Abstract
Phage-antibiotic combinations to treat bacterial infections are gaining increased attention due to the synergistic effects often observed when applying both components together. Most studies however focus on a single pathogen, although in many clinical cases multiple species are present at the site of infection. The aim of this study was to investigate the anti-biofilm activity of phage-antibiotic/antifungal combinations on single- and dual-species biofilms formed by P. aeruginosa and the fungal pathogen Candida albicans. The Pseudomonas phage Motto in combination with ciprofloxacin had significant anti-biofilm activity. We then compared biofilms formed by P. aeruginosa alone with the dual-species biofilms formed by bacteria and C. albicans. Here, we found that the phage together with the antifungal fluconazole was active against 6-h-old dual-species biofilms but showed only negligible activity against 24-h-old biofilms. This study lays the first foundation for potential therapeutic approaches to treat co-infections caused by bacteria and fungi using phage-antibiotic combinations.
Similar content being viewed by others
Introduction
Phage therapy makes use of bacteriophages to treat bacterial infections, in particular infectious ones that cannot be treated with conventional antibiotics due to multi-drug resistance1,2. Although most of the therapeutic applications of phages are in monotherapy or as phage cocktails, recently the combination of phages and antibiotics is getting attention through successful in vitro studies3,4. In most cases, phages and antibiotics were proven to act in synergy against bacteria5,6,7. Recent investigations showed that antibiotic resensitization can occur during phage exposure in antibiotic-resistant bacterial cells8,9.
Pseudomonas aeruginosa is a Gram-negative pathogen known to cause mild, but also life-threatening infections of the blood, the lungs and other parts of the body; here in particular after surgery. While many infections are treatable, an increasing number of antibiotic-resistant P. aeruginosa strains are being observed. This, together with the pathogen’s ability to form biofilms, can make the clinical control of infections challenging10. Recent studies showed the efficacy of Pseudomonas phages as anti-biofilm agents, while the use of phage-antibiotic combinations is gaining attention due to the noted synergistic effects11,12,13,14. Another major challenge with P. aeruginosa biofilms is that they often form as dual-species or multi-species biofilms13,15.
Microbe-microbe interactions can influence various infection parameters including virulence and biofilm formation. Dual-species biofilms formed by P. aeruginosa and Candida albicans are frequently found in cystic fibrosis patients but also in patients in association with catheters15,16. Candida albicans alone can cause opportunistic infections and is mostly found in the gastrointestinal tract, mouth and vagina17. Most bacterial-fungal dual-species biofilm infections are caused by the coexistence of Pseudomonas-Candida or Staphylococcus-Candida15,17. It is also known that the presence of P. aeruginosa can influence the C. albicans biofilms18 and longer exposure can inhibit the dual-species biofilm growth under in vitro conditions19,20. To date, antibiotics are the physicians’ choice for the treatment against dual-species biofilm infections but the recently increasing rates of antibiotic resistance can make the therapeutic approach unsuccessful and lead to life-threatening complications.
To understand the potential of using phage-antibiotic combinations on Pseudomonas-Candida embedded in biofilms, we tested various antibiotics and fungicides on single and dual-species biofilms. First, we systematically tested the effects of phages together with antibiotics on planktonic and then on biofilm-embedded bacteria before we studied the impact of antimicrobials in conjunction with phages on Pseudomonas-Candida biofilms. The hypothesis is that the biofilms formed by the Pseudomonas-Candida have exopolysaccharides which can be degraded by phage depolymerases so that the disturbed biofilm cells can be eliminated by phage Motto (as an anti-bacterial) and fluconazole (as an anti-fungal). The phage Motto used in this study was previously characterized to have anti-biofilm activity and found to have broad host range infectivity21,22. The anti-fungal fluconazole inhibits the fungal cell membrane synthesis and is mainly used to treat candidiasis and it has weak anti-biofilm activity.
Results
Antibiotics act synergistically with phage on planktonic cells
Phage-antibiotic combinations have attracted attention in the treatment of multidrug-resistant bacterial infections due to often observed synergistic effects in vitro and in vivo. We thus aimed to test the effect of phage Motto on its host in the presence of antibiotics. First, we determined the MIC of P. aeruginosa PA01 against different antibiotics. Five antibiotics, cefotaxime, ciprofloxacin, gentamicin, meropenem and tetracycline, were used in this study, which are either front-line or broad-spectrum antibiotics against P. aeruginosa infections. The isolate was found to be resistant to cefotaxime, gentamicin, meropenem and tetracycline but susceptible to ciprofloxacin according to the CLSI guidelines (Table 1).
For the following experiments, sublethal concentrations of antibiotics were chosen and accordingly, 1/4th of the MIC was selected. Next, all the antibiotics were tested for their phage-inhibitory effects to ensure that the phage activity was not affected by the compounds (see Figure S1). The effect of Pseudomonas phage Motto and sublethal concentrations of the antibiotics on P. aeruginosa PA01 was then investigated by determining the viable cell concentration (CFU/mL) after 18 h of exposure. In the control group (without phage and antibiotic), the bacterial count was 3.4 × 109 CFU/mL, whereas the phages with a final titer of 103 and 106 PFU/mL reduced the bacterial count to 2.1 × 106 CFU/mL and 1.2 × 103 CFU/mL, respectively (Fig. 1). No bacteria were found when the pathogen was exposed to phages at a titre of 1012 PFU/mL (Table 2).
Synergistic effect of Pseudomonas phage Motto with antibiotics as determined by statistical analysis. The combination provides a significant reduction in bacterial growth as observed by CFU/mL. In case no bars are visible, the bacterial count was zero. All the error bars indicated are standard errors and the ***p < 0.001, **p > 0.05 were determined by two-way ANOVA (between antibiotic only and phage-antibiotic combination) with Bonferroni correction.
In the absence of phages, antibiotics at sublethal concentrations (1/4th of the MIC) had minor or even no inhibitory effects. Accordingly, bacterial reductions were observed in the case of tetracycline (4.1 × 107 CFU/mL), cefotaxime (3.7 × 108 CFU/mL) and gentamicin (2.1 × 108 CFU/mL) but no effect was found when ciprofloxacin was used (1.1 × 109 CFU/mL). Likewise, meropenem had no significant effect (2.9 × 109 CFU/mL). While we observed synergistic effects of phages with three antibiotics, ciprofloxacin, cefotaxime and meropenem. The combination of ciprofloxacin (0.5 µg/mL) together with phages at 103 PFU/mL resulted in a seven-log reduction (Table 2). Similarly, meropenem (8 µg/mL) together with phages at 103 PFU/mL resulted in a six-log reduction. Phages at a higher titre of 106 PFU/mL (plus ciprofloxacin or meropenem) resulted in the complete elimination of bacterial cells. Cefotaxime-phage had synergistic activity resulting in a five-log (103 PFU/mL) and six-log (106 PFU/mL) reduction. The combination of 103 PFU/mL phages together with gentamicin (4 µg/mL) resulted in a four-log reduction, and at 106 PFU/mL a six-log reduction was observed. Tetracycline-phage combinations substantially reduced the number of viable cells: At a phage number of 103 PFU/mL a four-log reduction was seen, while a higher titre of 106 PFU/mL resulted in a five-log reduction of bacterial cells (Table 2).
Phage-antibiotic combinations show synergy against biofilm-forming P. aeruginosa cells
Often phages and antibiotics have different effects on the same bacterial strain depending on whether they are embedded in a biofilm or planktonic23,24. Thus, we determined the possible effects of phage-antibiotic combinations on bacterial biofilm-embedded cells. After forming biofilm-embedded cells in microtiter plates for 24 h, we added different concentrations of antibiotics together with different amounts of phages. A synography model was previously designed by the TAILΦR lab in Texas, to study and visualise the effectiveness of phage-antibiotic combinations across many stoichiometries4.
The analysis of our data shows that for all phage-antibiotic combinations, at high titres and antibiotic concentrations, the biofilm was reduced to a varying extent and depending on the antibiotic. In the treatment of the pseudomonal biofilm with cefotaxime alone, even the highest antibiotic concentration of 32 µg/mL did not show any significant anti-biofilm effect. However, complete removal of the biofilm was observed at concentrations of cefotaxime between 32 and 16 µg/mL when phages were present at high titres (Fig. 2A). MIC results showed that P. aeruginosa PA01 was sensitive to ciprofloxacin. Correlating with this, we observed a complete biofilm eradication at the higher concentrations of ciprofloxacin (> = 16 µg/mL) which appears at first glance surprising (Fig. 2B). Possibly the bactericidal effects lead to a release of bacterial enzymes from the cells which then degrade the biofilm as a direct effect of the ciprofloxacin is less likely; this interpretation however, is speculation and requires further experimental validation. Nevertheless, synergistic effects were observed with increasing amounts of phages. Gentamicin alone exhibited minor anti-biofilm properties but combinatorial effects can be seen when phages are added at titres higher than 103 PFU/mL (Fig. 2C). Similarly, meropenem, which had no obvious effect on biofilms on its own, did only reduce the biofilm when phages were present. Clear synergy was observed at values higher than 4 µg/mL and titres higher than 107 PFU/mL (Fig. 2D). While tetracycline alone showed -to some extent- anti-biofilm properties in our assay, the combination of the antibiotic with the phage exhibited significant synergistic effects at concentrations higher than 4 µg/mL and phage numbers higher than 107 PFU/mL (Fig. 2E).
Anti-biofilm effect of Pseudomonas phage Motto and different antibiotics on P. aeruginosa biofilms. The effect of different antibiotics was studied: (A) Cefotaxime; (B) Ciprofloxacin; (C) Gentamicin; (D) Meropenem; (E) Tetracycline. The bacterial biofilms (24 h old) were treated with different combinations of phages and antibiotics. The synograms represent the OD595nm values read after 24 h of treatment and the mean reduction percentage of each treatment from three independent replicates.
Combinations of phage and the antifungal fluconazole have minor effects on dual-species biofilms
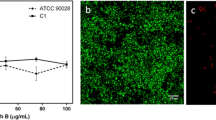
To investigate the formation of mono- and dual-species biofilms, we cultured cells of P. aeruginosa PA01 and C. albicans C11 either alone or together in microtiter plates. After 6 h, cultures of P. aeruginosa PA01 quantitatively formed less biofilm compared to C. albicans C11, according to the assay we employed. Both organisms together, however, formed even more biofilm than the individual ones combined (Fig. 3A). After 24 h, biofilms increased for both the bacterial and the fungal pathogen (mono), while the dual-species biofilm was less than the sum of the individual biofilms from P. aeruginosa PA01 and of C. albicans C11 (Fig. 3B).
Biofilm of C. albicans and P. aeruginosa clinical isolates in mono- and dual-species at 6 h (left) and 24 h (right). The results represent the biofilm formation after 6 and 24 h as the absorbance was read at OD595nm and the error bars represent the standard mean of the three independent experiments.
The eradication of dual-species biofilms is impossible in the presence of phage alone or antibiotics alone as the fungal pathogen can multiply and continue to produce biofilm. Therefore, we tested phage-antifungal combinations. A complete eradication was not observed, even at the highest phage and fluconazole concentrations (Fig. 4). No synergistic effect was observed when a phage-antifungal combination was used against C. albicans (mono) biofilms (see Figure S2). Nonetheless, a trend at high phage and antibiotic concentrations with a biofilm-adverse effect can be observed in both cases of up to 30%, with 6 and 24-h biofilm samples (Fig. 4). Though crystal violet assay cannot distinguish between the two species in a biofilm, it is worth noting that at higher phage concentrations (without fluconazole) Motto was penetrating the P. aeruginosa biofilms. It is clear that the phage has a positive impact on the removal of the dual-species biofilms in combination with exposure to fluconazole.
Phage-fluconazole synergism in the reduction of dual-species biofilms formed by Pseudomonas-Candida. Effect of Pseudomonas phage Motto (102 to 1012) and fluconazole (128 to 2 µg/mL) on dual-species biofilms. The dual-species biofilms [6 h old (top) and 24 h old (bottom)] were treated with different combinations of Pseudomonas phage and fluconazole. The synograms represent the OD595nm values as read after 24 h of treatment and the mean reduction percentage of treatment from three independent replicates.
Antifungals are required for dual-species biofilm removal, as phage-antibacterial combinations have no effect
We established that phage-antibiotic combinations are effective on biofilms formed by P. aeruginosa alone. We also demonstrated that phage-antifungal combinations resulted in the reduction of biofilms formed by the bacterial pathogen together with C. albicans, albeit to a minor extent. Thus, we next tested if the combination of phages together with antibiotics acting on P. aeruginosa leads to a reduction of dual-species biofilms. However, even at the highest concentration and highest phage titre tested, biofilms remained unaltered (see Figure S3). This is somewhat surprising, as one might suspect that the bacterial biofilm is reduced. However, the fungal pathogen possibly continues to thrive and thus produces more biofilm. Crystal violet assay cannot distinguish between the two species in a biofilm. It is possible that the phage-antibiotics are killing P. aeruginosa but not C. albicans, allowing C. albicans to grow. If P. aeruginosa is being killed, another explanation is the size difference between the two species, causing crystal violet to stain C. albicans primarily. Alternatively, it is possible that the presence of C. albicans and its extracellular matrix components protects P. aeruginosa from the phage-antibiotic treatment.
Antimicrobial combinations of the antifungal fluconazole together with antibacterials act synergistically at high concentrations
Although this study focused on the antibiofilm properties of a P. aeruginosa phage in combination with antimicrobial compounds, we also investigated how antibiotics alone act on dual-species biofilms. Interestingly, we observe antibiotic-specific synergy in some cases; clear effects can be seen in the case of cefotaxime and ciprofloxacin up to 60% reduction, while the reduction of biofilm using gentamicin together with fluconazole was less pronounced with a 50% reduction. Both meropenem and tetracycline in conjunction with the antifungal were unable to reduce the biofilm with the reduction of < 40% (Fig. 5).
Fluconazole-antibiotic synergism in the reduction of dual-species biofilms formed by Pseudomonas-Candida. Effect of fluconazole (0.5–64 µg/mL) and antibiotics (cefotaxime, ciprofloxacin, gentamicin, meropenem, tetracycline at 0.5–128 µg/mL) on dual-species biofilms. The dual-species biofilms (24 h old) were treated with different combinations of fluconazole and antibiotics. The synograms represent the OD595nm values as read after 24 h of treatment and the mean reduction percentage of treatment from three independent replicates.
Discussion
Pseudomonas aeruginosa is known to cause life-threatening infections in humans and is one of the common nosocomial pathogens to cause respiratory tract infections. To overcome the threat of antibiotic-resistant pseudomonal infections, non-antibiotic therapies and antibiotic combinatorial therapies are being investigated as valuable alternatives25. The use of phage-antibiotic combination therapies has been therapeutically successful, possibly due to the emergence of phage-resistant strains that show increased antibiotic susceptibility8,26,27. However, many infections are complicated by the formation of biofilms, which inhibit the diffusion of antibiotic compounds and form a kind of protective layer around the pathogens. Due to their unique properties, phages have been found to be effective in dissolving biofilms, both in vitro and in vivo28,29. This was also demonstrated in the case of P. aeruginosa infections30,31. Thus, phages can act synergistically as a biofilm-disrupting agent, allowing antibiotics to penetrate the target. Despite this, many infections are caused not by one species but by several, known as polymicrobial infections. Such “collaborative infections” are common for P. aeruginosa which is often found together with S. aureus32. Especially in the lungs of cystic fibrosis (CF) patients, P. aeruginosa is present with C. albicans33,34. Thus, there is growing interest in multispecies biofilms. This is particularly important for those that are formed by different domains of life. The treatment failures are mainly due to the impermeability of dual-species biofilms by chemotherapeutic drugs.
Our study aimed to investigate the potential of phage-antibiotic combinations in eradicating biofilms formed by P. aeruginosa and dual-species biofilms of P. aeruginosa-C. albicans. Initially, P. aeruginosa PA01 planktonic cells were treated with phage-antibiotic combinations in order to establish a baseline for potentially observed phage-antibiotic synergy. Here, we found that ciprofloxacin and meropenem had a more pronounced synergistic effect (Fig. 1). On the other end of the spectrum, cefotaxime, gentamicin, and tetracycline had the least degree of synergism. Despite the bacteria being susceptible to ciprofloxacin (MIC of 0.5 µg/mL), when combined with phages even at the sublethal concentrations (1/4th MIC), a lethal anti-pseudomonal effect was observed (Fig. 1). The three antibiotics (ciprofloxacin, cefotaxime and meropenem) had a synergistic effect with a minimum of four-log reductions when compared to antibiotics alone and at least two-log reductions when compared to phages alone. Notably, irrespective of the antibiotic class, the Pseudomonas phage Motto was found to work synergistically with all the tested antibiotics in this study (Fig. 1). Our data is similar to a recent study which showed the anti-pseudomonal effect of phage-antibiotic (sub-MIC) combinations on pathogenic P. aeruginosa strains27. As we were interested in the effects on biofilm, we tested the reduction of pseudomonal biofilms when exposed to phage-antibiotic combinations (Fig. 2). Here, we observed that phage-ciprofloxacin exhibited enhanced biofilm eradication compared to other antibiotics (cefotaxime, gentamicin, meropenem and tetracycline) (Fig. 2). Similar results were reported previously showing that the phage-ciprofloxacin combination has better biofilm eradication ability compared to the single-compound treatment14. In our study, the synogram showed that phage Motto was acting synergistically with all tested antibiotics and was effective at disrupting P. aeruginosa biofilms (Fig. 2).
As P. aeruginosa is often found together with C. albicans in biofilms, we focused on this important aspect next: The inhibition of P. aeruginosa-C. albicans dual-species biofilms when exposed to the combination of phage together with the fungicide fluconazole were tested. To this end, we investigated the formation of biofilm by the pathogens on their own or when grown together. Curiously, while P. aeruginosa PA01 and C. albicans C11 were forming moderate amounts of biofilm within 6 h, we observed that the production of biofilm was additive when both pathogens were present. More substantial biofilms were produced by the individual species after 24 h, while the dual-species biofilm reached even higher quantities in our assay, yet not the sum of the individual amounts of mono-species biofilms (Fig. 3).
After establishing the extent of the formation of biofilms at the two-time points, we next tested the combination of the phage Motto together with the antifungal compound fluconazole. While complete biofilm eradication was observed in the case of 6-h-old biofilms, the 24-h-old biofilms were only partially (50%) disintegrated after 16 h of phage-fluconazole exposure (Fig. 4). A possible explanation for this strong difference is the change in biofilm composition over time, which remains to be investigated. While many phages are known to degrade bacterial biofilms, whether the depolymerases produced by phages can degrade dual-species biofilms, especially the ones made by fungi, remains unknown.
We also tested the combination of antibacterial compounds together with the antifungal drug (Fig. 5). Here, we observed a clear synergy albeit at high concentrations of both compounds. To our surprise, no effects (overall biomass) were seen at all when phage-antibacterial combinations were used to treat the dual-species biofilm (see Figure S3). A previous study had also showed meropenem tolerance of P. aeruginosa in the presence of C. albicans in dual-species biofilms35. However, one other study conducted previously showed the effect of phage combinations and ciprofloxacin to limit S. aureus- C. albicans biofilms36. Our study aimed to shed light on the complexity of polymicrobial biofilms and the effects of phages on their structure. At this point, there is no concluding evidence to prove the eradication of polymicrobial infections caused by pathogenic bacteria and fungi using phage-antibiotic combinations. It becomes obvious that we need more studies to understand the effect of phages on such complex systems in order to develop treatment regimes for dual-species infections or biofilm removal before phages can be considered for therapeutic purposes.
Limitations of the study
Our study clearly illustrates the potential of using phages to disintegrate P. aeruginosa biofilms. Anti-biofilm properties are more pronounced when antibiotics are used together with the phage. The effect is not an additive one, as the compounds together exhibit synergy. However, underlying mechanisms for this synergy remain speculative as antibiotics on their own do not have anti-biofilm properties. Possibly, a re-sensitisation to antibiotics occurs in bacteria that acquire phage resistance, in turn leading to bacterial killing by the antibacterial compounds, as was previously observed7,8,37. When studying dual-species biofilms, the composition of the material is likely to be highly heterogeneous, as they are produced by both organisms. Such biofilms might possibly be even different from the combination of those formed by each individual species alone; there might be a yet unknown interplay, influencing the structure and composition of the matrix when both opportunistic pathogens are present. Using phages for the treatment of infections caused by two species might lead to C. albicans producing more biofilm and replacing the bacterial one. The fungal biofilm is unlikely to be efficiently degraded by the phage-derived enzymes that are known to often show specificity towards certain bacteria.
Materials and methods
Bacteria, Candida and bacteriophages
In this study, pathogenic mucoid P. aeruginosa PA01 and C. albicans C11 were used which were previously collected by the diagnostic centres in Chennai, Tamil Nadu, India. C. albicans C11 was isolated from the urine sample which is associated with virulence. Minimal inhibitory concentration (MIC) tests were performed following the micro-broth dilution method using cefotaxime, ciprofloxacin, gentamicin, meropenem and tetracycline (Merck KGaA, Darmstadt, Germany). The results were interpreted according to CLSI guidelines. Previously characterized lytic Pseudomonas phage Motto was used in this study21,22.
Phage-antibiotic combination against planktonic P. aeruginosa
To study synergistic effects, the antibiotics were added at the sub-inhibitory concentrations (1/4th MIC) and the phages were used at concentrations of 103, 106 and 1012 PFU/mL. Briefly, antibiotics were diluted to the sub-inhibitory concentrations (1/4th MIC) which were mixed with the 50 µL of phages at respective concentrations in the micro-titre plates. Then, 5 µL of P. aeruginosa at 5 × 105 CFU/mL was added. The plates were incubated at 37 °C for 18 h and 100 µL was removed, serially diluted (up to 10–6) and plated on LB agar plates. Colony-forming units (CFU/mL) were determined and compared to the control (phage and antibiotic alone). All the data are presented as mean ± standard deviation (SD) of at least three independent experiments.
Phage-antibiotic combination against biofilm-forming P. aeruginosa
For the anti-biofilm studies, cefotaxime, ciprofloxacin, gentamicin, meropenem and tetracycline were used. Briefly, biofilms were formed using the exponentially growing bacterial cells from the overnight culture. Overnight cultures were grown at 37 °C in LB broth and diluted in a microtiter plate and incubated at 37 °C for 24 h. The phage-antibiotic combinations were prepared following the checkerboard assay (antibiotics from 0.5 to 32 µg/mL were prepared in columns and the phage concentrations from 102 to 109 PFU/mL were prepared in rows; the study design is represented in Figure S4). Then, the plate was incubated at 37 °C for 24 h, washed twice to remove the planktonic cells then stained using crystal violet. The optical density (OD) was determined at 595 nm using a microtitre plate reader (BioTek, India).
Phage-antibiotic effects on dual-species biofilms
To study the inhibitory effect of Pseudomonas phage Motto and antimicrobial compounds including the fungicide fluconazole against P. aeruginosa-C. albicans mixed species biofilms, we allowed a dual-species biofilm to be formed: Briefly, overnight cultures of P. aeruginosa PA01 were grown at 37 °C in LB broth (tryptone, yeast extract and NaCl), and overnight cultures of C. albicans C11 were grown at 30 °C with shaking in YPD (Yeast extract, Peptone, and Dextrose) medium. For dual-species biofilms, equal volumes (equivalent to an OD600 value of 0.1) of P. aeruginosa and C. albicans (prepared in their respective medium) were mixed and incubated at 37 °C for 6 and 24 h. Plates were then washed twice to remove the planktonic cells. Again, checkerboard assays were performed as represented in Figure S1. Briefly, phages at 102 to 1012 PFU/mL and fluconazole from 2 to 128 µg/mL were added (fluconazole in columns and phages in rows) and transferred to dual-species biofilm plates either after 6 h or 24 h (96-well microtiter plates). After the addition of phage-fluconazole combinations, the plates were incubated for 16 h, washed, and stained using crystal violet and OD595nm was measured. The control groups include pseudomonal biofilm without challenge, C. albicans biofilm without challenge, and dual-species biofilm challenged with phage alone and fluconazole alone. All the data are presented as mean ± standard deviation (SD) of at least three independent experiments.
In the case of phage-antibacterial agents, the dual-species biofilms (24 h old) were treated with phages at 102 to 109 PFU/mL and antibacterials (cefotaxime, ciprofloxacin, gentamicin, meropenem and tetracycline) at 0.5–128 µg/mL. Accordingly, the dual-species biofilms (24 h old) were treated with fluconazole at 0.5 to 64 µg/mL and antibacterials (cefotaxime, ciprofloxacin, gentamicin, meropenem and tetracycline) at 0.5 to 128 µg/mL. After the addition of phage/fluconazole-antibacterial combinations, the plates were incubated for 16 h, washed then stained using crystal violet and OD595nm was measured. Statistical analysis was performed using GraphPad Prism software 7.0 (GraphPad Software, Inc., La Jolla, USA).
Data availability
Genome sequence data have been deposited at NCBI and are publicly available as of the date of publication. The accession number of the Pseudomonas phage Motto is ON843697. Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.
References
Kortright, K. E., Chan, B. K., Koff, J. L. & Turner, P. E. Phage therapy: A renewed approach to combat antibiotic-resistant bacteria. Cell Host Microbe. 25, 219–232 (2019).
Luong, T., Salabarria, A. C. & Roach, D. R. Phage therapy in the resistance era: Where do we stand and where are we going?. Clin. Ther. 42, 1659–1680 (2020).
Segall, A. M., Roach, D. R. & Strathdee, S. A. Stronger together? Perspectives on phage-antibiotic synergy in clinical applications of phage therapy. Curr. Opin. Microbiol. 51, 46–50 (2019).
Gu Liu, C. et al. Phage-antibiotic synergy is driven by a unique combination of antibacterial mechanism of action and stoichiometry. MBio 11, e01462-e1520 (2020).
Uchiyama, J. et al. Piperacillin and ceftazidime produce the strongest synergistic phage–antibiotic effect in Pseudomonas aeruginosa. Arch. Virol. 163, 1941–1948 (2018).
Manohar, P. et al. Synergistic effects of phage-antibiotic combinations against Citrobacter amalonaticus. ACS Infect. Dis. 8, 59–65 (2022).
Gordillo Altamirano, F. et al. Bacteriophage-resistant Acinetobacter baumannii are resensitized to antimicrobials. Nat. Microbiol. 6, 157–161 (2021).
Wang, X., Loh, B., Yu, Y., Hua, X. & Leptihn, S. Colistin-phage combinations decrease antibiotic resistance in Acinetobacter baumannii via changes in envelope architecture. Emerg. Microbes Infect. 10, 2205–2219 (2021).
Engeman, E. et al. Synergistic Killing and re-sensitization of Pseudomonas aeruginosa to antibiotics by phage-antibiotic combination treatment. Pharmaceuticals 14, 184 (2021).
Mah, T. F. et al. A genetic basis for Pseudomonas aeruginosa biofilm antibiotic resistance. Nature 426, 306–310 (2003).
Oliveira, V. C. et al. Identification and characterization of new bacteriophages to control multidrug-resistant Pseudomonas aeruginosa biofilm on endotracheal tubes. Front. Microbiol. 11, 580779 (2020).
Chegini, Z. et al. Bacteriophage therapy against Pseudomonas aeruginosa biofilms: A review. Ann. Clin. Microbiol. Antimicrob. 19, 1–7 (2020).
Akturk, E. et al. Synergistic action of phage and antibiotics: Parameters to enhance the killing efficacy against mono and dual-species biofilms. Antibiotics 8, 103 (2019).
Chang, R. Y. et al. Bacteriophage PEV20 and ciprofloxacin combination treatment enhances removal of Pseudomonas aeruginosa biofilm isolated from cystic fibrosis and wound patients. AAPS J. 21, 49 (2019).
Kasetty, S., Mould, D. L., Hogan, D. A. & Nadell, C. D. Both Pseudomonas aeruginosa and Candida albicans accumulate greater biomass in dual-species biofilms under flow. mSphere 6, e00416-e421 (2021).
Hogan, D. A. & Kolter, R. Pseudomonas-Candida interactions: An ecological role for virulence factors. Science 296, 2229–2232 (2002).
Carolus, H., Van Dyck, K. & Van Dijck, P. Candida albicans and Staphylococcus species: A threatening twosome. Front. Microbiol. 10, 2162 (2019).
Hogan, D. A., Vik, Å. & Kolter, R. A Pseudomonas aeruginosa quorum-sensing molecule influences Candida albicans morphology. Mol. Microbiol. 54, 1212–1223 (2004).
Bandara, H. M., Yau, J. Y., Watt, R. M., Jin, L. J. & Samaranayake, L. Pseudomonas aeruginosa inhibits in-vitro Candida biofilm development. BMC Microbiol. 10, 125 (2010).
Morales, D. K. et al. Control of Candida albicans metabolism and biofilm formation by Pseudomonas aeruginosa phenazines. MBio 4, e00526-e612 (2013).
Manohar, P. et al. Complete Genome Sequence of Pseudomonas Phage Motto. Microbiol. Resour. Announc. 11, e00740-e822 (2022).
Manohar, P., Loh, B., Turner, D., Tamizhselvi, R., Mathankumar, M., Elangovan, N., Nachimuthu, R. & Leptihn, S. In vitro and in vivo evaluation of the biofilm-degrading Pseudomonas phage Motto, as a candidate for phage therapy. Front. Microbial. 15, 344962 (2024).
Sharma, D., Misba, L. & Khan, A. U. Antibiotics versus biofilm: An emerging battleground in microbial communities. Antimicrob. Resist. Infect. Control 8(1), 1 (2019).
Azeredo, J., García, P. & Drulis-Kawa, Z. Targeting biofilms using phages and their enzymes. Curr. Opin. Biotechnol. 68, 251–261 (2021).
Jault, P. et al. Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. Lancet Infect. Dis. 19, 35–45 (2019).
Altamirano, F. L. et al. Phage-antibiotic combination is a superior treatment against Acinetobacter baumannii in a preclinical study. EBioMedicine 80, 104045 (2022).
Aghaee, B. L., Khan Mirzaei, M., Alikhani, M. Y., Mojtahedi, A. & Maurice, C. F. Improving the inhibitory effect of phages against Pseudomonas aeruginosa isolated from a burn patient using a combination of phages and antibiotics. Viruses 13, 334 (2021).
Kebriaei, R. et al. Eradication of Biofilm-Mediated Methicillin-Resistant Staphylococcus aureus Infections In Vitro: Bacteriophage-Antibiotic Combination. Microbiol. Spectr. 10, e00411-e422 (2022).
Grygorcewicz, B. et al. Environmental phage-based cocktail and antibiotic combination effects on Acinetobacter baumannii biofilm in a human urine model. Microb. Drug Resist. 27, 25–35 (2021).
Ferry, T. et al. Personalized bacteriophage therapy to treat pandrug-resistant spinal Pseudomonas aeruginosa infection. Nat. Commun. 13, 4239 (2022).
Chang, R. Y. et al. The effects of different doses of inhaled bacteriophage therapy for Pseudomonas aeruginosa pulmonary infections in mice. Clin. Microbiol. Infect. 28, 983–989 (2022).
Hotterbeekx, A., Kumar-Singh, S., Goossens, H. & Malhotra-Kumar, S. In vivo and In vitro Interactions between Pseudomonas aeruginosa and Staphylococcus spp. Front. Cell. Infect. Microbiol. 7, 106 (2017).
Leclair, L. W. & Hogan, D. A. Mixed bacterial-fungal infections in the CF respiratory tract. Med. Mycol. 48(Supplement_1), S125–S132 (2010).
O’Brien, S. & Fothergill, J. L. The role of multispecies social interactions in shaping Pseudomonas aeruginosa pathogenicity in the cystic fibrosis lung. FEMS Microbiol. Lett. 364, fnx128 (2017).
Alam, F., Catlow, D., Di Maio, A., Blair, J. M. & Hall, R. A. Candida albicans enhances meropenem tolerance of Pseudomonas aeruginosa in a dual-species biofilm. J. Antimicrob. Chemother. 75, 925–935 (2020).
Roszak, M. et al. Bacteriophage–ciprofloxacin combination effectiveness depends on Staphylococcus aureus–Candida albicans dual-species communities’ growth model. Microb. Drug Resist. 28(6), 613–622 (2022).
Łusiak-Szelachowska, M. et al. Bacteriophages and antibiotic interactions in clinical practice: What we have learned so far. J. Biomed. Sci. 29, 1–7 (2022).
Acknowledgements
The authors would like to thank the Vellore Institute of Technology for the partial support provided by the VIT-SEED grant.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
P.M.: Conceptualization, Data curation, Formal analysis, Study design, Methodology, Funding acquisition, Writing—original draft. B.L.: Validation, Visualization, Writing—review and editing. R.N.: Investigation, Project administration, Supervision. S.L.: Study design, Data interpretation, Resources, Funding acquisition, Supervision, Validation, Writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manohar, P., Loh, B., Nachimuthu, R. et al. Phage-antibiotic combinations to control Pseudomonas aeruginosa–Candida two-species biofilms. Sci Rep 14, 9354 (2024). https://doi.org/10.1038/s41598-024-59444-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59444-2
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.