Abstract
Emergent surgery is a common approach for incarcerated obturator hernias, with high morbidity and mortality rates. Moreover, there have been reports of elective surgery cases after noninvasive manual reduction. For a decade, the initial approach in our institution is also manual reduction unless bowel viability is poor. This study aimed to clarify the efficacy and safety of manual reduction followed by elective surgery. We retrospectively reviewed 50 cases of incarcerated obturator hernia from 2010 to 2022 at Iwate Prefectural Iwai Hospital. Manual reduction was attempted in 31 (62%) patients. The reduction was successful in 21 (42%) patients, and most of them received mesh repair using the extraperitoneal approach as elective surgery. However, two patients underwent emergent surgery in the waiting period because of late-onset constriction and a small bowel perforation. Patients with irreducible hernia underwent emergent surgery, except for two patients who received the best supportive care. Postoperative complications were observed in 5% and 22% of reducible and irreducible cases, respectively. Postoperative mortality was zero in both groups. Manual reduction is useful in some cases, but careful observation is needed because late-onset constriction and perforation could occur.
Similar content being viewed by others
Introduction
Obturator hernias (OH) are relatively rare, accounting for 0.07–1% of all hernias1. OH occur more frequently in older and slender women1. Emergent surgery is a common approach for incarcerated OH, and its morbidity and mortality rates are high because of advanced patient age and serious comorbidities2. Moreover, there have been reports of elective surgery after noninvasive manual reduction3,4,5. However, the efficacy and safety of manual reduction are still unclear5. For a decade, the initial approach in our institution is also manual reduction unless bowel viability is poor. In this study, we retrospectively reviewed our cases and examined the validity of our approach.
Methods
This study analyzed 50 patients with incarcerated OH from 2010 to 2022 at Iwate Prefectural Iwai Hospital. All patients were diagnosed with incarcerated OH using computed tomography (CT) scans. We retrospectively reviewed patient characteristics, therapeutic approach, and operative outcomes. Postoperative complications were defined as adverse events occurring within 30 days of surgery or during hospitalization, and severity was assessed using the Clavien–Dindo (C–D) classification (grades I–V)6.
The study protocol was approved by our institution's ethics committee or institutional review board (Accession no. Iwai Hospital 2022–1077). Informed consent was obtained from all study participants.
Manual reduction maneuver
The patient was positioned supine with the leg in abduction, flexion, and lateral rotation (Fig. 1). The surgeon visually recognized the incarcerated OH at the anterior side of the adductor longus muscle with ultrasound (Fig. 2). Subsequently, manual reduction was performed by compressing the posterior side of the adductor longus muscle and lateral side of the labium majora manually, until the hypoechoic mass disappeared. If the incarcerated hernia is not released promptly, the assistant bends and stretches the patient’s leg repeatedly3,4,7. After the maneuver, the patient underwent a CT scan to confirm the release of the hernia and the absence of perforation (Fig. 3).
Manual reduction maneuver. The patient is supine with the leg in abduction, flexion, and lateral rotation. The surgeon detected the incarcerated obturator hernia at the anterior side of the adductor longus muscle via ultrasound (US). Manual reduction was performed by compressing the posterior side of the adductor longus muscle and the lateral side of the labium majora.
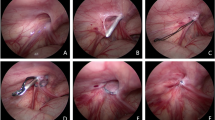
Surgical procedure
If manual reduction was successful, the suprapubic midline extraperitoneal approach was employed as elective surgery8. A 4–6-cm suprapubic vertical incision was made, the space of Retzius was dissected, and the obturator hernia was inverted in direct view. In three extraperitoneal approach cases, the process was visualized laparoscopically (Fig. 4). Conversely, a lower midline laparotomy was employed as emergent surgery.
Statistical analysis
All statistical analyses were performed using JMP Pro version 15 with Student’s t test and Fisher’s exact test. P < 0.05 denoted statistical significance.
Ethical approval and Informed consent
All procedures performed in this study involving human participants were in accordance with the ethical standards of our institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all study participants.
Results
The patient characteristics are summarized in Table 1. The mean age was 84.8 years. There were 48 female patients and two male patients. The mean interval from symptom onset to hospital admission was 64.9 h. There were 13 American Society of Anesthesiologists physical status (ASA-PS), 2 cases (26%), 33 ASA-PS 3 cases (66%), and 4 ASA-PS 4 cases (8%). Consequently, ASA-PS 4 cases avoided surgery. The overall postoperative morbidity (C–D grade II or higher) rate was 15%: ileus in 11% of the cases, pneumonia in 7%, and tachycardia in 2% (Table 2). Perioperative mortality was zero.
A flowchart of patients is shown in Fig. 5. Manual reduction was attempted in 31 patients. The reduction was successful in 21 patients, of which two selected watchful waiting because of chronic pulmonary insufficiency. The two watchful waiting cases did not involve hernia recurrence, late-onset necrosis, or perforation. One died from acute exacerbation of interstitial lung disease 2 years later, and another died from bacterial pneumonia on hospital day 31. Of the 21 patients, 19 selected elective surgery, but two patients underwent emergent surgery in the waiting period because of late-onset constriction and a small bowel perforation. Manual reduction failed in 10 patients, and 8 underwent emergent surgery. Two patients received the best supportive care because of poor general condition, and they, unfortunately, died the next day. The remaining 19 patients underwent emergent surgery because of suspicions of poor bowel viability.
Patient flowchart. Manual reduction was attempted in 31 patients. Reduction was successful in 21 patients, two selected watchful waiting, and 19 selected elective surgeries, but two patients underwent emergent surgery in the waiting period. In 10 patients, manual reduction failed, 8 received emergent surgery, and two received the best supportive care. The remaining 19 patients underwent immediate emergent surgery.
We divided the patients who underwent manual reduction into two groups: manually reducible and irreducible (Table 3). No significant difference was detected in age, sex, hernia localization, ASA-PS, and laboratory findings between the two groups. The average time from the onset was 39.8 h in the reducible group compared with 73.7 h in the irreducible group (P = 0.13).
We also divided the patients who underwent surgery into manually reducible and irreducible groups (Table 4). The time from arrival at the hospital to surgery was 27 days in the reducible group. In the reducible and irreducible groups, postoperative complications were observed in 5% and 22% of the cases, respectively (P = 0.21). Bowel resection was significantly less common in the group that underwent surgery after reduction (P = 0.04), whereas mesh repair was significantly common (P < 0.001). The group that underwent surgery after reduction included two patients whose elective surgery failed because of constriction and small bowel perforation (Fig. 5).
Discussion
Our results demonstrated that 21 of 50 (42%) cases of incarcerated OH were reducible at the first visit. When it was reducible, mesh repair was often performed as elective surgery. Although significance was not reached, the complication rate tended to be low in the group that underwent surgery after reduction. A previous report preferred mesh repair to prevent recurrence if there are no contraindications9. Moreover, some case reports have suggested that elective surgery after manual reduction is favorable because the surgery can be performed in a favorable condition3,5.
These findings suggest the validity of our therapeutic approach, but late-onset constriction and perforation occurred in two patients and needed emergent laparotomy. In inguinal and femoral hernia guidelines, a medical history, systemic inflammatory response syndrome, contrast-enhanced CT findings, lactate, serum creatinine phosphokinase, and D-dimer levels predict bowel strangulation10. For example, the time from the onset of ≥ 24 h and lactate level of ≥ 2.0 mmol/L were suggested to be useful predictors of non-viable bowel strangulation10. However, a consensus was not established for indications of manual reduction of incarcerated OH5. Previous reports have suggested that the criteria for incarcerated OH were less likely to be severe than those for incarcerated inguinal hernias because OH often contains part of the small bowel circumference as a Richter-type hernia5,11. In our cases, the mean time from the onset of reducible cases was 40 h, which could be fatal in inguinal hernia11. Further investigation is needed to indicate a manual reduction, and careful long-term observation after the manual reduction is needed to make the procedure feasible3.
This study has some limitations. First, whether attempting manual reduction or not was based mainly on the surgeon’s discretion. Second, the waiting times for elective surgery were inconsistent.
Conclusion
Manual reduction followed by elective surgery could be an option for incarcerated OH; however, careful observation after reduction is needed because late-onset constriction and perforation could occur.
Data availability
The datasets analyzed during the current study are available from the corresponding author.
References
Schizas, D. et al. Obturator hernias: A systematic review of the literature. Hernia 25, 193–204. https://doi.org/10.1007/s10029-020-02282-8 (2021).
Chan, K. V., Chan, C. K. O., Yau, K. W. & Cheung, M. T. Surgical morbidity and mortality in obturator hernia: A 10-years retrospective risk factor evaluation. Hernia 18, 387–392. https://doi.org/10.1007/s10029-013-1169-5 (2014).
Tanaka, N., Kikuchi, J. & Ando, T. Elective plug repair of an incarcerated obturator hernia by the thigh approach after noninvasive manual reduction: Report of two cases. Surg. Today 40, 181–184 (2010).
Shigemitsu, Y. et al. The maneuver to release an incarcerated obturator hernia. Hernia 16, 715–717 (2012).
Kawanaka, H. et al. Therapeutic strategy for incarcerated obturator hernia using preoperative manual reduction and laparoscopic repair. Am. Coll. Surg. 226, 891–901 (2018).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240, 205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae (2004).
Kamihata, K. et al. A new repositioning maneuver for incarcerated obturator hernia. Jpn. J. Gastroenterol. Surg. 55, 1–9. https://doi.org/10.5833/jjgs.2020.0169 (2022).
Gray, S. W., Skandalakis, J. E., Soria, R. E. & Rowe, J. S. Jr. Strangulated obturator hernia. Surgery 75, 20–27. https://doi.org/10.5555/uri:pii:0039606074901743 (1974).
Karasaki, T., Nomura, Y. & Tanaka, N. Long-term outcomes after obturator hernia repair: retrospective analysis of 80 operations at a single institution. Hernia 8, 393–397. https://doi.org/10.1007/s10029-013-1159-7 (2014).
Birindelli, A. et al. 2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J. Emerg. Surg. 12, 37. https://doi.org/10.1186/s13017-017-0149-y (2017).
Stamatiou, D., Skandalakis, L. J., Zoras, O. & Mirilas, P. Obturator hernia revisited: surgical anatomy, embryology, diagnosis, and technique of repair. Am. Surg. 77, 1147–1157. https://doi.org/10.1177/000313481107700926 (2011).
Acknowledgements
We thank Enago (www.enago.jp) for the English language review. We would like to acknowledge Dr. Takayuki Ishida for technical support.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Y.G. and Y.O. The first draft of the manuscript was written by Y.G., and all authors commented on the previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gokon, Y., Ohki, Y., Ogino, T. et al. Manual reduction for incarcerated obturator hernia. Sci Rep 13, 5504 (2023). https://doi.org/10.1038/s41598-023-31634-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31634-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.