Abstract
Advanced systemic mastocytosis (AdvSM) is a rare, KIT D816V-driven hematologic neoplasm characterized by mast cell infiltration and shortened survival. We report the results of a prespecified interim analysis of an ongoing pivotal single-arm phase 2 trial (no. NCT03580655) of avapritinib, a potent, selective KIT D816V inhibitor administered primarily at a once-daily starting dose of 200 mg in patients with AdvSM (n = 62). The primary endpoint was overall response rate (ORR). Secondary endpoints included mean baseline change in AdvSM–Symptom Assessment Form Total Symptom Score and quality of life, time to response, duration of response, progression-free survival, overall survival, changes in measures of disease burden and safety. The primary endpoint was successfully met (P = 1.6 × 10-9), with an ORR of 75% (95% confidence interval 57–89) in 32 response-evaluable patients with AdvSM who had sufficient follow-up for response assessment, including 19% with complete remission with full or partial hematologic recovery. Reductions of ≥50% from baseline in serum tryptase (93%), bone marrow mast cells (88%) and KIT D816V variant allele fraction (60%) were observed. The most frequent grade ≥3 adverse events were neutropenia (24%), thrombocytopenia (16%) and anemia (16%). Avapritinib demonstrated a high rate of clinical, morphological and molecular responses and was generally well tolerated in patients with AdvSM.
Similar content being viewed by others
Main
Systemic mastocytosis (SM) is a rare hematologic neoplasm that is associated with the KIT D816V mutation in ~95% of cases. The KIT D816V mutation drives the increased proliferation and accumulation of neoplastic mast cells, leading to severe, debilitating and often unpredictable symptoms and poor quality of life (QoL)1,2,3. In AdvSM, mast cell infiltration leads to organ damage, referred to as ‘C-findings’ (that is, cytopenias or liver dysfunction), with limited treatment options and poor survival2,4,5,6. AdvSM is comprised of three subtypes: aggressive SM (ASM), SM with an associated hematologic neoplasm (SM-AHN) and mast cell leukemia (MCL)2. In SM-AHN, which represents 60–70% of cases of AdvSM7,8, patients concurrently have both SM and another World Health Organization-defined hematologic neoplasm, usually myeloid (for example, myelodysplastic syndrome, myeloproliferative neoplasm or an overlap)9. The KIT D816V mutation is frequently also present in cells comprising the AHN component9. Molecular subtyping of patients with AdvSM often reveals a heterogenous genetic landscape, with high-risk mutations in splicing factors, epigenetic regulators and transcription factors such as SRSF2, ASXL1 and RUNX1, respectively10,11,12. Treatment options are very limited, with only the multikinase inhibitor midostaurin and, more recently, the selective KIT kinase inhibitor avapritinib approved for the treatment of AdvSM.
Avapritinib is a selective KIT and platelet-derived growth factor receptor-alpha (PDGFRA) kinase inhibitor with high potency for the KIT D816V and homologous PDGFRA-mutant proteins1. As detailed in the accompanying report13, avapritinib was investigated in patients with AdvSM in the phase 1 EXPLORER trial (no. NCT02561988)14. In this trial, avapritinib exhibited an ORR of 75% by modified (m)IWG–MRT–ECNM (International Working Group–Myeloproliferative Neoplasms Research and Treatment and European Competence Network) criteria, including 36% with complete remission with full (CR) or partial hematologic recovery (CRh), with a median follow-up of 23 months. Responses were seen at all starting doses (30–400 mg once daily (QD)) and deepened over subsequent cycles, but occurred most rapidly at 200 mg QD and higher. Patients experienced profound reductions in objective measures of mast cell burden, including complete molecular remission of KIT D816V, reversion of mast-cell-related organ damage and improvements in symptoms. Review of safety, rapid reduction of disease burden and response rate led to selection of 200 mg as the optimal dose for patients with AdvSM.
Here, we present the results of a prespecified interim analysis from the PATHFINDER trial15, an ongoing, international, multicenter, open-label, single-arm, phase 2 registrational trial (no. NCT03580655) of avapritinib 200 mg QD in adult patients with a centrally confirmed diagnosis of AdvSM. Patients were enrolled into cohort 1 (efficacy evaluable) if they had an evaluable mIWG–MRT–ECNM C-finding (that is, cytopenias, liver function abnormalities, splenomegaly, ascites, pleural effusion) (Supplementary Table 1) at baseline, or MCL irrespective of the presence of C-findings. The primary endpoint of the trial was ORR, including CR/CRh, partial remission (PR) and clinical improvement (CI), as per mIWG–MRT–ECNM criteria (Supplementary Table 2), which was tested against 28%, the ORR of midostaurin, as per IWG–MRT–ECNM criteria16. A prespecified interim analysis was performed when 32 patients in cohort 1 had sufficient follow-up for response evaluation (interim analysis efficacy population). In addition, cohort 2 included patients without an evaluable C-finding at baseline (that is, evaluable C-findings that resolved with previous therapy or nonevaluable C-findings such as weight loss or large osteolytic lesions) and were therefore not evaluable for response. All enrolled patients (safety population) were included in secondary endpoints, which included changes in patient symptoms, reduction in measures of disease burden and safety.
Results
Participants
Between 21 November 2018 and 23 June 2020, 62 patients with prospectively centrally adjudicated AdvSM were enrolled (ASM (n = 9), SM-AHN (n = 43) and MCL (n = 10)) and received avapritinib primarily at a starting dose of 200 mg QD (n = 60; two patients started at 100 mg QD), across cohort 1 (n = 52) and cohort 2 (n = 10) (Extended Data Fig. 1). Avapritinib was administered continuously in 28-day cycles until progression, intolerance, withdrawal by the investigator or patient or death.
The interim analysis was triggered when 32 response-evaluable patients in cohort 1 achieved sufficient follow-up for confirmed evaluation of response. The median age was 68 years (range, 37–85) and 56% of patients were male (Table 1). By central assessment, 94% were positive for the KIT D816V mutation and 53% carried an additional mutation in at least one of the genes SRSF2, ASXL1 or RUNX1 (S/A/R), which is associated with poor survival in SM12. The majority of patients (72%) had received previous antineoplastic therapy, including 53% with midostaurin (Extended Data Fig. 2). Baseline median bone marrow mast cell percentage was 50% (range, 10–95) and median serum tryptase was 293 ng ml–1 (range, 24–1,600). The median KIT D816V variant allele fraction (VAF) in peripheral blood (which rarely has circulating mast cells) was 15% (range, 0–45). Median spleen volume was 939 ml (range, 150–2,270). Baseline characteristics were generally balanced between the safety population and those included versus not included in the interim analysis efficacy population (Extended Data Fig. 3). In the interim analysis efficacy population, the most common baseline eligible mIWG–MRT–ECNM C-findings (Supplementary Table 1) were splenomegaly (44%), elevated alkaline phosphatase (41%) and transfusion-independent anemia (41%) (Extended Data Fig. 4).
Interim analysis of efficacy
Among 32 patients in the interim analysis efficacy population (median follow-up of 10.4 months), the confirmed ORR (CR/CRh/PR/CI; primary endpoint) was 75% (n = 24, 95% confidence interval, 57–89, P = 1.6 × 10-9), with six patients (19%) achieving CRh. Ten patients (31%) achieved PR and eight (25%) had CI (Table 2). Responses were observed in all AdvSM subtypes, regardless of exposure to previous therapy (Table 2). Additionally, ORR was similar among patients with (71% (95% confidence interval, 44–90), 12/17) and without (80% (95% confidence interval, 52–96), 12/15) baseline S/A/R mutations. Responses were rapid, with a median time to response of 2 months (range, 0.3–12.2). Responses continued to improve over time (Fig. 1), with a median time to CRh of 5.6 months (range, 1.8–6.1).
In the safety population (n = 62), consistent and profound reductions in measures of mast cell burden (secondary endpoint) were observed in all enrolled patients with baseline and postbaseline assessments. A reduction of ≥50% in bone marrow mast cells was observed in 88% (44/50) of patients, and 60% (30/50) had elimination of bone marrow mast cell aggregates (Fig. 2a). The serum tryptase level decreased by ≥50% in 93% (54/58) of patients, and 43% (25/58) of patients achieved serum tryptase levels <20 ng ml–1 (Fig. 2b).
Profound reductions in disease activity beyond mast cells were also observed, with a decrease of ≥50% in absolute monocyte counts in 80% (16/20) of patients with SM and chronic myelomonocytic leukemia (SM-CMML), and a decrease of ≥50% in absolute eosinophil counts in 88% (14/16) of patients with eosinophilia, including all three patients with SM and chronic eosinophilic leukemia (SM-CEL) (Extended Data Fig. 5). Consistent with efficacy against KIT D816V mutant-bearing cells, there was a substantial (≥50%) reduction in KIT D816V VAF in the peripheral blood in 60% (33/55) of patients; 35% (19/55) of patients achieved a VAF of <1% (Fig. 2c). Spleen volume, which may be greatly enlarged due to involvement by both neoplastic mast cells and AHN, was reduced from baseline by ≥35% in 66% (31/47) of patients (Fig. 2d).
The majority of mIWG–MRT–ECNM C-findings in patients in the interim analysis efficacy population resolved from baseline, including 83% of pleural effusions, 79% of splenomegaly and 57% of ascites (Extended Data Fig. 4). Resolution of cytopenia was less frequent, despite elimination of bone marrow mast cell aggregates in the majority of patients, consistent with additional etiologies for cytopenia, such as persistent AHN and/or avapritinib-related myelosuppression.
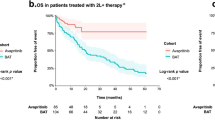
Median progression-free survival (PFS) in the interim analysis efficacy population and median overall survival (OS) in the safety population (secondary endpoints) had not been reached at the time of data cutoff. The estimated 6-, 9- and 12-month PFS rates were 91, 87 and 79%, respectively; corresponding OS rates were 94, 86 and 86%.
Safety
As of the data cutoff, 52 (84%) of 62 patients were still on treatment with a median follow-up of 7.0 months (range 5.6–8.1). Reasons for treatment discontinuation included adverse events (AEs) in six patients (with three considered treatment-related according to the local site investigator (decreased weight, subdural hematoma and bleeding propensity with subcutaneous hematoma)), disease progression as per the investigator in three patients (with one transformation to acute myeloid leukemia and two with worsening AHN) and consent withdrawal in one patient (Extended Data Fig. 1).
The most frequent AEs are presented in Table 3. The most frequent nonhematologic AEs (any grade; grade ≥3) were peripheral edema (50%; 3%), periorbital edema (48%; 3%), diarrhea (23%; 2%), nausea (18%; 2%) and vomiting (18%; 2%). The most frequent hematologic AEs (any grade; grade ≥3) were thrombocytopenia (45%; 16%), anemia (32%; 16%) and neutropenia (24%; 24%), although grade 4 neutropenia (absolute neutrophil count <0.5 × 109 l–1) was uncommon, at 8%. Grade ≥3 treatment-related AEs were reported in 32 (52%) patients, the most frequent of which were neutropenia (23%) and thrombocytopenia (15%). There were three (5%) deaths due to AEs (disease progression, necrotizing fasciitis and hemorrhagic shock), none of which were considered related to treatment. Cognitive effects (confusional state, memory impairment and cognitive disorder) occurred in seven (11%) patients (Table 3) and were primarily grade 1 (n = 6), with one grade 2.
There was one (1.6%) intracranial bleeding (ICB) event (subdural hemorrhage), in a patient with severe thrombocytopenia at baseline (platelets, 49 × 109 l–1) who was enrolled before the exclusion (below) of such patients. The patient was treated with avapritinib despite worsening thrombocytopenia (platelets, 33 × 109 l–1) and developed a grade 2 subdural hematoma 2 days after a single dose of enoxaparin. The patient was not taking antiplatelet agents and had a relatively normal international normalized ratio and activated partial thromboplastin time of 1.2 and 28.1 s, respectively, before the ICB event. The patient subsequently recovered from the event and was retreated with avapritinib due to continuing benefit. However, the patient subsequently developed a grade 4 subdural hematoma despite platelets being 167 × 109 l–1, leading to treatment discontinuation.
Safety analysis of this event and similar ICB events in the concurrent phase 1 trial identified patients with baseline severe thrombocytopenia at substantially increased risk of ICB; therefore, patients with platelets <50 × 109 l–1 at baseline were subsequently excluded from enrollment in both studies. In addition, the studies were amended to include increased platelet count monitoring, updated dose guidance for interruption, support for severely low platelet counts and treatment discontinuation for any grade of ICB events.
In total, six patients (10%) experienced AEs leading to permanent treatment discontinuation. Two (5%) patients discontinued due to a treatment-related serious AE (subdural hematoma and bleeding propensity with subcutaneous hematoma). Dose interruptions due to AEs occurred in 34 (55%) patients, most commonly due to neutropenia (21%) and thrombocytopenia (16%) (Extended Data Fig. 6). AEs led to dose reductions in 42 (68%) patients, most commonly due to neutropenia (19%) and thrombocytopenia (18%). The median time to dose reduction was 7.4 weeks, and most patients were taking a daily dose of 100 mg after cycle 3. The median daily dose was 138 mg (range, 38–240), consistent between patients with or without before exposure to therapy or midostaurin.
Patient-reported outcomes and QoL
Patients’ baseline QoL was negatively impacted by their disease, with a pretreatment mean European Organization for Research and Treatment of Cancer Core QoL Questionnaire C30 (EORTC–QLQ–C30–QoL) score of only 37.8 (range, 0–100, where 0 represents the lowest QoL and 100 the highest) and a high proportion of patients (31%) with a poor Eastern Cooperative Oncology Group (ECOG) performance status of 2 or 3. Mean and median Patient Global impression of Symptom Severity (PGIS) scores were 2.6 and 3.0, respectively (where 0 represents no symptoms and 4 very severe symptoms). The AdvSM–Symptom Assessment Form (SAF), an AdvSM-specific patient reported outcomes tool, showed that fatigue, abdominal pain and spots were the most severe symptoms, with a mean total symptom score (TSS) of 18.3, which was the sum of eight possible common symptoms (each scored 0–10, where 0 represents no symptoms and 10 is the worst imaginable). At baseline, patients had frequent supportive care medication use, including H1 antihistamines (58%), H2 antihistamines (39%) and corticosteroids (32%). Patients on corticosteroids remained evaluable if their dose did not exceed 20 mg d–1 of prednisone or equivalent.
Patient-reported symptoms, as measured by TSS score, improved rapidly following treatment initiation, dropping by 7.1 points from baseline at cycle 3 (n = 51) and by 9.8 points from baseline at treatment cycle 11 (n = 22; P < 0.001) (secondary endpoint; Fig. 3a). Mean symptom scores were lower than baseline at cycles 3 and 11 for all SM symptoms, including fatigue, abdominal pain, spots, itching, flushing, nausea, diarrhea and vomiting. Mean and median PGIS scores improved to 1.6 and 2.0 (moderate symptoms that are difficult to ignore), respectively, by cycle 3 and to 1.2 and 1.0 (minimal symptoms that are easy to ignore), respectively, by cycle 11 (secondary endpoint).
Quality of life, as assessed by EORTC–QLQ–C30, improved on trial with noteworthy improvements in physical (strenuous activity), role (work or household jobs), emotional (irritability, feeling tense and depression), cognitive (memory and concentration) and social (family life and social activities) functioning domains (secondary endpoint; Fig. 3b).
Discussion
This prespecified interim analysis of the phase 2 PATHFINDER trial demonstrated that avapritinib at a starting dose of 200 mg QD exhibited clinical benefit in patients with AdvSM, confirming findings from the phase 1 EXPLORER trial. In total, 75% of patients achieved a response regardless of AdvSM subtype, previous therapy or adverse S/A/R comutations, with a rapid median time to response of 2 months. With median follow-up of 10.4 months, 19% of patients had normalized all baseline evaluable C-findings, eliminated mast cell aggregates and reduced tryptase to <20 ng ml–1, to achieve CRh. In June 2021, data from this and the phase 1 EXPLORER trial (no. NCT02561988) formed the basis of approval by the United States Food and Drug Administration for the treatment of adults with AdvSM at a recommended starting dose of 200 mg orally QD.
Consistent and profound reductions in mast cell burden (bone marrow mast cells, serum tryptase) and normalization of SM-related organ damage (that is, liver function abnormalities, ascites, spleen size) were observed in patients across all AdvSM subtypes regardless of previous therapy. Although improvements in cytopenias were seen in some patients, including improvement of transfusion-dependent anemia in one patient, cytopenias were less likely to normalize than other C-findings, even in patients who no longer had bone marrow mast cell aggregates. This implies that persistent cytopenias were related to non-mast cell causes, such as drug effect and/or the remaining AHN component.
In addition, avapritinib demonstrated evidence of broader disease activity in patients with SM-AHN, which comprises the majority of AdvSM variants. For example, substantial reductions of monocytosis in 80% of patients with SM-CMML and eosinophilia in 88% patients with baseline eosinophilia or SM-CEL were observed. Overall, 60% of patients had substantial reductions in peripheral blood KIT D816V VAF, consistent with broad activity against both KIT D816V-positive mast cells (which rarely circulate in the blood) and cells derived from the AHN which often harbor KIT D816V, reflecting multilineage involvement of the mutation. Some patients with SM-AHN may need AHN therapy in combination or in sequence with a KIT-inhibitor-based regimen to address the genetic and biologic heterogeneity which underpins this AdvSM subtype. However, most patients had improvement in their AHN with avapritinib alone. This activity supports exploration of avapritinib in other KIT D816V-positive hematologic malignancies.
Patients had marked impairments in QoL at baseline due to their AdvSM symptoms yet reported rapid, durable and substantial reductions from baseline in every AdvSM symptom assessed, and improvements in QoL and functional impairment. Median global symptom severity as measured by PGIS had improved from severe to minimal by cycle 11.
Avapritinib was generally well tolerated, with few discontinuations due to AEs. Overall, the safety profile at the starting dose of 200 mg QD in the PATHFINDER trial included mostly low-grade fluid retention and gastrointestinal symptoms as the most common nonhematologic AEs. Cytopenias were the most common grade ≥3 AEs and reason for dose reduction, most commonly in patients with baseline cytopenias, and 100 mg was the median daily dose after cycle 3. Cognitive effects, which are dose-related, were relatively uncommon at a starting dose of 200 mg.
The incidence of ICB was low (1.6%), and similar to that observed with avapritinib in patients with GIST17,18, probably due to mitigation steps for severe thrombocytopenia which were implemented early in enrollment. These included exclusion of patients with platelets <50 × 109 l–1, closer monitoring of platelet counts, stricter dose modification guidelines and use of platelet transfusions and growth factors to maintain platelet count to ≥50 × 109 l–1. Dose-related, low-grade cognitive events were observed but did not result in substantial dose reductions. The optimal starting dose of 200 mg QD was confirmed in the current trial, because preliminary data generated in the EXPLORER trial suggested that this dose maintained efficacy while improving tolerability.
These data reinforce KIT D816V as a clinically validated drug target in AdvSM. While the multikinase inhibitor midostaurin is already approved for use in patients with AdvSM, there remains a substantial need for improvement in the overall rate, durability and quality of responses19,20,21,22. Treatment with midostaurin for AdvSM can lead to challenging gastrointestinal side effects, limiting its efficacy. With avapritinib, a potent, selective inhibitor of KIT D816V, the clinical aim in AdvSM is to achieve deeper and enduring clinical, morphological and molecular responses, which could translate into extended survival with improved QoL.
A potential limitation of this prespecified interim analysis is the short duration of follow-up (10.4 months) in a subset of trial patients, which will be addressed in long-term follow-up analyses of the study. It is anticipated that findings from long-term analyses will be consistent with those observed in the phase 1 trial13.
In conclusion, interim results from the current phase 2 PATHFINDER trial corroborate the promising and durable outcomes observed in the phase 1 EXPLORER trial. Avapritinib administered at a starting dose of 200 mg QD was well tolerated and led to profound reductions in disease burden, improved patient symptoms and QoL, and elicited deep molecular responses of KIT D816V, highlighting the potential for modification of AdvSM disease natural history.
Methods
Participants
Eligible patients were ≥18 years of age and with a diagnosis of AdvSM confirmed by central review. The primary efficacy endpoint of ORR as per mIWG–MRT–ECNM criteria23 required an evaluable baseline C-finding (Supplementary Table 1), and these patients were enrolled into cohort 1. Patients who did not have an evaluable C-finding at baseline could not be assessed for the primary endpoint and were enrolled into cohort 2, with the exception of patients with MCL who, as per criteria, were enrolled in cohort 1 and evaluated for reductions in disease burden. As a result of emerging evidence that an increased risk of ICB is associated with grade 3 thrombocytopenia, the protocol was amended to exclude patients with baseline platelet count <50 × 109 l–1.
Additional inclusion criteria were as follows: patients with SM-AHN who had received previous treatment for the AHN component of disease if, in the opinion of the investigator, such therapy was appropriate; bone marrow biopsy taken within 56 days of cycle 1, day 1 (C1D1); serum tryptase levels ≥20 ng ml–1; ECOG performance status 0–3; discontinued cytoreductive therapy due to disease progression, refractory disease, lack of efficacy or intolerance if receiving therapy within the preceding 12 weeks; stable dose of nonantineoplastic SM therapies or corticosteroids (≤20 mg d–1 prednisone or equivalent) for ≥14 days before C1D8; and able to provide written informed consent. Patients were excluded for the following reasons: received previous treatment with avapritinib; received any cytoreductive therapy or an investigational agent <14 days and, for cladribine, interferon alpha, pegylated interferon and any antibody therapy, <28 days before obtaining screening bone marrow biopsy; received previous radiotherapy or any hematopoietic growth factor within 14 days before screening bone marrow biopsy; requires concomitant medication that is a strong inhibitor, strong inducer or moderate inducer of cytochrome P450 3A4; had a major surgical procedure within 14 days of the first dose of study drug; is a candidate for allogeneic hematopoietic stem cell transplantation for treatment of SM; eosinophilia and known positivity for the FIP1L1–PGDFRA fusion, unless the patient has demonstrated relapse or progressive disease on previous imatinib therapy; has history of another primary malignancy (within 3 years before the first dose of study drug), cerebrovascular accident or transient ischemic attacks (within 1 year before the first dose of study drug), or seizure disorder; has abnormal laboratory findings or QT interval corrected using Fridericia’s formula >480 ms; has known risk or recent history of ICB; has a primary brain malignancy or metastases to the brain; has clinically significant, uncontrolled cardiovascular disease; unless postmenopausal (females) or surgically sterile; is unwilling to abstain from sexual intercourse or employ highly effective contraception from the first dose of study drug and for at least 6 weeks after the last dose of study drug; pregnant or breastfeeding; hypersensitivity to avapritinib or to any of the excipients; unwilling or unable to comply with the study procedures or requirements; and participation in another interventional study.
Trial design and treatment
PATHFINDER (ClinicalTrials.gov identifier no. NCT03580655) is an ongoing, international, multicenter, open-label, single-arm, phase 2 registrational trial conducted in North America and Europe. Avapritinib was administered at a starting dose of 200 mg QD in 28-day cycles until progression, intolerance, withdrawal by the investigator or patient or death. Dose modification to as low as 25 mg QD was allowed as per prespecified criteria. Dose increases to 300 mg QD were allowed for lack of efficacy and dose interruptions for platelet counts <50 × 109 l–1 were required, although platelet transfusion and growth factor support were allowed on trial.
Previous cytoreductive therapy or investigational agents were permitted if received up to 14 days before the screening bone marrow sample or up to 28 days (cladribine, interferon alpha, pegylated interferon or any antibody therapy) before the screening marrow biopsy. Medications, including palliative and supportive care for disease-related symptoms, were permitted during the study and may include the following classes of agents: histamine receptor H1 and H2 blockers; proton pump inhibitors; osteoclast inhibitors (that is, bisphosphonates); leukotriene receptor antagonists; corticosteroids (not exceeding 20 mg d–1 of prednisone or equivalent, and dose must be stable for ≥14 days before C1D8); cromolyn sodium and other mast cell stabilizers; and omalizumab.
Trial outcomes and assessments
The primary endpoint was optimal ORR as per mIWG–MRT–ECNM criteria (Supplementary Table 2). Modifications to the IWG–MRT–ECNM criteria were previously described7,13. Responses as per mIWG–MRT–ECNM criteria were adjudicated by the Study Steering Committee based on data from every trial visit, and required confirmation of ≥12 weeks. Bone marrow samples were assessed by central pathology, and serum tryptase and KIT D816V VAF in the blood were analyzed by central laboratory.
The primary analysis was originally planned after 63 patients in cohort 1 had received at least ten cycles of therapy but, due to the high efficacy observed in the EXPLORER trial, an interim analysis was introduced early in the PATHFINDER trial, to be triggered when 32 patients in cohort 1 (interim analysis efficacy population) had sufficient follow-up to be adjudicated for response as per mIWG–MRT–ECNM criteria.
The key secondary endpoint was mean change from baseline in patient-reported TSS of the AdvSM–SAF, a validated measure to assess treatment benefit in AdvSM patients24,25. Other secondary endpoints included time to response (time from the start of treatment to the response according to mIWG–MRT–ECNM criteria); duration of response (DOR; time from first documented response to the date of the first documented disease progression/loss of response or death due to any cause, whichever occurred first); PFS (time from the start of treatment to the date of the first documented disease progression as per mIWG–MRT–ECNM criteria or death due to any cause, whichever occurred first); OS (time from the start of treatment to the date of death); and changes in mast cell burden, safety and QoL using EORTC–QLQ–C30. Additional planned secondary endpoints not reported in this manuscript included pharmacokinetics of avapritinib and morphological response based on the Pure Pathological Response criteria7,26.
Response according to mIWG–MRT–ECNM criteria was assessed at C1D15, C2D1, C3D1, C7D1 and every six cycles thereafter, 12 weeks after documentation of CR or PR, 4 weeks after progressive disease of the AdvSM and/or AHN components and at the end of therapy if discontinued for a reason other than progressive disease or initiation of alternative cytoreductive therapy. Patient-reported outcomes (AdvSM–SAF, PGIS and EORTC–QLQ–C30) were collected at each visit through cycle 17 and at the end of therapy (if before or at cycle 17).
All patients were followed for safety (until 30 days after treatment discontinuation) and for long-term survival every 3 months. Safety assessments included determination of ECOG performance status, clinical laboratory testing, vital signs, electrocardiograms, brain imaging (magnetic resonance imaging or computerized tomography scan) and physical examinations. Treatment-emergent AEs were defined as any AE that occurred between the first dose of avapritinib through 30 days after the last dose of avapritinib, and were graded according to National Cancer Institute Common Terminology Criteria for AEs, v.5.0.
Statistical analysis
The null hypothesis ORR of 28% versus the alternative hypothesis, ORR of 50%, a one-sided type I error rate of 0.025 and a sample size of approximately 63 patients in cohort 1 were determined to have 93.5% power using the exact one-sample binomial test. The null hypothesis, ORR of 28%, was based on ORR as per IWG–MRT–ECNM criteria for midostaurin19. The data cutoff date for this interim analysis was 23 June 2020, and was performed when 32 patients in cohort 1 had received six cycles of treatment and at least two postbaseline bone marrow assessments or had an end-of-study assessment at any timepoint. In the interim analysis, the null hypothesis was rejected if one-sided P < 0.00625. In the case of failure of the interim analysis, the final analysis would be tested at a one-sided alpha level of 0.02178. Two-sided 95% confidence intervals were based on the exact binomial distribution (Clopper–Pearson method). Time-to-event outcomes (DOR, PFS and OS) were determined using the Kaplan–Meier method, and estimates were computed using Greenwood’s formula. Summary statistics are presented for time to response. Maximum percentage baseline reduction in clinicopathological measures of response (bone marrow mast cells, serum tryptase, KIT D816V VAF and spleen volume) was based on patients with both baseline (last observation before the date of the first dose of avapritinib, including pre-dose assessments on this date) and at least one baseline assessment. The mean change from baseline AdvSM–SAF TSS to C11D1 was tested against the null hypothesis of ≥0. If one-sided, one-sample t-test P < 0.025, the null hypothesis was rejected. Summary statistics and change from baseline are presented for PGIS and QoL assessment by EORTC–QLQ–C30.
All safety analyses, QoL outcomes and secondary analyses were evaluated in the safety population, comprising all enrolled patients. All statistical analyses were conducted using SAS v.9.4 or higher.
Trial oversight and review
The trial was designed by the sponsor (Blueprint Medicines Corporation) and trial investigators. The full protocol was approved by the institutional review board (IRB) or independent ethics committee (IEC) of each participating center: St Michael’s Hospital Research Ethics Board, Toronto, Canada; East of England – Cambridge South Research Ethics Committee, Nottingham, UK; University of Pennsylvania Office of Regulatory Affairs, PA, USA; Dana-Farber Cancer Institute, Office for Human Research Studies, MA, USA; University of Utah IRB, UT, USA; University of Michigan Medical School Institutional Review Board, MI, USA; MD Anderson Cancer Center, Office of Protocol Research, TX, USA; Stanford University, Research Compliance Office, CA, USA; Columbia University Medical Center IRB, NY, USA; Western IRB, WA, USA; Rush University Medical Center IRB, IL, USA; Washington University, Human Research Protocol Office, MO, USA; Roswell Park IRB, NY, USA; Region Syddanmark, Vejle, Denmark; Comité de protection des personnes Sud Est 1, Saint-Étienne, France; Ethikkommission II der Universität Heidelberg, Medizinische Fakultät, Mannheim, Germany; Medical Ethics Review Board, Groningen, the Netherlands; Comitato Etico Campania Sud – ASL; Napoli 3 Sud, Italy; Comitato Etico Area Vasta Centro, Florence, Italy; CEIC Hospital Universitari Pare Tau Ii – Oficina de Recerca, Barcelona, Spain; REK SØR/ØST, Oslo, Norway; and Independent Bioethics Committee for Scientific Research at the Medical University of Gdansk, Gdansk, Poland. The trial was conducted in accordance with the Declaration of Helsinki, International Conference on Harmonisation guidelines for Good Clinical Practice and local regulations. All patients provided written informed consent. Participants were not compensated, except for reimbursement of reasonable travel expenses. Each local IRB/IEC was notified based on local regulations (where required by the IRB/IEC) of all serious, unexpected adverse drug reactions involving risk to human patients. The sponsor and authors jointly collected and analyzed the data. All authors had access to all data, reviewed and provided critical input to the manuscript and made the decision to submit it for publication. All authors vouch for the validity of the trial results and adherence to the protocol.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The anonymized derived data from this trial that underlie the results reported in this article will be made available, beginning 12 months and ending 5 years after this article’s publication, to any investigators who sign a data access agreement and provide a methodologically sound proposal to medinfo@blueprintmedicines.com. The trial protocol will also be made available, as will a data fields dictionary.
References
Evans, E. K. et al. A precision therapy against cancers driven by KIT/PDGFRA mutations. Sci. Transl. Med. 9, eaao1690 (2017).
Pardanani, A. Systemic mastocytosis in adults: 2019 update on diagnosis, risk stratification and management. Am. J. Hematol. 94, 363–377 (2019).
Orfao, A., Garcia-Montero, A. C., Sanchez, L. & Escribano, L. Recent advances in the understanding of mastocytosis: the role of KIT mutations. Br. J. Haematol. 138, 12–30 (2007).
Cohen, S. S. et al. Epidemiology of systemic mastocytosis in Denmark. Br. J. Haematol. 166, 521–528 (2014).
Lim, K.-H. et al. Systemic mastocytosis in 342 consecutive adults: survival studies and prognostic factors. Blood 113, 5727–5736 (2009).
Valent, P., Akin, C. & Metcalfe, D. D. Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood 129, 1420–1427 (2017).
Shomali, W. & Gotlib, J. Response criteria in advanced systemic mastocytosis: evolution in the era of KIT inhibitors. Int. J. Mol. Sci. 22, 2983 (2021).
Jawhar, M. et al. The clinical and molecular diversity of mast cell leukemia with or without associated hematologic neoplasm. Haematologica 102, 1035–1043 (2017).
Reiter, A., George, T. I. & Gotlib, J. New developments in diagnosis, prognostication, and treatment of advanced systemic mastocytosis. Blood 135, 1365–1376 (2020).
Awada, H., Thapa, B. & Visconte, V. The genomics of myelodysplastic syndromes: origins of disease evolution, biological pathways, and prognostic implications. Cells 9, 2512 (2020).
Ustun, C. et al. Advanced systemic mastocytosis: from molecular and genetic progress to clinical practice. Haematologica 101, 1133–1143 (2016).
Jawhar, M. et al. Additional mutations in SRSF2, ASXL1 and/or RUNX1 identify a high-risk group of patients with KIT D816V(+) advanced systemic mastocytosis. Leukemia 30, 136–143 (2016).
DeAngelo, D. J. et al. Safety and efficacy of avapritinib in advanced systemic mastocytosis: the phase 1 EXPLORER trial. Nat. Med. (in the press).
(EXPLORER) Study of BLU-285 in Patients with Advanced Systemic Mastocytosis (AdvSM) and Relapsed or Refractory Myeloid Malignancies (2021); https://clinicaltrials.gov/ct2/show/NCT02561988
(PATHFINDER) Study to Evaluate Efficacy and Safety of Avapritinib (BLU-285), a Selective KIT Mutation-Targeted Tyrosine Kinase Inhibitor, in Patients with Advanced Systemic Mastocytosis (2020); https://clinicaltrials.gov/ct2/show/NCT03580655
Blueprint Medicines (Netherlands) B.V. AYVAKYT® (avapritinib). Summary of product characteristics. https://ir.blueprintmedicines.com/news-releases/news-release-details/blueprint-medicines-announces-european-commission-approval (2020).
Heinrich, M. C. et al. Avapritinib in advanced PDGFRA D842V-mutant gastrointestinal stromal tumour (NAVIGATOR): a multicentre, open-label, phase 1 trial. Lancet Oncol. 21, 935–946 (2020).
Kang, Y. K. et al. Avapritinib versus regorafenib in locally advanced unresectable or metastatic GI stromal tumor: a randomized, open-label phase III study. J. Clin. Oncol. https://ascopubs.org/doi/full/10.1200/JCO.21.00217 (2021).
Novartis Europharm Limited. RYDAPT (midostaurin). Summary of product characteristics. https://www.ema.europa.eu/en/medicines/human/EPAR/rydapt (2021).
Novartis Pharmaceuticals Corporation. RYDAPT (midostaurin). Prescribing information. https://www.hcp.novartis.com/products/rydapt/acute-myeloid-leukemia/dosing-administration/ (2021).
Gotlib, J. et al. Efficacy and safety of midostaurin in advanced systemic mastocytosis. N. Engl. J. Med. 374, 2530–2541 (2016).
Stone, R. M. et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N. Engl. J. Med. 377, 454–464 (2017).
Gotlib, J. et al. International Working Group–Myeloproliferative Neoplasms Research and Treatment (IWG-MRT) & European Competence Network on mastocytosis (ECNM) consensus response criteria in advanced systemic mastocytosis. Blood 121, 2393–2401 (2013).
Gotlib, J. et al. Avapritinib, a potent and selective inhibitor of KIT D816V, improves symptoms of advanced systemic mastocytosis (AdvSM): analyses of patient reported outcomes (PROs) from the phase 1 (EXPLORER) study using the (AdvSM) Symptom Assessment Form (AdvSM-SAF), a new PRO questionnaire for (AdvSM). Blood 132, Suppl. 1 (2018).
Taylor, F. et al. Psychometric evaluation of the Advanced Systemic Mastocytosis Symptom Assessment Form (AdvSM-SAF). Leuk. Res. 108, 106606 (2021).
Gotlib, J. et al. Pure pathologic response is associated with improved overall survival in patients with advanced systemic mastocytosis receiving avapritinib in the phase I EXPLORER study. In American Society of Hematology 62nd Annual Meeting and Exposition (Virtual, 2020).
Acknowledgements
The trial was funded by Blueprint Medicines Corporation. The Sponsor was involved in the trial design, collection, analysis and interpretation of data, as well as data checking of information provided in the manuscript. However, ultimate responsibility for opinions, conclusions and data interpretation lies with the authors. We thank the patients, their families and all investigators involved in this trial. Additional pathology support was provided by A. Rets, K. Moser and K. Karner (University of Utah/ARUP Laboratories, Salt Lake City, UT, USA). Data management support was provided by C. Langford (Stanford Cancer Institute, Stanford, CA, USA). Medical writing support, including assisting authors with the development of drafts, preparation of figures, incorporation of comments, data checking and referencing, was provided by K. Tran and C. Tomas (both of Paragon, Knutsford, UK), and editorial support, including formatting, proofreading and submission, was provided by T. Taylor (Paragon, Knutsford, UK, supported by Blueprint Medicines Corporation in accordance with Good Publication Practice guidelines (www.ismpp.org/gpp3). J.G. is supported by an internal grant from the Stanford Cancer Institute Clinical Innovation Fund. A.R. is supported by the Deutsche José-Carreras Leukämiestiftung grant (no. DJCLS 08R/2020). A.M.V. is supported in part by a grant from Association Italiana per la Ricerca sul Cancro, Mynerva project (no. 21267). E.O.H. is supported by the National Cancer Institute (National Institutes of Health (NIH) nos. 1UE5CA246744-01 and P01-CA214278-03), the National Center for Advancing Translational Sciences (NIH no. NIH-NCATS UL1TR001878) and the National Heart, Lung, and Blood Institute (NIH no. R01-HL-148014-01A1). R.M. is supported by a P30 grant (no. CA054174). P.B. is supported by the National Cancer Institute (NIH, MD Anderson Cancer Center support grant P30 no. CA016672).
Author information
Authors and Affiliations
Contributions
B.G.M. was the medical monitor of the study. H.-M.L. led the generation of data analyses. J.G., A.R. and D.J.D. contributed equally. All authors were involved in data interpretation and in the writing, revision and critical review of the manuscript. All authors have approved the submitted version and are accountable for their contributions and the integrity of the work.
Corresponding author
Ethics declarations
Competing interests
J.G. is the Chair of the Study Steering Committee of the PATHFINDER trial, Chair of the Response and Adjudication Committee for the EXPLORER trial, has received research funding, served on advisory boards and received honoraria and funding to cover travel expenses from Blueprint Medicines Corporation. He has received research funding, is the co-chair of the phase 2 trial of ripretinib in AdvSM Study Steering Committee and has honoraria for these roles and serves on advisory boards for Deciphera. He also serves as Chair of the Central Response Review Committee for the phase 2 trial of bezuclastinib in AdvSM. A.R. has been a clinical advisory board/study steering committee member (PATHFINDER trial) and received honoraria and funding to cover travel expenses from Blueprint Medicines Corporation. He has received advisory board fees, speaking fees and travel support from Novartis, Deciphera, Incyte, Celgene, AOP Pharmaceuticals and AbbVie, and research support from Novartis. D.H.R. has been a clinical advisory board/study steering committee member (EXPLORER and PATHFINDER studies) for Blueprint Medicines Corporation, and was involved with educational events and advisory boards for Novartis. M.W.D. has received honorarium fees from Blueprint Medicines Corporation, Incyte, Medscape, Sangamo and Takeda; consultancy fees from Blueprint Medicines Corporation, DisperSol, Fusion Pharma, Novartis and Sangamo; and research funding from Blueprint Medicines Corporation, Incyte, Leukemia & Lymphoma Society, Novartis, Pfizer, SPARC and Takeda. He is part of Study Steering Committees for Blueprint Medicines Corporation and Takeda and is a case author for Medscape. T.I.G. has been a clinical advisory board/study steering committee member (EXPLORER and PATHFINDER studies) and has received consulting fees from Blueprint Medicines Corporation, Celgene and Incyte. J.P. has received honorarium fees from Apellis, Blueprint Medicines Corporation, BMS, Grünenthal, MSD, Sobi and F. Hoffmann-La Roche. He has served on the speaker’s bureau of Alexion, Boehringer Ingelheim, Novartis, Pfizer and Chugai. A.M.V. has participated in speakers’ bureaux for AOP, BMS-Celgene, Novartis and Shire, and on advisory boards for AbbVie, BMS-Celgene, CTI BioPharma, Incyte and Novartis. U.P. received research funding from BMS, Amgen, Novartis, Curis and BerGenBio. I.A.-T. has served on advisory boards for, and received honoraria and research funding from, Blueprint Medicines Corporation and has participated in educational events for Novartis. A.M. has received honorarium fees from Takeda, Pfizer, Novo Nordisk, Behring, AbbVie, Novartis, Cilag, Janssen and Bayer. O.H. received research funding from AB Science, BMS/Celgene, Alexion, Novartis and Inatherys, consulted for AB Science and is a shareholder for AB Science. I.D. has received advisory board fees from Novartis. E.O.H. has received research support (institution) from Blueprint Medicines Corporation, Samus Therapeutics and Novartis Oncology. She serves on a data safety monitoring committee for Blueprint Medicines Corporation and is a member of the hematology exam committee for the American Board of Internal Medicine. L.K.H. has received research support (institution) from Gilead Sciences. L.S. has no disclosures. R.M. has been a consultant for Novartis, Sierra Oncology and La Jolla Pharma and has received research support from Celgene, Incyte, AbbVie, Samus, Genentech, Promedior and CTI BioPharma. P.B. has received research support from Incyte, Celgene (now BMS), CTI BioPharma, Kartos, Blueprint Medicines Corporation, Constellation, Astellas, Pfizer, NS Pharma and Promedior; and honoraria from Incyte, Celgene (now BMS), CTI BioPharma, Kartos and Blueprint Medicines Corporation. K.M.P. has participated on advisory boards for CTI BioPharma, PharmaEssentia and Kura Oncology. M.L.H. has received research funding from Blueprint Medicines Corporation, BMS, CTI BioPharma, Deciphera, Incyte, Novartis and Sierra Oncology; and consulting fees from AbbVie, CTI BioPharma, Novartis, Blueprint Medicines Corporation and Partner Therapeutics. S.T.O. has been a consultant for Gilead Sciences, Novartis, Kartos Therapeutics, CTI BioPharma, Celgene/Bristol Myers Squibb, Disc Medicine, Blueprint Medicines Corporation, PharmaEssentia, Constellation and Incyte. J.S., H.-M.L. and B.G.M. are employees and/or equity holders of Blueprint Medicines Corporation. D.J.D. has been a clinical advisory board/study steering committee member (EXPLORER and PATHFINDER studies) for Blueprint Medicines Corporation. He has served as a consultant for Amgen, Agios, Autolus, Forty-Seven, Incyte Corporation, Jazz, Novartis, Pfizer, Shire and Takeda; and has received research funding from AbbVie, GlycoMimetics and Novartis.
Additional information
Peer review information Nature Medicine thanks Jongphil Kim, Michael Mauro and Guillermo Garcia-Manero for their contribution to the peer review of this work. Primary Handling Editor: Saheli Sadanand, in collaboration with the Nature Medicine team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Patient Disposition.
*Cohort 1: Patients with AdvSM and ≥1 mIWG-MRT-ECNM criteria for evaluable disease (have severe and quantifiable organ damage (an evaluable C-finding) or have MCL (regardless of C-findings)) as confirmed by the SSC. Twenty patients in Cohort 1 were not included in the interim analysis efficacy population due to lack of sufficient follow-up. †Patients with AdvSM who were not considered eligible for an adjudicated response and were confirmed centrally to have ASM or SM-AHN, but were lacking an evaluable C-finding as determined by the SSC. ‡No patient discontinued from treatment due to lost to follow-up, protocol deviation, pregnancy, investigator decision, non-compliance, sponsor decision, or other reason. AdvSM, advanced systemic mastocytosis; AHN, associated hematologic neoplasm; AML, acute myeloid leukemia; ASM, aggressive systemic mastocytosis; MCL, mast cell leukemia; mIWG-MRT-ECNM, modified International Working Group-Myeloproliferative Neoplasms Research and Treatment and European Competence Network on Mastocytosis; SM-AHN, systemic mastocytosis with an associated hematologic neoplasm; SSC, study steering committee; WHO, World Health Organization.
Extended Data Fig. 2 Prior Anti-Neoplastic Therapies (Interim Analysis Efficacy Population, n = 32).
Table shows details of prior therapies received by patients that ended on or before the first dose date of avapritinib.
Extended Data Fig. 3 Baseline Characteristics.
Baseline characteristics including for patients not included in the interim analysis (n = 30). AdvSM, advanced systemic mastocytosis; ASM, aggressive systemic mastocytosis; ddPCR, droplet digital polymerase chain reaction; ECOG, Eastern Cooperative Oncology Group; MCL, mast cell leukemia; mIWG-MRT-ECNM, modified International Working Group-Myeloproliferative Neoplasms Research and Treatment and European Competence Network on Mastocytosis; SM-AHN, systemic mastocytosis with associated hematologic neoplasm.
Extended Data Fig. 4 Response by mIWG-MRT-ECNM C-Findings (Interim Analysis Efficacy Population, n = 32).
*Definitions of C-findings per mIWG-MRT-ECNM and criteria for measuring clinical improvement are presented in Supplementary Table 1 and Supplementary Table 2. †Percentages are based on the number of patients with C-finding at baseline. ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; mIWG-MRT-ECNM, modified International Working Group-Myeloproliferative Neoplasms Research and Treatment and European Competence Network on Mastocytosis; ORR, overall response rate; ULN, upper limit of normal.
Extended Data Fig. 5 Change from Baseline in Clinicopathological Measures of Disease Burden.
a, Peripheral blood absolute monocyte count in patients with SM-CMML. b, Peripheral blood absolute eosinophil count in patients with baseline eosinophilia. SM-CMML, systemic mastocytosis with chronic myelomonocytic leukemia.
Extended Data Fig. 6 Adverse Events Leading to Dose Modifications.
*Pooled terms. †Patient reported to have increased bleeding propensity with subcutaneous hematoma. AE, adverse event.
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gotlib, J., Reiter, A., Radia, D.H. et al. Efficacy and safety of avapritinib in advanced systemic mastocytosis: interim analysis of the phase 2 PATHFINDER trial. Nat Med 27, 2192–2199 (2021). https://doi.org/10.1038/s41591-021-01539-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01539-8
This article is cited by
-
Adverse Event Reporting in Cancer Clinical Trials: Incorporating Patient-Reported Methods. A Systematic Scoping Review
The Patient - Patient-Centered Outcomes Research (2024)
-
Allogeneic haematopoietic cell transplantation for advanced systemic mastocytosis: Best practice recommendations on behalf of the EBMT Practice Harmonisation and Guidelines Committee
Leukemia (2024)
-
Allogeneic Hematopoietic Cell Transplantation in Advanced Systemic Mastocytosis: A retrospective analysis of the DRST and GREM registries
Leukemia (2024)
-
SETD2 non genomic loss of function in advanced systemic mastocytosis is mediated by an Aurora kinase A/MDM2 axis and can be therapeutically targeted
Biomarker Research (2023)
-
Diagnostik und Therapie der systemischen Mastozytose
best practice onkologie (2023)