Abstract
Diabetic nephropathy (DN) is one of the most prevalent and severe complications of diabetes mellitus (DM) and is associated with increased morbidity and mortality. We aimed to investigate the associations between red, processed, and white meat consumption and the odds of developing kidney damage and DN in women. We enrolled 105 eligible women with DN and 105 controls (30–65 years). A validated and reliable food frequency questionnaire (FFQ) was used to evaluate the consumption of red, processed, and white meat. Biochemical variables and anthropometric measurements were assessed for all patients using pre-defined protocols. Binary logistic regression was conducted to examine possible associations. The results of the present study showed that there was a direct significant association between high consumption of red meat and processed meats and odds of microalbuminuria (red meat 2.30, 95% CI 1.25, 4.22; P-value = 0.007, processed meat: OR 2.16, 95% CI 1.18, 3.95; P-value = 0.01), severe albuminuria (red meat OR 3.25, 95% CI 1.38, 7.46; P-value = 0.007, processed meat: OR 2.35, 95% CI 1.01, 5.49; P-value = 0.04), BUN levels (red meat: OR 2.56, 95% CI 1.10, 5.93; P-value = 0.02, processed meat: OR 2.42, 95% CI 1.04, 5.62; P-value = 0.03), and DN (red meat 2.53, 95% CI 1.45, 4.42; P-value = 0.001, processed meat: OR 2.21; 95% CI 1.27, 3.85; P-value = 0.005). In summary, our study suggests that higher consumption of red and processed meat sources may be associated with microalbuminuria, severe albuminuria, higher BUN level, and higher odds of DN.
Similar content being viewed by others
Introduction
One of the most prevalent and severe side effects of diabetes mellitus is diabetic nephropathy (DN)1, which is linked to higher mortality and morbidity rates in diabetic individuals2. It is projected that as diabetes becomes more common, the prevalence of DN will also rise significantly if DN prevention does not improve promptly3,4.
Diabetes-related kidney damage, known as DN, is characterized by elevated blood pressure, decreased kidney function, and macroalbuminuria (urinary albumin excretion > 300 mg/day), among other symptoms1,5. "More than 50,000 diabetic people began therapy for end-stage renal disease (ESRD) in the US in 2014, compared to more than 40,000 in 2000" and "Consuming red and processed meat can increase oxidative stress and inflammation"6. Similarly, over 40% of Japanese diabetes patients in Asian nations have DN7. Ethnicity, family history, dyslipidemia, hypertension, insulin resistance, gestational diabetes, obesity, dyslipidemia, and high blood pressure are important risk factors for DN, some of which are controllable8,9,10. DN is the leading cause of ESRD in high-income countries, affecting around 25% of individuals with type 2 diabetes (T2D)11. Obesity, inactivity, and a poor diet are among the variables that may be contributing to the rise in the prevalence of type 2 diabetes mellitus (T2DM)12,13.
Diet composition significantly impacts insulin sensitivity and the chance of developing T2D14, which may help explain the considerable effect of dietary variables on the risk of T2D. Red meat, which includes beef, lamb, pork, and game, is an animal protein. It can be further divided into processed red meat (PRM) and unprocessed red meat (URM), depending on whether it has been altered to extend its shelf life through curing, smoking, salting, or adding chemical preservatives15. According to specific research, eating PRM or URM is linked favorably to developing T2D and insulin resistance16,17,18,19. Furthermore, it has been demonstrated that excessive consumption of red meat is strongly linked to higher levels of high-sensitivity C-reactive protein (hs-CRP)20. In contrast, consuming processed meat is linked to higher levels of interleukin 6 (IL-6) and lower tumor necrosis factor-alpha (TNF-) levels21. Consuming red and processed meat can increase oxidative stress and inflammation20,22,23,24,25. Oxidative stress is a typical byproduct of numerous metabolic pathways, including hyperglycemia itself, which are implicated in the pathogenesis of DN26. The main factor in the development of DN is an increase in reactive oxygen species (ROS) brought on by hyperglycemia27. Indeed, red meat is frequently discovered to contain nitrites, nitrates, heme iron, and advanced glycation end-products (AGEs)28. It is significant to note that individuals with ESRD have higher levels of circulatory AGEs, and dietary AGEs have been hypothesized to contribute to DM because of their oxidative capabilities29. The food sources acquired from the main food groups, particularly protein intake from different sources, are effective in eliciting insulin resistance and whole-body insulin sensitivity, and therefore inflammation, or directly in the development of inflammation21,30,31,32,33,34,35. However, some studies have found that fish and its byproducts can positively impact inflammatory markers36,37,38. According to one study, adding chicken to the usual diet (UD) instead of red meat decreased the urine albumin excretion rate (UAER) by 46%39, whilst withdrawing red meat from the diet reduced the UAER40. Also, a dietary pattern with white meats includes chicken and fish as the only meat protein source has been shown to decrease the glomerular filtration rate (GFR) in the hyper-filtering normoalbuminuric insulin-dependent diabetes mellitus (IDDM) sufferers41. Higher dietary intake of animal fat and two or more servings per week of red meat may increase the risk for microalbuminuria42; indeed, evidence from animal and human studies suggests that high protein consumption, especially animal protein, may accelerate the decline in GFR43,44,45. Urinary protein excretion, serum creatinine and uric acid levels, blood urea nitrogen (BUN) levels, and oxidative stress have all been documented to rise significantly in response to the elevated protein concentrations46.
Based on existing research, it seems that the consumption of red meat, processed meat, and white meat may be linked to the development of kidney damage and a condition known as Diabetic Nephropathy (DN). However, up to this point, no comprehensive study has been conducted to explore these connections. In light of this gap in the literature, we aimed to investigate the potential associations between the consumption of red meat, processed meat, and white meat, and the likelihood of women developing kidney damage and Diabetic Nephropathy.
Results
General characteristics of study population
This case–control study included 210 participants. The clinical characteristics of the participants are presented in Table 1. The mean and standard deviation (SD) for age, weight, and BMI of the individuals were 55.37 ± 7.07 years, 72.49 ± 12.71 kg, and 28.09 ± 4.59 kg/m2, respectively. In total, 50% of the participants had a history of nephropathy, and 22.4% had a history of cardiovascular disease (CVD).
General characteristics and dietary intakes of participants according to intakes of red, white, and processed meat
The general characteristics of the study among participants with low and high red, white, and processed meat intake are shown in Table 2. In the case group, a positive and significant difference was observed between the levels of FBS (P-value = 0.02) and Cr (P-value = 0.04) and the amount of red meat intake. No significant differences were found in other variables (P-value > 0.05). In the control group, a significant difference in ACIE intake was observed (P-value = 0.04). Greater red meat intake was associated with higher FBS (P-value = 0.05), TC (P-value = 0.06), LDL-c (P-value = 0.03), BUN (P-value = 0.05), and albumin (P-value = 0.004) levels. A significant inverse difference was observed between DBP (P-value = 0.007) and TC (P-value = 0.02) with the intake of white meat in the subject group. More consumption of white meat was associated with lower levels of DBP and TC in the case group, whilst in the control group, higher white meat intake was associated with lower HbA1c (P-value = 0.03), TG (P-value = 0.03), and albumin (P-value = 0.002). In the case group, higher processed meat intake was associated with higher FBS (P-value = 0.05) and Cr (P-value = 0.02). In the control group, a positive and significant difference was found between the level of FBS and the amount of processed meat consumption (P-value = 0.03).
The dietary intake of the study participants, based on the mean consumption of red meat, white meat, and processed meat, is presented in Table 3. After adjustment for confounders (age and total energy intake), a significant positive difference was observed between the mean values of total fat, MUFA, oleic acid, B5, vitamin K, vitamin E, vitamin A, sodium, calcium, glucose, galactose, fructose, and sucrose with the intake of red meat. There was also a significant inverse difference between the mean values of vitamin E, B5, glucose, and fructose with the intake of red meat (P-value < 0.05). In the adjusted model, there was a significant direct difference between the mean values of protein, oleic acid, B5, vitamin E, potassium, calcium, phosphor, magnesium, and sucrose with the consumption of white meat, except for oleic acid (P-value < 0.05). In the adjusted model, a significant direct difference was observed between the mean values of MUFA, oleic acid, B6, vitamin K, sodium, calcium, magnesium, galactose, and sucrose with the intake of processed meat, except for magnesium (P-value < 0.05).
The association between red, white, and processed meat and odds of DN, ACR, GFR and increase BUN
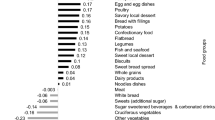
Binary logistic regression was used, in both crude and adjusted models (adjustment for confounders such as age, energy intake, albumin, hemoglobin, physical activity, CVD, and disease duration), to investigate the association between consumption of different types of meat with the odds of DN (Table 4). There was a significant direct relationship between high consumption of red meat (OR 2.53, 95% CI 1.45, 4.42; P-value = 0.001) and odds of DN, which remained significant after adjusting for confounding variables (OR 2.62, 95% CI 1.39, 4.93; P-value = 0.003). A higher intake of white meat was associated with a reduction in the risks of DM by 81% in the crude model (OR 0.19; 95% CI 0.10, 0.34; P-value 0.001), remained significant after adjusting for confounding variables (OR 0.20 95% CI 0.10, 0.40; P-value < 0.001), equating to an 80% reduction in odds of DN. The odds of DN in individuals with a high intake of processed meats is 2.21 times higher than the reference group (OR 2.21; 95% CI 1.27, 3.85; P-value = 0.005), decreased to 2.19 after adjustment (OR 2.19; 95% CI 1.17, 4.12; P-value = 0.01) (Fig. 1).
There was a direct significant relationship between high consumption of red meat and odds of microalbuminuria (OR 2.30, 95% CI 1.25, 4.22; P-value = 0.007) and severe albuminuria (OR 3.25, 95% CI 1.38, 7.46; P-value = 0.007). Also, this significant association remained even after adjustment for potential confounding variables. The occurrence of microalbuminuria and severe albuminuria were 2.46 and 3.22 times greater, respectively, in high consumption of red meat compared to low intake (Table 4). In the crude model, there was an inverse association between higher consumption of white meat compared with low intake associated with odds of microalbuminuria (OR 0.21, 95% CI 0.11, 0.41; P-value < 0.001) and severe albuminuria (OR 0.13, 95% CI 0.05, 0.34; P-value < 0.001). High consumption of white meat, compared with low intake, was associated with lower odds of microalbuminuria (OR 0.23, 95% CI 0.11, 0.47; P-value < 0.001) and severe albuminuria (OR 0.13, 95% CI 0.04, 0.39; P-value < 0.001). In the crude model, there was a direct significant association between higher intake of processed meats, compared to low intake, and higher odds of microalbuminuria (OR 2.16, 95% CI 1.18, 3.95; P-value = 0.01) and severe albuminuria (OR 2.35, 95% CI 1.01, 5.49; P-value = 0.04) in participants. In the adjusted model, the odds of severe albuminuria were 2.16 times greater when participants consumed more processed meats (OR 2.16, 95% CI 0.81, 5.76; P-value = 0.02) (Table 4, Fig. 2).
In the adjusted model, higher consumption of red meat was associated with higher odds of mild to severe GFR decrease (OR 2.87; 95% CI 1.10, 7.51; P-value = 0.03). And also, the odds of mild to severe GFR decrease were 2.55 times higher when participants consumed more processed (OR 2.55, 95% CI 1.02, 6.53; P-value = 0.05) (Table 4, Fig. 3).
In the crude model, there was a direct significant association between consumption of red meat and greater odds of mild to severe increased BUN (OR 2.56, 95% CI 1.10, 5.93; P-value = 0.02). Patients with higher consumption of processed meats had 2.42 times higher odds of increased BUN (OR 2.42, 95% CI 1.04, 5.62; P-value = 0.03) in the crude model (Table 4, Fig. 4).
Discussion
To the best of the authors' knowledge, this study is the first to investigate the relationship between the prevalence of DN, renal function indicators, and the consumption of various types of meat. The results of the current case–control study demonstrated that increased consumption of red and processed meat sources was associated with microalbuminuria, severe albuminuria, higher BUN levels, and higher odds ratios for developing DN. In the adjusted model, an inverse relationship between GFR and the consumption of red and processed meat was observed. Individuals with high consumption of white meat sources had lower odds ratios for microalbuminuria, severe albuminuria, and DN.
The results of the current case–control study align with previous research on the relationship between the consumption of various types of meat and renal function in a healthy population. Notably, a study involving 3000 women found that a dietary intake high in animal fat and two or more servings of red meat was associated with microalbuminuria42. In a cross-sectional study with a population of 19,000 people, the Western dietary style was linked to hyper-albuminuria due to its high consumption of saturated fatty acids. However, polyunsaturated fatty acids (PUFAs) and trans fatty acids were neither associated with hyper-albuminuria nor with the estimated glomerular filtration rate (eGFR)47. A previous study reported that high scores for the Western dietary pattern were correlated with microalbuminuria and a rapid decline in eGFR48. Furthermore, a higher intake of long-chain omega-3 PUFAs and fish was linked to a decreased incidence of chronic kidney disease (CKD) in those over 50, although this connection was not found with the consumption of total omega-3 and omega-6 PUFAs49.
The findings of the current case–control study indicated that higher consumption of red meat was associated with increased odds of DN, which aligns with cohort studies conducted in healthy populations. The frequency of chronic kidney disease (CKD) in a healthy population showed inconsistent correlations with processed meat50,51 and fish intake50,52. In the present investigation, the prevalence of DN was positively correlated with consuming processed meat and negatively correlated with white meat intake. Following healthy eating patterns in diabetic patients has been shown to help maintain optimal kidney function53,54,55,56,57. Studies on the amount of protein necessary to maintain renal function have produced conflicting results. Both the quantity and source of dietary protein have been associated with renal dysfunction and tissue damage in both healthy and diabetic adult58. Moreover, several studies evaluating the effects of low protein diets (LPD) in animal models have found that LPD has reno-protective benefits in the presence of renal disorders59,60. In animal models of type 2 diabetes with advanced diabetic nephropathy, LPD has been effective in restoring autophagy by suppressing the mechanistic target of rapamycin complex (mTORC1)61.
However, despite the beneficial effects of LPD reported in animal models and earlier research40,62 a meta-analysis found no advantage of a low-protein diet over a higher protein diet for diabetic nephropathy, improving glomerular filtration rate (GFR), or reducing proteinuria63. An observational study of 6213 subjects with type 2 diabetes found no clear benefit in renal parameters from a low-protein diet64. According to randomized controlled trials (RCTs), the type of protein is just as crucial as the quantity of protein40,65. Similar to LPD, diet protein based on chicken reduced and elevated blood levels of UAER and PUFAs, respectively, in research done on T2D patients with macroalbuminuria40. The results in type 1 diabetes patients were consistent with the study by Mello et al.62. The current case–control study's findings align with previous research that suggested a connection between increased consumption of white protein sources and a reduced risk of DN. Chicken has been shown to reduce urinary albumin excretion rate (UAER) by 36% in type 2 diabetes (T2D) patients with microalbuminuria compared to a typical diet39. Additionally, chicken and a low-protein diet (LPD) caused total cholesterol (TC), low-density lipoprotein (LDL), and alpha-lipoprotein levels in individuals with microalbuminuria to decrease, although glomerular filtration rate (GFR) levels in people with normo-albuminuria declined39. This finding is consistent with the results of studies on type 1 diabetes and the replacement of animal protein with plant protein41,66,67 The mechanism behind this effect may be related to the reduction of renal plasma flow43.
Inflammation may help explain renal dysfunction. According to the Multi-Ethnic Study of Atherosclerosis (MESA), inflammatory markers, including high-sensitivity C-reactive protein (hs-CRP) and E-selectin, were negatively correlated with a balanced diet pattern that includes fruits, vegetables, whole grains, and seafood. In contrast, the Western food pattern, which is rich in red meat and processed foods high in fat, increased inflammatory markers such as hs-CRP, interleukin-6 (IL-6), E-selectin, cytokine regulation of cellular adhesion molecule-1 (CAM-1), and vascular cell adhesion molecule-1 (VCAM-1)68,69.
The quantity of protein is similar in red, white, and processed meat from various sources, but the fatty acid composition differs. Compared to red and processed meat, white meat contains higher levels of monounsaturated fatty acids (MUFAs) and polyunsaturated fatty acids (PUFAs) and lower levels of saturated fatty acids (SFAs)70. Consumption of foods low in PUFAs is inversely related to inflammatory markers71 and can cause endothelial dysfunction72,73. The difference in their fatty acid composition is likely responsible for the superior benefits of white protein sources on renal function compared to red and processed meat. In summary, endothelial dysfunction can disrupt normal kidney function by affecting blood flow regulation, promoting inflammation and oxidative stress, and contributing to conditions like hypertension and diabetes, all of which can lead to renal dysfunction and kidney disease.
High levels of serum cholesterol are known to be a risk factor for diabetic nephropathy (DN) in type 2 diabetes (T2D) patients74. Reducing the intake of saturated fatty acids (SFAs) and increasing the intake of monounsaturated fatty acids (MUFAs) and polyunsaturated fatty acids (PUFAs) can lower total cholesterol (TC)75. In the present study, patients with higher scores for red and processed meat consumption had a higher intake of saturated fatty acids. However, this association was inverse for patients with higher scores for white meat consumption. Additionally, those with higher intakes of white meat sources had lower TC.
Moderate protein restriction is associated with decreased urinary albumin excretion rate (UAER) in type 2 diabetes76,77, although one study produced conflicting results39. It has been suggested that switching to white meat, such as chicken or fish, may be more advantageous than merely reducing overall protein intake78. An observational study found that consuming more protein sources from white meat, including chicken and fish, improves kidney function in diabetic patients, which aligns with the findings of a recent study78. The different amino acid composition of white meat and red meat may be one of the reasons for the advantages of substituting white meat for red meat79. Beef, for instance, has higher levels of arginine and glycine compared to chicken, which can affect kidney function79, although in patients with type 1 diabetes, plasma amino acid levels were not significantly different in those following a diet based on chicken and fish compared to beef41.
The present study has several strengths, including being the first to evaluate the association between types of meat and diabetic nephropathy (DN). Food intake was assessed using a valid and reliable food frequency questionnaire (FFQ), and sampling was conducted at a single center over an appropriate period. However, this study also had limitations that should be noted. It employed a case–control study design, which can introduce bias. All participants were female, limiting generalizability to males. The matching of the case and control groups was based on age and duration of diabetes, which may influence the results due to the presence of other confounding variables, although most confounding variables were considered in the analysis. Further investigations into the association between kidney function factors and the consumption of red, white, and processed meat could provide deeper insights.
To our knowledge, this is the first study to assess the association between the prevalence of DN and kidney function markers and the consumption of different types of meat. In conclusion, we observed that higher consumption of red and processed meat sources was linked to microalbuminuria, severe albuminuria, higher blood urea nitrogen (BUN) levels, and a higher odds ratio of DN. Given the inconclusive literature, we recommend further well-controlled RCT studies in different populations and ethnicities with other designs such as cohorts.
Methods and materials
Subjects
In this case–control study, a total of 210 participants, comprising 105 cases and 105 controls aged 30–65 years, with a 3- to 10-year history of type 2 diabetes (T2D), were referred to the Kowsar Diabetes Clinic in Semnan, Iran, between July and December 2016. The diagnosis of diabetes in this study was based on the American Diabetes Association's new diagnostic criteria, which include glycosylated hemoglobin (HbA1c) ≥ 6.5%, fasting blood glucose (FBG) ≥ 126 mg/dL, 2-h post-load blood glucose (2hrBG) ≥ 200 mg/dL, or, in a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥ 200 mg/dL (11.1 mmol/L)80. Participants with a previous history of cancer, autoimmune disorders, liver disease, coronary angiography, myocardial infarction, or stroke were excluded from the study. Additionally, individuals with poor responses to the Food Frequency Questionnaire (FFQ) or total energy intake below 500 or above 3500 kcal per day were excluded. All participants in this study read and signed written informed consent before participating. In 2016, the study protocol was approved by the ethics committee of Tehran University of Medical Sciences (TUMS) with the identification number IR.TUMS.REC.1395.2644.
Anthropometric measurements
Body weight (kg) was measured while participants were unshod and wore light clothes, according to standard protocols. Body mass index (BMI) was calculated by dividing weight by the square of height (kg/m2).
Dietary assessment
Dietitians assessed the dietary intake of participants over the past year through face-to-face interviews using a validated Food Frequency Questionnaire (FFQ)81. Dietary intakes were reported and recorded in terms of yearly, monthly, weekly, or daily frequency, and then converted to grams per day using household measurements. The obtained amounts were adjusted for energy intake using the residual method82. The calculation of macro- and micronutrient content and grams of foods was performed using NUTRITIONIST IV software (version 3.5.3.; N‐Squared Computing, Salem, OR, USA).
This study focused on the consumption of three different types of meat as extracted from the FFQ, measured in grams per day: (1) The red meat category included beef, lamb, and sheep/mutton, as well as organ meats like beef liver, kidney, tongue, and heart; (2) White meat comprised fish and poultry, including chicken and turkey; and (3) Processed meats included sausages, Kalbas, hamburgers, Mortadella, and canned fish.
Assessment of DN
DN is defined as the ratio of urinary albumin to creatinine (ACR) ≥ 30 mg/g in a random spot urine sample83, and its’ diagnosis was confirmed by a clinician.
Assessment of markers of kidney function
GFR is generally accepted as the best overall index of kidney function and is the most important parameter to determine in the clinical evaluation of kidney function. Normal GFR ≥ 90 mL/min/1.73 m2 and mild to severe GFR (< 90 mL/min/1.73 m2) is, by itself, sufficient for the diagnosis of chronic kidney disease (CKD), regardless of the presence or absence of other markers of kidney damage84.
Patients were then divided into two groups: ‘normal’, if BUN was ≤ 20, and ‘high’ if BUN was > 2085. Participants' albuminuria was determined based on ACR categories using the Epidemiology Collaboration (EPI) equation formula, as reported by Levey et al.86: Normal < 30 mg/g, micro 30–300 mg/g, and severe 300 mg/g.
Assessment of blood pressure
Systolic and diastolic blood pressure (SBP, DBP) of participants were measured on the left arm, after 15 min of rest, by using an automatic sphygmomanometer.
Blood parameters
Biochemical variables consisted of fasting blood sugar (FBS), HbA1c, 2hrBG, kidney function tests [BUN, total serum creatinine (Cr), albumin6], and lipid profile such as total cholesterol (TC), high-density lipoprotein cholesterol (HDL_C), low-density lipoprotein cholesterol (LDL_C), and triglycerides (TG), and were obtained from the most recent 3 months of participants medical records.
Demographic variables and physical activity
Through a demographic questionnaire, demographic information including weight, height, age, medical history, and the type of drugs/medicines (including angiotensin-converting enzyme inhibitors (ACE), Beta-blockers, Metformin, Sulfonylurea, and Insulin) was obtained. The physical activity of the participants was assessed using the International Physical Activity Questionnaire (IPAQ). The scores of the IPAQ were categorized into three levels of physical activity: 'low physical activity' (point score < 600 metabolic equivalents (MET)/hour per week), 'moderate physical activity' (point score between 600 and 3000 MET/hour per week), and 'high physical activity' (point score > 3000 MET/hour per week).
Statistical analysis
The normality of the quantitative variables was evaluated using the Kolmogorov–Smirnov test. Quantitative variables, including age, height, weight, and BMI, were compared between cases, and controls were described as mean ± standard deviation9, and for categorical variables, frequency (%) was used. Independent t-test and chi-square tests were used for quantitative variables and categorical variables across the low adherence and high adherence to the red, white, and processed meat between cases and controls, respectively. To characterize the distribution of the qualitative variables across the low adherence and high adherence to the red, white, and processed meat between cases and controls in an adjusted model, we used Analysis of Covariance (ANCOVA). Logistic regression was used to determine the association between food groups and odds of DN. Variables including age, energy intake, Albumin, hemoglobin, physical activity, history of cardiovascular diseases (CVD), and disease duration were controlled for in the adjusted model. SPSS software (Version 25, SPSS Inc., Chicago, IL, USA) was used to analyze data and P < 0.05 was considered statistically significant.
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of Tehran University of medical sciences (IR.TUMS.MEDICINE.REC.1401.811) and is acknowledged by authors. All participants signed a written informed consent.
Statement
We state that all methods are based on the relevant guidelines and regulations.
Data availability
The data that support the findings of this study are available from Dr. Khadijeh Mirzaei but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Dr. Khadijeh Mirzaei.
Abbreviations
- ARB:
-
Angiotensin receptor blockers
- ACIE:
-
Angiotensin-converting enzyme inhibitors
- ANCOVA:
-
Analysis of covariance
- AGEs:
-
Advanced glycation end products
- ACR:
-
Albumin to creatinine
- BUN:
-
Blood urea nitrogen
- BMI:
-
Body mass index
- Cr:
-
Creatinine
- CVD:
-
Cardiovascular diseases
- CKD:
-
Chronic kidney disease
- CAM-1:
-
Cellular adhesion molecule
- DN:
-
Diabetic nephropathy
- DM:
-
Diabetes mellitus
- DASH:
-
Dietary approaches to stop hypertension
- DBP:
-
Diastolic blood pressure
- ESRD:
-
End-stage renal disease
- EPI:
-
Epidemiology collaboration
- eGFR:
-
Estimated glomerular filtration rate
- FBS:
-
Fasting blood sugar
- FBG:
-
Fasting blood glucose
- FFQ:
-
Food Frequency Questionnaire
- GFR:
-
Glomerular filtration rate
- 2hrBG:
-
2-H post-load blood glucose
- HbA1c:
-
Glycosylated hemoglobin A1c
- HDL-C:
-
High-density lipoprotein cholesterol
- Hs-CRP:
-
High-sensitivity C-reactive protein
- LDL-C:
-
Low-density lipoprotein cholesterol
- IPAQ:
-
International Physical Activity Questionnaire
- IDDM:
-
Insulin-dependent diabetes mellitus
- IL-6:
-
Interleukin 6
- LPD:
-
Low protein diet
- MUFAs:
-
Mono unsaturated fatty acids
- MESA:
-
Multi-Ethnic Study of Atherosclerosis
- mTORC1:
-
Mechanistic target of rapamycin complex 1
- PRM:
-
Processed red meat
- PUFAs:
-
Poly unsaturated fatty acids
- ROS:
-
Reactive oxygen species
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- SFAs:
-
Saturated fatty acids
- TNF-α:
-
Tumor necrosis factor alpha
- T2D:
-
Type 2 diabetes
- T2DM:
-
Type 2 diabetes mellitus
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- URM:
-
Unprocessed red meat
- UD:
-
Usual diet
- UAER:
-
Urinary albumin excretion rate
- VCAM-1:
-
Vascular cell adhesion molecule 1
References
Inker, L. A. et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am. J. Kidney Dis. 63, 713–735 (2014).
Valencia, W. M. & Florez, H. How to prevent the microvascular complications of type 2 diabetes beyond glucose control. BMJ 356, i6505 (2017).
Gheith, O., Farouk, N., Nampoory, N., Halim, M. A. & Al-Otaibi, T. Diabetic kidney disease: World wide difference of prevalence and risk factors. J. Nephropharmacol. 5, 49 (2016).
Stenvinkel, P. Chronic kidney disease: A public health priority and harbinger of premature cardiovascular disease. J. Intern. Med. 268, 456–467 (2010).
Rabieenia, E., Jalali, R. & Mohammadi, M. Prevalence of nephropathy in patients with type 2 diabetes in Iran: A systematic review and meta-analysis based on geographic information system (GIS). Diabetes Metab. Syndr. Clin. Res. Rev. 14, 1543–1550 (2020).
Burrows, N. R., Hora, I., Geiss, L. S., Gregg, E. W. & Albright, A. Incidence of end-stage renal disease attributed to diabetes among persons with diagnosed diabetes—United States and Puerto Rico, 2000–2014. Morb. Mortal. Wkly. Rep. 66, 1165 (2017).
Gohda, T. & Tomino, Y. A paradigm shift for the concept of diabetic nephropathy. Juntendo Med. J. 60, 293–299 (2014).
Raile, K. et al. Diabetic nephropathy in 27,805 children, adolescents, and adults with type 1 diabetes: Effect of diabetes duration, A1C, hypertension, dyslipidemia, diabetes onset, and sex. Diabetes Care 30, 2523–2528 (2007).
Tapp, R. J. et al. Albuminuria is evident in the early stages of diabetes onset: Results from the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Am. J. Kidney Dis. 44, 792–798 (2004).
Gall, M.-A., Hougaard, P., Borch-Johnsen, K. & Parving, H.-H. Risk factors for development of incipient and overt diabetic nephropathy in patients with non-insulin dependent diabetes mellitus: Prospective, observational study. BMJ 314, 783 (1997).
de Boer, I. H. et al. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 305, 2532–2539 (2011).
Jannasch, F., Kröger, J. & Schulze, M. B. Dietary patterns and type 2 diabetes: A systematic literature review and meta-analysis of prospective studies. J. Nutr. 147, 1174–1182 (2017).
Rojas-Carranza, C. A. et al. Diabetes-related neurological implications and pharmacogenomics. Curr. Pharm. Des. 24, 1695–1710 (2018).
Snowdon, D. A. & Phillips, R. L. Does a vegetarian diet reduce the occurrence of diabetes?. Am. J. Public Health 75, 507–512 (1985).
Wolk, A. Potential health hazards of eating red meat. J. Intern. Med. 281, 106–122 (2017).
Pan, A. et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am. J. Clin. Nutr. 94, 1088–1096 (2011).
Consortium & I,. Association between dietary meat consumption and incident type 2 diabetes: The EPIC-InterAct study. Diabetologia 56, 47–59 (2013).
Marí-Sanchis, A. et al. Association between pre-pregnancy consumption of meat, iron intake, and the risk of gestational diabetes: the SUN project. Eur. J. Nutr. 57, 939–949 (2018).
Talaei, M., Wang, Y.-L., Yuan, J.-M., Pan, A. & Koh, W.-P. Meat, dietary heme iron, and risk of type 2 diabetes mellitus: The Singapore Chinese Health Study. Am. J. Epidemiol. 186, 824–833 (2017).
Montonen, J. et al. Consumption of red meat and whole-grain bread in relation to biomarkers of obesity, inflammation, glucose metabolism and oxidative stress. Eur. J. Nutr. 52, 337–345 (2013).
Schwedhelm, C. et al. Plasma inflammation markers of the tumor necrosis factor pathway but not C-reactive protein are associated with processed meat and unprocessed red meat consumption in Bavarian adults. J. Nutr. 147, 78–85 (2017).
Azadbakht, L. & Esmaillzadeh, A. Red meat intake is associated with metabolic syndrome and the plasma C-reactive protein concentration in women. J. Nutr. 139, 335–339 (2009).
Damiao, R. et al. Dietary intakes associated with metabolic syndrome in a cohort of Japanese ancestry. Br. J. Nutr. 96, 532–538 (2006).
Esmaillzadeh, A. et al. Dietary patterns and markers of systemic inflammation among Iranian women. J. Nutr. 137, 992–998 (2007).
Ley, S. H. et al. Associations between red meat intake and biomarkers of inflammation and glucose metabolism in women. Am. J. Clin. Nutr. 99, 352–360 (2014).
Kopel, J., Pena-Hernandez, C. & Nugent, K. Evolving spectrum of diabetic nephropathy. World J. Diabetes 10, 269 (2019).
Krishan, P. & Chakkarwar, V. A. Diabetic nephropathy: Aggressive involvement of oxidative stress. J. Pharm. Educ. Res. 2, 35 (2011).
Kim, Y., Keogh, J. & Clifton, P. A review of potential metabolic etiologies of the observed association between red meat consumption and development of type 2 diabetes mellitus. Metabolism 64, 768–779 (2015).
Semba, R. D., Nicklett, E. J. & Ferrucci, L. Does accumulation of advanced glycation end products contribute to the aging phenotype?. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 65, 963–975 (2010).
Hodgson, J. M., Ward, N. C., Burke, V., Beilin, L. J. & Puddey, I. B. Increased lean red meat intake does not elevate markers of oxidative stress and inflammation in humans. J. Nutr. 137, 363–367 (2007).
O’Connor, L. E., Kim, J. E., Clark, C. M., Zhu, W. & Campbell, W. W. Effects of total red meat intake on glycemic control and inflammatory biomarkers: A meta-analysis of randomized controlled trials. Adv. Nutr. 12, 115–127 (2021).
DeFronzo, R. A. From the triumvirate to the ominous octet: A new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 58, 773–795 (2009).
O’Connor, L. E., Paddon-Jones, D., Wright, A. J. & Campbell, W. W. A Mediterranean-style eating pattern with lean, unprocessed red meat has cardiometabolic benefits for adults who are overweight or obese in a randomized, crossover, controlled feeding trial. Am. J. Clin. Nutr. 108, 33–40 (2018).
Maki, K. C. et al. Substituting lean beef for carbohydrate in a healthy dietary pattern does not adversely affect the cardiometabolic risk factor profile in men and women at risk for type 2 diabetes. J. Nutr. 150, 1824–1833 (2020).
Turner, K. M., Keogh, J. B. & Clifton, P. M. Red meat, dairy, and insulin sensitivity: A randomized crossover intervention study. Am. J. Clin. Nutr. 101, 1173–1179 (2015).
Pischon, T. et al. Habitual dietary intake of n-3 and n-6 fatty acids in relation to inflammatory markers among US men and women. Circulation 108, 155–160 (2003).
Trebble, T. et al. Inhibition of tumour necrosis factor-α and interleukin 6 production by mononuclear cells following dietary fish-oil supplementation in healthy men and response to antioxidant co-supplementation. Br. J. Nutr. 90, 405–412 (2003).
Ciubotaru, I., Lee, Y.-S. & Wander, R. C. Dietary fish oil decreases C-reactive protein, interleukin-6, and triacylglycerol to HDL-cholesterol ratio in postmenopausal women on HRT. J. Nutr. Biochem. 14, 513–521 (2003).
Gross, J. L. et al. Effect of a chicken-based diet on renal function and lipid profile in patients with type 2 diabetes: A randomized crossover trial. Diabetes Care 25, 645–651 (2002).
de Mello, V. D., Zelmanovitz, T., Perassolo, M. S., Azevedo, M. J. & Gross, J. L. Withdrawal of red meat from the usual diet reduces albuminuria and improves serum fatty acid profile in type 2 diabetes patients with macroalbuminuria. Am. J. Clin. Nutr. 83, 1032–1038 (2006).
Pecis, M., Azevedo, M. J. D. & Gross, J. L. Chicken and fish diet reduces glomerular hyperfiltration in IDDM patients. Diabetes Care 17, 665–672 (1994).
Lin, J., Hu, F. B. & Curhan, G. C. Associations of diet with albuminuria and kidney function decline. Clin. J. Am. Soc. Nephrol. 5, 836–843 (2010).
Brenner, B. M., Lawler, E. V. & Mackenzie, H. S. The hyperfiltration theory: A paradigm shift in nephrology. Kidney Int. 49, 1774–1777 (1996).
Machado, A. D. et al. Dietary intake of non-dialysis chronic kidney disease patients: The PROGREDIR study. A cross-sectional study. Sao Paulo Med. J. 136, 208–215 (2018).
Kusano, K., Segawa, H., Ohnishi, R., Fukushima, N. & Miyamoto, K.-I. Role of low protein and low phosphorus diet in the progression of chronic kidney disease in uremic rats. J. Nutr. Sci. Vitaminol. 54, 237–243 (2008).
Tovar-Palacio, C. et al. Proinflammatory gene expression and renal lipogenesis are modulated by dietary protein content in obese Zucker fa/fa rats. Am. J. Physiol. Ren. Physiol. 300, F263–F271 (2011).
Lin, J. et al. Associations of dietary fat with albuminuria and kidney dysfunction. Am. J. Clin. Nutr. 92, 897–904 (2010).
Lin, J., Fung, T. T., Hu, F. B. & Curhan, G. C. Association of dietary patterns with albuminuria and kidney function decline in older white women: A subgroup analysis from the Nurses’ Health Study. Am. J. Kidney Dis. 57, 245–254 (2011).
Gopinath, B., Harris, D. C., Flood, V. M., Burlutsky, G. & Mitchell, P. Consumption of long-chain n-3 PUFA, α-linolenic acid and fish is associated with the prevalence of chronic kidney disease. Br. J. Nutr. 105, 1361–1368 (2011).
Haring, B. et al. Dietary protein sources and risk for incident chronic kidney disease: Results from the Atherosclerosis Risk in Communities (ARIC) Study. J. Ren. Nutr. 27, 233–242 (2017).
Mirmiran, P. et al. A prospective study of dietary meat intake and risk of incident chronic kidney disease. J. Ren. Nutr. 30, 111–118 (2020).
Lee, C. C. et al. Association between fish consumption and nephropathy in American Indians—The Strong Heart study. J. Ren. Nutr. 22, 221–227 (2012).
Nettleton, J. A., Steffen, L. M., Palmas, W., Burke, G. L. & Jacobs, D. R. Jr. Associations between microalbuminuria and animal foods, plant foods, and dietary patterns in the Multiethnic Study of Atherosclerosis. Am. J. Clin. Nutr. 87, 1825–1836 (2008).
Hsu, C.-C. et al. Associations between dietary patterns and kidney function indicators in type 2 diabetes. Clin. Nutr. 33, 98–105 (2014).
Fried, L. F., Orchard, T. J. & Kasiske, B. L. Effect of lipid reduction on the progression of renal disease: A meta-analysis. Kidney Int. 59, 260–269 (2001).
Azadbakht, L., Atabak, S. & Esmaillzadeh, A. Soy protein intake, cardiorenal indices, and C-reactive protein in type 2 diabetes with nephropathy: A longitudinal randomized clinical trial. Diabetes Care 31, 648–654 (2008).
Yokoyama, M. et al. Dietary polyunsaturated fatty acids slow the progression of diabetic nephropathy in streptozotocin-induced diabetic rats. Nutr. Res. 30, 217–225 (2010).
Stevens, L. A. et al. Comparative performance of the CKD Epidemiology Collaboration (CKD-EPI) and the Modification of Diet in Renal Disease (MDRD) Study equations for estimating GFR levels above 60 mL/min/1.73 m2. Am. J. Kidney Dis. 56, 486–495 (2010).
Sakaguchi, M. et al. Inhibition of mTOR signaling with rapamycin attenuates renal hypertrophy in the early diabetic mice. Biochem. Biophys. Res. Commun. 340, 296–301 (2006).
Solon-Biet, S. M. et al. The ratio of macronutrients, not caloric intake, dictates cardiometabolic health, aging, and longevity in ad libitum-fed mice. Cell Metab. 19, 418–430 (2014).
Kitada, M. et al. A very-low-protein diet ameliorates advanced diabetic nephropathy through autophagy induction by suppression of the mTORC1 pathway in Wistar fatty rats, an animal model of type 2 diabetes and obesity. Diabetologia 59, 1307–1317 (2016).
Pedrini, M. T., Levey, A. S., Lau, J., Chalmers, T. C. & Wang, P. H. The effect of dietary protein restriction on the progression of diabetic and nondiabetic renal diseases: A meta-analysis. Ann. Intern. Med. 124, 627–632 (1996).
Zhu, H.-G. et al. Efficacy of low-protein diet for diabetic nephropathy: A systematic review of randomized controlled trials. Lipids Health Dis. 17, 1–9 (2018).
Benabe, J. E., Wang, S., Wilcox, J. N. & Martinez-Maldonado, M. Modulation of ANG II receptor and its mRNA in normal rat by low-protein feeding. Am. J. Physiol. Ren. Physiol. 265, F660–F669 (1993).
de Mello, V. D., Zelmanovitz, T., Azevedo, M. J., de Paula, T. P. & Gross, J. L. Long-term effect of a chicken-based diet versus enalapril on albuminuria in type 2 diabetic patients with microalbuminuria. J. Ren. Nutr. 18, 440–447 (2008).
Wiseman, M., Bognetti, E., Dodds, R., Keen, H. & Viberti, G. Changes in renal function in response to protein restricted diet in type 1 (insulin-dependent) diabetic patients. Diabetologia 30, 154–159 (1987).
Becker, G. F. Efeito da dieta hipocalórica de baixo índice glicêmico sobre níveis de grelina, leptina, parâmetros metabólicos e desfechos reprodutivos em mulheres inférteis com excesso de peso: um ensaio clínico randomizado. (2015).
Lopez-Garcia, E. et al. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 80, 1029–1035 (2004).
Nettleton, J. A. et al. Dietary patterns are associated with biochemical markers of inflammation and endothelial activation in the Multi-Ethnic Study of Atherosclerosis (MESA). Am. J. Clin. Nutr. 83, 1369–1379 (2006).
Britten, P., Cleveland, L. E., Koegel, K. L., Kuczynski, K. J. & Nickols-Richardson, S. M. Updated US Department of Agriculture Food Patterns meet goals of the 2010 dietary guidelines. J. Acad. Nutr. Diet. 112, 1648–1655 (2012).
Fernández-Real, J.-M., Broch, M., Vendrell, J. & Ricart, W. Insulin resistance, inflammation, and serum fatty acid composition. Diabetes Care 26, 1362–1368 (2003).
Steer, P., Vessby, B. & Lind, L. Endothelial vasodilatory function is related to the proportions of saturated fatty acids and alpha-linolenic acid in young men, but not in women. Eur. J. Clin. Investig. 33, 390–396 (2003).
Sarabi, M., Vessby, B., Millgård, J. & Lind, L. Endothelium-dependent vasodilation is related to the fatty acid composition of serum lipids in healthy subjects. Atherosclerosis 156, 349–355 (2001).
Ravid, M., Brosh, D., Ravid-Safran, D., Levy, Z. & Rachmani, R. Main risk factors for nephropathy in type 2 diabetes mellitus are plasma cholesterol levels, mean blood pressure, and hyperglycemia. Arch. Intern. Med. 158, 998–1004 (1998).
Mensink, R. P. & Katan, M. B. Effect of dietary fatty acids on serum lipids and lipoproteins. A meta-analysis of 27 trials. Arterioscler. Thromb. J. Vasc. Biol. 12, 911–919 (1992).
Pomerleau, J., Verdy, M., Garrel, D. & Nadeau, M. H. Effect of protein intake on glycaemic control and renal function in type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 36, 829–834 (1993).
Pijls, L., de Vries, H., Donker, A. & Van Eijk, J. The effect of protein restriction on albuminuria in patients with type 2 diabetes mellitus: a randomized trial. Nephrol. Dial. Transplant. 14, 1445–1453 (1999).
Mollsten, A. V., Dahlquist, G. G., Stattin, E.-L. & Rudberg, S. Higher intakes of fish protein are related to a lower risk of microalbuminuria in young Swedish type 1 diabetic patients. Diabetes Care 24, 805–810 (2001).
Ando, A. et al. Effects of dietary protein intake on renal function in humans. Kidney International Supplement (1989).
Association, A. D. 6. Glycemic targets: Standards of medical care in diabetes—2019. Diabetes Care 42, S61–S70 (2019).
Esfahani, F. H., Asghari, G., Mirmiran, P. & Azizi, F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J. Epidemiol. 20, 150–158 (2010).
Willett, W. C., Howe, G. R. & Kushi, L. H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 65, 1220S-1228S (1997).
Molitch, M. E., DeFronzo, R. A., Franz, M. J. & Keane, W. F. Nephropathy in diabetes. Diabetes Care 27, S79 (2004).
Levey, A. S. et al. Nomenclature for kidney function and disease—executive summary and glossary from a Kidney Disease: Improving Global Outcomes (KDIGO) consensus conference. Eur. Heart J. 41, 4592–4598 (2020).
Group & I. G. O. C. W,. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl 3, 1–150 (2013).
Levey, A. S. et al. Nomenclature for kidney function and disease: Executive summary and glossary from a Kidney Disease: Improving Global Outcomes consensus conference. Nephrol. Dial. Transplant. 35, 1077–1084 (2020).
Acknowledgements
This study was supported by Tehran University of Medical Sciences Grant (No: 94-04-161-31155). We thank all the participants in this study, as well as the school of Nutritional and Dietetics at Tehran University of Medical Sciences.
Funding
This study was supported by Tehran University of Medical Sciences (Grant No: 1401-4-212-64149).
Author information
Authors and Affiliations
Contributions
A.M. contributed to conception and design. Z.R., R.Kh., Y.A. and M.R. contributed to all experimental work, F.A. contributed to data and statistical analysis. K.M., supervised the whole project. All authors performed editing and approving the final version of this paper for submission, also participated in the finalization of the manuscript and approved the final draft. All authors read and approved the final manuscript. All authors performed editing and approving the final version of this paper for submission, also participated in the finalization of the manuscript and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mirzababaei, A., Abaj, F., Roumi, Z. et al. Consumption of red, white, and processed meat and odds of developing kidney damage and diabetic nephropathy (DN) in women: a case control study. Sci Rep 14, 10344 (2024). https://doi.org/10.1038/s41598-024-59097-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59097-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.