Abstract
While increasing literature demonstrating the direct and indirect impacts of climate change focuses on health, the capacity and preparedness of healthcare systems to deal with these impacts are less frequently considered. Here we performed a systematic analysis of peer-reviewed and grey literature to assess the current and projected coping capacity for healthcare systems under climate change. Data from the 129 included publications focused broadly on seven topics: workforce, tools and frameworks, infrastructure and urban planning, communication, surge capacity and increased system burden, service interruption and financial costs. Publications were biased towards high-level representation of acute disaster events, particularly in Global North countries. Non-peer-reviewed literature such as policy and planning documents, which may offer further insights into preparedness, were under-represented and could be a feature of next-generation research. Health systems need to be future proofed through effective policies, adequately trained workforces and redesigned infrastructure to meet the increasing burdens of climate change.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All datasets generated and analysed for this study, including the search strategy, list of the included and excluded studies, data extracted, analysis plans and quality assessment are available in the article or Supplementary Information. This includes all data used for creating display items. No individual participant data was used for this study.
References
Costello, A. et al. Climate change threatens our health and survival within decades. Lancet 401, 85–87 (2023).
The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment (US Global Change Research Program, 2016).
Romanello, M. et al. The 2022 report of the Lancet Countdown on health and climate change: health at the mercy of fossil fuels. Lancet 400, 1619–1654 (2022).
Al-Marwani, S. Climate change impact on the healthcare provided to patients. Bull. Natl Res. Cent. 47, 51 (2023).
Climate change and health. World Health Organization https://www.who.int/teams/environment-climate-change-and-health/climate-change-and-health/country-support/building-climate-resilient-health-systems (2024).
Organisation for Economic Co-operation and Development. Ready for the Next Crisis? Investing in Health System Resilience (OECD, 2023).
R3 Report—Requirement, Rationale, Reference (The Joint Commission, 2021).
Rocklöv, J. & Dubrow, R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat. Immunol. 21, 479–483 (2020).
How can climate change affect natural disasters? USGS https://www.usgs.gov/faqs/how-can-climate-change-affect-natural-disasters (2024).
Montgomery, H. E. et al. The future of UK healthcare: problems and potential solutions to a system in crisis. Ann. Oncol. 28, 1751–1755 (2017).
Asthana, S. & Gibson, A. The National Health Service (NHS) in ‘crisis’: the role played by a shift from horizontal to vertical principles of equity. Health Econ. Policy L 15, 1–17 (2020).
Orton, P. & Gray, D. P. Burnout in NHS staff. Lancet 385, 1831 (2015).
Zhang, J., Budhdeo, S. & Ashrafian, H. Failing IT infrastructure is undermining safe healthcare in the NHS. Br. Med. J. 379, e073166 (2022).
OECD. Health at a Glance 2021: OECD Indicators Ch. 5, 138–139 (OECD, 2021).
Propper, C., Stoye, G. & Zaranko, B. The wider impacts of the coronavirus pandemic on the NHS. Fisc. Stud. 41, 345–356 (2020).
Petterson, J. S., Stanley, L. D., Glazier, E. & Philipp, J. A preliminary assessment of social and economic impacts associated with Hurricane Katrina. Am. Anthropol. 108, 643–670 (2006).
Vaughan, A. Deadly floods in Pakistan. N. Sci. 255, 7 (2022).
Cameron, P. A. et al. Black Saturday: the immediate impact of the February 2009 bushfires in Victoria, Australia. Med. J. Aust. 191, 11–16 (2009).
Jalaludin, B., Johnston, F., Vardoulakis, S. & Morgan, G. Reflections on the catastrophic 2019–2020 Australian bushfires. Innovation 1, 100010 (2020).
Clarke, B., Otto, F., Stuart-Smith, R. & Harrington, L. Extreme weather impacts of climate change: an attribution perspective. Environ. Res. Clim. 1, 012001 (2022).
Newman, R. & Noy, I. The global costs of extreme weather that are attributable to climate change. Nat. Commun. 14, 6103 (2023).
Ebi, K. L., Ogden, N. H., Semenza, J. C. & Woodward, A. Detecting and attributing health burdens to climate change. Environ. Health Perspect. 125, 085004 (2017).
Rocque, R. J. et al. Health effects of climate change: an overview of systematic reviews. BMJ Open 11, e046333 (2021).
Liu, F., Chang-Richards, A., Wang, K. I.-K. & Dirks, K. N. Effects of climate change on health and wellbeing: a systematic review. Sustain. Dev. 31, 2067–2090 (2023).
Cronbach, L. J. Coefficient alpha and the internal structure of tests. Psychometrika 16, 297–334 (1951).
Negev, M. et al. Adaptation of health systems to climate-related migration in Sub-Saharan Africa: closing the gap. Int. J. Hyg. Environ. Health 222, 311–314 (2019).
Kendrovski, V. & Schmoll, O. Priorities for protecting health from climate change in the WHO European Region: recent regional activities. Bundesgesundheitsbl 62, 537–545 (2019).
Lowe, R. et al. Building resilience to mosquito-borne diseases in the Caribbean. PLoS Biol. 18, e3000791 (2020).
World Bank country and lending groups. World Bank https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (2024).
Alson, R., Alexander, D., Leonard, R. B. & Stringer, L. W. Analysis of medical treatment at a field hospital following Hurricane Andrew, 1992. Ann. Emerg. Med. 22, 1721–1728 (1993).
Grover, J. M. et al. Novel use of telemedicine by hurricane evacuation shelters. Prehosp. Emerg. Care 24, 804–812 (2020).
Clay, L. A., Stone, K. W. & Horney, J. A. Quantifying disaster impacts on local public health agency’s leadership, staffing, and provision of essential public health services. Disaster Med. Public Health Prep. 16, 1552–1557 (2022).
Davis, M. V., MacDonald, P. D., Cline, J. S. & Baker, E. L. Evaluation of public health response to hurricanes finds North Carolina better prepared for public health emergencies. Public Health Rep. 122, 17–26 (2007).
Smith, C. M. & Graffeo, C. S. Regional impact of Hurricane Isabel on emergency departments in coastal southeastern Virginia. Acad. Emerg. Med. 12, 1201–1205 (2005).
Radcliff, T. A., Chu, K., Der-Martirosian, C. & Dobalian, A. Comparing primary health-care service delivery disruptions across disasters. Disaster Med. Public Health Prep. 16, 1802–1805 (2021).
Hamichi, S. E., Gold, A. S., Graversen, V. K., Latiff, A. & Murray, T. G. Disaster preparedness impact in a complex ophthalmology practice: a review of patients receiving intravitreal injections. Clin. Ophthalmol. 13, 1999–2002 (2019).
Chowdhury, M. A. B. et al. Health impact of Hurricanes Irma and Maria on St Thomas and St John, US Virgin Islands, 2017–2018. Am. J. Public Health 109, 1725–1732 (2019).
Irvin-Barnwell, E. A. et al. Evaluating disaster damages and operational status of health-care facilities during the emergency response phase of Hurricane Maria in Puerto Rico. Disaster Med. Public Health Prep. 14, 80–88 (2020).
Kleinpeter, M. A. Shifts in dialysis patients from natural disasters in 2005. Hemodial. Int. 11, S33–S37 (2007).
Pierce, J. R. Jr, Pittard, A. E. I., West, T. A. & Richardson, J. M. Medical response to Hurricanes Katrina and Rita: local public health preparedness in action. J. Public Health Manag. Pract. 13, 441–446 (2007).
Hutson, L. R. Jr, Vega, J. & Schubert, A. Impact of Hurricanes Katrina and Rita on the anesthesiology workforce. Ochsner J. 11, 29–33 (2011).
Adalja, A. A. et al. Absorbing citywide patient surge during Hurricane Sandy: a case study in accommodating multiple hospital evacuations. Ann. Emerg. Med. 64, 66–73.e61 (2014).
Greenstein, J., Chacko, J., Ardolic, B. & Berwald, N. Impact of Hurricane Sandy on the Staten Island University Hospital emergency department. Prehosp. Disaster Med. 31, 335–339 (2016).
Lin, C.-J., Pierce, L. C., Roblin, P. M. & Arquilla, B. Impact of Hurricane Sandy on hospital emergency and dialysis services: a retrospective survey. Prehosp. Disaster Med. 29, 374–379 (2014).
Mbewe, C. & Jones, M. Hurricane Sandy: competencies needed to contend with natural disasters. MedSurg. Nurs. 22, 1–5 (2013).
Sebek, K., Jacobson, L., Wang, J., Newton-Dame, R. & Singer, J. Assessing capacity and disease burden in a virtual network of New York City primary care providers following Hurricane Sandy. J. Urban Health 91, 615–622 (2014).
Stryckman, B., Walsh, L., Carr, B. G., Hupert, N. & Lurie, N. Impact of Superstorm Sandy on Medicare patients' utilization of hospitals and emergency departments. West. J. Emerg. Med. 18, 1035–1041 (2017).
Bonilla-Félix, M. & Suárez-Rivera, M. Disaster management in a nephrology service: lessons learned from Hurricane Maria. Blood Purif. 47, 199–204 (2019).
Bucher, J. et al. EMS dispatches during Hurricanes Irene and Sandy in New Jersey. Prehosp. Emerg. Care 22, 15–21 (2017).
Doran, K. et al. Emergency department visits for homelessness or inadequate housing in New York City before and after Hurricane Sandy. J. Urban Health 93, 331–344 (2016).
Kim, H., Ahn, M. E., Lee, K. H., Kim, Y. C. & Hong, E. S. Disaster medical assistance in super typhoon Haiyan: collaboration with the local medical team that resulted in great synergy. Ulus. Travma Acil Cerrahi Derg. 21, 143–148 (2015).
Gray, N. A., Wolley, M., Liew, A. & Nakayama, M. Natural disasters and dialysis care in the Asia Pacific. Nephrology 20, 873–880 (2015).
Johnson, D. W. et al. Renal services disaster planning: lessons learnt from the 2011 Queensland floods and North Queensland cyclone experiences. Nephrology 18, 41–46 (2013).
Ryan, B. J. et al. Analyzing the impact of Severe Tropical Cyclone Yasi on public health infrastructure and the management of noncommunicable diseases. Prehosp. Disaster Med. 30, 28–37 (2015).
Nates, J. L. Combined external and internal hospital disaster: impact and response in a Houston trauma center intensive care unit. Crit. Care Med. 32, 686–690 (2004).
Paterson, J., Berr, P., Ebi, K. & Varangu, L. Health care facilities resilient to climate change impacts. Int. J. Environ. Res. Public Health 11, 13097–13116 (2014).
Lai, T., Shih, F., Chiang, W., Shen, S. & Chen, W. Strategies of disaster response in the health care system for tropical cyclones: experience following Typhoon Nari in Taipei City. Acad. Emerg. Med. 10, 1109–1112 (2003).
van Oldenborgh, G. J. et al. Attribution of extreme rainfall from Hurricane Harvey, August 2017. Environ. Res. Lett. 12, 124009 (2017).
Irish, J. L., Sleath, A., Cialone, M. A., Knutson, T. R. & Jensen, R. E. Simulations of Hurricane Katrina (2005) under sea level and climate conditions for 1900. Clim. Change 122, 635–649 (2014).
Clarke, B. J., Otto, F. E. L. & Jones, R. G. Inventories of extreme weather events and impacts: implications for loss and damage from and adaptation to climate extremes. Clim. Risk Manag. 32, 100285 (2021).
Irvin, C. B. & Atas, J. G. Management of evacuee surge from a disaster area: solutions to avoid non-emergent, emergency department visits. Prehosp. Disaster Med. 22, 220–223 (2007).
Hamilton, D. R. et al. Houston’s medical disaster response to Hurricane Katrina: part 1: the initial medical response from trauma service area Q. Ann. Emerg. Med. 53, 505–514 (2009).
Hamilton, D. R. et al. Houston’s medical disaster response to Hurricane Katrina: part 2: transitioning from emergency evacuee care to community health care. Ann. Emerg. Med. 53, 515–527 (2009).
Hoang Van, M. et al. Primary healthcare system capacities for responding to storm and flood-related health problems: a case study from a rural district in central Vietnam. Glob. Health Action 7, 1–11 (2014).
Joy, T. L. & Kemp, H. N. Managing the Hurricane Katrina disaster in the Midwest. J. Trauma Nurs. 14, 70–72 (2007).
Rakotoarison, N. et al. Assessment of risk, vulnerability and adaptation to climate change by the health sector in Madagascar. Int. J. Environ. Res. Public Health 15, 2643 (2018).
Rathnayake, D., Clarke, M. & Jayasooriya, L. Hospital surge capacity: the importance of better hospital pre-planning to cope with patient surge during dengue epidemics—a systematic review. Int. J. Healthc. Manag. 14, 723–730 (2021).
Shoaf, K. Organizing the health sector for response to disasters. Ciên Saúde Colet. 19, 3705–3715 (2014).
Toloo, G., Hu, W., Fitzgerald, G., Aitken, P. & Tong, S. Projecting excess emergency department visits and associated costs in Brisbane, Australia, under population growth and climate change scenarios. Sci. Rep. 5, 12860 (2015).
Turner, L. R., Connell, D. & Tong, S. The effect of heat waves on ambulance attendances in Brisbane, Australia. Prehosp. Disaster Med. 28, 482–487 (2013).
Boom, J. A., Dragsbaek, A. C. & Nelson, C. S. The success of an immunization information system in the wake of Hurricane Katrina. Pediatrics 119, 1213–1217 (2007).
Broz, D. et al. Lessons learned from Chicago’s emergency response to mass evacuations caused by Hurricane Katrina. Am. J. Public Health 99, 1496–1504 (2009).
Calkins, M. M., Isaksen, T. B., Stubbs, B. A., Yost, M. G. & Fenske, R. A. Impacts of extreme heat on emergency medical service calls in King County, Washington, 2007–2012: relative risk and time series analyses of basic and advanced life support. Environ. Health 10.1186/s12940-016-0109-0 (2016).
Carrington, M. A., Ranse, J. & Hammad, K. The impact of disasters on emergency department resources: review against the Sendai framework for disaster risk reduction 2015–2030. Australas. Emerg. Care 24, 55–60 (2021).
Casey, J. A. et al. Wildfire particulate matter in Shasta County, California and respiratory and circulatory disease-related emergency department visits and mortality, 2013–2018. Environ. Epidemiol. 5, e124 (2021).
Eastman, A. L., Rinnert, K. J., Nemeth, I. R., Fowler, R. L. & Minei, J. P. Alternate site surge capacity in times of public health disaster maintains trauma center and emergency department integrity: Hurricane Katrina. J. Trauma 63, 253–257 (2007).
Klein, K. R., Pepe, P. E., Burkle, F. M. Jr, Nagel, N. E. & Swienton, R. E. Evolving need for alternative triage management in public health emergencies: a Hurricane Katrina case study. Disaster Med. Public Health Prep. 2, S40–S44 (2008).
Rublee, C., Bills, C., Sorensen, C., Lemery, J. & Calvello Hynes, E. At ground zero—emergency units in low- and middle-income countries building resilience for climate change and human health. World Med. Health Policy 13, 36–68 (2021).
Acharya, L., Upadhya, K. D. & Kortmann, F. Mental health and psychosocial support aspects in disaster preparedness: Nepal. Int. Rev. Psychiatry 18, 587–592 (2006).
Baker, N. D., Feldman, M. S. & Lowerson, V. Working through disaster: re-establishing mental health care after Hurricane Katrina. Disaster Med. Public Health Prep. 6, 311–315 (2012).
Bassilios, B., Reifels, L. & Pirkis, J. Enhanced primary mental health services in response to disaster. Psychiat. Serv. 63, 868–874 (2012).
Hoffpauir, S. A. & Woodruff, L. A. Effective mental health response to catastrophic events: lessons learned from Hurricane Katrina. Fam. Commun. Health 31, 17–22 (2008).
Palinkas, L. A., O’Donnell, M. L., Lau, W. & Wong, M. Strategies for delivering mental health services in response to global climate change: a narrative review. Int. J. Environ. Res. Public Health 17, 8562 (2020).
Gavagan, T. F. et al. Hurricane Katrina: medical response at the Houston astrodome/reliant center complex. South. Med. J. 99, 933–939 (2006).
Hwong, A. R. et al. Climate change and mental health: implications for the psychiatric workforce. Psychiat. Serv. 73, 592–595 (2022).
Bambrick, H. J., Woodruff, R. E. & Hanigan, I. V. Climate change could threaten blood supply by altering the distribution of vector-borne disease: an Australian case-study. Glob. Health Action 2, 2059 (2009).
Hogue, M. D., Hogue, H. B., Lander, R. D., Avent, K. & Fleenor, M. The nontraditional role of pharmacists after Hurricane Katrina: process description and lessons learned. Public Health Rep. 124, 217–223 (2009).
Howard, D., Zhang, R., Huang, Y. & Kutner, N. Hospitalization rates among dialysis patients during Hurricane Katrina. Prehosp. Disaster Med. 27, 325–329 (2012).
Kenney, R. J. Emergency preparedness concepts for dialysis facilities: reawakened after Hurricane Katrina. Clin. J. Am. Soc. Nephrol. 2, 809–813 (2007).
Kleinpeter, M. A. End-stage renal disease use in hurricane-prone areas: should nephrologists increase the utilization of peritoneal dialysis? Adv. Chronic Kidney Dis. 14, 100–104 (2007).
Kleinpeter, M. A., Norman, L. D. & Krane, N. K. Dialysis services in the hurricane-affected areas in 2005: lessons learned. Am. J. Med. Sci. 332, 259–263 (2006).
Kleinpeter, M. A., Norman, L. D. & Krane, N. K. Disaster planning for peritoneal dialysis programs. Adv. Perit. Dial. 22, 124–129 (2006).
Kopp, J. B. et al. Kidney patient care in disasters: lessons from the hurricanes and earthquake of 2005. Clin. J. Am. Soc. Nephrol. 2, 814–824 (2007).
Mitchell, L. et al. Lessons learned from Hurricane Ike. Assoc. Oper. Room Nurs. 89, 1073–1078 (2009).
Gay, H. A. et al. Lessons learned from Hurricane Maria in Puerto Rico: practical measures to mitigate the impact of a catastrophic natural disaster on radiation oncology patients. Pract. Radiat. Oncol. 9, 305–321 (2019).
Bluth, E. I. et al. Managing in a catastrophe: radiology during Hurricane Katrina. Am. J. Roentgenol. 188, 630–632 (2007).
De Guzman, R. & Malik, M. Global cancer burden and natural disasters: a focus on Asia’s vulnerability, resilience building, and impact on cancer care. J. Glob. Oncol. 5, 1–8 (2019).
Barfield, W. D. & Krug, S. E. Disaster preparedness in neonatal intensive care units. Pediatrics 139, e20170507 (2017).
Bein, T., Karagiannidis, C. & Quintel, M. Climate change, global warming, and intensive care. Intens. Care Med. 46, 485–487 (2020).
van Stralen, D., McKay, S. D. & Mercer, T. A. Disaster series: prolonged improvisation during hurricanes—high reliability organizing in the NICU. Neonatol. Today 17, 10–27 (2022).
Alzaga, A. G., Varon, J. & Nanlohy, S. Natural catastrophes: disaster management and implications for the acute care practitioner. Crit. Care Shock 8, 1–5 (2005).
Apisarnthanarak, A., Mundy, L. M., Khawcharoenporn, T. & Mayhall, C. G. Hospital infection prevention and control issues relevant to extensive floods. Infect. Control Hosp. Epidemiol. 34, 200–206 (2013).
Baten, A., Wallemacq, P., van Loenhout, J. A. F. & Guha-Sapir, D. Impact of recurrent floods on the utilization of maternal and newborn healthcare in Bangladesh. Matern. Child Health J. 24, 748–758 (2020).
Hoyt, K. S. & Gerhart, A. E. The San Diego County wildfires: perspectives of healthcare. Disaster Manag. Response 2, 46–52 (2004).
Khademipour, G. & Sheikhbardsiri, H. Disaster risk assessment of primary healthcare facilities in South East of Iran: a study with approach of disaster risk reduction. Disaster Emerg. Med. J. 7, 11–20 (2022).
Kim, J., Lee, A. & Rossin-Slater, M. What to expect when it gets hotter. Am. J. Health Econ. 7, 281–305 (2021).
Koka, P. M. et al. Disaster preparedness and response capacity of regional hospitals in Tanzania: a descriptive cross-sectional study. BMC Health Serv. Res. 18, 835 (2018).
Lin, S. et al. Excessive heat and respiratory hospitalizations in New York State: estimating current and future public health burden related to climate change. Environ. Health Perspect. 120, 1571–1577 (2012).
Milsten, A. Hospital responses to acute-onset disasters: a review. Prehosp. Disaster Med. 15, 32–45 (2000).
Munasinghe, N. L. & Matsui, K. Examining disaster preparedness at Matara District General Hospital in Sri Lanka. Int. J. Disaster Risk Reduct. 40, 101154 (2019).
Nenković-Riznić, M., Brankov, B., Petrović, S. & Pucar, M. Safe healthcare facilities—their place and role in resilient cities. Therm. Sci. 22, S1001–S1010 (2018).
Blazejczyk, A., Blazejczyk, K., Baranowski, J. & Kuchcik, M. Heat stress mortality and desired adaptation responses of healthcare system in Poland. Int. J. Biometeorol. 62, 307–318 (2018).
Lilienfeld, E., Nicholas, P. K., Breakey, S. & Corless, I. B. Addressing climate change through a nursing lens within the framework of the United Nations Sustainable Development Goals. Nurs. Outlook 66, 482–494 (2018).
Andrews, R. J. & Quintana, L. M. Unpredictable, unpreventable and impersonal medicine: global disaster response in the 21st century. EPMA J. 6, 2 (2015).
Arrieta, M. I., Foreman, R. D., Crook, E. D. & Icenogle, M. L. Insuring continuity of care for chronic disease patients after a disaster: key preparedness elements. Am. J. Med. Sci. 336, 128–133 (2008).
Farley, J. M., Suraweera, I., Perera, W. L. S. P., Hess, J. & Ebi, K. L. Evaluation of flood preparedness in government healthcare facilities in Eastern Province, Sri Lanka. Glob. Health Action 10, 1331539 (2017).
Li, L. Z., Liao, S. N., Yuan, J. F., Wang, E. D. & She, J. J. Analyzing healthcare facility resilience: scientometric review and knowledge map. Front. Public Health 9, 764069 (2021).
Ramana Dhara, V., Schramm, P. J. & Luber, G. Climate change & infectious diseases in India: implications for health care providers. Indian J. Med. Res. 138, 847–852 (2013).
Abbas, H. B. & Routray, J. K. A semi-quantitative risk assessment model of primary health care service interruption during flood: case study of Aroma locality, Kassala State of Sudan. Int. J. Disaster Risk Reduct. 6, 118–128 (2013).
Älgå, A., Dang, T. A. T., Saulnier, D. D., Nguyen, G. T. & von Schreeb, J. Hope for the best, prepare for the worst—an assessment of flood preparedness at primary health care facilities in central Vietnam. Int. J. Environ. Res. Public Health 15, 2689 (2018).
McMichael, T., Blashki, G. & Karoly, D. J. Climate change and primary health care. Aust. Fam. Physician 36, 12 (2007).
Walker, R. Climate change and primary health care intervention framework. Aust. J. Prim. Health 15, 276–284 (2009).
Achour, N., Pascale, F., Soetanto, R. & Price, A. D. F. Healthcare emergency planning and management to major hazards in the UK. Int. J. Emerg. Manag. 11, 1–19 (2015).
Balbus, J. et al. Enhancing the sustainability and climate resiliency of health care facilities: a comparison of initiatives and toolkits. Rev. Panam. Salud Publica 40, 174–180 (2016).
Bartlett, J. G. Planning for avian influenza. Ann. Intern. Med. 145, 141–144 (2006).
Bartlett, J. G. & Borio, L. The current status of planning for pandemic influenza and implications for health care planning in the United States. Clin. Infect. Dis. 46, 919–925 (2008).
Hassan, E. M. & Mahmoud, H. N. Orchestrating performance of healthcare networks subjected to the compound events of natural disasters and pandemic. Nat. Commun. 12, 1338 (2021).
Kumar, A. et al. National programme on climate change and human health—India, 2019. J. Commun. Dis. 52, 43–48 (2020).
Mousavi, A. et al. Climate change and health in Iran: a narrative review. J. Environ. Health Sci. 18, 367–378 (2020).
Operational Framework for Building Climate Resilient Health Systems (World Health Organization, 2015).
Sellers, S. & Ebi, K. L. Climate change and health under the Shared Socioeconomic Pathway framework. Int. J. Environ. Res. Public Health 15, 3 (2018).
Tadesse, L. & Ardalan, A. Health sector initiatives for disaster risk management in Ethiopia: a narrative review. PLoS Curr. https://doi.org/10.1371/currents.dis.949664319ad451313b499f9c90cd9c0f (2014).
Tekeli-Yeşil, S. Public health and natural disasters: disaster preparedness and response in health systems. J. Public Health 14, 317–324 (2006).
Berry, P., Enright, P. M., Shumake-Guillemot, J., Villalobos Prats, E. & Campbell-Lendrum, D. Assessing health vulnerabilities and adaptation to climate change: a review of international progress. Int. J. Environ. Res. Public Health 15, 2626 (2018).
Bishop-Williams, K. E. et al. Understanding weather and hospital admissions patterns to inform climate change adaptation strategies in the healthcare sector in Uganda. Int. J. Environ. Res. Public Health 15, 2402 (2018).
Blashki, G. et al. Preparing health services for climate change in Australia. Asia Pac. J. Public Health 23, 133S–143S (2011).
Boodram, L.-L. G. et al. Health impact and multisectoral response to a major flooding event in Trinidad, October 2018. Int. Public Health J. 12, 427–433 (2020).
Butterfield, P., Leffers, J. & Vásquez, M. D. Nursing’s pivotal role in global climate action. Br. Med. J. 373, n1049 (2021).
Chen, T., Radke, J. D., Lang, W. & Li, X. Environment resilience and public health: assessing healthcare’s vulnerability to climate change in the San Francisco Bay area. Growth Change 51, 607–625 (2020).
Confalonieri, U. E., Menezes, J. A. & de Souza, C. M. Climate change and adaptation of the health sector: the case of infectious diseases. Virulence 6, 554–557 (2015).
Curtis, S., Fair, A., Wistow, J., Val, D. V. & Oven, K. Impact of extreme weather events and climate change for health and social care systems. Environ. Health 16, 23–32 (2017).
Darsey, D. A., Carlton, F. B. Jr & Wilson, J. The Mississippi Katrina experience: applying lessons learned to augment daily operations in disaster preparation and management. South. Med. J. 106, 109–112 (2013).
DeVita, T., Brett-Major, D. & Katz, R. How are healthcare provider systems preparing for health emergency situations? World Med. Health Policy 14, 102–120 (2021).
Ebi, K. L. et al. Stress testing the capacity of health systems to manage climate change-related shocks and stresses. Int. J. Environ. Res. Public Health 15, 2370 (2018).
Achour, N. & Price, A. D. F. Resilience strategies of healthcare facilities: present and future. Int. J. Disaster Resil. Built Environ. 1, 264–276 (2010).
Jackson, R. & Shields, K. N. Preparing the US health community for climate change. Annu. Rev. Public Health 29, 57–73 (2008).
Wolf, T., Martinez, G. S., Cheong, H.-K., Williams, E. & Menne, B. Protecting health from climate change in the WHO European Region. Int. J. Environ. Res. Public Health 11, 6265–6280 (2014).
Frumkin, H., Hess, J., Luber, G., Malilay, J. & McGeehin, M. Climate change: the public health response. Am. J. Public Health 98, 435–445 (2008).
Corvalan, C. et al. Towards climate resilient and environmentally sustainable health care facilities. Int. J. Environ. Res. Public Health 17, 1–18 (2020).
Ebi, K. L. et al. Extreme weather and climate change: population health and health system implications. Annu. Rev. Public Health 42, 293–315 (2021).
Kirkpatrick, D. V. & Bryan, M. Hurricane emergency planning by home health providers serving the poor. J. Health Care Poor Underserved 18, 299–314 (2007).
Opoku, S. K., Leal Filho, W., Hubert, F. & Adejumo, O. Climate change and health preparedness in Africa: analysing trends in six African countries. Int. J. Environ. Res. Public Health 18, 4672 (2021).
Brevard, S. B. et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: lessons learned from a level I trauma center. J. Trauma 65, 1126–1132 (2008).
Allahbakhshi, K., Khorasani-Zavareh, D., Jazani, R. K. & Ghomian, Z. Preparedness components of health systems in the Eastern Mediterranean region for effective responses to dust and sand storms: a systematic review. F1000 Res. 10.12688%2Ff1000research.17543.1 (2019).
Han, B. A. & Drake, J. M. Future directions in analytics for infectious disease intelligence: toward an integrated warning system for emerging pathogens. EMBO Rep. 17, 785–789 (2016).
Geroy, L. S. A. & Pesigan, A. M. Disaster risk reduction for health facilities in the Western Pacific region. Int. J. Disaster Resil. 2, 268–277 (2011).
Hyogo Framework for Action 2005–2015: Building the Resilience of Nations and Communities to Disasters (International Strategy for Disaster Reduction, 2005).
Sendai framework for disaster risk reduction 2015–2030. UNDRR https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030 (2015).
Longden, T., Quilty, S., Haywood, P., Hunter, A. & Gruen, R. Heat-related mortality: an urgent need to recognise and record. Lancet Planet. Health 4, e171 (2020).
Let’s talk about the weather: injuries related to extreme weather. Australian Institute of Health and Welfare https://www.aihw.gov.au/reports/injury/extreme-weather-injuries/contents/about (2023).
Geiger, N., Gore, A., Squire, C. V. & Attari, S. Z. Investigating similarities and differences in individual reactions to the COVID-19 pandemic and the climate crisis. Clim. Change 167, 1 (2021).
Spence, A., Poortinga, W., Butler, C. & Pidgeon, N. F. Perceptions of climate change and willingness to save energy related to flood experience. Nat. Clim. Change 1, 46–49 (2011).
Bechtel, M. M. & Mannino, M. Ready when the big one comes? Natural disasters and mass support for preparedness investment. Polit. Behav. 45, 1045–1070 (2023).
Ecker, U. K. H. et al. Using the COVID-19 economic crisis to frame climate change as a secondary issue reduces mitigation support. J. Environ. Psychol. 70, 101464 (2020).
Morris, A. M., Ricci, K. A., Griffin, A. R., Heslin, K. C. & Dobalian, A. Personal and professional challenges confronted by hospital staff following hurricane Sandy: a qualitative assessment of management perspectives. BMC Emerg. Med. 16, 18 (2016).
Lawrence, J.-M., Ibne Hossain, N. U., Jaradat, R. & Hamilton, M. Leveraging a Bayesian network approach to model and analyze supplier vulnerability to severe weather risk: a case study of the US pharmaceutical supply chain following Hurricane Maria. Int. J. Disaster Risk Reduct. 49, 101607 (2020).
National health and climate strategy. Australian Government https://www.health.gov.au/resources/publications/national-health-and-climate-strategy (2023).
Fretheim, A., Oxman, A. D., Lavis, J. N. & Lewin, S. SUPPORT tools for evidence-informed policymaking in health 18: planning monitoring and evaluation of policies. Health Res. Policy Syst. 7, S18 (2009).
Judice, N. R. et al. Road Map for Implementing and Monitoring Policy and Advocacy Interventions (Health Policy Project, 2013).
Liese, B. H., Gribble, R. S. F. & Wickremsinhe, M. N. International funding for mental health: a review of the last decade. Int. Health 11, 361–369 (2019).
Drennan, V. M. & Ross, F. Global nurse shortages—the facts, the impact and action for change. Br. Med. Bull. 130, 25–37 (2019).
Langan, J. C., Lavin, R., Wolgast, K. A. & Veenema, T. G. Education for developing and sustaining a health care workforce for disaster readiness. Nurs. Adm. Q 41, 118–127 (2017).
van Oldenborgh, G. J. et al. Pathways and pitfalls in extreme event attribution. Clim. Change 166, 13 (2021).
Emergency preparedness, resilience and response (EPRR). NHS https://www.england.nhs.uk/ourwork/eprr/ (2023).
IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty Ch. SPM, 3–24 (IPCC, Cambridge Univ. Press, 2018); https://doi.org/10.1017/9781009157940.001
Jones, M. et al. Climate change and Australian rural health: five key lessons from Africa. Aust. J. Rural Health 30, 839–841 (2022).
Uttley, L. et al. The problems with systematic reviews: a living systematic review. J. Clin. Epidemiol. 156, 30–41 (2023).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101 (2006).
Zscheischler, J. et al. Future climate risk from compound events. Nat. Clim. Change 8, 469–477 (2018).
Romanello, M. et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 398, 1619–1662 (2021).
Berrang-Ford, L. et al. Systematic mapping of global research on climate and health: a machine learning review. Lancet Planet. Health 5, e514–e525 (2021).
Zurynski, Y. et al. How can the healthcare system deliver sustainable performance? A scoping review. BMJ Open 12, e059207 (2022).
Braithwaite, J. et al. Healthcare Systems: Future Predictions for Global Care (CRC Press, 2018).
What is the United Nations Framework Convention on Climate Change? United Nations Climate Change https://unfccc.int/process-and-meetings/what-is-the-united-nations-framework-convention-on-climate-change (2023).
Kapiriri, L. International validation of quality indicators for evaluating priority setting in low income countries: process and key lessons. BMC Health Serv. Res. 17, 418 (2017).
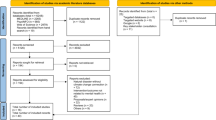
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br. Med. J. 372, n71 (2021).
Bevacqua, E. et al. Guidelines for studying diverse types of compound weather and climate events. Earth’s Future 9, e2021EF002340 (2021).
Hong, Q. N. et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ. Inform. 34, 285–291 (2018).
Baethge, C., Goldbeck-Wood, S. & Mertens, S. SANRA—a scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 4, 5 (2019).
Aromataris, E. et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 13, 132–140 (2015).
Tyndall, J. Authority, Accuracy, Coverage, Objectivity, Date, Significance (AACODS) Checklist (Flinders Univ., 2010).
Acknowledgements
Thanks to S. Wijekulasuriya and R. Patel for providing desktop support for the project. We also thank M. Simons, a Clinical Librarian at Macquarie University who we consulted to devise the search strategy. J.B., E.C. and J.W. report funding from the National Health and Medical Research Council (NHMRC) for the Partnership Centre for Health System Sustainability to support this work (grant ID 9100002). J.B., E.C. and J.W. are in receipt of NHMRC Leadership Fellowships (IG GNT1176620, IG GNT2008645 and IG GNT1174021, respectively). The agencies providing funding sources had no role in data collection, data analysis, data interpretation or writing of the report.
Author information
Authors and Affiliations
Contributions
J.B. conceived of the project and led the work. C.L.S. and Y.Z. co-conceived the project. L.E., E.L., G.D., C.L.S., A.C., K.B.-C. and E.M. screened the publications. E.L., G.D., K.B.-C., A.C., C.L.S. and E.M. extracted data from the publications and synthesized the findings from the review. J.B. directly accessed and verified the underlying data reported in the manuscript. J.B. drafted the manuscript with co-authorship from E.L., G.D., K.B.-C., A.C., C.L.S. and E.M. E.C., J.W. and Y.Z. made critical comments on the emerging draft. All authors critically reviewed the final manuscript and take responsibility for its accuracy and presentation.
Corresponding authors
Ethics declarations
Competing interests
J.B., E.C., J.W., Y.Z. and C.L.S. report grants from the NHMRC during the conduct of the review. J.B., E.C., J.W. and Y.Z. report multiple grants from a range of sources, which are all administered by the Macquarie University Research Office. C.L.S. reports a grant from Research Australia. J.B., E.C. and J.W. report financial support for travel from various conferences and invited keynote addresses. J.B. reports financial support for air travel from the International Society for Quality in Health Care. J.B. reports being the Chair of the Board of the International Society for Quality in Health Care and a member of various committees for the OECD and WHO (all unpaid roles). Y.Z. reports being a member of several governance committees such as Australian Health and Hospitals Association, The Deeble Institute for Policy Research and Rare Voices Australia (all unpaid roles). E.L., G.D., L.E., K.B.-C., A.C. and E.M. declare no competing interests.
Peer review
Peer review information
Nature Climate Change thanks Rachel Lookadoo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Included publications by year of publication, and trendline.
Results showing the number of publications by year, and the trend in publications. The graph includes publications between 1990 and May 2022, resulting in fewer publications identified in the final year.
Extended Data Fig. 2 Comparison of tropical cyclone-specific publications to other weather and disease-related publications by topic.
Number of tropical cyclone-specific publications (including hurricanes, typhoons, and tropical storms) discussing one or more of the seven topics identified from the full literature set compared to those discussing other climate-related impacts (for example, droughts, floods, heatwaves, vector-bone diseases). Filled bars represent tropical-cyclone specific publications. Unfilled indicates all other publications.
Extended Data Fig. 3 Percentage of publications covering key topics at each health system level.
Percentage of publications discussing identified topic areas from the included literature within a specific level of the health system (micro: ranging from the clinic or department level to whole hospital or facility level; meso: ranging from a local governance level to the provincial or state level; macro: at the whole-system, or at the national to global level).
Supplementary information
Supplementary Information
Supplementary Fig. 1, Tables 1–3, Information 1 and 2 and References.
Supplementary Data 1
Extracted data from included manuscripts (1A and 1B), reason for exclusion of studies at full-text review (1C) and risk of bias assessment and quality appraisal for included studies (1D–1G).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Braithwaite, J., Leask, E., Smith, C.L. et al. Analysing health system capacity and preparedness for climate change. Nat. Clim. Chang. (2024). https://doi.org/10.1038/s41558-024-01994-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41558-024-01994-4