further investigations are required to provide more reliable evidence regarding the onset of a hypercoagulable state in patients with PH and TDL, as well as the potential benefits and safety of anticoagulants in this population.
For predicting PH in patients with TDL, we developed a model based on four variables: age, D-dimer levels, PaCO2 levels, and number of destroyed lung lobes. This model resulted in a sensitivity of 76.6% and specificity of 73.2%, the area under the curve (AUC) reached 80.6%. The combination of these four variables has a significant predictive value for PH in active PTB patients with TDL. Both tuberculosis (TB) and PH predominantly affect individuals in low-income and middle-income countries, millions of tuberculosis patients at risk of developing PH are unlikely to be identified and receive appropriate treatment due to the lack of skilled medical professionals and inadequate equipment25. Utilizing a simple yet effective predictive model for screening PH in active PTB patients with TDL might serve as an easily accessible assessment tool for early diagnosis. Further validation of our predictive model in an independent cohort study is needed.
There are several limitations in our study. Firstly, as a retrospective study, pulmonary function testing was not routinely performed in our study. We only used TDL on CT images to assess the damage of lung structures, which was insufficient for a comprehensive assessment of impaired lung function. Moreover, echocardiography was not a routine examination in all patients with TDL. The decision for echocardiography was up to the physician according to their personal experiences. This might introduce a selection bias and lead to missed diagnosis of PH. Secondly, we relied on Doppler echocardiography as the standard for assessing PH in our study. However, it is important to note that Doppler echocardiography is not considered the gold standard for diagnosing PH. Although previous studies have shown a strong correlation between echocardiography and right heart catheterization26, it is worth mentioning that echocardiography might underestimate the presence of PH27. Thirdly, it is worth mentioning that dyspnea, a symptom reported by the patients, was used as a diagnostic criterion in our study. It is important to recognize that subjective symptoms reported by patients may vary and have individual differences, thereby introducing potential selection bias.
In conclusion, our study has successfully demonstrated that several risk factors are correlated with the development of PH in active TB patients with TDL. These risk factors include old age, elevated levels of D-dimer, hypercapnia, and severe lung damage. By combining these four variables into a predictive model, we might be able to screen PH in active TB patients with severe lung damage. A well-designed prospective study is required to further investigate the exact contribution of PH and validate our predictive model in patients with severe tuberculous lung destruction.
Data availability
The datasets analyzed in the current study available from the corresponding author on reasonable request.
References
World Health Organization. Global Tuberculosis Report 2022 (World Health Organization, 2022).
Kim, H. Y. et al. Thoracic sequelae and complications of tuberculosis. Radiographics 21(4), 839–858. https://doi.org/10.1148/radiographics.21.4.g01jl06839 (2001) (Epub 2001/07/14).
Ryu, Y. J., Lee, J. H., Chun, E. M., Chang, J. H. & Shim, S. S. Clinical outcomes and prognostic factors in patients with tuberculous destroyed lung. Int. J. Tuberc. Lung Dis. 15(2), 246–250 (2011) (Epub 2011/01/12).
Mandras, S. A., Mehta, H. S. & Vaidya, A. Pulmonary hypertension: A brief guide for clinicians. Mayo Clin Proc. 95(9), 1978–1988. https://doi.org/10.1016/j.mayocp.2020.04.039 (2020) (Epub 2020/08/31).
Galiè, N. et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Respir. J. 46(4), 903–975. https://doi.org/10.1183/13993003.01032-2015 (2015) (Epub 2015/09/01).
Louw, E. et al. The prevalence of pulmonary hypertension after successful tuberculosis treatment in a community sample of adult patients. Pulm Circ. 13(1), 2184. https://doi.org/10.1002/pul2.12184 (2023) (Epub 2023/01/27).
Ahmed, A. E., Ibrahim, A. S. & Elshafie, S. M. Pulmonary hypertension in patients with treated pulmonary tuberculosis: Analysis of 14 consecutive cases. Clin. Med. Insights Circ. Respir. Pulm. Med. 5, 1–5. https://doi.org/10.4137/ccrpm.S6437 (2011) (Epub 2011/02/23).
Seeger, W. et al. Pulmonary hypertension in chronic lung diseases. J. Am. Coll. Cardiol. 62(25 Suppl), D109–D116. https://doi.org/10.1016/j.jacc.2013.10.036 (2013) (Epub 2013/12/21).
Nathan, S. D. et al. Pulmonary hypertension in chronic lung disease and hypoxia. Eur. Respir. J. 53(1), 1. https://doi.org/10.1183/13993003.01914-2018 (2019) (Epub 2018/12/14).
Maguire, G. P. et al. Pulmonary tuberculosis, impaired lung function, disability and quality of life in a high-burden setting. Int. J. Tuberc. Lung Dis. 13(12), 1500–1506 (2009) (Epub 2009/11/19).
Walsh, K. F. & Lui, J. K. Post-tuberculosis pulmonary hypertension: a case of global disparity in health care. Lancet Glob Health. 10(4), e476. https://doi.org/10.1016/S2214-109X(22)00042-0 (2022) (Epub 2022/03/19).
World Health Organization, Systematic screening for active tuberculosis: an operational guide (2015).
Augustine, D. X. et al. Echocardiographic assessment of pulmonary hypertension: A guideline protocol from the British Society of Echocardiography. Echo Res. Pract. 5(3), G11–G24. https://doi.org/10.1530/ERP-17-0071 (2018).
Rudski, L. G. et al. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 23(7), 685–788. https://doi.org/10.1016/j.echo.2010.05.010 (2010).
Chaouat, A., Naeije, R. & Weitzenblum, E. Pulmonary hypertension in COPD. Eur. Respir. J. 32(5), 1371–1385. https://doi.org/10.1183/09031936.00015608 (2008) (Epub 2008/11/04).
Gredic, M. et al. Pulmonary hypertension in chronic obstructive pulmonary disease. Br. J. Pharmacol. 178(1), 132–151. https://doi.org/10.1111/bph.14979 (2021) (Epub 2020/01/25).
Jo, Y. S. et al. Risk factors for pulmonary arterial hypertension in patients with tuberculosis-destroyed lungs and their clinical characteristics compared with patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon Dis. 12, 2433–2443. https://doi.org/10.2147/COPD.S136304 (2017) (Epub 2017/09/02).
Kim, S. J. et al. Effect of airflow limitation on acute exacerbations in patients with destroyed lungs by tuberculosis. J. Korean Med. Sci. 30(6), 737–742. https://doi.org/10.3346/jkms.2015.30.6.737 (2015) (Epub 2015/06/02).
Wen-Ting, L., Chang-Wei, W., De-Jian, B. & Wei, S. Arterial partial pressure of oxygen and procalcitonin levels correlate with pulmonary artery systolic pressure in patients with active pulmonary tuberculosis. Int. J. Infect. Dis. 117, 87–92. https://doi.org/10.1016/j.ijid.2022.01.060 (2022) (Epub 2022/02/06).
Huang, J. et al. Hypoxia-induced pulmonary hypertension and chronic lung disease: Caveolin-1 dysfunction an important underlying feature. Pulm Circ. 9(1), 876. https://doi.org/10.1177/2045894019837876 (2019) (Epub 2019/02/27).
Zuoyou, L. et al. Borderline pulmonary hypertension associated with chronic hypercapnia in chronic pulmonary disease. Respir. Physiol. Neurobiol. 262, 20–25. https://doi.org/10.1016/j.resp.2019.01.003 (2019) (Epub 2019/01/21).
Smits, A. J. et al. A systematic review with meta-analysis of biomarkers for detection of pulmonary arterial hypertension. ERJ Open Res. 8(2), 1. https://doi.org/10.1183/23120541.00009-2022 (2022) (Epub 2022/06/03).
Bazan, I. S. & Fares, W. H. Hypercoagulability in pulmonary hypertension. Clin. Chest Med. 39(3), 595–603. https://doi.org/10.1016/j.ccm.2018.04.005 (2018) (Epub 2018/08/21).
Lai, J., Feng, S., Xu, S. & Liu, X. Effects of oral anticoagulant therapy in patients with pulmonary diseases. Front. Cardiovasc. Med. 9, 987652. https://doi.org/10.3389/fcvm.2022.987652 (2022) (Epub 2022/08/30).
Hoeper, M. M. et al. A global view of pulmonary hypertension. Lancet Respir. Med. 4(4), 306–322. https://doi.org/10.1016/s2213-2600(15)00543-3 (2016) (Epub 2016/03/16).
Kovacs, G. et al. Assessment of pulmonary arterial pressure during exercise in collagen vascular disease: Echocardiography vs right-sided heart catheterization. Chest. 138(2), 270–278. https://doi.org/10.1378/chest.09-2099 (2010) (Epub 2010/04/27).
Fisher, M. R. et al. Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur. Respir. J. 30(5), 914–921. https://doi.org/10.1183/09031936.00033007 (2007) (Epub 2007/07/27).
Funding
This work was supported by Shenzhen Science and Technology Plan Project (No. JCYJ20210324132012035), Technology Project of Guangdong Province (No. 2020B1111170014) which are government fund for tuberculosis treatment and control.
Author information
Authors and Affiliations
Contributions
WL: data curation, formal analysis, writing original draft preparation. YX: helped with data analysis and edited the manuscript. LY: data curation, writing reviewing and editing. SZ: writing reviewing and made conceptual contributions to the manuscript. KP: helped with data analysis and interpretation. HL: helped to ensure methodological rigor. HQ: provided oversight and supervision based on her knowledge of qualitative methodology and the context. PZ: conceptualization, methodology, writing-original draft preparation. All authors contributed to the completion of this manuscript and have read and approved it.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, W., Xu, Y., Yang, L. et al. Risk factors associated with pulmonary hypertension in patients with active tuberculosis and tuberculous destroyed lung: a retrospective study. Sci Rep 14, 10108 (2024). https://doi.org/10.1038/s41598-024-59679-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59679-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.