Abstract
Polycystic ovary syndrome (PCOS) is one of the most common reproductive endocrine metabolic disorders. The lncRNA metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) reportedly can regulate the reproductive system. Despite studies, the alteration of MALAT1 expression in granulosa cells (GCs) from PCOS patients was inconsistent. To evaluate MALAT1 expression in GCs in different PCOS subgroups and its association with PCOS phenotypes, we collected GCs from 110 PCOS cases and 71 controls, and examined MALAT1 expression by quantitative PCR. The results showed MALAT1 expression was upregulated in PCOS cases, especially in insulin resistant (IR) PCOS subgroup, obese PCOS subgroup and non-hyperandrogenic (NHA) PCOS subgroup. MALAT1 expression was positively correlated with BMI and several metabolic parameters in controls. Interestingly, MALAT1 expression was notably associated with some critical endocrine indexes for PCOS, including E2, FSH, LH and LH/FSH ratio. In different PCOS subgroups, we found significant positive correlations with LH/FSH ratio in IR-PCOS and PCOS with normal weight, and with serum T and LH level in NHA-PCOS subgroup. Integrated analysis with lncRNA target databases and PCOS-related databases revealed MALAT1 could participate in PCOS by influencing immune response and lipids metabolism in GCs. In conclusion, MALAT1 was differently expressed in GCs in PCOS, especially in IR, obese and NHA PCOS subgroups. MALAT1 was likely involved in metabolism and immune response in GCs in PCOS. However, more studies are necessary to establish this concept.
Similar content being viewed by others
Introduction
Polycystic ovary syndrome (PCOS) is a common reproductive endocrine metabolic disorder in women of reproductive age, affecting 5–18% of women1,2. Clinical manifestations of PCOS are heterogenous, characterised by excessive androgens, ovulatory dysfunction and polycystic ovarian morphology. Due to the complexity of PCOS, its etiology needs further exploration, which, with advances in research, has suggested that PCOS development partially depends on noncoding RNAs and epigenetic factors3. Ovarian granulosa cells (GCs), are the main site of steroid hormone synthesis in females, and can be involved in the formation of the follicular microenvironment and the growth and development of oocytes4,5. The disturbance of cellular biology and gene expression in GCs is implicated in the development of PCOS6.
Long noncoding RNAs (lncRNAs) consist of 200–800 nucleotides and, despite lacking protein-coding capacity, play vital roles in various cellular activities and human diseases7,8. Metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) is a conserved lncRNA in humans and was initially identified to be upregulated in human lung cancer9. Recently, a few studies have focused on its role in reproductive system, like pregnancy process and PCOS10,11,12,13,14. While studies have shown differential expression of MALAT1 in GCs and peripheral blood from PCOS patients and PCOS-model rats7,10,11,12,13,14, how MALAT1 expression is altered in GCs is inconsistent across studies due to small research cohorts11,13,14. Apart from this, the alterations of MALAT1 expression in GCs in PCOS and in different PCOS subtypes are still unclear.
In our study, we aimed to investigate the changes in MALAT1 expression in GCs by studying a larger cohort of patients, including different subtypes of PCOS. Additionally, we explored the relationship between MALAT1 expression and various clinical parameters, providing the theoretical foundation for clarifying the pathophysiology of PCOS.
Materials and methods
Participants and ethical statement
A total of 181 Chinese women participated in this study, including 110 patients with polycystic ovary syndrome (PCOS) and 71 controls. From October 2015 to June 2016, ovarian granulosa cells were collected from participants undergoing treatment at the Center for Reproductive Medicine, Shandong University. PCOS was diagnosed according to the Rotterdam criteria15, requiring the presence of at least two among the following: (1) clinical and/or biochemical indications of hyperandrogenism; (2) polycystic ovaries, the presence of 12 or more follicles measuring 2–9 mm in diameter in each ovary and/or an ovarian volume of more than 10 mL as determined by ultrasound; (3) oligo- or anovulation, menstrual cycle length of less than 21 or more than 35 days, and/or fewer than eight cycles per year. Participants with other etiologies such as androgen-secreting tumors, Cushing’s syndrome, or congenital adrenal hyperplasia and other hypothalamus, pituitary gland, and ovaries disorders were excluded. Control participants had regular menstrual cycles (26–35 days), normal steroid hormone levels, and normal ovarian morphology. Control participants visited the IVF center because of oviduct and/or male factors related infertility. The long gonadotropin-releasing hormone agonist protocol was applied for participants’ treatment.
This study was approved by Ethics Committee of Hospital for Reproductive Medicine Affiliated to Shandong University and Ethics Committee of Shandong University (No. 2014020) on March 4th, 2014. As well, all experiments involving human patients were in line with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All participants provided informed consent. All experimental protocols were conducted in line with the respective guidelines and regulations approved by the Institutional Review Board of Shandong University.
Ovarian stimulation and granulosa cells (GCs) sampling
All participants who underwent the long gonadotropin-releasing hormone agonist protocol received injections of gonadotropin-releasing hormone agonists at the onset of the mid-luteal phase, and ultrasound scans of follicular development and serum estradiol measurements were performed at 1- to 3-day intervals. When more than 3 follicles were measuring ≥ 18 mm in diameter, an appropriate amount of human chorionic gonadotropin (hCG) was then injected. Thirty-six hours after the hCG injection, oocytes were retrieved under ultrasound guidance. GCs from each participant were derived from several pooled follicles and collected from approximately 40–50 mL of follicular fluid using sterile tubes and isolated using Ficoll-Percoll (Solarbio-Life-Sciences, Beijing, China) as previously described16.
RNA extraction and quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA extraction was conducted from GCs isolated from approximately 40–50 ml of follicular fluid using TRIzol Reagent (Takara Bio, Inc., Dalian, China) as recommended by the manufacturer. For each sample, a total of 1 μg extracted RNA was transcribed into cDNA after treatment with Prime Script RT reagent Kit with gDNA Eraser (Takara Bio, Inc., Dalian, China). The subsequent qRT-PCR analysis used SYBR Premix Ex Taq (Takara Bio, Inc., Dalian, China) and a LightCycler 480 system. There were four stages in qPCR. The first stage (initial denaturation): the reaction temperature was 95 °C for 30 s. The second stage (PCR): the reaction temperature was 95 °C for 5 s and then 60 °C for 30 s. This stage was set at 40 cycles. The third stage (melting): the reaction temperature was 95 °C for 5 s and then 65 °C for 60 s. The fourth stage (cooling): the reaction temperature was 50 °C for 30 s and then 4 °C. The normalization was undertaken to the housekeeping gene Actin, and the 2−ΔCt method was applied for MALAT1 relative expression calculation.
Forward primer sequence for Actin was TTCGAGCAAGAGATGGCCA (5′–3′), and reverse primer sequence for Actin was CGTACAGGTCTTTGCGGATG (5′–3′). Forward primer sequence for MALAT1 was AAAGCAAGGTCTCCCCACAAG, reverse primer sequence for MALAT1 was GGTCTGTGCTAGATCAAAAGGCA (5′–3′).
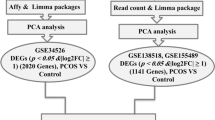
Bioinformatic prediction and integrated analysis with public database
PCOS related genes were downloaded by searching with Associated Phenotypes “PCO (polycystic ovarian syndrome)” from Ovarian Kaleidoscope Database (OKdb) (https://appliedbioinfo.com/4_search.html) (Supplementary Table S1). PCOS related miRNAs list was downloaded from Knowledgebase on Polycystic Ovary Syndrome (PCOSKB) (http://pcoskb.bicnirrh.res.in/mirna.php?page=0#) (Supplementary Table S2). MALAT1 target gene list was downloaded from LncRNA2Target (http://123.59.132.21/lncrna2target/index.jsp) (Supplementary Table S3). MALAT1 target gene list from LncSEA (https://bio.liclab.net/LncSEAv2/download.php) was downloaded and filtered in RNA binding protein class (Supplementary Table S4). MALAT1 target miRNAs list from LncSEA was downloaded and filtered in MicroRNA class (Supplementary Table S5). We compared MALAT1 target genes and target miRNAs with PCOS related genes and miRNAs separately.
Study design and statistical analyses
The threshold for defining insulin resistance is homeostasis model assessment for insulin resistance (HOMA-IR) > 2.5. The threshold for defining hyperandrogenemia is serum total testosterone (T) > 48.1 ng/dL. The threshold for defining obesity is body mass index (BMI) > 25 kg/m2.
Data was analysed using R software (version 4.2.1). Spearman was used for correlation analysis. P < 0.05 was statistically significant. Our data were presented as the mean ± standard deviation (SD). Student’s t-test was performed to analyse two different groups, whereas one-way ANOVA followed by Tukey’s test was performed for multiple comparisons. Figures were generated using ggplot2 R package (version 3.4.2).
Results
Baseline characteristics
We compared the baseline characteristics of 110 PCOS cases and 71 controls enrolled in our study in Table 1. The age range of all participants was 20–38 years old. Participants with PCOS had a significantly higher BMI compared to the control group (p < 0.001***). PCOS cases also had worse glucose and lipid metabolism profile, characterised by higher level of FPG (p < 0.001***), FINS (p < 0.001***), HOMA-IR (p < 0.001***), TC (p < 0.05*) and TG (p < 0.001***). As expected, serum LH (p < 0.001***), LH/FSH ratio (p < 0.001***), TT (p < 0.001***) and AMH (p < 0.001***) was significantly higher in PCOS patients compared to controls, but serum FSH (p < 0.01**) was lower.
MALAT1 expression in granulosa cells of controls and PCOS cases
Firstly, we extracted RNA in GCs and performed qRT-PCR to detect the expression level of MALAT1. We found a remarkable increase of MALAT1 expression in PCOS cases (p < 0.01**, Fig. 1A). To study the relationship of MALAT1 expression with other classical PCOS phenotypes, we further clarified PCOS cases into IR-PCOS and NIR-PCOS subtypes according to HOMA-IR index. We found that only IR-PCOS rather than NIR-PCOS patients showed MALAT1 expression upregulation compared to controls (p < 0.01**, Fig. 1B). Moreover, PCOS patients were divided into HA-PCOS and NHA-PCOS subgroups depending on the presence of hyperandrogenism or not. Their comparison result showed the upregulation of MALAT1 in NHA-PCOS cases compared to controls (p < 0.05*, Fig. 1C). Considering that PCOS was often associated with obesity, we also focused on the MALAT1 expression difference between controls and PCOS cases with normal weight and obesity (Obe). We noticed that the expression of MALAT1 expression in Obe-PCOS GCs was higher not only than controls (p < 0.01**, Fig. 1D), but also than PCOS with normal weight (p < 0.05*, Fig. 1D). The results of this part illustrated that abnormal metabolism, obesity and abnormal androgen were associated with MALAT1 expression in GCs.
MALAT1 expression was increased in GCs from PCOS, especially IR, NHA-PCOS and Obese subgroups. Data were normalized by Actin. (A) The relative expression of MALAT1 in PCOS cases (n = 110) and control women (n = 71). (B) The normalized expression of MALAT1 in IR-PCOS cases (n = 72), NIR-PCOS cases (n = 38) and control women (n = 71). (C) The normalized expression of MALAT1 in HA-PCOS cases (n = 31), NHA-PCOS cases (n = 79) and control women (n = 71). (D) The normalized expression of MALAT1 in PCOS cases with normal weight (n = 61), obese PCOS cases (n = 49), control women with normal weight (n = 62) and obese control women (n = 9).
Association of the MALAT1 expression with clinical characteristics
We compared correlation results of MALAT1 expression and clinical characteristics in PCOS and control groups using Spearman’s correlation. Interestingly, the correlation analysis showed that the expression of MALAT1 was remarkedly positively correlated with BMI (R = 0.25, p = 0.039*; Fig. 2A) only in controls. Constantly, there were positive correlations between the expression of MALAT1 and metabolic parameters only in controls as well, including FPG (R = 0.36, p = 0.0021*; Fig. 2B), HOMA-IR (R = 0.24, p = 0.048*; Fig. 2C) and TG (R = 0.24, p = 0.047*, Fig. 2D).
MALAT1 expression was correlated with some clinical characteristics in controls and PCOS cases. (A–H) The relationships of MALAT1 expression and BMI, FPG, HOMA-IR, TG, E2, FSH, LH and LH/FSH ratio in control group and PCOS group. Statistical analysis of the data was performed using Spearman’s test. The blue dots represented control group and the red dots represented PCOS group.
As for endocrine profiles, we observed the significant correlations between the MALAT1 expression and several important hormone indexes for PCOS. MALAT1 expression was significantly correlated with serum E2 level (R = -0.3, p = 0.0098**, Fig. 2E) and serum FSH level (R = − 0.35, p = 0.0032**, Fig. 2F) only in controls. Besides, we observed the significant positive correlations between MALAT1 expression and serum LH level (R = 0.24, p = 0.011*, Fig. 2G) and LH/FSH ratio (R = 0.28, p = 0.0034**, Fig. 2H) in PCOS group. We suggested that MALAT1 in GCs could take part in endocrine regulation in female.
Association of the MALAT1 expression with clinical characteristics in different PCOS subgroups
Next, we further detected the association of the MALAT1 expression with clinical characteristics in different PCOS subgroups. Firstly, we compared the associations amongst controls, NIR-PCOS and IR-PCOS subgroups. Results showed the significant correlations between the MALAT1 expression and serum LH/FSH ratio (R = 0.26, p = 0.03*, Fig. 3A) only in IR-PCOS group.
MALAT1 expression was correlated with LH/FSH ratio in different PCOS subgroups. (A) The relationship of MALAT1 expression and LH/FSH ratio in controls, NIR-PCOS and IR-PCOS cases. (B) The relationship of MALAT1 expression and LH/FSH ratio in controls, obese controls, PCOS and obese PCOS cases. Statistical analysis of the data was performed using Spearman’s test.
Besides, the serum LH/FSH ratio was significantly positively correlated with MALAT1 expression (R = 0.31, p = 0.014*, Fig. 3B) in PCOS women with normal weight when we detected the associations amongst controls, obese controls, PCOS and obese PCOS cases.
We then explored the associations amongst controls, NHA-PCOS and HA-PCOS subgroups. Interestingly, we found the significant positive correlations between MALAT1 expression and serum LH level (R = 0.24, p = 0.033*, Fig. 4A) and serum T level (R = 0.3, p = 0.0072**, Fig. 4B) solely in NHA-PCOS subgroup.
MALAT1 expression was correlated with some clinical characteristics in controls, NHA-PCOS and HA-PCOS cases. (A) The relationship of MALAT1 expression and serum LH level in controls, NHA-PCOS and HA-PCOS cases. (B) The relationship of MALAT1 expression and serum TT level in controls, obese controls, PCOS and obese PCOS cases. Statistical analysis of the data was performed using Spearman’s test.
Regulation network of MALAT1 by integrated analysis with public database
Aiming to explore the biological function of MALAT1 in PCOS, we integrated two critical lncRNA databases, LncSEA (http://bio.liclab.net/LncSEA/index.php) and LncRNA2Target (http://123.59.132.21/lncrna2target/index.jsp) with PCOS related Ovarian Kaleidoscope Database (OKdb) and Knowledgebase on Polycystic Ovary Syndrome (PCOSKB) databases. First of all, referring to the PCOS related genes in Ovarian Kaleidoscope Database (OKdb) and LncRNA2Target, there were 8 overlapped genes, including ABCA1, CCL2, CD36, HMGB1, MAPK1, MIR206, MIR21 and MIR429 (Fig. 5A). Moreover, when referring to PCOS related genes in OKdb and RNA binding protein term in LncSEA, there were 61 overlapped genes (Fig. 5B, left). We then enriched these genes into Reactome gene set, and found they were mainly involved in immune pathways, like Interleukin-4 and Interleukin-13 signaling, Signaling by Interleukins and Cytokine Signaling in Immune system (Fig. 5B, right).
Regulation network of MALAT1 was generated by integrated analysis with public database. (A) Overlapped genes of MALAT1 target genes in LncRNA2Target and PCOS-related genes in OKdb. (B) Overlapped genes of MALAT1 target genes in RNA binding protein term in LncSEA and PCOS-related genes in OKdb, and these genes enrichment according to Reactome gene set. (C) Overlapped miRNAs of MALAT1 target miRNAs in microRNA term in LncSEA and PCOS-related miRNAs in PCOSKB.
MALAT1 can also regulate various miRNAs expression. Combining microRNA term in LncSEA with PCOS related miRNA database PCOSKB (http://pcoskb.bicnirrh.res.in/), we observed 14 overlapped miRNAs, including MIR574, MIR132, MIR 21, MIR222, MIR25, MIR93, MIR145, MIR483, MIR16-2, MIR126, MIR592, MIR155, MIR429 and MIR638 (Fig. 5C). Altogether, our research was summarised in Fig. 6.
Discussions
As a conserved lncRNA, MALAT1 was reported to exert great impact on multiple biological processes9,17,18. However, its alteration in GCs in PCOS and its association with PCOS remained unclear yet. In the present study, we systematically evaluated MALAT1 expression level in GCs in a large cohort, and compared MALAT1 expression in different PCOS subgroups. We showed that the expression of MALAT1 was significantly higher in PCOS GCs, partly consistent with the recently published study14. In the meanwhile, MALAT1 was upregulated especially in IR-PCOS, Obe-PCOS and NHA-PCOS subgroups. We found MALAT1 gene expression was significantly positively correlated with BMI and several metabolic parameters in controls, like FPG, HOMA-IR and TG. Interestingly, MALAT1 gene expression was also remarkedly associated with a few critical endocrine indexes for PCOS, including serum E2, FSH, LH and LH/FSH ratio. Moreover, further exploration of associations in different PCOS subgroups, we found the significant positive correlation with LH/FSH ratio in IR-PCOS and PCOS with normal weight, and the significant positive correlations with serum T and LH level in NHA-PCOS subgroup. In the end, we integrated MALAT1 targets with public PCOS databases and constructed the regulation network of MALAT1. These findings partially shed light on the roles of MALAT1 during the pathophysiological process of PCOS.
Emerging evidence indicated MALAT1 expression was altered in PCOS. It was reported that MALAT1 expression was downregulated in peripheral blood from PCOS patients7,11. However, there was divergence on the alterations in PCOS patients’ GCs. Zhao et.al and Tan et.al found lower expression level of MALAT1 in GCs from PCOS patients12,13, while high-throughput sequencing and qRT-PCR results in one study published in 2022 revealed the upregulation of MALAT1 in PCOS GCs14. Moreover, upregulation of AMH, one of the characteristics of PCOS, had the capacity to increase MALAT1 expression in GCs14. PCOS cases involved in previous two studies had higher T level, but in our study PCOS cases were clarified into hyperandrogenic and non-hyperandrogenic subgroups12,13. In the meanwhile, another study revealing the MALAT1 upregulation also only included non-hyperandrogenic PCOS patients14. Consistently, in our research, we observed the absolute upregulation of MALAT1 in NHA-PCOS subgroup, and the significant positive correlation of MALAT1 expression and serum T level in NHA-PCOS patients. Besides, we also found the significant positive correlation of MALAT1 expression and serum LH level especially in NHA-PCOS patients. Altogether, these results suggested that there might be different pathophysiology involving MALAT1 in GCs in PCOS with or without hyperandrogenism.
Interestingly, in our study we detected the notable correlation between MALAT1 expression and BMI, FPG, HOMA-IR and TG, but only in controls. Besides, the increase of MALAT1 was much more obvious in IR-PCOS subgroup. The role of MALAT1 was demonstrated in some metabolic disorders, like obesity and diabetes19,20. Preliminary research on obese and normal-weight female participants found that MALAT1 expression in adipose tissue was significantly positively correlated with HOMA-IR19. Moreover, positive correlations were also found between MALAT1 gene expression and some key lipid metabolism genes, including PPARγ, PGC1, SREBP-1c, FASN, and ACC in adipose tissue19. Similarly, when referring to MALAT1 target genes and PCOS related genes, the common genes were also enriched in some lipid metabolism pathways, like PPARA activates gene expression, Regulation of lipid metabolism by PPARalpha and Metabolism of lipids. These results suggested that MALAT1 affected GCs widely in PCOS, as a complex endocrine and metabolism disorder. Except for the extensively-investigated role of MALAT1 in controlling GCs proliferation11,12,13,14, it was necessary to switch the focus onto its role on metabolism in GCs in the field of PCOS.
As for the signaling pathway affected by MALAT1 in GCs, one research showed that MALAT1 knockdown in GCs could inhibit the phosphorylation of SMAD2/3, one of the most important mediators in immune response13. Consistent with our joint analysis with external databases, MALAT1 may indeed function in GCs by regulating immunity. However, in PCOS model rats, MALAT1 expression was shown to be downregulated in ovarian tissue of PCOS rats. It was found that overexpression of MALAT1 seemed to play a protective role in reducing ovarian tissue damage and endocrine disorder in PCOS by regulating miR-302d-3p mediated leukemia inhibitory factor activity10. Although the effect of MALAT1 was controversial with our findings for its undertaken in rats, it revealed the critical role of MALAT1 in the immune regulation. Moreover, it was reported that MALAT1 contributed to the pathophysiological process of PCOS by regulating TGFβ signaling through sponging miR-125b and miR-203a13. To sum up, the contribution of MALAT1 in PCOS has been poorly studied, and the specific pathology of MALAT1 on PCOS development needs to be further explored.
Overall, the findings of this study demonstrate the differential expression of MALAT1 in GCs in PCOS, especially in IR, obese and NHA PCOS subgroups and underscore the potential role of MALAT1 in metabolism and immune response in GCs in PCOS. However, it is important to recognise the limitations of this study. The absence and unavailability of protein samples from these participants enrolled in the research prevented MALAT1 protein analysis, hindering the comprehensiveness of the study. The MALAT1 protein analysis in GCs in PCOS needs to be conducted in the future for the comprehensiveness. Moreover, more studies are needed to further investigate the role of MALAT1 in glucose and lipid metabolism and immune response in PCOS.
To summarise, we have investigated that the MALAT1 expression in GCs of PCOS patients was notably increased, and the increase was much more significant in the NHA-PCOS, IR-PCOS and obe-PCOS subgroups, indicating that the MALAT1-mediated action might take vital roles for the steroid metabolism, IR and metabolism of PCOS in GCs. Regulation network generated by integrating external resource revealed MALAT1’s potential but important role on lipid metabolism and immune response in GCs in PCOS. This study gave a theorical basis for MALAT1’s role in understanding the underlying mechanism of PCOS.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MALAT1:
-
Metastasis-associated lung adenocarcinoma transcript 1
- PCOS:
-
Polycystic ovary syndrome
- lncRNAs:
-
Long noncoding RNAs
- GCs:
-
Granulosa cells
- hCG:
-
Human chorionic gonadotropin
- PCR:
-
Polymerase chain reaction
- IR:
-
Insulin resistant
- HA:
-
Hyperandrogenic
- NHA:
-
Non-hyperandrogenic
- BMI:
-
Body mass index
- FPG:
-
Fasting plasma glucose
- FINS:
-
Fasting insulin
- HOMA-IR:
-
Homeostasis model assessment for insulin resistance
- TC:
-
Total cholesterol
- TG:
-
Total glycerol
- FSH:
-
Follicle stimulating hormone
- LH:
-
Luteinizing hormone
- E2:
-
Estradiol
- TT:
-
Total testosterone
- AMH:
-
Anti-Müllerian hormone
- OKdb:
-
Ovarian Kaleidoscope Database
- PCOSKB:
-
Knowledgebase on Polycystic Ovary Syndrome
- SMAD:
-
Small mother against decapentaplegic
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- PGC1:
-
Peroxisome proliferator-activated receptor gamma coactivator 1 alpha
- FASN:
-
Fatty acid synthase
- ACC:
-
Acetyl-CoA carboxylase alpha
References
Joham, A. E. et al. Polycystic ovary syndrome. Lancet Diabetes Endocrinol. 10, 668–680. https://doi.org/10.1016/S2213-8587(22)00163-2 (2022).
Yang, H., Pawitan, Y., Fang, F., Czene, K. & Ye, W. Biomarkers and disease trajectories influencing women’s health: Results from the UK biobank cohort. Phenomics 2, 184–193. https://doi.org/10.1007/s43657-022-00054-1 (2022).
Escobar-Morreale, H. F. Polycystic ovary syndrome: Definition, aetiology, diagnosis and treatment. Nat. Rev. Endocrinol. 14, 270–284. https://doi.org/10.1038/nrendo.2018.24 (2018).
Fan, H. Y. et al. MAPK3/1 (ERK1/2) in ovarian granulosa cells are essential for female fertility. Science 324, 938–941. https://doi.org/10.1126/science.1171396 (2009).
Wen, L. et al. Recent advances in mammalian reproductive biology. Sci. China Life Sci. 63, 18–58. https://doi.org/10.1007/s11427-019-1572-7 (2020).
Belani, M. et al. Differential insulin and steroidogenic signaling in insulin resistant and non-insulin resistant human luteinized granulosa cells-A study in PCOS patients. J. Steroid Biochem. Mol. Biol. 178, 283–292. https://doi.org/10.1016/j.jsbmb.2018.01.008 (2018).
Butler, A. E. et al. Alterations in long noncoding RNAs in women with and without polycystic ovarian syndrome. Clin. Endocrinol. 91, 793–797. https://doi.org/10.1111/cen.14087 (2019).
Zhao, K. et al. lncRNA HITT inhibits lactate production by repressing PKM2 oligomerization to reduce tumor growth and macrophage polarization. Research https://doi.org/10.34133/2022/9854904 (2022).
Goyal, B. et al. Diagnostic, prognostic, and therapeutic significance of long non-coding RNA MALAT1 in cancer. Biochim. Biophys. Acta Rev. Cancer 1875, 188502. https://doi.org/10.1016/j.bbcan.2021.188502 (2021).
Chen, Y., Chen, Y., Cui, X., He, Q. & Li, H. Down-regulation of MALAT1 aggravates polycystic ovary syndrome by regulating MiR-302d-3p-mediated leukemia inhibitory factor activity. Life Sci. 277, 119076. https://doi.org/10.1016/j.lfs.2021.119076 (2021).
ElMonier, A. A. et al. LncRNA NEAT1 and MALAT1 are involved in polycystic ovary syndrome pathogenesis by functioning as competing endogenous RNAs to control the expression of PCOS-related target genes. Noncoding RNA Res. 8, 263–271. https://doi.org/10.1016/j.ncrna.2023.02.008 (2023).
Li, Y., Xiang, Y., Song, Y., Zhang, D. & Tan, L. MALAT1 downregulation is associated with polycystic ovary syndrome via binding with MDM2 and repressing P53 degradation. Mol. Cell Endocrinol. 543, 111528. https://doi.org/10.1016/j.mce.2021.111528 (2022).
Zhang, D., Tang, H. Y., Tan, L. & Zhao, D. M. MALAT1 is involved in the pathophysiological process of PCOS by modulating TGFbeta signaling in granulosa cells. Mol. Cell Endocrinol. 499, 110589. https://doi.org/10.1016/j.mce.2019.110589 (2020).
Tu, M. et al. Effect of lncRNA MALAT1 on the granulosa cell proliferation and pregnancy outcome in patients with PCOS. Front. Endocrinol. 13, 825431. https://doi.org/10.3389/fendo.2022.825431 (2022).
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 81, 19–25. https://doi.org/10.1016/j.fertnstert.2003.10.004 (2004).
Li, M. et al. The HMGA2-IMP2 pathway promotes granulosa cell proliferation in polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 104, 1049–1059. https://doi.org/10.1210/jc.2018-00544 (2019).
Chen, Y. et al. The lncRNA Malat1 regulates microvascular function after myocardial infarction in mice via miR-26b-5p/Mfn1 axis-mediated mitochondrial dynamics. Redox Biol. 41, 101910. https://doi.org/10.1016/j.redox.2021.101910 (2021).
Xu, W. W., Jin, J., Wu, X. Y., Ren, Q. L. & Farzaneh, M. MALAT1-related signaling pathways in colorectal cancer. Cancer Cell Int. 22, 126. https://doi.org/10.1186/s12935-022-02540-y (2022).
Ebrahimi, R. et al. Adipose tissue gene expression of long non-coding RNAs; MALAT1, TUG1 in obesity: Is it associated with metabolic profile and lipid homeostasis-related genes expression?. Diabetol. Metab. Syndr. 12, 36. https://doi.org/10.1186/s13098-020-00544-0 (2020).
Chang, W. W. et al. Association of tag single nucleotide polymorphisms (SNPs) at lncRNA MALAT1 with type 2 diabetes mellitus susceptibility in the Chinese Han population: A case-control study. Gene 851, 147008. https://doi.org/10.1016/j.gene.2022.147008 (2023).
Acknowledgements
The authors would also like to thank every member in the Center for Reproductive Medicine, Shandong University for their kind help in granulosa cells samples collection and thank all the participants who agreed to take part in this study. This work was supported by the National Key Research and Development Program of China (2021YFC2700400), the Basic Science Center Program of NSFC (31988101), the National Natural Science Foundation of China (32370916, 82101707, and 82071606), the Natural Science Foundation of Shandong Province for Excellent Youth Scholars (ZR2023YQ061), CAMS Innovation Fund for Medical Sciences (2021-I2M-5–001), Shandong Provincial Key Research and Development Program (2020ZLYS02), the Program for Chang Jiang Scholars (Q2022144), the Taishan Scholars Program of Shandong Province (ts20190988), and the Fundamental Research Funds of Shandong University (2023QNTD004).
Author information
Authors and Affiliations
Contributions
Z.-J.C. designed the study. S.L. and X.G. wrote the main manuscript text and S.Z. modified it. Y.L., X.Y., Z.Y. and Y.W. helped collect patients samples and isolate granulosa cells.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, S., Li, Y., Yan, X. et al. MALAT1 expression in granulosa cells in PCOS patients with different phenotypes. Sci Rep 14, 5019 (2024). https://doi.org/10.1038/s41598-024-55760-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55760-9
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.