Abstract
mRNA-based vaccines have been used globally to eradicate the coronavirus-disease 2019 (COVID-19) pandemic. Vaccine efficacy and adverse reactions depend on immune responses, such as proinflammatory cytokine production and lymphocyte activation. We conducted a prospective cohort study to investigate relationships among specific antibody titers, adverse reactions, proinflammatory cytokine production, and immune-regulatory microRNA (miRNA) levels in serum extracellular vesicles (EVs) after COVID-19 vaccination (BNT162b2). Local adverse reactions after the second dose, such as local pain and swelling, were less correlated with those of systemic symptoms, such as fever and muscle pain, whereas serum TNF-α levels were associated with systemic adverse reactions and with specific antibody titers. Interestingly, EV miR-92a-2-5p levels in sera were negatively correlated with degrees of adverse reactions, and EV miR-148a levels were associated with specific antibody titers. Our data suggest a potential of circulating EV miRNAs as biomarkers for vaccine efficacy and adverse reactions.
Similar content being viewed by others
Introduction
Vaccination is the best prophylaxis to prevent infectious diseases, and vaccines comprise antigens and adjuvants. Adjuvants elicit innate immune responses, such as proinflammatory cytokine production and dendritic cell maturation, required for activating adaptive immune responses, leading to antigen-specific antibody production1. Aluminum salts have been used as adjuvants in many types of vaccines2,3,4, and ligands for pattern-recognition receptors, such as toll-like receptors, are also used as adjuvants5. However, even in the absence of those molecules, components of the vaccine itself could function as adjuvants. For instance, viral RNAs within the whole-virus vaccine of influenza-A virus activate TLR7, thereby evoking innate immune responses, including proinflammatory cytokine production6.
Although vaccine-induced adverse reaction itself is not serious in many cases, fears of adverse reactions sometimes drop the vaccination rate, resulting in insufficient eradication of infectious diseases, such as human papillomavirus-induced cervical cancers7. Thus, appropriate understanding of the mechanism underlying adverse reactions is important to dispel the fear. A well-known adverse reaction is anaphylaxis, which is a type-I hypersensitivity, with a sufficiently established mechanism and treatment regimen8,9. Other adverse reactions, such as fever, local pain, swelling, and redness, are supposed to be caused by proinflammatory cytokine and lipid mediators10,11,12,13,14. Moreover, it has been shown that systemic proinflammatory cytokine is a cause of those adverse reactions after seasonal flu vaccination15.
Extracellular vesicles (EVs), including exosomes and microvesicles, are enriched in the blood, and contain functional proteins and RNAs, delivering them from donor to recipient cells16,17. MicroRNAs (miRNAs) target mRNAs and regulate their translation18,19,20. EVs contain immune-regulatory miRNAs, and EV miRNAs have been shown to regulate host innate and adaptive immune responses21. Previously, we found that miR-451a levels in serum EVs were weakly associated with adverse reactions after seasonal flu vaccination14,22.
SARS-CoV-2 causes the coronavirus-disease 2019 (COVID-19) pandemic in 202023,24, and several COVID-19 vaccines have been approved and used worldwide to eradicate the coronavirus disease. BNT162b2 (Pfizer) is a COVID-19 vaccine that contains mRNA-encoding viral spike proteins25. It has been reported that after vaccination with BNT162b2, there are several adverse reactions, such as local pain, redness, swelling, fever, fatigue, and muscle pain25, which are supposed to be caused by immune responses. However, it remains unknown whether these adverse reactions are associated with proinflammatory cytokines and EV miRNAs. Additionally, whether the viral spike-protein-specific antibody production is related to the severity of adverse reactions, proinflammatory cytokine, and miRNA levels is unclear. To investigate the correlations among these factors, we conducted a prospective cohort study with BNT162b2.
Results
Demographic characteristics and vaccination data
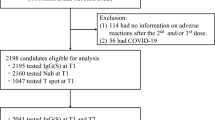
Between March and June 2021, 61 persons were enrolled and received two doses of BNT162b2 as shown in Fig. 1a and b. The demographic characteristics of study samples are shown in Fig. 1c. The gender ratio is almost 1:1 (1.18 male to female), and all the participants are of Asian ethnicity, 45.9% of the population aged 30–39 years, and 18% of participants are more than 50 years old. All participants were healthy or had stable medical conditions and received two doses of BNT162b2 (Pfizer) (Fig. 1c). Sera were collected from 61 subjects before and after the first dose and from 24 subjects after the second dose (Fig. 1a and b). No one had severe adverse events such as death, hemorrhagic stroke, and myocardial infarction after vaccination.
Local and systemic adverse reactions after COVID-19 vaccination
First, we collected the degree of local and systemic symptoms from 61 subjects after the first and second doses, as indicated in Fig. 1. Almost all subjects had local pain at injection sites after the first and second doses. The degrees of other adverse reactions were more severe after the second dose than those after the first dose (Fig. 2a, b), which was consistent with a previous report25. Comparing the level of each symptom, all subjects were classified into two groups: one group has no or mild local pain, and the other has a more severe local-pain symptom. After the first dose, the group with severe local pain has more severe swelling, redness, fatigue, headache, muscle pain, and joint pain (Fig. 2c and Supplementary table 1). By contrast, the differences in the degree of fever or muscle pain after the second dose were relatively marginal between the two groups, although swelling was more severe in subjects with severe local pain (Fig. 2d and Supplementary table 1).
a, b Data on local and systemic symptoms of 61 patients within 1 week after the first (a) and second (b) doses were collected as described in the “Methods”. The data are shown as percentages of the degree of each symptom (n = 61). c, d Subjects were classified into two groups, ≦mild (no or mild local pain) and ≧moderate (mild, severe, and grade-4 local pain), and percentages of each symptom degree are shown. e–g Degrees of each symptom were scored as no (0), mild (1), moderate (2), severe (3), and grade 4 (4), and p-values of the correlation coefficient of scores between two symptoms after the first dose (e), after the second dose (f), and after the first and second doses (g) were calculated. P-values are shown as heat maps. Red color represents statistical significance (p < 0.05).
To further investigate the relationship among each symptom, the degree of each adverse reaction was scored from 0 to 4, according to the severity, such as none = 0, mild = 1, moderate = 2, severe = 3, and grade 4 = 4. We calculated the statistical significance (p-values) of correlations of each pair of adverse reactions. Additionally, local and systemic scores were defined as sums of scores of local and systemic symptoms, respectively.
Interestingly, a heatmap of the p-values of correlation of two symptoms suggested that scores of adverse reactions were roughly correlated with each other after the first dose (Fig. 2e). However, after the second dose, scores of local adverse reactions were not related to those of the systemic adverse reactions, such as fever, chills, muscle pain, and joint pain (Fig. 2f). By contrast, the systemic symptoms, such as fever, fatigue, and muscle pain, were correlated with each other after the second dose (Fig. 2f).
We also found that scores of the local symptoms were roughly correlated between the first and second doses (9 blocks on the upper left in Fig. 2g), but those of systemic symptoms were not (blocks on the lower right in Fig. 2g), implying that the systemic symptoms after the second dose are not associated with the local symptoms. To further elucidate this point, we compared local and systemic scores. The coefficient of determination between local and systemic scores after the second dose was below 0.2 (Supplementary Fig. 1). By contrast, the coefficient of determination between the local and systemic scores after the first dose was above 0.2 (R2 = 0.26), suggesting a weak correlation (Supplementary Fig. 1). These data also suggest that systemic symptoms after the second dose are not associated with local symptoms. Moreover, we found that coefficients of determination between local scores after the first and second doses were above 0.2 (R2 = 0.36) (Supplementary Fig. 1).
Subjects with antipyretic medication had more severe local and systemic symptoms than those without it (Supplementary Fig. 2), which is consistent with the assumption that subjects with severe symptoms would take an antipyretic medication.
IL-6 and TNF-α levels in sera after vaccination
It is previously reported that the production of proinflammatory cytokines after vaccination is associated with adverse reactions15,26, and thus, we measured serum proinflammatory cytokine levels. IL-6 levels 1 day after the first dose were elevated compared with the levels before vaccination, and the levels were further elevated after the second dose (Fig. 3a). Serum TNF-α levels did not increase after the first dose but increased significantly after the second dose (Fig. 3b). Although there was no correlation between IL-6 and TNF-α levels before vaccination (Fig. 3c), there were moderate correlations between serum IL-6 and TNF-α levels after the first and second doses (Fig. 3d and e). These data suggest that proinflammatory cytokines were produced in response to BNT162b2 vaccination, especially after the second dose.
a, b Sera were collected before (pre) and after the first and second doses (days 1, 2, or 3). Serum IL-6 (a) and TNF-α (b) protein levels were determined by ELISA. Paired t-test (pre and post 1 day) and one-way ANOVA (each right panel) were performed (*p < 0.05). The bars represent mean ± standard deviation (SD). c–e Correlation between IL-6 and TNF-α protein levels at pre (c), 1 day after the first dose, and 1 day after the second dose (e) was investigated. The coefficient of determination (R2) and p-values were calculated (Pearson correlation test, *p < 0.05). Each dot represents a subject.
Next, we investigated the correlation between proinflammatory cytokine levels and adverse reactions after vaccination. We chose serum samples collected at 1 day post vaccination for comparison, because cytokine levels exhibited a trend to decrease within a few days (Fig. 3). After the first dose, we could not observe any significant correlation between proinflammatory cytokine levels and adverse reaction scores (Fig. 4a and b). Although local scores after the second dose were not correlated with either IL-6 or TNF-α level in sera, systemic scores were correlated with serum TNF-α levels after the second dose (Fig. 4c and d). This is consistent with the notion that proinflammatory cytokine is a cause of adverse reactions after vaccination26.
a, b Local and systemic scores were compared with serum IL-6 (a) and TNF-α (b) levels 1 day after the first dose. There were no correlations. c, d Local and systemic scores were compared with serum IL-6 (c) and TNF-α (d) levels 1 day after the second dose. The coefficient of determination (R2) and p-values were calculated (Pearson correlation test, *p < 0.05). Each dot represents a subject.
TNF-α in serum is correlated with the vaccine efficacy
Next, we determined SARS-CoV-2 spike-protein-specific antibody levels in sera (Fig. 5a), and investigated whether proinflammatory cytokine levels were associated with specific antibody levels. We confirmed that treatment with an antipyretic medication did not reduce specific antibody titers, but the titers were higher in the subjects with treatment than in those without it (Supplementary Fig. 3).
a Anti-spike-protein antibody titers in sera at 35 days after the first dose were determined via ELISA. b, c Specific antibody titers were compared with serum IL-6 and TNF-α levels 1 day after the first (b) and second (c) doses. d, e Specific antibody titers were compared with local and systemic scores after the first (d) or second (e) doses. The coefficient of determination and p-values of correlation were calculated (Pearson correlation test, *p < 0.05). Each dot represents a subject.
Serum IL-6 and TNF-α levels after the first dose were not correlated with S-protein-specific antibody titers (Fig. 5b), but serum TNF-α levels after the second dose were associated with specific antibody titers (Fig. 5c).
We next investigated the correlations between adverse reactions and specific antibody titers. Local scores after the first and second doses were not correlated with specific antibody titers (Fig. 5d and e), but systemic scores after the second dose were associated with specific antibody titers (Fig. 5e). These observations are consistent with the notion that adverse reactions and proinflammatory cytokine production are caused by immune responses to antigens, leading to production of antigen-specific antibody production.
Circulating EV microRNAs associated with immune responses
Since we had previously found that serum EV miRNA levels before vaccination were associated with adverse reactions after seasonal flu vaccination14, we measured several miRNA levels in serum EVs by RT-qPCR and compared them with local and systemic scores. The size and concentration of collected serum EVs are shown in Supplementary Fig. 4a. On the basis of previous reports14,27,28,29,30,31, we focused on 16 immune-regulatory microRNAs (Fig. 6a). miRNA levels in serum EVs were normalized to miR-16 levels, because we have previously found that miR-16 is suitable to normalize miRNA levels in human serum EVs rather than U6 RNA22. We have also found that miRNA levels normalized to miR-16 were correlated to cytokine expression in response to components of influenza vaccines14,22. Additionally, we confirmed that U6/miR-16 ratio in EVs released from macrophage cell line was not affected by stimulation with poly I:C, dsRNA analog, suggesting that miR-16 levels in EVs are stable as U6 levels are (Supplementary Fig. 4b). Interestingly, multiple-regression analysis suggested that miR-92a-2-5p levels in serum EVs 1 day before the first dose were negatively correlated with local scores after the first and second doses, and also correlated with systemic scores after the second dose (Fig. 6b–e). Additionally, miR-148a levels were positively correlated with systemic scores after the first dose (Fig. 6c). Unlike seasonal flu vaccination, miR-451a levels were not connected with any scores (Fig. 6b–e). Since EV miR-92a-2-5p levels were correlated with local and systemic scores, we investigated which symptoms were associated with miR-92a-2a-5p. Our statistical analyses suggested that miR-92a-2-5p levels in serum EVs were significantly decreased in subjects who had redness, headache, or joint-pain symptoms (Fig. 6f). Systemic scores of females were higher than those of males, but there was no difference in miR-92a-2-5p levels between females and males (Supplementary Fig. 5a, b), suggesting that miR-92a-2-5p is not associated with gender difference.
a EV miRNA levels in sera collected at 1 day before the first dose were determined by RT-qPCR. The heatmap represents the ln (miRNA) values of each miRNA. b–e Local and systemic scores after the first (b, c) and second (d, e) doses were compared with ln (miR) levels. Multiple linear-regression analyses were performed, and multiple coefficients of determination (R2) were calculated. The tables show coefficient (β), standard error (SE), and p-values of each ln (miR). f All subjects were classified into two groups on the basis of the degree of each symptom as indicated. Ln (miR-92a-2-5p) levels in the two groups were compared. Student t-tests were performed (*p < 0.05). The bars represent mean ± SD. Each dot represents a subject.
Subsequently, we compared miRNA levels with specific antibody titers. Multiple-regression analysis suggests the relationships of the level of miR-132, miR-148a, miR-221, and miR-625-3p with the antibody titers (Fig. 7a), whereas other miRNA levels were not connected with the antibody titers. To further investigate correlations between each miRNA and the antibody titers, we compared miRNA levels between the groups with high and low specific antibody titers. Interestingly, we found that miR-148a levels were significantly lower in the group with high antibody titers (Fig. 7b). Next, we performed multiple-regression analysis to compare the cytokine levels with serum EV miRNAs. miR-126 and miR-451 were connected to TNF-α levels after the first dose (Fig. 7c). Since TNF-α was not induced after the first dose, it is expected that TNF-α levels after the first dose reflect only basal TNF-α levels. No miRNAs were connected to TNF-α and IL-6 levels after the second dose (Fig. 7d). Collectively, our data imply that miR-92a-2-5p and miR-148a are expected to be associated with immune responses after vaccination with BNT162b2.
a Correlation between ln (miRNA) levels and specific antibody titers was investigated via multiple-regression analysis. Multiple coefficients of determination (R2) were calculated. The table shows the coefficient (β), standard error (SE), and p-values of each ln (miR). b ln (miR-132), ln (miR-148a), ln (miR-221), and ln (miR-625-3p) levels were compared between a group with a high specific antibody titer (top 20%) and that with a low level (bottom 20%). Each dot represents a subject (*p < 0.05, t-test). The bars represent mean ± SD. c, d Correlation between ln (miRNA) levels and cytokine levels 1 day after the first (c) or second (d) doses was investigated by multiple linear-regression analysis. Multiple coefficients of determination (R2) were calculated. The tables show coefficient (β), standard error (SE), and p-values of each ln (miR).
Discussion
Adverse reactions of vaccines are thought to be caused by immune responses, and previous studies have shown that proinflammatory cytokine production is a cause of those adverse reactions10,11,12,13. This study investigated the correlation between proinflammatory cytokine levels in sera and adverse reactions after COVID-19 vaccination, and found that systemic TNF-α levels were connected with the systemic scores after the second dose. This observation also supports the notion that proinflammatory cytokine is a cause of adverse reactions after vaccination. Although we could not find significant correlation between the cytokine levels and local adverse reactions, it is possible that cytokine levels at the injection site were different from those in sera. Another possibility is that other cytokines and lipid mediators, such as prostaglandins, caused local symptoms, such as local pain, swelling, and redness at the vaccination site. However, further analyses must reveal the underlying mechanisms of adverse reactions.
Interestingly, the degrees of systemic symptoms were largely unrelated to local symptoms after the second dose. These data imply that factors causing local adverse reactions would be different from those causing systemic symptoms. Since innate immunity is expected to be activated in response to the components of vaccines at the vaccination site, local symptoms after the first and second doses might reflect the innate immune response, and thus, systemic symptoms after the second doses are expected to be caused by an adaptive immune response, such as T-cell-mediated proinflammatory cytokines.
Our study showed a correlation of specific antibody titers with serum TNF-α levels after the second dose. TNF-α has been reported to be required for the formation of primary B-cell follicles and essential for the production of antigen-specific IgG32. Recombinant TNF-α can also promote B-cell proliferation33. TNF-α is secreted from myeloid cells and B- and T cells in response to antigens34. Hence, TNF-α is expected to be secreted from lymphocytes in response to vaccination, resulting in augmented production of specific antibodies against the viral spike protein.
Previous studies have shown that circulating EV miRNAs regulate immune responses after vaccination. We have reported that miR-451 and miR-192 in EVs regulate proinflammatory cytokine expression in response to seasonal flu vaccine14,22,27. Unlike our expectation, we could not find any association of these miRNAs with local and systemic symptoms in this cohort study. It is possible that miR-451a and miR-192 might not be involved in immune responses caused by vaccination with BNT162b2. By contrast, we found that miR-92a-2-5p levels were negatively correlated with local and systemic scores, and miR-148a was associated with production of specific antibodies. These data suggest that miR-92a-2-5p and miR-148a are involved in immune responses to components of BNT162b2.
miR-92a-2-5p has been identified as a biomarker for small-cell lung cancer35,36, and later studies suggested that it targeted TLR2 and suppresses TLR-2-mediated liver fibrosis37. Our previous microarray analysis showed that miR-92a-2-5p was a miRNA highly expressed in serum EVs of subjects14. Although the role of miR-92a-2-5p in the immune response after vaccination remains unclear, we prefer the interpretation that miR-92a-2-5p might reflect some unknown physical condition related to immune responses. Furthermore, miR-148a was associated with specific antibody production. miR-148a negatively regulates innate immune response and antigen presentation by dendritic cells38. Considering that dendritic cells play crucial roles in priming naive T cells required for B-cell activation, leading to antibody production, it is expected that miR-148a would regulate dendritic cell function, thereby affecting the levels of specific antibodies after vaccination.
Interestingly, miR-126, miR-132, miR-221, and miR-625-3p were also connected with the antibody titers or serum-cytokine levels after vaccination in our regression analyses. miR-126 inhibits VCAM-1 expression in endothelial cells, thereby reducing leukocyte adherence to endothelial cells29, and miR-126 is known to be increased in sepsis39. miR-126-5p, which is produced from the same pre-miR-126 RNA as miR-126 is, binds to capsase-3 and prevents dimerization of the caspase40. Thus, miR-126-5p inhibits the caspase activity to limit apoptosis in endothelial cells40. Because endothelial cells are a source of EVs41, it is interesting to investigate whether miR-126-5p is concomitantly expressed with miR-126 and whether miR-126 and miR-126-5p affect the production of miRNA-containing EVs and immune responses after vaccination. miR-132 targets SOX4 in B cells required for B-cell development30, and miR-221 regulates redirection of precursor B cells to bone marrow42. But, it is still unclear whether these miRNAs are involved in immune responses after vaccination. Recent studies elucidated miRNAs related to SARS-CoV-243,44,45. Functional analyses of these miRNAs are important to reveal the role of the miRNAs in immune responses after vaccination.
EVs include exosomes, microvesicles (also called ectosomes), and apoptotic bodies. Recent studies have shown that not only exosomes but also other vesicles deliver miRNAs to other cells18,19,20. Our nanoparticle-tracking analysis showed that most of isolated particles were smaller than 100 nm, although a part of particles was larger than 100 nm. It is possible that specific types of EVs contain miRNAs related to immune responses. Further studies are required to fully reveal the function of EVs in immune responses after vaccination.
In this study, we found several immune-regulatory miRNAs associated with a part of immune responses after COVID-19, including antibody titers and adverse reactions. miRNAs have been identified as biomarkers for several diseases. Alternatively, miRNAs in EVs have been reported to regulate immune responses. Most of the adverse reactions are not serious, however, fears against adverse reactions drop vaccination rate, and thus prevent herd immunity. Further studies on miRNAs are expected to identify new biomarkers to predict preventive effects and adverse reactions of vaccines, leading to an understanding of the mechanism underlying individual differences in the responses after vaccination.
Methods
Participants
Between March 2021 and June 2021, 61 participants, mainly including the staff and faculty members in Kumamoto University and its hospital, were recruited. Those with unstable-disease conditions or symptoms were not recruited to this study. All participants provided written informed consent. In total, 24 subjects agreed with the blood sampling after the second dose. Antipyretic medicines (Tylenol A) were handed to all participants, and they took the medicines if it was needed. All participants gave written informed consent prior to participation. The ethics committee of the Faculty of Life Science at Kumamoto University approved this study (RINRI 1524), and all experiments have been conducted according to the principles expressed in the Declaration of Helsinki.
EV isolation and microRNA qPCR
According to the manufacturer’s protocol, EVs in serum were collected using a Total Exosome Isolation Kit (from serum, Thermo Fisher). Total RNA in EVs was extracted using the TRI reagent (MOR). miRNAs were reverse-transcribed using MirX miRNA First-Standard Synthesis Kit (Clontech). Quantitative PCR was conducted using Power SYBR Green Master Mix (Thermo Fisher) on Step One Real-Time PCR System (ABI). The levels of each miRNA are measured twice and its value was averaged. Expression of each miRNA was normalized to miR-16 expression using the comparative 2[−ΔΔCt] method. Primer sequences used for quantitative PCR analyses were listed in Supplementary Table 2.
Vaccine data and the scores of subjective symptoms
Participants were vaccinated with two 30 μg doses of BNT162b2 (Pfizer), containing nucleoside-modified RNA encoding the SARS-CoV-2 full-length spike, apart from 21 days, except for two people (they are 34 days apart). Subjective symptoms were counted on the basis of a questionnaire completed by the subjects within 7 days of each vaccination. The questionnaire inquired about the degrees of each symptom, such as local pain, swelling and redness at the injection site or fever, fatigue, headache, chills, muscle pain, joint pain, vomiting, and diarrhea. Degrees of symptoms were classified according to a previous report25, and were scored as follows: none, 0; mild, 1; moderate, 2; severe, 3; and grade 4, 4. Local scores were determined as the sum of scores of local pain, swelling, and redness. Systemic scores were defined as the sum of scores of the degrees of fever, headache, chills, muscle pain, joint pain, vomiting, and diarrhea.
ELISA
The levels of IL-6 and TNF-α in serum were analyzed at before vaccination, and post day 1, day 2, or day 3 after vaccination using a Quantikine HS ELISA human IL-6 (HS600C) or TNF-a (HSTA00E) immunoassay kit (R & D system) according to the manufacturer’s protocol. The levels of antibody against SARS-CoV-2 spike protein were analyzed at 14 days after the second dose using Human SARS-CoV-2 Spike (Trimer) Ig Total ELISA kit (Thermo Fisher) according to the manufacturer’s protocol. A few subjects exhibited too high basal IL-6 levels in sera, and thus their data could not be determined via ELISA. Those data were eliminated from the analysis. We did not exclude the data of cytokine levels of subjects with antipyretic medication.
Statistical analyses
Data were analyzed using unpaired Student’s t-test when comparing two experimental groups. Multiple comparisons were conducted using one-way analysis of variance (ANOVA) followed by the Tukey–Kramer post hoc test. Pearson correlation coefficients, and multiple-regression analysis were conducted using Prism v.7 or v.9 for Mac OS X. Error bars represent the standard deviation (SD). P-values less than 0.05 (*) were considered statistically significant. Statistical significance of the correlation coefficient of each pair of symptom scores (p-values) was calculated using Prism 7 software.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data generated or analyzed during this study are included in the publication article and its supplementary information files.
References
Temizoz, B., Kuroda, E. & Ishii, K. J. Vaccine adjuvants as potential cancer immunotherapeutics. Int. Immunol. 28, 329–338 (2016).
Demento, S. L. et al. Inflammasome-activating nanoparticles as modular systems for optimizing vaccine efficacy. Vaccine 27, 3013–3021 (2009).
Hornung, V. et al. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat. Immunol. 9, 847–856 (2008).
Kuroda, E. et al. Silica crystals and aluminum salts regulate the production of prostaglandin in macrophages via NALP3 inflammasome-independent mechanisms. Immunity 34, 514–526 (2011).
Mata-Haro, V. et al. The vaccine adjuvant monophosphoryl lipid A as a TRIF-biased agonist of TLR4. Science 316, 1628–1632 (2007).
Koyama, S. et al. Plasmacytoid dendritic cells delineate immunogenicity of influenza vaccine subtypes. Sci. Transl. Med. 2, 25ra24 (2010).
Hanley, S. J., Yoshioka, E., Ito, Y. & Kishi, R. HPV vaccination crisis in Japan. Lancet 385, 2571 (2015).
Su, J. R. et al. Anaphylaxis after vaccination reported to the vaccine adverse event reporting system, 1990-2016. J. Allergy Clin. Immunol. 143, 1465–1473 (2019).
Erlewyn-Lajeunesse, M., Hunt, L. P., Heath, P. T. & Finn, A. Anaphylaxis as an adverse event following immunisation in the UK and Ireland. Arch. Dis. Child 97, 487–490 (2012).
Kawabata, A. Prostaglandin E2 and pain–an update. Biol. Pharm. Bull. 34, 1170–1173 (2011).
Vandenbroucke, E., Mehta, D., Minshall, R. & Malik, A. B. Regulation of endothelial junctional permeability. Ann. N. Y. Acad. Sci. 1123, 134–145 (2008).
Dinarello, C. A. Infection, fever, and exogenous and endogenous pyrogens: some concepts have changed. J. Endotoxin. Res. 10, 201–222 (2004).
Dinarello, C. A. Cytokines as endogenous pyrogens. J. Infect. Dis. 179, S294–S304 (1999).
Miyashita, Y. et al. Immune-regulatory microRNA expression levels within circulating extracellular vesicles correspond with the appearance of local symptoms after seasonal flu vaccination. PLoS ONE 14, e0219510 (2019).
Christian, L. M., Porter, K., Karlsson, E. & Schultz-Cherry, S. Proinflammatory cytokine responses correspond with subjective side effects after influenza virus vaccination. Vaccine 33, 3360–3366 (2015).
Simons, M. & Raposo, G. Exosomes–vesicular carriers for intercellular communication. Curr. Opin. Cell Biol. 21, 575–581 (2009).
Valadi, H. et al. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 9, 654–659 (2007).
Kouwaki, T., Okamoto, M., Tsukamoto, H., Fukushima, Y. & Oshiumi, H. Extracellular vesicles deliver host and virus RNA and regulate innate immune response. Int J. Mol. Sci. 18, 666 (2017).
Robbins, P. D. & Morelli, A. E. Regulation of immune responses by extracellular vesicles. Nat. Rev. Immunol. 14, 195–208 (2014).
Colombo, M., Raposo, G. & Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev. Cell Dev. Biol. 30, 255–289 (2014).
Alexander, M. et al. Exosome-delivered microRNAs modulate the inflammatory response to endotoxin. Nat. Commun. 6, 7321 (2015).
Okamoto, M. et al. MicroRNA-451a in extracellular, blood-resident vesicles attenuates macrophage and dendritic cell responses to influenza whole-virus vaccine. J. Biol. Chem. 293, 18585–18600 (2018).
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).
Li, Q. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382, 1199–1207 (2020).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615 (2020).
Oshiumi, H. Circulating extracellular vesicles carry immune regulatory miRNAs and regulate vaccine efficacy and local inflammatory response after vaccination. Front. Immunol. 12, 685344 (2021).
Tsukamoto, H., Kouwaki, T. & Oshiumi, H. Aging-associated extracellular vesicles contain immune regulatory microRNAs alleviating hyperinflammatory state and immune dysfunction in the elderly. iScience 23, 101520 (2020).
Smyth, L. A., Boardman, D. A., Tung, S. L., Lechler, R. & Lombardi, G. MicroRNAs affect dendritic cell function and phenotype. Immunology 144, 197–205 (2015).
Harris, T. A., Yamakuchi, M., Ferlito, M., Mendell, J. T. & Lowenstein, C. J. MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc. Natl Acad. Sci. USA 105, 1516–1521 (2008).
Mehta, A. et al. The microRNA-212/132 cluster regulates B cell development by targeting Sox4. J. Exp. Med. 212, 1679–1692 (2015).
Verma, K. et al. miR-625-3p is upregulated in CD8+ T cells during early immune reconstitution after allogeneic stem cell transplantation. PLoS ONE 12, e0183828 (2017).
Pasparakis, M., Alexopoulou, L., Episkopou, V. & Kollias, G. Immune and inflammatory responses in TNF alpha-deficient mice: a critical requirement for TNF alpha in the formation of primary B cell follicles, follicular dendritic cell networks and germinal centers, and in the maturation of the humoral immune response. J. Exp. Med. 184, 1397–1411 (1996).
Jelinek, D. F. & Lipsky, P. E. Enhancement of human B cell proliferation and differentiation by tumor necrosis factor-alpha and interleukin 1. J. Immunol. 139, 2970–2976 (1987).
Thompson, C. B. et al. CD28 activation pathway regulates the production of multiple T-cell-derived lymphokines/cytokines. Proc. Natl Acad. Sci. USA 86, 1333–1337 (1989).
Yu, Y. et al. Plasma miR-92a-2 as a biomarker for small cell lung cancer. Cancer Biomark. 18, 319–327 (2017).
Ranade, A. R. et al. MicroRNA 92a-2*: a biomarker predictive for chemoresistance and prognostic for survival in patients with small cell lung cancer. J. Thorac. Oncol. 5, 1273–1278 (2010).
Zhao, Y., Dang, Z. & Chong, S. Mmu-miR-92a-2-5p targets TLR2 to relieve Schistosoma japonicum-induced liver fibrosis. Int. Immunopharmacol. 69, 126–135 (2019).
Liu, X. et al. MicroRNA-148/152 impair innate response and antigen presentation of TLR-triggered dendritic cells by targeting CaMKIIalpha. J. Immunol. 185, 7244–7251 (2010).
Zou, Q., Yang, M., Yu, M. & Liu, C. Influences of regulation of miR-126 on inflammation,Th17/Treg subpopulation differentiation, and lymphocyte apoptosis through caspase signaling pathway in sepsis. Inflammation 43, 2287–2300 (2020).
Santovito, D. et al. Noncanonical inhibition of caspase-3 by a nuclear microRNA confers endothelial protection by autophagy in atherosclerosis. Sci. Transl. Med. 12, eaaz2294 (2020).
Raposo, G. & Stoorvogel, W. Extracellular vesicles: exosomes, microvesicles, and friends. J. Cell Biol. 200, 373–383 (2013).
Knoll, M., Simmons, S., Bouquet, C., Grun, J. R. & Melchers, F. miR-221 redirects precursor B cells to the BM and regulates their residence. Eur. J. Immunol. 43, 2497–2506 (2013).
Jafarinejad-Farsangi, S., Jazi, M. M., Rostamzadeh, F. & Hadizadeh, M. High affinity of host human microRNAs to SARS-CoV-2 genome: an in silico analysis. Noncoding RNA Res. 5, 222–231 (2020).
Chow, J. T. & Salmena, L. Prediction and analysis of SARS-CoV-2-targeting microRNA in human lung epithelium.Genes 11, 1002 (2020).
Natarelli, L. et al. MicroRNAs and long non-coding RNAs as potential candidates to target specific motifs of SARS-CoV-2. Noncoding RNA 7, 14 (2021).
Acknowledgements
We thank all our laboratory members for their helpful discussion. This work is supported by AMED (20fk0108142) and CREITO.
Author information
Authors and Affiliations
Contributions
H.O., K.N., K.M., S.F., and Y.M. designed the cohort study. Y.M., T.Y., and Y.T. collected samples. H.T. and T.K. supervised the experiments to measure cytokine, antibody, and miRNA levels. H.O., K.T., and Y.M. analyzed the data. H.O. and Y.M. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Miyashita, Y., Yoshida, T., Takagi, Y. et al. Circulating extracellular vesicle microRNAs associated with adverse reactions, proinflammatory cytokine, and antibody production after COVID-19 vaccination. npj Vaccines 7, 16 (2022). https://doi.org/10.1038/s41541-022-00439-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41541-022-00439-3
This article is cited by
-
The use of RNA-based treatments in the field of cancer immunotherapy
Molecular Cancer (2023)
-
Impact of sex and age on vaccine-related side effects and their progression after booster mRNA COVID-19 vaccine
Scientific Reports (2023)