Abstract
How cancer cells adapt to evade the therapeutic effects of drugs targeting oncogenic drivers is poorly understood. Here we report an epigenetic mechanism leading to the adaptive resistance of triple-negative breast cancer (TNBC) to fibroblast growth factor receptor (FGFR) inhibitors. Prolonged FGFR inhibition suppresses the function of BRG1-dependent chromatin remodelling, leading to an epigenetic state that derepresses YAP-associated enhancers. These chromatin changes induce the expression of several amino acid transporters, resulting in increased intracellular levels of specific amino acids that reactivate mTORC1. Consistent with this mechanism, addition of mTORC1 or YAP inhibitors to FGFR blockade synergistically attenuated the growth of TNBC patient-derived xenograft models. Collectively, these findings reveal a feedback loop involving an epigenetic state transition and metabolic reprogramming that leads to adaptive therapeutic resistance and provides potential therapeutic strategies to overcome this mechanism of resistance.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
CRISPR screen, RNA-seq, ATAC-seq and ChIP-seq data that support the findings of this study have been deposited in the Gene Expression Omnibus (GEO) under accession code GSE168027. Mass spectrometry data have been deposited in ProteomeXchange with the dataset identifier PXD028549. Unprocessed blots and statistical source data are presented within the paper. All other data supporting the findings of this study are available from the corresponding author on reasonable request. Source data are provided with this paper.
Code availability
We did not use any custom code or mathematical algorithm that is deemed central to the conclusions. All software and packages used are listed in the Reporting Summary and are publicly available.
References
Sanchez-Vega, F. et al. Oncogenic signaling pathways in the Cancer Genome Atlas. Cell 173, 321–337 (2018).
Lee, H. J. et al. Low prognostic implication of fibroblast growth factor family activation in triple-negative breast cancer subsets. Ann. Surg. Oncol. 21, 1561–1568 (2014).
Turner, N. et al. Integrative molecular profiling of triple negative breast cancers identifies amplicon drivers and potential therapeutic targets. Oncogene 29, 2013–2023 (2010).
Cheng, C. L. et al. Expression of FGFR1 is an independent prognostic factor in triple-negative breast cancer. Breast Cancer Res. Treat. 151, 99–111 (2015).
Priestley, P. et al. Pan-cancer whole-genome analyses of metastatic solid tumours. Nature 575, 210–216 (2019).
Sharpe, R. et al. FGFR signaling promotes the growth of triple-negative and basal-like breast cancer cell lines both in vitro and in vivo. Clin. Cancer Res. 17, 5275–5286 (2011).
Dey, J. H. et al. Targeting fibroblast growth factor receptors blocks PI3K/AKT signaling, induces apoptosis, and impairs mammary tumor outgrowth and metastasis. Cancer Res. 70, 4151–4162 (2010).
Liu, H. et al. Identifying and targeting sporadic oncogenic genetic aberrations in mouse models of triple-negative breast cancer. Cancer Discov. 8, 354–369 (2018).
Loriot, Y. et al. Erdafitinib in locally advanced or metastatic urothelial carcinoma. N. Engl. J. Med. 381, 338–348 (2019).
Abou-Alfa, G. K. et al. Pemigatinib for previously treated, locally advanced or metastatic cholangiocarcinoma: a multicentre, open-label, phase 2 study. Lancet Oncol. 21, 671–684 (2020).
Javle, M. M. et al. Final results from a phase II study of infigratinib (BGJ398), an FGFR-selective tyrosine kinase inhibitor, in patients with previously treated advanced cholangiocarcinoma harboring an FGFR2 gene fusion or rearrangement. J. Clin. Oncol. 39, 265–265 (2021).
Nogova, L. et al. Evaluation of BGJ398, a fibroblast growth factor receptor 1-3 kinase inhibitor, in patients with advanced solid tumors harboring genetic alterations in fibroblast growth factor receptors: results of a global phase I, dose-escalation and dose-expansion study. J. Clin. Oncol. 35, 157–165 (2017).
Tabernero, J. et al. Phase I dose-escalation study of JNJ-42756493, an oral pan-fibroblast growth factor receptor inhibitor, in patients with advanced solid tumors. J. Clin. Oncol. 33, 3401–3408 (2015).
Andre, F. et al. Targeting FGFR with dovitinib (TKI258): preclinical and clinical data in breast cancer. Clin. Cancer Res. 19, 3693–3702 (2013).
Guagnano, V. et al. FGFR genetic alterations predict for sensitivity to NVP-BGJ398, a selective pan-FGFR inhibitor. Cancer Discov. 2, 1118–1133 (2012).
Guagnano, V. et al. Discovery of 3-(2,6-dichloro-3,5-dimethoxy-phenyl)-1-{6-[4-(4-ethyl-piperazin-1-yl)-phenylamino]-pyrimidin-4-yl}-1-methyl-urea (NVP-BGJ398), a potent and selective inhibitor of the fibroblast growth factor receptor family of receptor tyrosine kinase. J. Med. Chem. 54, 7066–7083 (2011).
Xu, H. et al. Sequence determinants of improved CRISPR sgRNA design. Genome Res. 25, 1147–1157 (2015).
Li, W. et al. Quality control, modeling and visualization of CRISPR screens with MAGeCK-VISPR. Genome Biol. 16, 281 (2015).
McDonald, E. R. III et al. Project DRIVE: a compendium of cancer dependencies and synthetic lethal relationships uncovered by large-scale, deep RNAi screening. Cell 170, 577–592 (2017).
Pearson, A. et al. High-level clonal FGFR amplification and response to FGFR inhibition in a translational clinical trial. Cancer Discov. 6, 838–851 (2016).
Hsu, P. P. et al. The mTOR-regulated phosphoproteome reveals a mechanism of mTORC1-mediated inhibition of growth factor signaling. Science 332, 1317–1322 (2011).
Manning, B. D. & Toker, A. AKT/PKB signaling: navigating the network. Cell 169, 381–405 (2017).
Mendoza, M. C., Er, E. E. & Blenis, J. The Ras-ERK and PI3K-mTOR pathways: cross-talk and compensation. Trends Biochem. Sci. 36, 320–328 (2011).
Cordenonsi, M. et al. The hippo transducer TAZ confers cancer stem cell-related traits on breast cancer cells. Cell 147, 759–772 (2011).
Wang, Y. et al. Comprehensive molecular characterization of the hippo signaling pathway in cancer. Cell Rep. 25, 1304–1317 (2018).
Zanconato, F. et al. Transcriptional addiction in cancer cells is mediated by YAP/TAZ through BRD4. Nat. Med. 24, 1599–1610 (2018).
Goberdhan, D. C., Wilson, C. & Harris, A. L. Amino acid sensing by mTORC1: intracellular transporters mark the spot. Cell Metab. 23, 580–589 (2016).
Nicklin, P. et al. Bidirectional transport of amino acids regulates mTOR and autophagy. Cell 136, 521–534 (2009).
Shimobayashi, M. & Hall, M. N. Multiple amino acid sensing inputs to mTORC1. Cell Res. 26, 7–20 (2016).
Jewell, J. L. et al. Metabolism. Differential regulation of mTORC1 by leucine and glutamine. Science 347, 194–198 (2015).
Chantranupong, L. et al. The CASTOR proteins are arginine sensors for the mTORC1 pathway. Cell 165, 153–164 (2016).
Hara, K. et al. Amino acid sufficiency and mTOR regulate p70 S6 kinase and eIF-4E BP1 through a common effector mechanism. J. Biol. Chem. 273, 14484–14494 (1998).
Zheng, R. et al. Cistrome Data Browser: expanded datasets and new tools for gene regulatory analysis. Nucleic Acids Res. 47, D729–D735 (2019).
Heinz, S. et al. Simple combinations of lineage-determining transcription factors prime cis-regulatory elements required for macrophage and B cell identities. Mol. Cell 38, 576–589 (2010).
Turner, N. & Grose, R. Fibroblast growth factor signalling: from development to cancer. Nat. Rev. Cancer 10, 116–129 (2010).
Chang, L. et al. The SWI/SNF complex is a mechanoregulated inhibitor of YAP and TAZ. Nature 563, 265–269 (2018).
Schulte, M. L. et al. Pharmacological blockade of ASCT2-dependent glutamine transport leads to antitumor efficacy in preclinical models. Nat. Med. 24, 194–202 (2018).
Gao, H. et al. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat. Med. 21, 1318–1325 (2015).
Song, S. et al. A novel YAP1 inhibitor targets CSC-enriched radiation-resistant cells and exerts strong antitumor activity in esophageal adenocarcinoma. Mol. Cancer Ther. 17, 443–454 (2018).
Cassidy, J. W., Caldas, C. & Bruna, A. Maintaining tumor heterogeneity in patient-derived tumor xenografts. Cancer Res. 75, 2963–2968 (2015).
Zheng, G. X. et al. Massively parallel digital transcriptional profiling of single cells. Nat. Commun. 8, 14049 (2017).
Kandasamy, P., Gyimesi, G., Kanai, Y. & Hediger, M. A. Amino acid transporters revisited: new views in health and disease. Trends Biochem. Sci. 43, 752–789 (2018).
Park, Y. Y. et al. Yes-associated protein 1 and transcriptional coactivator with PDZ-binding motif activate the mammalian target of rapamycin complex 1 pathway by regulating amino acid transporters in hepatocellular carcinoma. Hepatology 63, 159–172 (2016).
Singleton, K. R. et al. Kinome RNAi screens reveal synergistic targeting of MTOR and FGFR1 pathways for treatment of lung cancer and HNSCC. Cancer Res. 75, 4398–4406 (2015).
Cai, W., Song, B. & Ai, H. Combined inhibition of FGFR and mTOR pathways is effective in suppressing ovarian cancer. Am. J. Transl. Res. 11, 1616–1625 (2019).
Cong, L. et al. Multiplex genome engineering using CRISPR/Cas systems. Science 339, 819–823 (2013).
Ianevski, A., He, L., Aittokallio, T. & Tang, J. SynergyFinder: a web application for analyzing drug combination dose-response matrix data. Bioinformatics 33, 2413–2415 (2017).
Weekes, M. P. et al. Quantitative temporal viromics: an approach to investigate host-pathogen interaction. Cell 157, 1460–1472 (2014).
McAlister, G. C. et al. MultiNotch MS3 enables accurate, sensitive, and multiplexed detection of differential expression across cancer cell line proteomes. Anal. Chem. 86, 7150–7158 (2014).
Cornwell, M. et al. VIPER: Visualization Pipeline for RNA-seq, a Snakemake workflow for efficient and complete RNA-seq analysis. BMC Bioinformatics 19, 135 (2018).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Trapnell, C. et al. Transcript assembly and quantification by RNA-seq reveals unannotated transcripts and isoform switching during cell differentiation. Nat. Biotechnol. 28, 511–515 (2010).
Wang, L., Wang, S. & Li, W. RSeQC: quality control of RNA-seq experiments. Bioinformatics 28, 2184–2185 (2012).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Yuan, M., Breitkopf, S. B., Yang, X. & Asara, J. M. A positive/negative ion-switching, targeted mass spectrometry-based metabolomics platform for bodily fluids, cells, and fresh and fixed tissue. Nat. Protoc. 7, 872–881 (2012).
Buenrostro, J. D., Wu, B., Chang, H. Y. & Greenleaf, W. J. ATAC-seq: a method for assaying chromatin accessibility genome-wide. Curr. Protoc. Mol. Biol. 109, 21.29.1–21.29.9 (2015).
Carroll, J. S. et al. Chromosome-wide mapping of estrogen receptor binding reveals long-range regulation requiring the forkhead protein FoxA1. Cell 122, 33–43 (2005).
Qin, Q. et al. ChiLin: a comprehensive ChIP-seq and DNase-seq quality control and analysis pipeline. BMC Bioinformatics 17, 404 (2016).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Zhang, Y. et al. Model-based analysis of ChIP-Seq (MACS). Genome Biol. 9, R137 (2008).
Qiu, X. et al. CoBRA: containerized bioinformatics workflow for reproducible ChIP/ATAC-seq analysis. Genomics Proteomics Bioinformatics https://doi.org/10.1016/j.gpb.2020.11.007 (2021).
Ramirez, F. et al. deepTools2: a next generation web server for deep-sequencing data analysis. Nucleic Acids Res. 44, W160–W165 (2016).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Manjunath, M. et al. ClusterEnG: an interactive educational web resource for clustering and visualizing high-dimensional data. PeerJ Comput. Sci. 4, e155 (2018).
Corces, M. R. et al. An improved ATAC-seq protocol reduces background and enables interrogation of frozen tissues. Nat. Methods 14, 959–962 (2017).
Acknowledgements
This work was supported by a grant from the Breast Cancer Research Foundation (BCRF-21-019) to M.B. and support from the Ludwig Center at Harvard to M.B and A.T. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. We thank members from the Brown and Liu laboratories for helpful discussions and technical help. We thank the Molecular Biology Core Facilities (MBCF) at the Dana–Farber Cancer Institute for help with next-generation sequencing. We thank S. Gygi and R. Rodrigues from Thermo Fisher Scientific Center for Multiplexed Proteomics at Harvard Medical School for multiplexed proteomic analysis.
Author information
Authors and Affiliations
Contributions
Y.L. and M.B. designed the experiment. Y.L., X.Q., X.W., H.L., R.C.G., T.X., A.F.-T., K.L., P.-L.K., A.J., R.V., P.C., K.L.J. and M.M. performed methodology, investigations and validation. Y.L., X.Q., R.C.G. and Y.X. performed software and formal analysis. K.-H.C., P.C., Q.-D.N., H.W.L., X.S.L., A.T. and M.B. provided resources and supervision. Y.L., X.Q., A.K.T., A.T. and M.B. wrote the manuscript. All authors read and corrected the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.B. is a consultant to Novartis. He receives sponsored research support from Novartis and serves on the scientific advisory boards of Kronos Bio, H3 Biomedicine and GV20 Oncotherapy. A.T. is a consultant for Oncologie and Medicxi and is on the scientific advisory board for Bertis. X.S.L. is a cofounder, board member, SAB member and consultant of GV20 Oncotherapy and its subsidiaries, a stockholder of BMY, TMO, WBA, ABT, ABBV and JNJ, and received research funding from Takeda, Sanofi, Bristol Myers Squibb and Novartis. The remaining authors declare no competing interests.
Additional information
Peer review information Nature Cell Biology thanks Paul Wade, Richard Grose and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 A genome-wide CRISPR knock out screen identifies genetic dependencies in FGFR-aberrant TNBC.
a, Left, immunoblot of FGFR1 and FGFR2 protein levels in indicated cell lines. Right, copy number variation (CNV) of indicated cell lines from Cancer Cell Line Encyclopedia (CCLE) dataset. b, Population doublings of CAL-120 cells treated with DMSO or 300 nM infigratinib for 35 days during genome-wide CRISPR screen. c, Gene ontology analysis for cluster 1 essential genes from Fig. 1c. The bar plots represent number of overlapped gene; the dots indicate FDR value. d, Principal-component analysis of essentiality scores in cluster 2 genes from Fig. 1c applied across 29 TNBC cell lines in the DepMap RNAi genetic dependency dataset. FGFR-aberrant TNBC cell lines are depicted in blue. e, GSEA normalized enrichment score (NES) of FGF signature for essential genes in the indicated cell line. f, Plot of significantly enriched hallmark gene sets based on essential genes in CAL-120 cells treated with infigratinib versus DMSO. g, Immunoblot of mTOR protein levels in MFM-223 cells after introduction of CRISPR guide RNAs targeting AAVS1 (control) or mTOR. h, The relative cell viability of CAL-120, Hs578T and MFM-223 cells harbouring CRISPR knock out of AAVS1 (control) or mTOR in presence of DMSO. Data were normalized to AAVS1 depleted condition (100%). n = 3 biological independent samples. Data are presented as mean ± s.d. i, The relative cell viability of MFM-223 cells in the presence of 50 nM, or 500 nM infigratinib for 6 days versus DMSO. MFM-223 cells were depleted of mTOR or AAVS1 (control) as indicated. Data were normalized to DMSO treated condition (100%). n = 3 biological independent samples. Data are presented as mean ± s.d. Statistics: unpaired, two-tailed t-test. **P = 0.0015, **P = 0.0013, **P = 0.0053 and **P = 0.007. j, Immunoblot of mTOR, RPTOR, RICTOR, TSC2 and GAPDH protein levels in CAL-120 cells expressing indicated shRNA. k, The relative viability of CAL-120 cells expressing shRNA targeting mTOR, RPTOR, RICTOR, TSC2 versus control in presence of DMSO or 1000 nM infigratinib for 6 days. Data were normalized to AAVS1 depleted condition (100%). n = 3 biological independent samples. Data are presented as mean ± s.d.
Extended Data Fig. 2 Role of mTORC1 signaling in adaptive resistance to FGFR inhibitors.
a, Immunoblot of FGFR2, ERK1/2, AKT, S6K, and S6 phosphorylation and total protein levels in MFM-223 cells treated with 50 nM infigratinib at the indicated time points. b, Immunoblot of FGFR1, ERK1/2, AKT, S6K, and S6 phosphorylation and total protein levels in CAL-120 cells treated with 300 nM dovitinib at the indicated time points. c, Immunoblot of FGFR1, S6K, S6, ERK1/2 and AKT phosphorylation and GAPDH protein levels in CAL-120 cells depleted with FGFR1 by shRNA at indicated time points. d, Tumor volumes of Hs578T mouse xenografts treated with vehicle or infigratinib for 35 days. n = 8 (vehicle), n = 10 (infigratinib). Data are presented as mean ± s.d. Statistics: unpaired, two-tailed t-test, ***P = 0.001. e, Relative cell viability of CAL-120 cells treated with 1000 nM infigratinib alone or in combination with 500 nM MK2206 or 200 nM trametinib for 6 days. Data were normalized to DMSO treated condition (100%). n = 3 biological independent samples. Data are presented as mean ± s.d. f, Bliss synergy model of combination infigratinib and everolimus treatment in MFM-223 cells. g, Relative cell viability of CAL-120 cells treated with infigratinib in a dose-dependent manner alone or in combination with 5 nM rapalink-1 for 6 days. n = 3 biological independent samples. Data are presented as mean ± s.d.
Extended Data Fig. 3 Increased expression of YAP target genes and amino acid transporters are driven by FGFR inhibition.
Heatmap of protein expression levels detected by multiplexed proteomics in CAL-120 cells upon DMSO, 1d, or 12d of 300 nM infigratinib treatment. Rows are clustered by k-means analysis. b, GSEA analysis reveals a YAP signature is significantly enriched in genes and proteins differentially regulated by 12d of infigratinib treatment in CAL-120 cells. c, Normalized RNA-seq reads counts (RPKM) of VPS34, MAP4K3, Rag family of GTPases and PLD1 in CAL-120 cells treated with DMSO or infigratinib for 12 days. n = 3 biological independent samples. Data are presented as mean ± s.d. d, Immunoblot of S6K phosphorylation and total protein levels in CAL-120 cells treated with DMSO or infigratinib (300 nM) at indicated time points, cultured in full medium (AA + ), amino acid-free medium (AA-), or amino acid-free medium containing glutamine, leucine, and arginine (Gln/Leu/Arg) for 6 hours.
Extended Data Fig. 4 FGFR inhibition regulates enhancer landscape in TNBC cells.
a, MA plot of differentially regulated H3K27ac ChIP-seq peaks in CAL-120 cells treated with 12d infigratinib versus DMSO. Mean of normalized counts of each peak are plotted on the x-axis and log2 fold changes of differential peaks are plotted on the y-axis. Significantly changed peaks (FDR < 0.05) are marked in red. b, Heatmaps of ATAC-seq, H3K27ac and YAP ChIP-seq signals at regions of decreased chromatin accessibility (FDR < 0.01, Log2 fold change < -1.5, n = 2798) upon 12d infigratinib treatment. c, Genomic distribution of regions of increased chromatin accessibility upon 12d infigratinib treatment. d, Venn diagram depicting overlap between H3K27ac peaks (green) and YAP (blue) DNA binding peaks after 12d infigratinib treatment. e, YAP (blue) and H3k27ac (green) ChIP-seq tracks around YAP target gene FSTL1 in CAL120 cells in the presence of DMSO or infigratinib at indicated time points.
Extended Data Fig. 5 Infigratinib treatment decreases BRG1 chromatin binding and mediates enhancer reactivation.
a, Representative confocal images of YAP (green) subcellular localization and DAPI (blue) in presence with DMSO or 300 nM infigratinib for 8 days. b, Immunoblot of YAP phosphorylation and total protein levels in CAL-120 cells treated with 300 nM infigratinib at the indicated time points. c, Plot of similarity (GIGGLE score) between published binding profiles of chromatin binding factors and regions of increased chromatin accessibility in CAL-120 cells upon 12d infigratinib treatment. SWI/SNF subunits are marked by *. d, MA plot of differential BRG1 ChIP-seq signals in CAL-120 cells treated with 48 h infigratinib versus DMSO. Mean of normalized counts of each peak are plotted on the x-axis and log2 fold changes of peaks are plotted on the y-axis. Significantly changed peaks (FDR < 0.05) are marked in red. e, MA plot of differential H3K27ac ChIP-seq signals in CAL-120 cells depleted of BRG1 versus AAVS1 (control). Significantly changed peaks (FDR < 0.05) are marked in red. f, Venn diagram illustrating the overlap in the nearby gene to lost BRG1 binding sites upon 48 h FGFR inhibition from Extended Data Fig. 5d and nearby gene to gained H3K27ac signal after BRG1 depletion from Fig. 5f. g, RNA-seq analysis of RNA expression levels of the SLC7A5, SLC1A5 and SLC3A2 in CAL-120 cells depleted with AAVS1 (control) or BRG1. n = 3 biological independent samples. Data are presented as mean ± s.d.
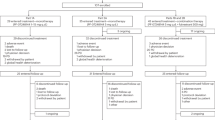
Extended Data Fig. 6 Combinatorial strategies for treating FGFR-aberrant patient-derived mouse xenografts.
a, Growth curve of CAL-120 cells treated with DMSO, 1000 nM infigratinib, 10 μM V-9302 or in combinations at the indicated time points. n = 3 biological independent samples. Data are presented as mean ± s.d. Statistics: two-way analysis of variance (ANOVA). ****P < 0.0001 for infigratinib versus infigratinib +V9302. b, Immunoblot of S6K phosphorylation levels in CAL-120 cells treated with DMSO or infigratinib for 6 days, including the combination of V-9302. c, Immunoblot of S6K phosphorylation, YAP and GAPDH protein levels in CAL-120 cells depleted with CRISPR guide RNAs targeting AAVS1 (control) or YAP, and treated with DMSO or infigratinib for 6 days as indicated. d, RT-qPCR analysis of RNA expression levels of indicated amino acid transporters in CAL-120 cells depleted with AAVS1 (control) or YAP in the presence of DMSO or infigratinib for 6 days. n = 3 biological independent samples. Data are presented as mean ± s.d. e, Growth curve of CAL-120 cells depleted with YAP or AAVS1 (control) in the presence or absence of 1000 nM infigratinib at the indicated time points. n = 3 biological independent samples. n = 3 biological independent samples. Data are presented as mean ± s.d. statistics: two-way analysis of variance (ANOVA), ****P < 0.0001 for YAP depletion versus control in presence of infigratinib f, Genetic alteration and relative mRNA expression of FGFR1-3 in FGFR-aberrant PDX models from Fig. 6a. The orange line indicates the cut off between sensitive and resistant tumors. g, Kaplan–Meier curves of NIBRX5249 tumors progression (doubling) time. Tumors were treated with vehicle control, 12.5 mg/kg infigratinib, 0.5 mg/kg everolimus, 1 mg/kg CA3 or in combination as indicated. Statistics: Log-rank test. **P = 0.0029 for vehicle versus infigratinib +everolimus. h, Kaplan–Meier curves of NIBRX6047 tumors progression (doubling) time. Tumors were treated with vehicle control, 12.5 mg/kg infigratinib, 0.5 mg/kg everolimus, 1 mg/kg CA3 or in combination as indicated. Statistics: Log-rank test. **P = 0.0014 for vehicle versus infigratinib +everolimus. ***P = 0.0006 for vehicle versus infigratinib +CA3. i and j, Relative body weights of NIBRX-5249 (i) and NIBRX-6047 (j) implanted mice from Fig. 6b and d, respectively. Data are presented as mean ± s.d.
Extended Data Fig. 7 Single cell profiling of chromatin accessibility in the NIBRX-5249 PDX model.
a, Quality control (QC) of scATAC-seq analysis in NIBRX-5249 PDX tumors treated with vehicle control or 12.5 mg/kg infigratinib from Fig. 6b. b, t-SNE plot showing cell clustering by sequencing depth. c, k-means clustering of cells from NIBRX-5249 PDX tumors treated with vehicle (left) or infigratinib (right) in t-SNE projection space. d, GSEA analysis reveals the YAP target gene signature is significantly enriched in NIBRX-5249 PDX treated with infigratinib versus vehicle. e, Heatmap represents relative mRNA expression levels of SLC7A5, SLC1A5 and SLC3A2 in NIBRX-5249 PDX samples treated with vehicle control, 12.5 mg/kg infigratinib, 1 mg/kg CA3 or in combination as indicated for 20 days.
Supplementary information
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 1
Unprocessed western blots.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 2
Unprocessed western blots.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 3
Unprocessed western blots.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Unprocessed western blots.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 1
Unprocessed western blots.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 2
Unprocessed western blots.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 3
Unprocessed western blots.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 5
Unprocessed western blots.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 6
Unprocessed western blots.
Rights and permissions
About this article
Cite this article
Li, Y., Qiu, X., Wang, X. et al. FGFR-inhibitor-mediated dismissal of SWI/SNF complexes from YAP-dependent enhancers induces adaptive therapeutic resistance. Nat Cell Biol 23, 1187–1198 (2021). https://doi.org/10.1038/s41556-021-00781-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41556-021-00781-z
This article is cited by
-
Super-enhancer RNA m6A promotes local chromatin accessibility and oncogene transcription in pancreatic ductal adenocarcinoma
Nature Genetics (2023)
-
RNF40 epigenetically modulates glycolysis to support the aggressiveness of basal-like breast cancer
Cell Death & Disease (2023)
-
Combined blockade of mTOR and p21-activated kinases pathways prevents tumour growth in KRAS-mutated colorectal cancer
British Journal of Cancer (2023)
-
Insights into recent findings and clinical application of YAP and TAZ in cancer
Nature Reviews Cancer (2023)
-
Discovery of a small molecule ligand of FRS2 that inhibits invasion and tumor growth
Cellular Oncology (2023)