Abstract
Diabetes is a chronic metabolic disease characterized by high glucose concentration in blood. Conventional management of diabetes requires skin pricking and subcutaneous injection, causing physical pain and physiological issues to diabetic individuals. Hydrogels possess unique advantages such as lightweight, stretchability, biocompatibility, and biodegradability, offering the opportunities to be integrated as flexible devices for diabetes management. This review highlights the development of hydrogels as flexible materials for diabetes applications in glucose monitoring, insulin delivery, wound care, and cell transplantation in recent years. Challenges and prospects in the development of hydrogel-based flexible devices for personalized management of diabetes are discussed as well.
Similar content being viewed by others
Introduction
Hydrogels are flexible semi-solids with high water content and crosslinked three-dimensional (3D) networks composed of swellable hydrophilic polymer chains1. In the past decades, hydrogels have received considerable attention due to their wide biological applications2,3,4,5,6,7. Their structures bear resemblance to the extracellular matrix (ECM) and possess properties similar to those of natural soft tissues. In general, hydrogels can be classified as either natural or synthetic based on the origin of their polymers. The most widely used natural polymers for fabrication of hydrogels include proteins (i.e., collagen and gelatin) and polysaccharides (i.e., starch, agarose, and alginate)8,9,10,11,12. Hydrogels composed of natural polymers possess inherent biocompatibility, biodegradability, and non-toxicity13. Synthetic polymer-based hydrogels generally contain hydrophilic chemical structures that allow them to interact with water, i.e., –OH, –COOH, and –CONH214,15. Physical and chemical cross-linkings between polymer chains enable hydrogels to be resistant to dissolution and stay intact, i.e., covalent bonding, hydrogen bonding, and van der Waals interactions16. These polymer chain entanglements allow entrapment of functional molecules like drugs or proteins for delivery purpose17,18,19. Mechanical properties of hydrogels are usually adjustable based on degree of polymer chain entanglements20,21,22. With different physicochemical properties, they can be made into stretchable or injectable materials23. Depending on biosafety, biodegradability, and biocompatibility of polymers used, hydrogels can be used as implantable materials or devices24. The porous structures of hydrogels allow diffusion of compounds, expanding their applicability for active compound delivery25. Given their unique and tunable characteristics, hydrogel-based materials have attracted great attention from the healthcare industry in developing personal care products26,27,28,29. drug delivery systems30, biosensors31, and new applications that have yet to be explored. The wide flexibility of hydrogels allows them to be utilized in a variety of applications relating to diabetes diagnosis, treatment, and management (Fig. 1).
Hydrogels possess unique and tunable characteristics such as biocompatibility, biodegradability, stretchability, etc. The wide flexibility of hydrogels allows them to be utilized in a variety of applications relating to diabetes, including glucose monitoring, insulin delivery, cell transplantation, wound care, and nursing management.
Diabetes is one of the most common chronic diseases among the leading causes of death globally. The International Diabetes Federation (IDF) statistics revealed that there were 463 million people with diabetes worldwide in 2019 and the number is expected to reach 700 million by 204532,33. There are two types of diabetes classified based on different pathogenetic mechanisms: type I and II. Type I diabetes is caused by insulin deficiency associated with impaired pancreatic islets and is highly dependent on insulin administration. In contrast, type II diabetes is caused by the occurrence of insulin resistance by the body34. Despite tremendous progress has been made to treat diabetes, there is no specific cure for diabetes35. With an increased glucose level, diabetic individuals could develop metabolic disorders at higher risks. They require regular monitoring of blood glucose level to keep low risks for diabetes complications36. Although commercial glucose meters and glycohemoglobin test kits are readily available for diagnosis and monitoring of diabetes37,38, patients require finger pricking 3–4 times/day for blood glucose checking. The process can be painful and inconvenient39. In addition, the process of collecting blood gives rise to a risk of bacterial infection and may lead to serious health issues40. Thus, it is necessary to develop real-time and non-invasive monitoring biosensors for glucose monitoring. In the early stage of diabetes, sustained insulin hypodermic injection by insulin-pump can be used to achieve optimal glycemic control41,42. As the disease progresses into advanced stage, it is likely for patients to develop insulin resistance and may face multiple long-term health complication such as end-stage renal disease, retinopathy, neuropathy, diabetic foot, etc34. The prevalence of diabetes generally rises with age, with the age group of 65–79 having the highest percentage of diabetes occurrence (19.9%, 111.2 million)43. With an increasing number of elderly patients in diabetes, advanced sensor devices need to be developed for effective, convenient management and nursing of elderly diabetic patients44,45.
The healthcare industry is entering the era of digital innovation, as digitalization can realize the goal of on-demand healthcare46,47,48,49. Digital health solutions such as telehealth, telemedicine, and remote patient monitoring, allow patients for decentralized medical care without sacrificing medical attention50,51,52,53,54,55. Replacing sporadic medical appointments with continuous monitoring via connected medical devices can provide improved diagnostic capability and the opportunity to deliver preventative care56,57,58,59. In short, digital healthcare could reduce medical costs while maintaining a high level of care compared to traditional healthcare. As digital healthcare is significant, it is of great interest to develop soft, foldable, stretchable, conformal, lightweight, and wearable digital healthcare devices for improving healthcare technology and patient compliance. Hydrogel is one of the most representative platforms that possess aforementioned properties and can be used for fabrication of flexible healthcare electronics, advancing the development in diabetes care and unlocking other possibilities. Herein, we discuss recent advances in the development of hydrogel-based flexible materials for diabetes diagnosis, treatment and management. We first focus on hydrogel-based blood glucose monitoring systems for diabetes diagnosis. We then review hydrogel-based therapeutic methods in cell transplantation and insulin delivery for type I and type II diabetes. We also discuss the application of hydrogels for wound care, targeting chronic diabetes wounds treatment specifically. In the final part of the review, we also describe how hydrogels help on developing flexible electronic-based nursing care devices for management of diabetes.
Glucose monitoring
Blood glucose level in diabetic patients fluctuate abnormally from time to time due to insufficient insulin secretion or defective insulin action60. Frequent monitoring of blood glucose is vital for diabetes diagnosis and management. Development in continuous glucose monitoring (CGM) systems in the last decade makes on-demand measurement of glucose level possible, which subsequently enables hypo/hyperglycemia detection and prediction, retrospective analysis, etc61,62. CGM systems provide patients with real-time blood glucose level that show information on trend, which is useful for monitoring the effectiveness of clinical treatment. CGM devices are therefore seen as the next-generation replacement for traditional glucose meters63,64. Hydrogels can be made into microbeads and fibers, offering potential advantages to be delivered as CGM systems to targeted areas for glucose monitoring in a minimally invasive way29,65,66,67,68. There are mainly three glucose detection methods in CGM systems: (1) the use of phenylboronic acid (PBA) moiety in binding glucose based on the high specificity of boronate group for cis-diols, (2) the use of glucose oxidase (GOx) in catalyzing glucose into hydrogen peroxide (H2O2) and D-gluconolactone (which would hydrolyze to gluconic acid), and (3) the use of concanavalin A (Con A) in binding glucose based on its strong affinity to hydrocarbon moiety69,70.
PBA and its derivatives are typical glucose-sensitive compounds and have been widely used for fabrication of glucose-responsive systems. Incorporation of PBA into hydrogels endow them with glucose-responsive performance71. In aqueous solution, PBA exists in the form of uncharged triangular and anionic tetrahedral in equilibrium. Glucose has a good affinity for the latter and can be reversibly bound with it to form a boronate ester (Fig. 2a)72. Increased negative charge density and hydrophilicity would lead to an increased distance between polymer chains, which eventually causes a change in the physicochemical properties of hydrogels, i.e., the binding of PBA to glucose changes the optical properties and glucose level can be detected by fluorescence intensity. On another note, glucose can be catalyzed by GOx to H2O2 and gluconic acid. The yielded H2O2 will be electrolyzed and electrochemically detected by electrodes (Fig. 2b). Aside from the use of PBA and GOx, Con A is a well-known mannose/glucose-binding lectin isolated from Jack beans (Canavalia ensiformis) and contains four sugar-binding sites. The sugar-binding sites of Con A can bind with α-D-mannopyranose, α-D-glucopyranose, and other non-reducing sugars. By incorporating competitors with fluorophore, glucose molecules can compete with them for binding sites of Con A and glucose level can be detected through fluorescence intensity (Fig. 2c). Due to PBA’s good biocompatibility and biodegradability, PBA-modified hydrogels can be implanted into the body without causing much immune response and can be used to develop CGM systems73. Yetisen et al. reported hydrogel-based optical fibers made of poly(acrylamide-co-poly(ethylene glycol) diacrylate) core and calcium alginate cladding for optical-based CGM system74. PBA moieties were covalently incorporated in the core for glucose sensing. When glucose permeates into the core and reacts with PBA, osmotic pressure of the hydrogel increases and causes a change in density (Fig. 3a). Light propagation through the fiber will be shifted and the differences can be detected through refractive index (RI) to get quantitative readout of glucose level (Fig. 3b). Excitingly, the hydrogel fiber can be injected into epidermis (as deep as 3 cm) and retractable (Fig. 3c). Besides, PBA-based glucose sensing hydrogels can also be designed with electrical signal as quantitative readout of glucose level75. Dautta et al. copolymerized polyacrylamide and PBA (p(PBA-co-AAm)) hydrogel for electrical signal-based CGM system76. When glucose level increased, the thickness of capacitor formed by coupling two split rings will change according to the swelling ratio of the hydrogel, which ultimately gives resonant frequency as a quantitative measure of glucose level (Fig. 3d). Power supply is not required for the sensor because it responses remotely via near-field coupling. The sensor can be implanted under the skin (Fig. 3e) and exhibited excellent sensitivity in frequency shift to glucose concentrations (Fig. 3f). In brief, a variety of detection methods (e.g., optics, electricity, and electrochemistry) can be incorporated in PBA-based glucose sensors for deriving glucose readings.
a Reversible and dynamic binding of glucose to anionic tetrahedral structure of PBA72. b Glucose is enzymatically converted to H2O2 and D-glucose acid, and H2O2 is electrolyzed to release electrons. c Con A have various binding sites for sugar. When free glucose molecules appear around Con A, they will compete the binding sites with competitors. Through labeling competitors with fluorophore, glucose level can be examined. Reprinted with permission from ref. 72. Copyright 2019 John Wiley & Sons.
a Structural composition of glucose-sensitive fiber core with calcium alginate cladding74. b Transmitted light intensity across the hydrogel fiber measured in different glucose concentrations (4.0–12.0 mM). c Implantation of hydrogel optical fibers in porcine tissue. d Glucose binding with p(PBA-co-AAm) triggers the hydrogel to swell. Modulation in thickness of the hydrogel changes the capacitance of resonator76. e A wireless CGM sensor implanted below the skin (chicken) for near-field coupling glucose measurement. f Sensor response via frequency shift to glucose concentration (2.8 mM) within chicken meat. Reprinted with permission from refs. 74,76. Copyright 2017 John Wiley & Sons and 2018 American Chemical Society.
In contrast to implantable sensors, non-invasive sensors can monitor glucose level by measuring body fluids, i.e., tears and sweats77,78,79,80. Studies have shown that there are glucose transporter proteases in human cornea and glucose can be transported by these proteases from blood to tears. Hence, blood glucose level can be monitored non-invasively via tears81. Apart from tears, blood glucose level can also be monitored via sweats as blood vessels around sweat glands are highly developed82. Contact lenses are one of the most representative non-invasive approaches to monitor glucose level via tears. Elsherif et al. reported PBA glucose sensing-based contact lenses that had laser-inscribed array structure imprinted on them for light diffusion. Light diffusion through the hydrogel is dependent on volumetric expansion of the hydrogel responding to glucose concentration83. Glucose concentration can then be detected by measuring the intensity of optical light diffused through the hydrogel. The diameter of diffused light spot reduces as glucose concentration increases.
In contrast, GOx-based hydrogel sensors are widely used due to their high sensitivity75. Kim et al. immobilized GOx with polyvinyl alcohol/β-cyclodextrin/GOx (PVA/b-CD/GOx) hydrogels crosslinked by citric acid. As mentioned earlier, glucose can be catalyzed by GOx to H2O2 and gluconic acid (Fig. 4a)84. H2O2 can be further oxidized and releases hydrogen ions and electrons that alter the conductivity of buffer solution. The changes in conductivity can be detected amperometrically (Fig. 4b). Apart from exhibited good biocompatibility and mechanical properties, the hydrogel sensor showed a relatively high sensitivity to glucose level ranged from 1.0 to 5.0 mM (7.59 μA mM−1) (Fig. 4c).
Con A is also widely used for hydrogel-based glucose sensing. Locke et al. reported a competitive binding glucose sensor based on fluorescently labeled PEGylated Con A and aminopyrene trisulfonate mannotetraose (APTS-MT)85. PEGylated Con A can reversibly bind to glucose at higher affinity and fluorescently labeled APTS-MT at lower affinity. As glucose concentration increases, glucose molecules compete the binding sites with APTS-MT. The changes in the ratio of fluorescence intensities between PEGylated Con A and APTS-MT can therefore reflect glucose level. Increased ratio of fluorescence intensities corresponds to higher glucose level. Despite Con A has good sensitivity towards glucose, it has poor stability and biocompatibility, hampering its application development86. Research from different science branches is required for establishing the toxicity profile of Con A used in hydrogels to overcome the risk of immunogenicity and cytotoxicity.
Insulin delivery
Insulin is a key hormone in regulating gluconeogenesis, playing important roles in diabetes treatment. It can be delivered via syringe pumps, injection syringes, pens, inhaler injections, and more recently, microneedles and oral administration87,88. Hydrogel has the ability to encapsulate insulin and continuously release it in response to environmental changes, holding great potential for the development of insulin delivery systems89. It can reduce pain and risk of infection of diabetic individuals caused by injection. Similar to CGM systems mentioned above, insulin delivery systems generally have three types of glucose-responsive elements, including PBA, GOx, and Con A.
GOx can be covalently immobilized within hydrogels and catalyzes glucose to generate H2O2, which subsequently lead to the break of crosslinkers to release insulin90. Wang et al. synthesized a core-shell microneedle array patch made of polyvinyl alcohol (PVA) gel91. The core of the microneedle contained GOx, which produces H2O2 that subsequently stimulates the release of insulin. To control the release of GOx, it was encapsulated with acrylate nanogel (GOx-NG) and immobilized with PVA network crosslinked by H2O2-labile linker, N1-(4-boronobenzyl)-N3(4-boronophenyl)-N1, N1, N3, N3-tetramethylpropane-1,3-diaminium (TSPBA). Increased blood glucose level triggers the production of H2O2, which subsequently activates the breaking of crosslinker TSBPA to release insulin modified with 4-nitrophenyl 4-(4,4,5,5-tetramethyl-1,3,2-dioxaborolan-2-yl) benzyl carbonate (insulin-NBC) (Fig. 5a). Insulin-NBC will then be hydrolyzed to modulate the corresponding blood glucose level. On the surface of microneedles, there were nanogels containing catalase (CAT) to decompose excess H2O2 produced in the catalytic reaction and reduce local inflammatory reaction. When diabetic mice were administered continuously for up to 40 h, their blood glucose levels were controlled in the range of 100–250 mg dL−1 and no hypoglycemia was recorded (Fig. 5b).
a Insulin release is triggered from the core matrix of PVA-TSPBA microneedle array patch by a hyperglycemic state91. b Blood glucose level of diabetic mice treated with microneedle array-array patches. Blue arrow indicates administration of microneedle array; red arrow indicates removal of microneedle. c Inclusion of PBA-PLGA MPs into DOP-HA hydrogel to form MP-gel93. d Therapeutic efficacy of insulin-loaded MP-gel in diabetic mice model. Reproduced with permission from refs. 91,93. Copyright 2018 American Chemical Society and 2017 Elsevier.
PBA derivatives have been widely used for glucose-regulated insulin delivery systems as they have better response towards glucose and good stability92. Zhao et al. incorporated PBA-modified porous poly(lactic-co-glycolic acid) microparticles (PBA-PLGA MPs) into dopamine-conjugated hyaluronic acid (DOP-HA) hydrogel via reversible phenyl borate esters93. At low glucose level, DOP-HA acts as a barrier to prevent the releasing of insulin from the microparticles; at high glucose level, glucose competes to replace DOP in response to PBA, causing the detachment of microparticles from the hydrogel and subsequently the releasing of insulin (Fig. 5c). A single injection of the insulin delivery system allowed diabetic mice to maintain normal blood glucose level for approximately two weeks (Fig. 5d).
Apart from PBA derivatives, glucose-binding proteins such as Con A also respond to changes in glucose level by competitive binding with glucose70. In general, Con A can be immobilized in a hydrogel network by physical cross-linking such as hydrogen bonding. However, physical cross-linking is a dynamic and weak force that could make hydrogels vulnerable to component loss. The leakage of Con A could lead to weak glucose sensitivity94. Alternatively, Con A can be covalently immobilized on the polymer matrix of hydrogels, in which the loss of Con A could be much restricted and improve the corresponding glucose-responsive properties. Lin et al. fabricated a glucose-sensitive hydrogel from covalently modified carboxylated pullulan and Con A95. Pullulan was carboxylated with succinic anhydride to yield a pullulan derivative bearing -COOH groups before reacting with Con A via amidization to form hydrogel. Insulin can then be controlled-released based on the hydrogel’s response to physiological pH condition, realizing closed-loop treatment’s concept for diabetes.
At present, oral administration is available to relieve the pain endured by diabetic individuals who require insulin injection. However, the bioavailability of orally taken insulin is low. The stringent enzyme and pH environments of gastrointestinal tract limit the oral absorption of insulin96,97,98,99,100,101,102. Qi et al. reported a rigid and highly elastic semi-interpenetrating polymer network (semi-IPN) hydrogel made of poly(acrylamide-co-acrylic acid) (PMA) with salecan for oral insulin delivery (Fig. 6a)103. In vivo experiments demonstrated that pharmacological efficacy of oral-administered insulin-containing hydrogels was 10-fold higher compared to oral-administered free insulin solution (Fig. 6b). Liu et al. prepared anionic insulin/heparin sodium nanoparticles coated with cationic chitosan and encapsulated them with hydrogels for intestinal insulin delivery (Fig. 6c)104. The pH and amylase-responsive hydrogel were synthesized via free radical copolymerization of methacrylic acid (MAA) and acrylate-grafted-carboxymethyl starch (CMS-g-AA) (Fig. 6d). The hydrogel improves acid stability of the system and protects insulin from disintegration in the gastric environment98. The presence of intestinal amylase triggers the releasing of insulin, facilitating oral delivery of insulin (Fig. 6e). More research is needed to develop intelligent insulin delivery systems with high selectivity, rapid response, better biocompatibility, great efficacy, and simple preparation methods.
a Fabrication of semi-IPN hydrogel using PMA as matrix and salecan polysaccharide as entrapped chain103. b Blood insulin level of diabetic mice after oral and injection administration of insulin. c Construction of nanoparticles prepared from chitosan and insulin/heparin (tagged as CS/Ins/HS NPs)104. d CS/Ins/HS NPs loaded in CMS-g-AA/PMAA hydrogel. e Blood glucose level of diabetic mice following oral and injection administration of insulin. Reproduced with permission from refs. 103,104. Copyright 2018 American Chemical Society and 2018 American Chemical Society.
Cell transplantation
In type I diabetes, the body’s insulin-producing cells are impaired, leading to insufficient insulin production. Islet transplantation is a process that transfers and implants healthy islets from a donor into a diabetic patient. It reduces the use of exogenous insulin and prevents the occurrence and development of diabetes complication. In brief, islet transplantation can improve life quality of a diabetic individual (especially of type I diabetes) in terms of insulin dependency and medical expenses. However, implementation of islet transplantation is hampered by challenges such as shortage of pancreas donors, transplant rejection by the immune system, adverse drug reaction, complication due to portal vein injection of cells, etc105. Encapsulation of islets by biomaterials and surface modification of islets may overcome some of these issues106. Hydrogels are particularly attractive for islet formation as they are able to provide environments similar to cytoplasmic matrix and improve islet’s function and stability107. In addition, hydrogels can encapsulate bioactive molecules such as peptide sequences, ECM proteins, cytokines, or accessory cells, and allow diffusion and exchange of oxygen, nutrients, secretory factors, and metabolic waste to support and protect islets108.
Hydrogel-based encapsulation systems for islets can be classified into macrocapsule and microcapsule devices109. Generally, macrocapsules prevent embedded cells from escaping into the body, and can be easily inserted and retrieved by subcutaneous transplantation110,111. On the other hand, microcapsules contain membranes to protect contained cells and facilitate selective transmission that may include diffusion of biological active substances and protection of islets from immune cells. Macrocapsules have been widely studied and used in real life while the application of microcapsules is facing hurdles such as quality control, toxicity, etc. An et al. reported a thread-reinforced alginate fiber for islet encapsulation (TRAFFIC) with enhanced mechanical strength, and simple implantation and retrieval steps109. They coated nylon suture with 7% (wt./vol.) poly(methyl methacrylate)/N,N dimethylformamide solution to get thread with nanoporous structure. The threads were spirally twisted and immersed in a solution of calcium chloride, resulting in a calcium ion-releasing nanoporous polymer threads. The threads promoted uniform in situ cross-linking and exerted strong adhesiveness to alginate hydrogel (Fig. 7a). When TRAFFIC was used to treat diabetic mice, blood glucose of diabetic mice dropped to normal range in 2 days after transplantation and remained stable until the retrieval of graft (Fig. 7b). Further experiment showed that TRAFFIC could be quickly removed from dogs using a minimally invasive laparoscopic procedure, having potential in clinical application (Fig. 7c). Cheng et al. developed a macrocapsule system for β-cells cryopreservation by combining hydrogel encapsulation with cold response nanocapsules (CR-NCs)112. CR-NCs were fabricated with poly-N-isopropylacrylamide-co-butylacrylate (PNIPAM-B), pluronic F127, and PLGA using double emulsion method. The nanocapsules were loaded with trehalose, a non-permeating cryoprotective agent (CPA), which has been recognized as less toxic and highly efficient at cryopreserving different kinds of cells or organisms. When temperature drops below 10 °C, PNIPAM-B would undergo phase transformation from hydrophobic to hydrophilic, causing disintegration of CR-NCs to release trehalose for freezing of β-cells (Fig. 7d). After transplanting the cell-laden hydrogels, blood glucose level of diabetic rats gradually decreased to the normal range and maintained for about 2 weeks, suggesting that cryopreserved cell-laden hydrogels have similar ability of regulating blood glucose as fresh islets (Fig. 7e). This system facilitates the establishment of ready-to-use biological samples.
a Fabrication of TRAFFIC device109. b Blood glucose concentration of diabetic mice after transplantation of encapsulated islets. c Rapid retrieval of macrocapsule in a dog model. d Fabrication of nanocapsule via double emulsion method112. e Blood glucose concentration (mmol/L) of diabetic mice of different treatment groups over a period of 14 days, n = 3. None indicates no operation was carried out; fresh indicates fresh cells were transplanted; cryopreserved indicates cryopreserved cells were transplanted. Reproduced with permission from refs. 109,112. Copyright 2018 National Academy of Sciences and 2019 Wiley-VCH.
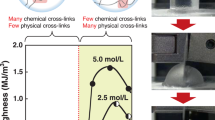
Geometry and hardness of microcapsules affect cell viability of islets to a certain extent. In general, microcapsules require good film forming performance, mechanical strength, stability, biocompatibility, inertness for not reacting with encapsulated cells, etc. Microcapsule systems fabricated by additive manufacturing have attracted great attention from scientists due to their better mechanical properties. In general, annular microcapsules have better mass transfer compared to spherical microcapsules113,114,115. Ernst et al. reported a recyclable annular islet microcapsule with enhanced encapsulation efficiency and mechanical properties. The annular microcapsule can be recovered from deformation (Fig. 8a)114. Its high encapsulation efficiency saves preparation time and its improved mechanical strength increased the survival rate of embedded cells for a longer duration. Each torus of the device has a 3D-printed elastomer scaffold coated by a cell-seeded alginate hydrogel layer (Fig. 8b). Specifically, the elastic double helix scaffold was wetted with calcium sulfate suspension and dried. It was then further coated with calcium alginate (Fig. 8c). Ring-shaped hydrogels were proven to be more suitable for the survival of islets as they provide adequate oxygenation for encapsulated islets, as opposed to sphere-shaped hydrogels where hypoxia can happen. Blood glucose level remained significantly lower in diabetic mice treated with toroidal microcapsule for more than 84 days whereas diabetic control was hyperglycemic at all times, demonstrating the effectiveness of the device (Fig. 8d).
a Top: the device recovered to its original configuration following a release after compression. Bottom: the device maintained its original configuration after tension was applied114. b Islet encapsulation device. c Fabrication process for islet encapsulation device. (d) Blood glucose concentration of diabetic mice receiving toroidal microcapsule transplantation (n = 4) and diabetic control (n = 1) for 88 days. Reproduced with permission from ref. 114. Copyright 2019 John Wiley & Sons.
Hydrogels immobilized with bioactive molecules like heparin or growth factors can prevent islets from degradation and help to regulate inflammatory responses during cell transplantation116,117. In particular, vascular endothelial growth factor (VEGF) has been shown to enhance revascularization of islet transplantation site and prevent the loss of islet function due to ischemia118. It can stimulate the recruitment of endothelial cells and accelerates angiogenesis119. To control the release of VEGF, Marchioli et al. constructed a 3D ring-shaped polycaprolactone scaffold platform composed of heparinized surface electrostatically bound to VEGF for islet encapsulation120. Heparin was covalently bound to the polymer using 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide/N-hydroxy succinimide, enhancing the polymer’s binding ability to VEGF. VEGF fixed on the surface of scaffold could stimulate rapid angiogenesis around the scaffold. Excitingly, the scaffold platform could preserve islet after 7 days by observing islet functional behavior on day 1 and day 7.
Wound care
Wound healing is a complex process, which includes four overlapping phases, namely coagulation, inflammation, proliferation, and remodeling121. The transition between phases depends on inflammatory cells, fibroblasts, keratinocytes and endothelial cells, as well as relative growth factors and enzymes122. However, diabetic wounds are chronic wounds through complex pathophysiological mechanisms and do not proceed through the four stages of normal wound healing. The cells around diabetic wounds undergo harmful phenotypic changes that impair their ability to respond to signaling cascade of cytokines and growth factors. Diabetic wounds generally contain a low level of growth factors (e.g., VEGF), which could lead to a reduction in angiogenesis. Apart from that, high levels of inflammatory macrophage around diabetic wounds would cause the production of inflammatory cytokines. Overproduction of inflammatory cytokines would subsequently increase fibroblast apoptosis and decrease angiogenesis. In brief, both fibroblasts and keratinocytes within diabetic wounds are dysfunctional in comparison to normal wounds, thereby making the former wound harder to heal123. This subsequently increases the risks for infection as defective cells lead to weaker bacterial load clearance and promote the formation of biofilms. Diabetic individual is known to be more susceptible to infections due to impaired immune system. Bacteria residing the cells would produce endotoxins, further causing damage to tissues and impeding the wound healing process124,125,126,127. Hence, custom-made wound dressings with additional functions are important for diabetic individuals to protect wound sites from infection while providing an undisturbed healing process.
Conventional wound dressings are generally made from a piece of gauze and an adhesive backing. They are on dry basis and could adhere to wounds, causing pain and trauma to patients during the removal process. Wound dressings that retain moist environments for wound sites are thought to be exerting positive effects for wound healing as they can reduce wound exudate, providing protection for the wound and accelerating tissue regeneration128,129. A moist environment could also promote keratinocytes migration and fibroblast proliferation, which are vital for epithelialization130,131,132. Hydrogels are perfect candidates for moist wound dressings. They are also more oxygen permeable compared to conventional wound dressings130,133. Furthermore, antimicrobial materials/drugs can be incorporated/loaded into hydrogels to speed up the wound healing process134,135,136,137. There are generally two mechanisms used for designing hydrogels in preventing microbial infection: contact killing and bactericide-releasing. Contact-killing mechanism involves killing microbes by lethal moieties of polymeric networks within a hydrogel; on the other hand, bactericide-releasing mechanism involves killing microbes by antimicrobial agents embedded within a hydrogel138,139,140. Contact-killing approaches kill microbes upon contact and are considered as the most direct sterilization method. Due to hydrogels’ good biocompatibility, they can be attached directly to wounds for contact killing. Quarterization generally involves the addition of hydrophobic alkyl side chain to amines, e.g., dimethyldecylammonium chitosan (with high quaternization)-graft-poly(ethylene glycol) methacrylate (DMDC-Q-g-EM) hydrogel (Fig. 9a-b)141. The cationic nature of chitosan attracts microbes with cell membranes of anionic nature. Microbes can then be sucked into the nanopores of the hydrogel, causing their death by initiating membrane disruption. Apart from contact killing, bactericide-releasing is a common method to kill bacteria, e.g., the incorporation of silver nanoparticles. Liu et al. reported a polysaccharide hydrogel embedded with gallic acid functionalized silver nanoparticles (GA-Ag NPs) for silver ion releasing to kill bacteria (Fig. 9c (i))142. Apart from acting as an antibacterial agent, GA-Ag NPs was also a photothermal agent that can convert 808 nm near-infrared (NIR) light into heat to provide synergistic antibacterial effect (Fig. 9c (ii)). Wound treated by GA-Ag NPs and NIR irradiation healed quicker compared to other treatment groups (Fig. 9d).
a Computer simulation on killing mechanism by DMDC-Q hydrogel: the ‘suctioning’ of Pseudomonas aeruginosa’s lipopolysaccharide (LPS) on bacterial membrane (lipid bilayer) by DMDC-Q hydrogel after 50 ns141. b Morphology of various pathogens in contact with DMDC-Q-g-EM hydrogel. Arrows indicate lesions and holes on the cell membranes. c Synthesis of GA-Ag NPs (i) and fabrication of GA-Ag NP hydrogel (ii) for combined antibacterial and photothermal effect to eliminate bacteria synergistically142. d Staphylococcus aureus-infected wounds with different treatment groups over a period of 7 days: phosphate buffer solution (PBS) (blank) (I); carrageenan hydrogel (control) (II); GA-Ag NP hydrogel (III); PBS + NIR (IV); Carrageenan hydrogel + NIR (IV); GA-Ag NP hydrogel + NIR (VI). Reprinted with permission from refs. 141,142. Copyright 2011 Nature Publishing Group and 2019 Elsevier.
As the inflammation phase is toned down, wound contraction occurs. Angiogenesis is essential to the migration-proliferation phases143,144,145,146,147,148. Delivery of growth factors to wounds accelerates tissue repair and wound healing149,150. Basic fibroblast growth factor (bFGF) induces angiogenesis and proliferation of fibroblasts, playing a critical role in promoting tissue repair151,152,153. Shi et al. reported alginate/calcium carbonate composite hydrogel microparticles loaded with bFGF and rifamycin (CD-F-R) for accelerating wound healing (Fig. 10a)154. Calcium carbonate was added to limit movement of polymer chains and hinder permeability of targeted drug to prolong drug release. bFGF and rifamycin were independently encapsulated in microparticles with different calcium carbonate concentrations to attain controlled releases of rifamycin and bFGF independently to achieve hemostasis, antibacterial properties, cell proliferation, and vascularization. Treatment with CD-F-R healed better compared to the control group (Fig. 10b).
a CD-F-R hydrogel dressing and its application in deep wound154. b Effect of treatment with CD-F-R hydrogel dressing on wound contraction for a period of 21 days. c Synthesis of BNN6@ZIF-8@PDA nanoparticles and fabrication of hydrogel158. d Photothermal releasing of nitric oxide (NO) in combating infection. e Hematoxylin and eosin staining of wound areas at day 3, 7 and 14. f Percentage of wound areas recovered over a period of 14 days. Reprinted with permission from refs. 154,158. Copyright 2019 American Chemical Society and 2020 Elsevier.
Multifunctional hydrogel dressings that simultaneously combat infection and promote cell growth are of interest. Researchers reported signaling molecules like nitric oxide (NO) play a crucial role in cell regeneration155. Exogenous NO can promote vascular perfusion and angiogenesis for modulating wound healing156,157. Moreover, NO can genetically alter bacterial biofilms and kill bacteria. Liu et al. reported a hydrogel loaded with NO bearing metal organic framework (MOF) materials to treat bacteria-infected chronic wound. NO donor, N,N’-di-sec-butyl-N,N’-dinitroso-1,4-phenylenediamine (BNN6) was selected to release NO under NIR treatment158. Zeolitic imidazolate framework-8 (ZIF-8), possesses a high specific surface area, was used to carry BNN6 non-covalently. Polydopamine (PDA) was coated onto ZIF-8 to enhance the photothermal effect of ZIF-8, which could also speed up the releasing rate of NO. The obtained nanoparticles (BNN6@ZIF-8@PDA) were encapsulated in a methacrylate/oxide dextran hydrogel (GEL/BZP) (Fig. 10c). Under NIR laser, the GEL/BZP hydrogel releases NO and possesses excellent photothermal properties to kill bacteria synergistically (Fig. 10d). After 14 days of GEL/BZP hydrogel and NIR treatment, the wound was healed quicker and sebaceous glands regenerated (red arrows) were larger compared to other treatment groups (Fig. 10e-f), demonstrating that combination of NO and NIR treatment is beneficial for wound healing by exerting antibacterial effect and promoting cell regeneration concomitantly.
Nursing management
Unlike acute lethal diseases, diabetes cause multiple health complication and older people would have higher risks for severe illness. Effective long-term nursing management is important to facilitate health complication associated with diabetes. While glucose monitoring is important to indicate patients for clinical treatment, monitoring of physiological activities of patients (e.g., human motion) is essential to manage diabetes as well. Flexible electronics play important roles in the development of monitoring and drug delivery devices. One of the most representative examples of flexible electronics for healthcare technology is electronic skin. Bao’s group proposed four important skin-like capabilities to be incorporated into electronic materials, namely, stretchability, self-healing ability, biocompatibility, and biodegradability159. Hydrogels are ideal materials for fabricating skin-like electronic devices for personal healthcare and human-activity monitoring as hydrogels can be designed and custom-made with aforementioned properties5,160. Mostafalu et al. reported a smart wound dressing bandage consisting of a pH- and temperature-responsive hydrogel loaded with thermo-responsive drug microbeads and an electrically controlled heating sensor (Fig. 11a)161. The thermo-responsive drug carrier was embedded in a layer of alginate brine gel that wrapped around a pH sensor and a heater to trigger the drug delivery system. The system was connected to a wireless electronic device to record signals and transmit them to a computer or mobile phone. The pH sensor monitors the pH of wounds, which is a key parameter of chronic wounds. When the pH of a wound drops below 6.5, the sensor would control the heater to heat up and release loaded drug into wound area based on thermal stimulation (Fig. 11b). The drug can be released uniformly when there is a triggered heat (Fig. 11c). For more comprehensive management of diabetes, wearable epidermal sensors that can capture human movements need to be developed, and it is important to improve the sensitivity and stability of sensors for better digital healthcare clinical application.
a Conceptual view of an automated smart bandage161. b In vitro test of pH variation over time followed by an activation of the heater at pH = 6.5. c Release rate of cefazolin adjusted by heating/re-heating. d Sensing components of a hydrogel sensor: sweat stimulation (left) and ISF extraction (right)162. e Sensor detecting biomarkers (e.g., lactate, caffeine, alcohol, and glucose) from sweat and ISF via iontophoresis. f Schematic illustration of how lactate, BP, and HR readings were taken for a volunteer. g Continuous current recording on sweat-lactate profile of a volunteer during cycling. h BP and HR signals recordings of a sedentary volunteer (left), when the volunteer was cycling (middle), and after cycling (right). Reprinted with permission from refs. 161,162. Copyright 2018 WILEY-VCH and 2021 Springer Nature.
Monitoring of physiological activities can provide accurate and up-to-date information about a patient’s condition and healthcare personnel can then come up with corresponding appropriate intervention and management measures. Monitoring the effects of daily activities on physiological responses requires sensors with excellent sensitivity. Sempionatto et al. reported a wearable sensor that allows dynamic self-monitoring of blood pressure (BP), heart rate (HR) and levels of lactate (Fig. 11d)162. The sensors were integrated with piezoelectric lead zirconate ultrasound transducers and printed hydrogel composite via solvent-soldering process. Chemical sensing starts with the introduction of an iontophoresis current from anode to cathode, allowing electro-repulsive delivery of sweat-stimulating molecule (P+, pilocarpine nitrate). Sweat-containing biomarkers (e.g., lactate, caffeine and alcohol) are then collected and quantified. The iontophoresis current leads to an osmotic flow of biomarkers (e.g., glucose) from interstitial fluid (ISF) to the skin surface, allowing their collection and the subsequent quantitative analysis. The parallel anodic and cathodic mode in the sensor allows real-time monitoring of cardiovascular parameters and biomarker levels in relation to sweat and ISF (Fig. 11e). Continuous lactate and BP were detected from a sedentary volunteer before, during, and after exercise (Fig. 11f). The current curve showed that lactate and BP of a sedentary volunteer after exercise is higher than that of before exercise (Fig. 11g-h), demonstrating that the sensor has high sensitivity for biomarkers detection and quantification.
In addition to sensors that detect chemical signals, there are strain sensors that detect physical signals via human movements. Zhao et al. reported a conductive hydrogel composed of supramolecular assembly of polydopamine modified silver nanoparticles (PDA@Ag NPs), polyaniline, and PVA for diabetic foot wound dressing and epidermal sensor (Fig. 12a)163. When attaching hydrogel sensors to ankle joints of normal and diabetic mice, motor reflection frequency can be obtained (Fig. 12b-c). Excellent conductive behavior of the hydrogel endows the epidermal sensor with high sensitivity for monitoring human activities. The sensor can not only monitor finger joint motion with current variations, but also finger motion at different angles (Fig. 12d). The sensor can also be adhered to elbow joint or knee to monitor the state of bending or deploying (Fig. 12e, f), having potential as a wearable sensor for monitoring human physiological signals.
a Synthesis of PDA@Ag NPs/CPHs and its application as both epidermal sensor and diabetic foot wound dressing simultaneously163. b Attachment of PDA@Ag NPs/CPHs to ankle joints of normal and diabetic mice on a 40 °C hot plate to monitor hydrogel sensors’ responses on the reflection movement of mice to thermal stimulus. c Motor reflection frequency during continuous thermal stimulation was recorded. It showed diabetic rats had a lower motor reflection frequency than normal rats. d–f PDA@Ag NPs/CPHs were adhered on a volunteer’s finger, elbow, knee joint, serving as strain sensors to detect motion of human body. g Resistance output from a hydrogel sensor for detecting vocal vibrations on throat164. h Movement recorded by liquid-metal-based cardiac patch inset on the surface of a beating heart of a rabbit. Reprinted with permission from refs. 163,164. Copyright 2019 John Wiley & Sons and 2019 John Wiley & Sons.
Excellent biocompatibility enables hydrogel to be made as an implantable material platform for flexible bioelectronic (e.g., cardiac patches) by incorporating Internet-of-Things and tissue-machine interfacing applications to monitor physiological parameters in vivo. Liu et al. reported a biocompatible and degradable hydrogel-based patch that monitor cardiac electrophysiological signal164. Perfusable fluidic microchannels were created on sheets of hydrogel prepared from acrylamide. Liquid metal was infused into microchannels to obtain a conductive hydrogel patch. The hydrogel patch detected vocal vibrations and distinguished different levels of volume (Fig. 12g). Owing to the biocompatibility and biodegradability of hydrogel, it can be assembled as a flexible cardiac patch to monitor the movement of heart tissues in vivo. The patch was attached to a rabbit’s heart and cardiac electrophysiological signal was recorded (Fig. 12h). Although there are many reports on the application of hydrogels for bioelectronics, it is necessary to further improve the respective detection accuracy and broaden their application range. Integration of hydrogels and other electronic materials into wearable flexible electronic devices is also of interest for better management of diabetes.
Conclusions and prospects
As a chronic disease, diabetes causes serious harm to the health and life quality of patients and is a major burden to the society. Although conventional devices and kits are readily available for diabetes diagnosis and treatment, it is critical to develop advanced technologies and devices for diabetes with improved comfortability, sensitivity, accuracy, and speed. This paper presented a brief summary on the application of hydrogel-based flexible materials and devices in blood glucose monitoring, insulin delivery, wound care, and cell transplantation for diabetes management in recent years.
Owing to their unique properties (e.g., high water content, biocompatibility, biodegradability, flexibility), hydrogels have opened up new opportunities and developments in the management and treatment of diabetes. Hydrogels possess excellent properties (e.g., physicochemical, mechanical, electrical, and optical properties) that are important to realize sensitive, accurate and rapid detection of changes in blood glucose concentration. With accurate CGM systems as the fundamentals, insulin delivery systems can be integrated on them with the aim to develop controllable and sustained insulin release systems. Hydrogels functionalized with antibacterial property are useful for combating diabetic wounds and medical devices-associated infections. One of the most appealing features of hydrogels is its similar biomechanical properties to the native ECM, providing platforms for cell transplantation and tissue engineering in diabetes treatments. Moreover, such mechanical properties expand its application range to fabricate flexible bioelectronic devices that conform to the physical and/or physiological properties of the subject (the body or tissues).
Having said that, there are also limitations of hydrogels to be overcome for expanding its potential in healthcare technologies. It is of great interest to further improve the chemical stability of hydrogels and explore their interactions with microenvironments. Hydrogels are rich in water, and they may pose a risk that could breed bacteria easily. Also, dehydration of hydrogels in long term use will influence the connection between hydrogels and electronic devices embedded, which may cause the devices cease to function. As a result, the service life and durability of hydrogel-based flexible electronics can be greatly reduced. Therefore, it is crucial to develop novel strategy to expand the applicability of hydrogels for improved service life and stability. Better material innovation, sensor or device design and fabrication, and system integration are necessary to achieve human-machine interaction and realize digital nursing management. At present, most of the applications of hydrogels in management and treatment of diabetes are still in the exploration and evaluation stage. Unfolding the potentials of hydrogels as flexible electronics for diagnosis, treatment, and management of diabetes would advance towards the vision of precision medicine while improving the health and quality life of patients.
Data availability
All data are available within the article or available from the authors upon reasonable request.
References
Slaughter, B. V., Khurshid, S. S., Fisher, O. Z., Khademhosseini, A. & Peppas, N. A. Hydrogels in regenerative medicine. Adv. Mater. 21, 3307–3329 (2009).
Zhang, Y. S. & Khademhosseini, A. Advances in engineering hydrogels. Science 356, eaaf3627 (2017).
Nele, V. et al. Tailoring gelation mechanisms for advanced hydrogel applications. Adv. Funct. Mater. 30, 2002759 (2020).
Yang, C. & Suo, Z. Hydrogel ionotronics. Nat. Rev. Mater. 3, 125–142 (2018).
Liu, H. et al. Biofriendly, stretchable, and reusable hydrogel electronics as wearable force sensors. Small 14, 1801711 (2018).
Shao, C. et al. Mimicking dynamic adhesiveness and strain-stiffening behavior of biological tissues in tough and self-healable cellulose nanocomposite hydrogels. ACS Appl. Mater. Interfaces 11, 5885–5895 (2019).
Liu, H. et al. Control of fibroblast shape in sequentially formed 3D hybrid hydrogels regulates cellular responses to microenvironmental cues. NPG Asia Mater. 1, 45 (2020).
Gyles, D. A., Castro, L. D., Silva, J. O. C. & Ribeiro-Costa, R. M. A review of the designs and prominent biomedical advances of natural and synthetic hydrogel formulations. Eur. Polym. J. 88, 373–392 (2017).
Luo, Z. et al. Biodegradable gelatin methacryloyl microneedles for transdermal drug delivery. Adv. Healthc. Mater. 8, e1801054 (2019).
Qi, X. et al. Facile formation of salecan/agarose hydrogels with tunable structural properties for cell culture. Carbohydr. Polym. 224, 115208 (2019).
Dang, Q. et al. Fabrication and evaluation of thermosensitive chitosan/collagen/alpha, beta-glycerophosphate hydrogels for tissue regeneration. Carbohydr. Polym. 167, 145–157 (2017).
Dafe, A., Etemadi, H., Dilmaghani, A. & Mahdavinia, G. R. Investigation of pectin/starch hydrogel as a carrier for oral delivery of probiotic bacteria. Int. J. Biol. Macromol. 97, 536–543 (2017).
Zu, Y. et al. Preparation and characterization of chitosan-polyvinyl alcohol blend hydrogels for the controlled release of nano-insulin. Int. J. Biol. Macromol. 50, 82–87 (2012).
Hu, C. et al. Stable, strain-sensitive conductive hydrogel with antifreezing capability, remoldability, and reusability. ACS Appl. Mater. Interfaces 10, 44000–44010 (2018).
Sharma, G. et al. Applications of nanocomposite hydrogels for biomedical engineering and environmental protection. Environ. Chem. Lett. 16, 113–146 (2018).
Qin, Z. Z. et al. Nonswellable and tough supramolecular hydrogel based on strong micelle cross-linkings. Biomacromolecules 20, 3399–3407 (2019).
Sabzi, M., Samadi, N., Abbasi, F., Mahdavinia, G. R. & Babaahmadi, M. Bioinspired fully physically cross-linked double network hydrogels with a robust, tough and self-healing structure. Mater. Sci. Eng. C: Mater. Biol. Appl. 74, 374–381 (2017).
Yang, J. W., Bai, R. B. X., Chen, B. H. & Suo, Z. G. Hydrogel adhesion: a supramolecular synergy of chemistry, topology, and mechanics. Adv. Funct. Mater. 30, 1901693 (2019).
Vermonden, T., Censi, R. & Hennink, W. E. Hydrogels for protein delivery. Chem. Rev. 112, 2853–2888 (2012).
Cheng, N. C., Lin, W. J., Ling, T. Y. & Young, T. H. Sustained release of adipose-derived stem cells by thermosensitive chitosan/gelatin hydrogel for therapeutic angiogenesis. Acta Biomater. 51, 258–267 (2017).
Wang, W., Zhang, Y. & Liu, W. Bioinspired fabrication of high strength hydrogels from non-covalent interactions. Prog. Polym. Sci. 71, 1–25 (2017).
Bao, Z., Xian, C., Yuan, Q., Liu, G. & Wu, J. Natural polymer-based hydrogels with enhanced mechanical performances: preparation, structure, and property. Adv. Healthc. Mater. 8, e1900670 (2019).
Seo, B. B., Park, M. R. & Song, S. C. Sustained release of exendin 4 using injectable and ionic-nano-complex forming polymer hydrogel system for long-term treatment of type 2 diabetes mellitus. ACS Appl. Mater. Interfaces 11, 15201–15211 (2019).
Farhoudi, N. et al. Smart hydrogel micromechanical resonators with ultrasound readout for biomedical sensing. ACS Sens. 5, 1882–1889 (2020).
Li, J. et al. Tough composite hydrogels with high loading and local release of biological drugs. Adv. Healthc. Mater. 7, e1701393 (2018).
Wu, M. et al. A smart hydrogel system for visual detection of glucose. Biosens. Bioelectron. 142, 111547 (2019).
Lee, H. et al. Wearable/disposable sweat-based glucose monitoring device with multistage transdermal drug delivery module. Sci. Adv. 3, e1601314 (2017).
He, R. et al. A hydrogel microneedle patch for point-of-care testing based on skin interstitial fluid. Adv. Healthc. Mater. 9, e1901201 (2020).
Elsherif, M., Hassan, M. U., Yetisen, A. K. & Butt, H. Hydrogel optical fibers for continuous glucose monitoring. Biosens. Bioelectron. 137, 25–32 (2019).
Daly, A. C., Riley, L., Segura, T. & Burdick, J. A. Hydrogel microparticles for biomedical applications. Nat. Rev. Mater. 5, 20–43 (2019).
Lei, Z., Wang, Q., Sun, S., Zhu, W. & Wu, P. A bioinspired mineral hydrogel as a self-healable, mechanically adaptable ionic skin for highly sensitive pressure sensing. Adv. Mater. 29, 1700321 (2017).
Cho, N. H. et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 138, 271–281 (2018).
Cho, J., Pandol, S. J. & Petrov, M. S. Risk of cause-specific death, its sex and age differences, and life expectancy in post-pancreatitis diabetes mellitus. Acta Diabetol. 58, 797–807 (2021).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14, 88–98 (2018).
Reyes-Martinez, J. E. et al. Advanced hydrogels for treatment of diabetes. J. Tissue Engz. Regen. Med. 13, 1375–1393 (2019).
Sabu, C., Henna, T. K., Raphey, V. R., Nivitha, K. P. & Pramod, K. Advanced biosensors for glucose and insulin. Biosens. Bioelectron. 141, 111201 (2019).
Kim, J., Campbell, A. S. & Wang, J. Wearable non-invasive epidermal glucose sensors: a review. Talanta 177, 163–170 (2018).
Klatman, E. L., Jenkins, A. J., Ahmedani, M. Y. & Ogle, G. D. Blood glucose meters and test strips: global market and challenges to access in low-resource settings. Lancet Diabetes Endocrinol. 7, 150–160 (2019).
Bandodkar, A. J. et al. Re-usable electrochemical glucose sensors integrated into a smartphone platform. Biosens. Bioelectron. 101, 181–187 (2018).
Shokrekhodaei, M. & Quinones, S. Review of non-invasive glucose sensing techniques: optical, electrical and breath acetone. Sensors 20, 1251 (2020).
Zhang, Y. et al. Advances in transdermal insulin delivery. Adv. Drug. Deliv. Rev. 139, 51–70 (2019).
Bekiari, E. et al. Artificial pancreas treatment for outpatients with type 1 diabetes: systematic review and meta-analysis. BMJ 361, k1310 (2018).
Saeedi, P. et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 157, 107843 (2019).
Alkhatib, A. et al. Functional foods and lifestyle approaches for diabetes prevention and management. Nutrients 9, 1310 (2017).
Umpierrez, G. E. & Pasquel, F. J. Management of inpatient hyperglycemia and diabetes in older adults. Diabetes Care 40, 509–517 (2017).
Zhou, Y. et al. Highly stretchable, elastic, and ionic conductive hydrogel for artificial soft electronics. Adv. Funct. Mater. 29, 1806220 (2019).
Trung, T. Q. & Lee, N. E. Flexible and stretchable physical sensor integrated platforms for wearable human-activity monitoringand personal healthcare. Adv. Mater. 28, 4338–4372 (2016).
Lin, S. et al. Stretchable hydrogel electronics and devices. Adv. Mater. 28, 4497–4505 (2016).
Chen, Y. H. et al. Skin-like biosensor system via electrochemical channels for noninvasive blood glucose monitoring. Sci. Adv. 3, e1701629 (2017).
Ma, Y. et al. Flexible hybrid electronics for digital healthcare. Adv. Mater. 32, e1902062 (2020).
Mehta, N. & Pandit, A. Concurrence of big data analytics and healthcare: a systematic review. Int. J. Med. Inform. 114, 57–65 (2018).
Fogel, A. L. & Kvedar, J. C. Artificial intelligence powers digital medicine. NPJ Digit. Med. 1, 5 (2018).
Kim, J. et al. Miniaturized battery-free wireless systems for wearable pulse oximetry. Adv. Funct. Mater. 27, 1604373 (2017).
Kim, S. B. et al. Soft, skin-interfaced microfluidic systems with wireless, battery-free electronics for digital, real-time tracking of sweat loss and electrolyte composition. Small 14, e1802876 (2018).
Sekine, Y. et al. A fluorometric skin-interfaced microfluidic device and smartphone imaging module for in situ quantitative analysis of sweat chemistry. Lab. Chip. 18, 2178–2186 (2018).
Yang, Y. & Gao, W. Wearable and flexible electronics for continuous molecular monitoring. Chem. Soc. Rev. 48, 1465–1491 (2019).
Xu, K., Lu, Y. & Takei, K. Multifunctional skin-inspired flexible sensor systems for wearable electronics. Adv. Mater. Technol. 4, 1800628 (2019).
Wang, F. et al. A flexible skin-mounted wireless acoustic device for bowel sounds monitoring and evaluation. Sci. China Inf. Sci. 62, 202402 (2019).
Kim, J., Campbell, A. S., de Avila, B. E. & Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 37, 389–406 (2019).
Wild, S., Roglic, G., Green, A., Sicree, R. & King, H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes care 27, 1047–1053 (2004).
Mauras, N., Fox, L., Englert, K. & Beck, R. W. Continuous glucose monitoring in type 1 diabetes. Endocrine 43, 41–50 (2013).
McGarraugh, G. & Bergenstal, R. Detection of hypoglycemia with continuous interstitial and traditional blood glucose monitoring using the FreeStyle Navigator Continuous Glucose Monitoring System. Diabetes Technol. Ther. 11, 145–150 (2009).
Dovc, K., Bratina, N. & Battelino, T. A new horizon for glucose monitoring. Horm. Res. Paediatr. 83, 149–156 (2015).
Lee, I., Probst, D., Klonoff, D. & Sode, K. Continuous glucose monitoring systems - Current status and future perspectives of the flagship technologies in biosensor research. Biosens. Bioelectron. 181, 113054 (2021).
Heo, Y. J., Shibata, H., Okitsu, T., Kawanishi, T. & Takeuchi, S. Long-term in vivo glucose monitoring using fluorescent hydrogel fibers. Proc. Natl Acad. Sci. USA 108, 13399–13403 (2011).
Shibata, H. et al. Injectable hydrogel microbeads for fluorescence-based in vivo continuous glucose monitoring. Proc. Natl Acad. Sci. USA 107, 17894–17898 (2010).
Zeng, Y. et al. Colloidal crystal microneedle patch for glucose monitoring. Nano Today 35, 100984 (2020).
Sawayama, J. & Takeuchi, S. Long-term continuous glucose monitoring using a fluorescence-based biocompatible hydrogel glucose sensor. Adv. Healthc. Mater. 10, e2001286 (2021).
Gu, Z. et al. Injectable nano-network for glucose-mediated insulin delivery. ACS Nano 7, 4194–4201 (2013).
Yin, R. et al. Design of genipin-crosslinked microgels from concanavalin A and glucosyloxyethyl acrylated chitosan for glucose-responsive insulin delivery. Carbohydr. Polym. 103, 369–376 (2014).
Steiner, M. S., Duerkop, A. & Wolfbeis, O. S. Optical methods for sensing glucose. Chem. Soc. Rev. 40, 4805–4839 (2011).
Wang, J. et al. Glucose-responsive insulin and delivery systems: innovation and translation. Adv. Mater. 32, e1902004 (2020).
Dou, Q. et al. High performance boronic acid-containing hydrogel for biocompatible continuous glucose monitoring. RSC Adv. 7, 41384–41390 (2017).
Yetisen, A. K. et al. Glucose-sensitive hydrogel optical fibers functionalized with phenylboronic acid. Adv. Mater. 29, 1606380 (2017).
Gupta, V. K. et al. A novel glucose biosensor platform based on Ag@AuNPs modified graphene oxide nanocomposite and SERS application. J. Colloid Interf. Sci. 406, 231–237 (2013).
Dautta, M., Alshetaiwi, M., Escobar, J. & Tseng, P. Passive and wireless, implantable glucose sensing with phenylboronic acid hydrogel-interlayer RF resonators. Biosens. Bioelectron. 151, 112004 (2020).
Chen, C. et al. Current and emerging technology for continuous glucose monitoring. Sensors 17, 182 (2017).
Villiger, M. et al. Evaluation and review of body fluids saliva, sweat and tear compared to biochemical hydration assessment markers within blood and urine. Eur. J. Clin. Nutr. 72, 69–76 (2018).
Chu, M. X. et al. Soft contact lens biosensor for in situ monitoring of tear glucose as non-invasive blood sugar assessment. Talanta 83, 960–965 (2011).
Yao, H., Shum, A. J., Cowan, M., Lahdesmaki, I. & Parviz, B. A. A contact lens with embedded sensor for monitoring tear glucose level. Biosens. Bioelectron. 26, 3290–3296 (2011).
Kumagai, A. K., Glasgow, B. J. & Pardridge, W. M. Glut1 glucose-transporter expression in the diabetic and nondiabetic human eye. Invest. Ophthalmol. Vis. Sci. 35, 2887–2894 (1994).
Moyer, J., Wilson, D., Finkelshtein, I., Wong, B. & Potts, R. Correlation between sweat glucose and blood glucose in subjects with diabetes. Diabetes Technol. Ther. 14, 398–402 (2012).
Elsherif, M., Hassan, M. U., Yetisen, A. K. & Butt, H. Glucose sensing with phenylboronic acid functionalized hydrogel-based optical diffusers. ACS Nano 12, 2283–2291 (2018).
Kim, G. J., Yoon, K. J. & Kim, K. O. Glucose-responsive poly(vinyl alcohol)/β-cyclodextrin hydrogel with glucose oxidase immobilization. J. Mater. Sci. 54, 12806–12817 (2019).
Locke, A. K. et al. A layer-by-layer approach to retain a fluorescent glucose sensing assay within the cavity of a hydrogel membrane. ACS Appl. Bio. Mater. 1, 1319–1327 (2018).
VandenBerg, M. A. & Webber, M. J. Biologically inspired and chemically derived methods for glucose-responsive insulin therapy. Adv. Healthc. Mater. 8, e1801466 (2019).
Chen, S. et al. Smart microneedle fabricated with silk fibroin combined semi-interpenetrating network hydrogel for glucose-responsive insulin delivery. ACS Biomater. Sci. Eng. 5, 5781–5789 (2019).
Demirdirek, B. & Uhrich, K. E. Novel salicylic acid-based chemically crosslinked pH-sensitive hydrogels as potential drug delivery systems. Int. J. Pharm. 528, 406–415 (2017).
Fan, L. et al. Responsive hydrogel microcarrier-integrated microneedles for versatile and controllable drug delivery. Adv. Healthc. Mater. 10, e2002249 (2021).
Li, X. et al. pH-sensitive peptide hydrogel for glucose-responsive insulin delivery. Acta Biomater. 51, 294–303 (2017).
Wang, J. et al. Core-shell microneedle gel for self-regulated insulin delivery. ACS Nano 12, 2466–2473 (2018).
Wang, J. et al. Injectable biodegradable polymeric complex for glucose-responsive insulin delivery. ACS Nano 15, 4294–4304 (2021).
Zhao, F. et al. An injectable particle-hydrogel hybrid system for glucose-regulatory insulin delivery. Acta Biomater. 64, 334–345 (2017).
Yin, R., Tong, Z., Yang, D. & Nie, J. Glucose and pH dual-responsive concanavalin A based microhydrogels for insulin delivery. Int. J. Biol. Macromol. 49, 1137–1142 (2011).
Lin, K. et al. Glucose-sensitive hydrogels from covalently modified carboxylated pullulan and concanavalin A for smart controlled release of insulin. React. Funct. Polym. 139, 112–119 (2019).
Ge, L. et al. Development of self-emulsifying nanoplatform as anti-diabetic sulfonylurea carrier for oral diabetes therapy. J. Biomed. Nanotechnol. 13, 931–945 (2017).
Al Rubeaan, K., Rafiullah, M. & Jayavanth, S. Oral insulin delivery systems using chitosan-based formulation: a review. Expert. Opin. Drug Deliv. 13, 223–237 (2016).
Li, L. et al. A composite hydrogel system containing glucose-responsive nanocarriers for oral delivery of insulin. Mater. Sci. Eng. C: Mater. Biol. Appl. 69, 37–45 (2016).
Sun, Q., Zhang, Z., Zhang, R., Gao, R. & McClements, D. J. Development of functional or medical foods for oral administration of insulin for diabetes treatment: gastroprotective edible microgels. J. Agric. Food Chem. 66, 4820–4826 (2018).
Meneguin, A. B., Beyssac, E., Garrait, G., Hsein, H. & Cury, B. S. F. Retrograded starch/pectin coated gellan gum-microparticles for oral administration of insulin: a technological platform for protection against enzymatic degradation and improvement of intestinal permeability. Eur. J. Pharm. Biopharm. 123, 84–94 (2018).
Harloff-Helleberg, S., Nielsen, L. H. & Nielsen, H. M. Animal models for evaluation of oral delivery of biopharmaceuticals. J. Control. Release 268, 57–71 (2017).
Gedawy, A., Martinez, J., Al-Salami, H. & Dass, C. R. Oral insulin delivery: existing barriers and current counter-strategies. J. Pharm. Pharmacol. 70, 197–213 (2018).
Qi, X., Yuan, Y., Zhang, J., Bulte, J. W. M. & Dong, W. Oral administration of salecan-based hydrogels for controlled insulin delivery. J. Agric. Food Chem. 66, 10479–10489 (2018).
Liu, L. et al. Dual stimuli-responsive nanoparticle-incorporated hydrogels as an oral insulin carrier for intestine-targeted delivery and enhanced paracellular permeation. ACS Biomater. Sci. Eng. 4, 2889–2902 (2018).
Marchioli, G. et al. Fabrication of three-dimensional bioplotted hydrogel scaffolds for islets of Langerhans transplantation. Biofabrication 7, 025009 (2015).
Foster, G. A. & Garcia, A. J. Bio-synthetic materials for immunomodulation of islet transplants. Adv. Drug Deliv. Rev. 114, 266–271 (2017).
Shrestha, P., Regmi, S. & Jeong, J.-H. Injectable hydrogels for islet transplantation: a concise review. J. Pharm. Investig. 50, 29–45 (2019).
Szabó, L. et al. Cross-reactive alginate derivatives for the production of dual ionic–covalent hydrogel microspheres presenting tunable properties for cell microencapsulation. ACS Appl. Polym. Mater. 1, 1326–1333 (2019).
An, D. et al. Designing a retrievable and scalable cell encapsulation device for potential treatment of type 1 diabetes. Proc. Natl Acad. Sci. USA 115, E263–E272 (2018).
Dimitrioglou, N., Kanelli, M., Papageorgiou, E., Karatzas, T. & Hatziavramidis, D. Paving the way for successful islet encapsulation. Drug Discov. Today 24, 737–748 (2019).
Kumar, M., Gupta, P., Bhattacharjee, S., Nandi, S. K. & Mandal, B. B. Immunomodulatory injectable silk hydrogels maintaining functional islets and promoting anti-inflammatory M2 macrophage polarization. Biomaterials 187, 1–17 (2018).
Cheng, Y., Yu, Y., Zhang, Y., Zhao, G. & Zhao, Y. Cold-responsive nanocapsules enable the sole-cryoprotectant-trehalose cryopreservation of beta cell-laden hydrogels for diabetes treatment. Small 15, e1904290 (2019).
Richardson, T., Barner, S., Candiello, J., Kumta, P. N. & Banerjee, I. Capsule stiffness regulates the efficiency of pancreatic differentiation of human embryonic stem cells. Acta Biomater. 35, 153–165 (2016).
Ernst, A. U., Wang, L. H. & Ma, M. Interconnected toroidal hydrogels for islet encapsulation. Adv. Healthc. Mater. 8, e1900423 (2019).
Chen, Y., Nguyen, D. T., Kokil, G. R., Wong, Y. X. & Dang, T. T. Microencapsulated islet-like microtissues with toroid geometry for enhanced cellular viability. Acta Biomater. 97, 260–271 (2019).
Liu, S., Zhang, L., Cheng, J., Lu, Y. & Liu, J. Sustained release of hepatocyte growth factor by cationic self-assembling peptide/heparin hybrid hydrogel improves beta-cell survival and function through modulating inflammatory response. Int. J. Nanomed. 11, 4875–4890 (2016).
Mao, D. et al. A macroporous heparin-releasing silk fibroin scaffold improves islet transplantation outcome by promoting islet revascularisation and survival. Acta Biomater. 59, 210–220 (2017).
Ferrara, N. & Kerbel, R. S. Angiogenesis as a therapeutic target. Nature 438, 967–974 (2005).
Rouwkema, J., Rivron, N. C. & van Blitterswijk, C. A. Vascularization in tissue engineering. Trends Biotechnol. 26, 434–441 (2008).
Marchioli, G. et al. Hybrid polycaprolactone/alginate scaffolds functionalized with vegf to promote de novo vessel formation for the transplantation of islets of langerhans. Adv. Healthc. Mater. 5, 1606–1616 (2016).
Vijayakumar, V., Samal, S. K., Mohanty, S. & Nayak, S. K. Recent advancements in biopolymer and metal nanoparticle-based materials in diabetic wound healing management. Int. J. Biol. Macromol. 122, 137–148 (2019).
Blakytny, R. & Jude, E. The molecular biology of chronic wounds and delayed healing in diabetes. Diabet. Med. 23, 594–608 (2006).
Kasiewicz, L. N. & Whitehead, K. A. Recent advances in biomaterials for the treatment of diabetic foot ulcers. Biomater. Sci. 5, 1962–1975 (2017).
Koivukangas, V., Annala, A. P., Samela, P. I. & Oikarinen, A. Delayed restoration of epidermal barrier function after suction blister injury in patients with diabetes mellitus. Diabet. Med. 16, 563–567 (1999).
Jeffcoate, W. J. & Harding, K. G. Diabetic foot ulcers. Lancet 361, 1545–1551 (2003).
Malone-Povolny, M. J., Maloney, S. E. & Schoenfisch, M. H. Nitric oxide therapy for diabetic wound healing. Adv. Healthc. Mater. 8, e1801210 (2019).
Wang, T. J. et al. Targeted polymer-based antibiotic delivery system: A promising option for treating bacterial infections via macromolecular approaches. Prog. Polym. Sci. 16, 101389 (2021).
Sliva, L. D., Carvalho, E. & Cruz, M. T. Role of neuropeptides in skin inflammation and its involvement in diabetic wound healing. Expert Opin. Biol. Ther. 10, 1427–1439 (2010).
Falanga, V. Wound healing and its impairment in the diabetic foot. Lancet 366, 1736–1743 (2005).
Moura, L. I., Dias, A. M., Carvalho, E. & de Sousa, H. C. Recent advances on the development of wound dressings for diabetic foot ulcer treatment-a review. Acta Biomater. 9, 7093–7114 (2013).
Winter, G. D. Formation of the scab and the rate of epithelization of superficial wounds in the skin of the young domestic pig. Nature 193, 293 (1962).
Bullock, A. J. et al. Development of a calcium-chelating hydrogel for treatment of superficial burns and scalds. Regen. Med. 5, 55–64 (2010).
Xu, Z., Han, S., Gu, Z. & Wu, J. Advances and impact of antioxidant hydrogel in chronic wound healing. Adv. Healthc. Mater. 9, e1901502 (2020).
Wang, H., Xu, Z., Zhao, M., Liu, G. & Wu, J. Advances of hydrogel dressings in diabetic wounds. Biomater. Sci. 9, 1530–1546 (2021).
Pang, Q. et al. Smart flexible electronics-integrated wound dressing for real-time monitoring and on-demand treatment of infected wounds. Adv. Sci. 7, 1902673 (2020).
Khan, M. I. et al. To decipher the antibacterial mechanism and promotion of wound healing activity by hydrogels embedded with biogenic Ag@ZnO core-shell nanocomposites. Chem. Eng. J. 417, 128025 (2021).
Lu, S. et al. Mussel-inspired blue-light-activated cellulose-based adhesive hydrogel with fast gelation, rapid haemostasis and antibacterial property for wound healing. Chem. Eng. J. 417, 129329 (2021).
Kaur, R. & Liu, S. Antibacterial surface design-Contact kill. Prog. Surf. Sci. 91, 136–153 (2016).
Salwiczek, M. et al. Emerging rules for effective antimicrobial coatings. Trends Biotechnol. 32, 82–90 (2014).
Krishnamoorthy, M., Hakobyan, S., Ramstedt, M. & Gautrot, J. E. Surface-initiated polymer brushes in the biomedical field: applications in membrane science, biosensing, cell culture, regenerative medicine and antibacterial coatings. Chem. Rev. 114, 10976–11026 (2014).
Li, P. et al. A polycationic antimicrobial and biocompatible hydrogel with microbe membrane suctioning ability. Nat. Mater. 10, 149–156 (2011).
Liu, Y. et al. Silver nanoparticle-embedded hydrogel as a photothermal platform for combating bacterial infections. Chem. Eng. J. 382, 122990 (2020).
Wang, P. et al. In situ formed anti-inflammatory hydrogel loading plasmid DNA encoding VEGF for burn wound healing. Acta Biomater. 100, 191–201 (2019).
Carthew, J. et al. In situ miRNA delivery from a hydrogel promotes osteogenesis of encapsulated mesenchymal stromal cells. Acta Biomater. 101, 249–261 (2020).
Komura, F., Okuzumi, K., Takahashi, Y., Takakura, Y. & Nishikawa, M. Development of RNA/DNA hydrogel targeting toll-like receptor 7/8 for sustained RNA release and potent immune activation. Molecules 25, 728 (2020).
Ding, L. et al. A self-assembled RNA-triple helix hydrogel drug delivery system targeting triple-negative breast cancer. J. Mater. Chem. B 8, 3527–3533 (2019).
Zhou, L. et al. TET2-interacting long noncoding RNA promotes active DNA demethylation of the MMP-9 promoter in diabetic wound healing. Cell Death Dis. 10, 813 (2019).
Pordzik, J. et al. Significance of circulating microRNAs in diabetes mellitus type 2 and platelet reactivity: bioinformatic analysis and review. Cardiovasc. Diabetol. 18, 113 (2019).
Losi, P. et al. Fibrin-based scaffold incorporating VEGF- and bFGF-loaded nanoparticles stimulates wound healing in diabetic mice. Acta Biomater. 9, 7814–7821 (2013).
Bennett, N. T. & Schultz, G. S. Growth factors and wound healing: part II. role in normal and chronic wound healing. Am. J. Surg. 166, 74–81 (1993).
Adhirajan, N., Shanmugasundaram, N., Shanmuganathan, S. & Babu, M. Collagen-based wound dressing for doxycycline delivery: in-vivo evaluation in an infected excisional wound model in rats. J. Pharm. Pharmacol. 61, 1617–1623 (2009).
Adhirajan, N., Shanmugasundaram, N. & Babu, M. Gelatin microspheres cross-linked with EDC as a drug delivery system for doxycyline: development and characterization. J. Microencapsul. 24, 659–671 (2008).
Masaya, Y., Yasuhiko, T. & Yoshito, I. Growth factor release from gelatin hydrogel for tissue engineering. J. Bioactive Compatible Polym. 14, 474–489 (1999).
Shi, M. et al. Sustainable dual release of antibiotic and growth factor from ph-responsive uniform alginate composite microparticles to enhance wound healing. ACS Appl. Mater. Inter. 11, 22730–22744 (2019).
Rong, F. et al. Nitric oxide-releasing polymeric materials for antimicrobial applications: a review. Antioxidants 8, 556 (2019).
Joseph, C. A. et al. Development of an injectable nitric oxide releasing poly(ethylene) glycol-fibrin adhesive hydrogel. ACS Biomater. Sci. Eng. 5, 959–969 (2019).
Barraud, N., Kelso, M. J., Rice, S. A. & Kjelleberg, S. Nitric oxide: a key mediator of biofilm dispersal with applications in infectious diseases. Curr. Pharm. Des. 21, 31–42 (2015).
Liu, H. et al. Nitric oxide released injectable hydrogel combined with synergistic photothermal therapy for antibacterial and accelerated wound healing. Appl. Mater. Today 20, 100781 (2020).
Oh, J. Y. & Bao, Z. Second skin enabled by advanced electronics. Adv. Sci. 6, 1900186 (2019).
Niu, Y. et al. Environmentally compatible wearable electronics based on ionically conductive organohydrogels for health monitoring with thermal compatibility, anti-dehydration, and underwater adhesion. Small 17, e2101151 (2021).
Mostafalu, P. et al. Smart bandage for monitoring and treatment of chronic wounds. Small 14, e1703509 (2018).
Sempionatto, J. R. et al. An epidermal patch for the simultaneous monitoring of haemodynamic and metabolic biomarkers. Nat. Biomed. Eng. 5, 737–748 (2021).
Zhao, Y. et al. Skin-inspired antibacterial conductive hydrogels for epidermal sensors and diabetic foot wound dressings. Adv. Funct. Mater. 29, 1901474 (2019).
Liu, Y. et al. Ultrastretchable and wireless bioelectronics based on all-hydrogel microfluidics. Adv. Mater. 31, e1902783 (2019).
Acknowledgements
This work was supported by National Natural Science Foundation of China (52003224, 52073230, and 61935017), Natural Science Basic Research Program of Shaanxi Province (2020GXLH-Z-013, 2019JQ-157, and 2019KJXX-064), Projects of International Cooperation and Exchanges NSFC (51811530018), Ningbo Natural Science Foundation (202003N4051) and Fundamental Research Funds for Central Universities. T.J.W. was supported by funding from Yulin Municipal Science and Technology Bureau and the open research fund of Key Laboratory for Organic Electronics and Information Displays.
Author information
Authors and Affiliations
Contributions
J.S., Y.N.Z., and S.Y.C. wrote original draft. Z.Y.D. and Y.J.Y contributed to paper writing. T.J.W. conceptualized, investigated, and wrote original draft, P.L. and W.H. conceptualized, supervised, and edited draft. All authors participated in scientific discussion. J.S., Y.N.Z., and S.Y.C. are co-first authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, J., Zhang, Y., Chan, S.Y. et al. Hydrogel-based flexible materials for diabetes diagnosis, treatment, and management. npj Flex Electron 5, 26 (2021). https://doi.org/10.1038/s41528-021-00122-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41528-021-00122-y
This article is cited by
-
MXene-based flexible electronic materials for wound infection detection and treatment
npj Flexible Electronics (2024)
-
Nanomaterial-based biohybrid hydrogel in bioelectronics
Nano Convergence (2023)
-
Nanotherapeutics with immunoregulatory functions for the treatment of bacterial infection
Biomaterials Research (2023)
-
Designing a new alginate-fibrinogen biomaterial composite hydrogel for wound healing
Scientific Reports (2022)
-
A temperature responsive adhesive hydrogel for fabrication of flexible electronic sensors
npj Flexible Electronics (2022)