Abstract
A systematic review of literature was conducted to evaluate the effectiveness of passive countermeasures in ameliorating the cardiopulmonary and musculoskeletal effects of gravitational unloading on humans during spaceflight. This systematic review is the third of a series being conducted by the European Space Agency to evaluate the effectiveness of countermeasures to physiologic deconditioning during spaceflight. With future long-duration space missions on the horizon, it is critical to understand the effectiveness of existing countermeasures to promote astronaut health and improve the probability of future mission success. An updated search for studies examining passive countermeasures was conducted in 2021 to supplement results from a broader search conducted in 2017 for all countermeasures. Ground-based analogue and spaceflight studies were included in the search. A total of 647 articles were screened following removal of duplicates, of which 16 were included in this review. Data extraction and analysis, quality assessment of studies, and transferability of reviewed studies to actual spaceflight based on their bed-rest protocol were conducted using dedicated tools created by the Aerospace Medicine Systematic Review Group. Of the 180 examined outcomes across the reviewed studies, only 20 were shown to have a significant positive effect in favour of the intervention group. Lower body negative pressure was seen to significantly maintain orthostatic tolerance (OT) closer to baseline as comparted to control groups. It also was seen to have mixed efficacy with regards to maintaining resting heart rate close to pre-bed rest values. Whole body vibration significantly maintained many balance-related outcome measures close to pre-bed rest values as compared to control. Skin surface cooling and centrifugation both showed efficacy in maintaining OT. Centrifugation also was seen to have mixed efficacy with regards to maintaining VO2max close to pre-bed rest values. Overall, standalone passive countermeasures showed no significant effect in maintaining 159 unique outcome measures close to their pre-bed rest values as compared to control groups. Risk of bias was rated high or unclear in all studies due to poorly detailed methodologies, poor control of confounding variables, and other sources of bias (i.e. inequitable recruitment of participants leading to a higher male:female ratios). The bed-rest transferability (BR) score varied from 2–7, with a median score of 5. Generally, most studies had good BR transferability but underreported on factors such as control of sunlight or radiation exposure, diet, level of exercise and sleep-cycles. We conclude that: (1) Lack of standardisation of outcome measurement and methodologies has led to large heterogeneity amongst studies; (2) Scarcity of literature and high risk of bias amongst existing studies limits the statistical power of results; and (3) Passive countermeasures have little or no efficacy as standalone measures against cardiopulmonary and musculoskeletal deconditioning induced by spaceflight related to physiologic deterioration due to gravity un-loading.
Similar content being viewed by others
Introduction
The human body undergoes numerous adaptations during spaceflight, many of which are sustained following return to Earth1. Without gravitational force providing axial head-to-toe loading, astronauts experience thoraco-cephalic fluid redistribution, autonomic nervous system dysregulation, muscle atrophy, and bone demineralisation1. Persistent adaptations to spaceflight last for inter-individually variable periods following return to Earth. Some of these adaptations include: orthostatic intolerance2, changes in resting heart rate and heart rate variability3, exercise intolerance4, decreases in postural stability, and changes in gait5. Spaceflight induced physiological deconditioning puts astronaut health at risk as well as potentially affecting their performance in completing mission-related tasks1,6. Understanding spaceflight deconditioning and its mitigation is of the utmost importance with the onset of exploration-class missions where astronauts will be exposed to longer periods of microgravity followed by variable gravitational environments without access to large medical care and support facilities or resources. Upon landing on a planetary surface, stringent mission timelines, limited access to rehabilitation exercise equipment as well as unknown responses to rehabilitation in hypogravity environments may limit mid-mission rehabilitation efforts. Autonomous functioning of deconditioned astronauts following prolonged hypogravity exposure could threaten both life and mission. Dangerous physiologic effects following spaceflight such as presyncope, perhaps from impaired cerebral blood flow autoregulation7,8, could lead to disastrous consequences following transit to the lunar surface. Moreover, it is not known how the human body will react to being exposed to hypogravity after prolonged exposure times to microgravity as foreseen in the current ARTEMIS and Lunar Gateway mission profiles. During the Apollo era, astronauts had only ~3 days of microgravity exposure before they landed on the lunar surface, yet some fell, stumbled, and had other mishaps during their lunar surface EVAs. Current Artemis missions foresee much longer exposure times to microgravity in lunar orbit and it is not known how this will affect crewmembers' orthostatic tolerance and balance when re-exposed to hypogravity on the moon. The moon itself may serve as an effective spaceflight analogue to further research spaceflight deconditioning and can be used as testbed for countermeasures in preparation for further missions to Mars and beyond9.
Various countermeasures have been developed and employed by space agencies in order to reduce the risk to astronaut health and increase mission success1. Space agencies employ exercise programmes to counteract some of the cardiopulmonary and musculoskeletal effects of microgravity during missions to the International Space Station (ISS)10,11. However, exercise as a countermeasure is constrained by mechanical failures, as well as technical, mass and space limitations on space vessels11. Pre-establishing in-space and on-surface countermeasure equipment has been postulated as a potential solution to overcome these limitations. However, establishment and use of this equipment comes with its own set of limitations including equipment failure and wear. Added technical complexity to mission planning such as mapping exact trajectories in order to allow for docking of crewmember-containing vessels to orbiting rehabilitation-centres increases the risk of error as well as potentially increasing mission duration. Moreover, evidence suggests that exercise equipment for sustained habitation on the Moon or Mars could be relatively basic to compensate for the “lack” of gravity as simple exercises like rope skipping could be applied to provide a very potent stimulus to maintain musculoskeletal and cardiovascular integrity12,13.
Currently, exercise is the primary countermeasure modality used on the ISS. Although it significantly counteracts bone and muscle loss as well as cardiovascular deconditioning in hypogravity—the countermeasure has not been seen to completely ameliorate the adverse cardiopulmonary or musculoskeletal effects of microgravity on the human body14,15. A level of acceptable deconditioning will likely need to be established for future exploration-class missions such as the NASA Artemis program16. Optimally, this level would allow for safe and efficient completion of mission tasks whilst using the least number of resources and time necessary to achieve. Increased effort and resources have been allocated towards developing effective countermeasures to micro-gravity induced deconditioning for LDSMs on the horizon. Passive countermeasures may have a greater probability of ensuring astronaut health and supporting mission success by maintaining levels of acceptable deconditioning during exploration-class missions which exercise alone may not be able to accomplish.
In this systematic review, passive countermeasures are defined as those wherein the individual using the countermeasure does not need to exert effort for its intended use. Nutritional countermeasures are excluded from this definition as those are examined in a separate dedicated systematic review17. To our knowledge, no previous review exists which has evaluated the effectiveness of passive countermeasures as stand-alone means of ameliorating physiologic deconditioning in microgravity. Passive countermeasures are generally used in concert with other types of countermeasures. However, the use of multiple types of countermeasures makes it difficult to discern which countermeasure is affecting measured outcomes and to what efficacy. In order to best establish passive countermeasure effectiveness, they must be examined as standalone measures.
Thus, the aim of this review is to examine the effectiveness of standalone passive countermeasures in preventing cardiopulmonary and musculoskeletal deconditioning in humans due to gravitational unloading in both spaceflight and ground-based analogue studies.
Results
Results by passive countermeasure
Although many passive countermeasures have been developed over the last few decades, this review identified five passive countermeasures which have been tested in space analogue studies and were of sufficient quality to be included. Briefly, they include:
Human centrifugation
Centrifugation involves replacing lost axial loading by gravitational force which humans experience on Earth with induced centripetal force, a countermeasure termed “artificial gravity (AG)”18. This force is created through the rotation of an arm at constant velocity around an axis. Space flight size constraints limit short arm centrifuges to a radius of 2 m19. In order to create sufficient centrifugal forces to mimic 1-g at the heart using such a short radius, a high rotation rate must be accomplished as the amplitude of centripetal acceleration is directly related to axis arm length18. Due to the high spin-rate, there is an increased risk of astronauts experiencing Coriolis cross-coupled illusion which can lead to disorientation and motion sickness20. Long-axis centrifuges have the potential to decrease the risk of Coriolis cross-couples illusion as lower spin rates are required to achieve 1 g as compared to their short-axis counterparts. However, many limitations exist which limit these centrifuges’ operational viability. Due to their mass and size, these centrifuges will likely have to be external to the vessel. Additionally, a large external centrifuge will impact navigational trajectory which must be compensated for through expenditure of increased amounts of fuel and added complexity to navigation.
Lower body negative pressure (LBNP)
LBNP is designed to counteract the thoraco-cephalic fluid shifts experienced in microgravity by simulating gravitational fluid shifts experienced on Earth21. The countermeasure also simulates some of the mechanical loading experienced terrestrially and which is lost during spaceflight22. Suits that provide LBNP during spaceflight have been used by Russian cosmonauts on the ISS21 and a National Aeronautics and Space Administration (NASA)-supported research team has recently developed a mobile LBNP suit for potential use during exploration-class missions23.
Thigh cuffs
Thigh cuffs (aka “bracelets”) apply about 30–40 mmHg of pressure to the thighs in order to reduce venous return to the heart from the lower extremities during spaceflight in order to reduce thoraco-cephalic fluid shift24. These devices have been used by Russian cosmonauts for many years, initially to counter the so-called “puffy-face-bird-leg” syndrome24.
Skin surface cooling
Skin surface cooling (SSC) may improve orthostatic tolerance through activation of the sympathetic nervous system, reduction in skin blood flow, increase in mean arterial pressures and preservation of cerebral blood flow velocity. Currently, astronauts wear water-cooled suits only for re-entry or for research purposes25.
Whole body vibration (WBV)
WBV consists of providing 15–45 Hz of sinusoidal vibration to the bottom of the feet through a vibrational platform26. The countermeasure works to preserve postural stability by limiting the sensorimotor adaptations which occur in microgravity due to the lack of tactile inputs which normally occur during ambulation on Earth6. In those muscles integral for postural stability, these inputs may lead to strength retention as they serve as a surrogate to normal terrestrial muscle loading 26.
Notably, there are numerous limitations to consider regarding the operational implementation of WBV for LDSMs. Firstly, WBV may impact microgravity research on crystalline structures through unintended vibrational disruption of these structures27. Current Microgravity Vibration Isolation Mounts such as those used on the ISS may be insufficient to attenuate the much larger levels of vibration transmitted through the vessel during WBV. Low amplitude vibration also increases the number of corrective saccadic eye movements needed to visually track a point stimulus28. Increasing vibrational exposure of crewmembers could therefore impact vision and coordination during LDSMs. Lastly, the energy dissipated through vibration could impact and damage electronics, further elucidating the importance of isolating vibrational instrumentation.
Characteristics of reviewed studies
Of the 16 included studies, 9 were randomised control trials (RCTs)19,25,26,29,30,31,32,33,34 whereas 7 were control trials (CTs)35,36,37,38,39,40,41. All included studies were ground-based analogue studies utilising bed rest (BR) to simulate microgravity-induced physiologic deconditioning. BR period durations of the included studies varied from 7 days to 90 days, with the median being 21 days. A total of 207 participants were included across all the studies. The median number of participants was 11. Only four of the studies included female participants25,26,31,33 with a total of 33 female participants. The mean age of participants was 32.5 years (SD = ± 5.20 years).
Nine broad outcome measures reported in the studies were consistent with those included in our search strategy (Table 1). Seven of the studies were conducted in campaigns which included the same participants in countermeasure and control groups19,32,33,34,35,36,39. Varying periods of time separated control and countermeasure campaigns in these studies. The remainder of the studies used different participants for control and countermeasure groups. Eleven of the included studies reported cardiopulmonary outcome measures25,29,30,32,33,34,35,36,38,39,41, 4 included musculoskeletal performance outcome measures19,26,33,37, and two studies included skeletal anthropometric outcome measures31,40. A total of five different passive countermeasures were tested across all 16 included studies: centrifugation, LBNP, thigh cuffs, SSC, and WBV.
Quality assessment of included studies
The results of the risk bias assessment are shown in Table 2. Both assessment tools showed an unclear or high risk of bias in all studies.
Bed rest transferability
BR transferability results are summarised in Table 2.
The average BR transferability score was 4.75 with a SD of 1.57. Overall, BR transferability for the included studies varied greatly with a median score of 5. Mostly, a lack of information included within a study’s methodologies contributed to a low score.
Main outcome parameters
Cardiopulmonary outcome measures
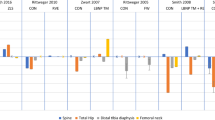
Effect sizes comparing control and countermeasure groups for cardiopulmonary outcome measures are displayed in Fig. 1.
Effect size plot of cardiopulmonary outcomes categorised into “VO2max”, “Orthostatic Tolerance”, and “Heart Rate”. Mean differences between pre and post bed rest values between control and intervention groups were used to calculate effect sizes. Effect sizes were calculated with Hedges’ G and bias corrected for sample size with a confidence interval of 95%. A positive value on the x-axis demonstrates positive effect of the intervention whereas a negative value demonstrates negative effect of the intervention on the outcome. LBNP is lower-body negative pressure, HDT is head-down tilt, HR is heart rate, OT is orthostatic tolerance, OTT is orthostatic tolerance time (stand test).
Peak power
Neither intermittent nor continuous centrifugation were found to have any significant effect on peak power as an outcome measure33.
VO2Max
Continuous centrifugation was found to have a positive effect on relative and absolute VO2max in one study41. However, data from two other studies showed no significant positive or negative effect of centrifugation on VO2max32,33.
OT
Intermittent centrifugation was found to have a significant positive effect on OT, however continuous centrifugation was not32. LBNP data showed that the countermeasure had a significant positive effect when orthostatic tolerance times (OTTs) were compared pre-HDT and after 21 days BR of but not after 10 days of BR29,30. Thigh cuffs were not seen to have a significant effect on OTTs34,35,39. Skin surface cooling was seen to have a significant positive effect on Cumulative Stress Index, an outcome measure of OT25.
Heart rate
LBNP was found to have a significant positive effect on HR mean variation three days post-HDT36. However, the countermeasure did not have a significant effect on HR one day post-HDT36 or in other reviewed studies30,38. Thigh cuffs35,39 and skin surface cooling25 were not found to have significant effects on HR either.
Effect size plots for musculoskeletal performance and skeletal anthropometric outcome measures are available as Supplementary Figs. 1 and 2, respectively, as they are too large for inclusion in the main text. Table 3 summaries the results from all the effect size plots.
Musculoskeletal performance outcome measures
Effect sizes comparing control and countermeasure groups for musculoskeletal performance outcome measures are summarised in Table 3.
Jump Performance
Neither continuous nor intermittent centrifugation were found to have significant effects on outcome measures related to jumping19.
Muscle strength
Neither centrifugation19,33 nor WBV were found to have significant effects on muscle strength-related outcome measures26.
Gait
LBNP was not found to have a significant effect on gait37.
Balance
Whole Body Vibration was found to have a significant positive effect on many balance-related outcome measures such as anterior-posterior root mean squared velocity with eyes closed at 90 days post-BR; but with no significant effect on others such as anterior-posterior root mean squared velocity with eyes open at 90 days post-BR26. Lower Body Negative Pressure was not found to have any significant effect on balance37.
Skeletal anthropometrics
Effect sizes comparing control and countermeasure groups for skeletal anthropometric outcome measures are summarised in Table 3.
Bone Mineral Density
Whole body vibration was found to only have a significant positive effect on ultrasound velocity when baseline data was compared to day 60 data31. Ultrasound Velocity (UV) is a component of quantitative ultrasound (QUS), which has been shown to be correlated with BMD in assessing for osteopenia42. Otherwise, the countermeasure was not found to have any significant effect on BMD-related outcome measures31. Continuous centrifugation was seen to have a significant negative effect on distal polar strength-strain index40. Otherwise, continuous centrifugation was not found to have significant effects on any other BMD-related outcome measure40.
Discussion
The results of this systematic review indicate that there are minimal effects of stand-alone passive countermeasures on cardiopulmonary and musculoskeletal outcomes. Additionally, quality of reviewed literature is poor due to high or unclear risks of biases. There is also large heterogeneity between studies, large variations in BR transferability criteria, a lack of standardisation between studies and a paucity of literature resulting in poor statistical power of results.
As with Sandal et al.17, this review sought articles examining outcomes in predefined domains within cardiopulmonary and musculoskeletal outcome measures. The absence of standardised outcome measures across the reviewed studies resulted in an inability to conduct a meta-analysis and limited data pooling of results. In fact, many of the reviewed findings are from single studies presenting unique outcome measures. Therefore, a high risk of bias exists with reporting on current findings with recommendations.
The risk of bias within the studies was either high or unclear, mostly attributed to insufficient description of methodologies. None of the RCTs included details of allocation concealment during randomisation19,25,26,29,30,31,32,33,34. However, given the nature of passive countermeasures, blinding of participants may be difficult as participants in the intervention groups undergo daily regimens of obvious countermeasure interventions. Additionally, most of the included RCTs35,36,37,38,39,40,41 and all of the reviewed CTs19,29,30,32,34 included only male participants or had a majority of male participants25. The inequitable recruitment of female participants in studies results in a lack of adequate understanding of gender-based differences in the physiologic response to spaceflight43. It is highly likely that these differences can have significant impacts on exploration-class mission crewmember health and mission success43.
Widely varied BR transferability scores amongst the reviewed studies make direct transfer of review outcomes to actual spaceflight difficult. Although, all the reviewed studies used head-down head tilt BR—various confounding factors may have influenced outcomes to differ from results that would be observed during space flight. For instance adequacy of sleep has been shown to effect athletic performance44, muscle strength45, and postural stability46. Yet, only four studies reported control of the sleep-wake cycles of their participants19,26,40,41.
Lower BR transferability scores were largely due to studies not mentioning whether or not certain confounding measures were being controlled. Unfortunately, while perfect simulation of the spaceflight environment is impossible, the validity of direct transfer of the results of microgravity simulation studies to actual spaceflight is likely decreased with low BR transferability score. In this review, none of the outcomes have been pooled and therefore results from reviews with differing BR transferability scores can only be observed independently from one another. Studies examining similar outcome measures but with differing levels of control of confounding variables seem to generally observe similar results with regards to whether or not the examined passive countermeasure had significant positive, negative or no significant effects on outcome measures. It cannot be stated with confidence that the results and conclusions from this review have direct validity for actual spaceflight.
Cardiopulmonary deconditioning during spaceflight presents a major risk to astronaut health47. Heart rate decreases in the microgravity environment due to the absence of head-to-foot gravitational force, altering venous return and resulting in structural and functional changes that can persist following return to Earth47. Heart rate variability has been used to reflect cardiopulmonary deconditioning in returning astronauts3. By reducing venous return to the heart, LBNP simulates some of the gravitational stress experienced by the cardiovascular system on Earth21. The current results are mixed in showing either positive36 or no significant effect of standalone passive countermeasures on HR30,38. It is therefore uncertain if LBNP as a standalone intervention can sufficiently simulate normal physiological stressors on the cardiovascular system to counteract microgravity induced changes to HR. Notably, the positive effect of LBNP on mean HR variation was significant at 3-days post-HDT but not at 1-day post-HDT. One possible explanation for this pertains to the impact of LBNP on the cardiovascular system’s baroreflex feedback loop. Through fluid redistribution and reduction of venous return, LBNP during HDT helps decrease stroke volume, which triggers baroreceptors in the heart and carotid artery to increase heart rate in order to maintain cardiac output (product of heart rate and stroke volume)48. This feedback mechanism may not have a significant impact after 1-day post-HDT due to the initial sudden redistribution of fluid (and therefore rapid reduction in heart rate) but may significantly normalise HR to baseline levels by day 3 post-HDT.
Notably, heart rate was also not significantly affected by other passive countermeasures such as thigh cuffs35,39 and skin surface cooling25.
Decreases in orthostatic tolerance from alterations in autonomic arterial pressure49 and postural vasoconstrictor response2 have been seen in those returning from spaceflight. LBNP may limit some of the cardiovascular remodelling which occurs in microgravity through provision of “gravity-like” stress on the cardiovascular system50. Maintenance of intravascular fluid volume, normalisation of cardiac filling pressures during orthosis, and limitations in cerebral circulatory changes have all been posited as possible explanations as to how the countermeasure can prevent losses in orthostatic tolerance50.
In this review, LBNP was seen to improve OTTs during stand-tests following 21 days of BR vs. controls29,30. However, it had no significant effect on the same outcome measure following 10 days of BR29. Intermittent centrifugation was also seen to have a positive effect on OTT, which the authors found was not related to maintenance of blood volume32. Instead, AG is theorised to improve the outcome measure via multiple mechanisms which overall improve sympathetic response to orthostatic loading32,41. In the absence of gravitational forces, vasoreactivity of vessels throughout the body are altered secondary to remodelling of vascular smooth muscle51. Vasoreactivity increases in cerebral vessels in order to compensate for cerebral hypertension whereas lower limb vessels experience decreases in vasoreactivity51. Thus, sympathetic response to orthostatic tolerance is altered due to vascular adaptation. Intermittent AG has been theorised to counteract this vascular adaptation by simulating Earth-like gravitational stress of the cardiovascular system and therefore improving orthostatic tolerance51. Supporting this theory, thigh cuffs were not seen to have a significant effect on OTT as they are designed to only maintain plasma volume in the lower limbs34,35,39. It is uncertain as to why the positive effects of centrifugation on OTT were not also seen with continuous centrifugation protocols32. Skin surface cooling was also found to have a positive effect on OT as indicated by an “Cumulative Stress Index” (CSI)25. Cumulative Stress Index was calculated in this study by summing the product of applied negative pressure with the duration of pressure stimulus during LBNP session stages25. The authors of this study postulated that this improvement in CSI was due to skin cooling increasing arterial pressure during the study25. Other proposed mechanisms include: attenuation in reduction of cerebral blood flow velocity and improvements in sympathetic responses to orthostatic loading52.
It is well known that astronauts returning from spaceflight experience reductions in exercise capacity due to physical deconditioning. Aerobic exercise capacity (VO2max) decreases following spaceflight which has been historically postulated as being due to decreases in blood volume53. A more recent study examining mechanistic components of oxygen transport demonstrated that decreases in VO2max may instead be due to decreases in O2 transport which are affected by cardiovascular system remodelling54. Although centrifugation has been seen to perhaps eliminate cardiovascular autonomic changes in microgravity, it has not been shown to improve exercise capacity as a stand-alone countermeasure55 which was also seen in another study32,33. However, the results from the reviewed studies which showed significant positive effects may have been skewed due to participants performing knee bends and heel raises while using the countermeasure41.
Deteriorations in postural stability following spaceflight are thought to be due, in part, to sensorimotor adaptations6. These adaptations may occur due to the lack of somatosensory input which humans are accustomed to on Earth6. Tactile inputs are important for the preparatory activations which allow for maintenance of postural stability6. In astronauts, the absence of these tactile inputs results in alterations in sensitivity to high and low frequency vibrations to their feet, which causes postural instability and alterations in walking6. In this way WBV can significantly improve balance-related outcome measures as seen in this review26. However, this positive effect was not ubiquitous across all the study conditions. It seems that comparisons of baseline data with BR-day 90 data more often showed no significant effect of the countermeasure. Whereas baseline data vs. BR-day 60 data showed more instances of significant positive effect. This may be due to maximal deterioration in postural stability occurring within 60 days as well as further muscle and endurance deteriorations as the study period progressed26. Eyes closed conditions also generally favoured the intervention while eyes open conditions more often showed no significant effect. The authors of the reviewed study postulate that this is due to the importance of visual cues in maintaining balance26. Therefore, in the eyes closed conditions, visual cues could not be used by the body to compensate for deteriorations in postural stability caused by deconditioning26. Although OT may play a role in balance, it does not appear to be significant as LBNP-induced improvements in OT did not correlate with significant effects on balance nor gait37. Therefore, sensorimotor pathways may play a larger role preserving postural stability as opposed to fluid-balance and cardiovascular remodelling. Likely, the sensorimotor adaptation which occurs in microgravity cannot be compensated for with improvements in other systems through LBNP6.
Significant muscle atrophy is seen in even short duration space flight56. Weight-bearing muscles and those used for gait such as the quadriceps femoris, hamstrings, sartorius, gracilis and triceps surae have been seen to significantly decrease in volume following spaceflight, most likely due to atrophy from the absence of axial loading57. The positive benefits previously seen using WBV on plantar flexor and dorsiflexor muscle strength58 were not seen in this review26. Centrifugation also seems to not provide sufficient loading to preserve muscle strength19,33 nor preserve jump-related outcome measures19. In the absence of gait and continuous loading by gravity, lower limb muscles will undergo substantial atrophy as loading cannot be sufficiently mimicked with short sessions of centrifugation nor loading through WBV.
Similar to muscle atrophy caused by unloading, disuse osteopenia presents a significant threat to astronaut health during exploration-class missions31,40. WBV has been seen in some studies to increase BMD and bone anabolism and has even been theorised as a treatment for osteoporosis59. In this review WBV was only seen to significantly positively effect UV31. However, the absence of effects on other components of QUS or BMD in the reviewed study31 make it unlikely that there was true significant positive benefit of WBV on bone density. As with other discussed outcome measures, it seems that WBV may not provide enough mechanical stimulation to simulate axial-loading on Earth and therefore cannot significantly alter micro-gravity induced bone catabolism. This is also true for the absence of a positive effect of centrifugation as seen in this review40. The reasoning for the significant negative effect of centrifugation on polar strength-strain index (SSI P—a surrogate marker of bone strength) of the distal tibia is uncertain.
This review aimed to examine the effectiveness of stand-alone passive countermeasures on cardiopulmonary and musculoskeletal deconditioning in humans due to gravitational unloading. This study had three main findings: (1) a lack of standardisation of outcome measurement and methodologies has led to a large amount of heterogeneity amongst studies; (2) overall, standalone passive countermeasures seem to have little significant effect on cardiopulmonary and musculoskeletal outcomes; and (3) scarcity of literature and high risk of bias amongst existing studies limits the statistical power of results.
The results of this review are pertinent to future deep space and planetary surface explorations, particularly as the space industry transitions from Low-Earth Orbit (LEO) missions to exploration-class missions. NASA’s Artemis program is an example of such an endeavour60. As early as 2024, humans will be sent to the moon for the first time in over five decades. The Artemis program is a herald to the paradigm shift occurring within the field of aerospace medicine. Currently, the goals of both passive and active countermeasures tested and utilised on the ISS are largely to maintain baseline human physiology during LEO missions.
Most spaceflight countermeasure studies examine the degree to which human physiology can be maintained close to baseline—that is to what degree measured physiologic parameters can be maintained in-flight and post-flight as compared to subjects’ normal physiology on Earth. As humanity transitions to longer distance and duration space travel, there must be some level of acceptance of deconditioning as it will prove difficult and perhaps operationally unnecessary to endeavour to completely maintain crewmembers at their baseline physiology. Classically used outcome measures for LEO spaceflight studies such as VO2max, BMD and muscle strength will be of less importance during planned Artemis missions as crewmember deconditioning of these parameters is unlikely to significantly impact mission success or threaten crewmember life. Instead, maintaining crewmember operational functionality with respect to orthostatic tolerance, balance-related outcomes, spatial orientation, and postural stability may be of increased importance as they perform extravehicular activities (EVAs) on the lunar surface.
The most critical point in time for crewmember health during the Artemis lunar surface missions will be during the transition from microgravity to lunar hypogravity. Many knowledge gaps exist with regards to how the physiologic toll of spaceflight coupled with the transition to a hypogravity environment will influence the ability of crewmembers to complete mission tasks. NASA has identified a significant research gap regarding the effect of lunar hypogravity on orthostatic intolerance61. The many effects of orthostatic intolerance such as headaches, vision changes, presyncope and syncope can prove extremely dangerous to crewmembers particularly during lunar EVAs. Although there may be some suggestion of protective benefits of lunar hypogravity on crewmember exposure to microgravity during transit; existing simulation studies are limited in number, quality, and transferability to actual spaceflight. Current exercise countermeasures during LEO missions and volume resuscitation upon landing have limited orthostatic intolerance in returning crewmembers62. Yet the same level of use of these countermeasures may be difficult or impossible during Artemis missions given resource constraints. Moreover, the extended duration of exposure to microgravity during Artemis missions, the much smaller gravitational loading present on the moon as compared to Earth, and the absence of availability of post-flight rehabilitation measures are some of the factors which may be barriers to recovery of OT following transit to the lunar surface as compared to return to Earth from LEO missions. During the Apollo program, astronauts were placed on the lunar surface after only 3 days of transit through space. In comparison, Artemis missions will likely require much longer durations of exposure to microgravity. Treadmills and/or advance resistive exercise equipment currently available for LEO missions may not be available during these missions. Operational space may be available on the Lunar Gateway however, overall, current limitations on the accessibility of exercise further highlight the potential importance of passive countermeasure utilisation.
Although limited in statistical power, the results of this review indicate that LBNP and skin-surface cooling demonstrated a significant positive effect on OT as standalone measures. Returning crewmembers have also been found to have experienced transient declines in postural stability and sensorimotor control which has led to post-flight disturbances in coordination, balance, and mobility63. These deteriorations are thought to stem from a lack of somatosensory stimulation during spaceflight as it leads to transient functional vestibular deficiency64. As mentioned in this review, mechanical stimulation through vibrational plates has been suggested and studied as a possible countermeasure to this deterioration. Additionally, counterpressure garments may have potential benefits for orthosis following lunar and Mars surface landing. Previously, counterpressure garments have been seen to have initial benefits on orthosis for crewmembers following return from LEO. These studies results could not be included in the data analysed in this review, however, due to potential confounding of outcomes during spaceflight secondary to the use of other countermeasures over the studies’ durations (i.e. exercise)65,66,67.
Spaceflight-Associated Neuro-Ocular Syndrome (SANS) includes a spectrum of findings and symptoms which have been seen to affect astronauts during long-duration space missions21,68. Optic disc oedema is the cardinal sign of SANS with globe flattening, cotton wool spots, choroidal and retinal folds, and hyperopic refractive error also often observed21,68. There is a potential of SANS to impact crewmember ability to safely and efficiently complete mission tasks with the main reported symptom being decreased near vision acuity21. These symptoms have been reported in individuals in as little as 3 weeks following microgravity exposure69. Although disease aetiology is poorly understood, a large component of SANS is thought to originate from increased intracranial pressure as a result of microgravity-induced cephalad fluid shift21,68. LBNP is being explored as a potential modality to limit the occurrence/severity of SANS due to its limiting of this fluid shift21. However, numerous unknowns must first be addressed prior to the use of LBNP for ameliorating the occurrence of SANS, as discussed in Harris et al.21. Some of these unknows include understanding the process of physiologic adaptation leading to SANS, how effective LBNP is at ameliorating SANS, how long the modality would need to be used for21, and whether there is an acceptable severity of SANS which needs to be accepted as a consequence of LDSM prolonged microgravity exposure. There is a need for further research to explore and answer these questions particularly considering how SANS may impact LDSMs on the horizon.
Although this study shows the potential positive effects of LBNP, skin-surface cooling and WBV on operationally-relevant outcome measures, these results were limited by the quality, quantity and transferability of extracted data. Therefore, this review serves to highlight these countermeasures as a possible focus for future research and demonstrates the potential of passive countermeasures to aid in the success of future space missions. There is a need for future studies to further examine the utility of passive countermeasures and their role for future spaceflight. Additionally, numerous passive countermeasures have not been adequately examined in CTs and RCTs such as compression clothing, electromagnetic stimulation, and specialised garments. As humanity moves towards deep space and planetary surface exploration, it is imperative that these knowledge gaps are filled to ensure mission success and protect crew health.
Methods
The European Space Agency’s (ESA) Space Medicine Team (SMT) is completing a systematic review series evaluating evidence regarding passive, active and nutritional countermeasures to microgravity-induced pathologies. The literature being examined is a mix of inflight studies as well as ground-based analogues. This review is the third in the series and the first to examine stand-alone passive countermeasures17,70. Data extraction, effect size calculation and quality assessment of literature were done using tools created by Aerospace Medicine SR Group (ASMRG)71.
Search strategy
An initial search was conducted and presented in 2017 by Fiebig et al.17 using several keywords and groupings (Table 4). These keywords were combined with Boolean logic as shown in Table 4. The main and specific categories as well as the overall search strategy were defined by the European Astronaut Centre space physiology and space medicine operations experts. Articles in English from the following databases were included: Pubmed, Web of Science, Embase, Institute of Electrical and Electronics Engineers (IEEE) database, the ESA’s “Erasmus Experiment Archive”, the NASA “Life Science Data Archive” and “Technical Reports Server” and the German Aerospace Centre’s (DLR) database.
In May of 2021, an updated search was performed for databases which had produced the majority of the relevant articles during the 2017 search: Pubmed, Web of Science, and Embase. For this update, the search strategy was modified to only include articles examining passive countermeasures. Keywords used to search for active and nutritional countermeasure studies were not included (search numbers 6, 8 and 9 in Table 4). Exclusion of these keywords required adjustment in Boolean operators (#9 was replaced with #7 in search #14 within Table 4).
In 2017, Fiebig and colleagues screened the titles and abstracts of n = 2695 unique records which the initial search yielded17. n = 433 unique records pertaining to passive countermeasures were identified to meet inclusion criteria based on title/abstract screening. These records were rescreened in 2021. The updated 2021 search yielded n = 286 results. All records (n = 647 following duplicate removal) were screened using established PICOS as defined in Sandal et al.17: “Population: Healthy humans; Interventions: Space flights and ground-based space flight analogues with a duration of ≥5 days with a stand-alone passive countermeasure; Control: Space flights and ground-based space flight analogues with a duration of ≥5 days without any form of countermeasure; Outcomes: Studies must contain cardiopulmonary/vascular and/or musculoskeletal/biomechanical outcome measures; and, Study designs: Randomized control trials (RCT) and controlled clinical trial (CT)”. The PRISMA flow diagram for the updated search is shown below (Fig. 2).
Data collection and analysis
Double blinded screening of articles was accomplished through use of the online software tool Rayyan72. Two screeners independently decided if articles met established inclusion criteria. A third screener resolved any disagreements. As detailed above, in 2017, two independent reviewers screened for ground-based analogue and spaceflight studies that examined countermeasures grouped into active, passive, nutritional and mixed countermeasures17. In 2021, an updated search was completed through the Pubmed, Web of Science and Embase databases. Following this search, two other independent reviewers did the abstract and title screening for passive countermeasure studies using records that passed title/abstract screening in 2017 in addition to records found through the updated search (Fig. 2). Full text versions of the resulting articles following title and abstract screening were obtained and screened further using the PICOS inclusion criteria. A third independent reviewer resolved any disagreements amongst the other two with regards to inclusion or exclusion as required. It should be noted that although spaceflight studies were screened, none met inclusion criteria due to risk of confounding as study participants concurrently used exercise and/or other countermeasures during study durations. Therefore, it would have been difficult to truly assess the effectiveness of passive countermeasure being studied as standalone measures.
Data extraction
The ASMRG Data Extraction and Analysis form was used to extract data from the included studies71. This form was created by the ASMRG as a tool to standardise data extraction and analysis for systematic reviews in aerospace medicine completed by the group. Means and standard deviations of control vs. countermeasure groups pre- and post- BR protocol were extracted from included studies and entered into the AMSRG form in order to calculate effect sizes.
Quality assessment
The lead author assessed the risk of bias for each of the included studies using one of two tools depending on whether the included articles were RCTs or CTs. For RCTs, a risk of bias tool curated by the Space Biomedicine SR Methods Group was utilised17. For non-randomised CTs, the Risk of Bias Assessment for Non-Randomised Studies (RoBANS) was used to evaluate risk of bias73.
Bed rest transferability
The ASMRG bed-rest (BR) transferability tool allows for ground-based analogue studies using BR to be assessed on their ability to mimic microgravity conditions on the human body as experienced during actual human spaceflight74. The tool is used to evaluate each study on 8 different criteria with points awarded if a criterion is met. These criteria were developed from the International Academy of Aeronautics’ (IAA) Guidelines for Standardization of Bed Rest Studies in the Spaceflight Context75. The more criteria which are met, the higher the score and therefore the greater the transferability of the study to human space flight74. Transferability is ranked from 1 (poor) to 8 (excellent). The 8 criteria are as follows: (1) Was 6° head-down tilt utilised?; (2) Was diet controlled?; (3) Were sleep-wake cycles controlled?; (4) Were BR phases standardised?; (5) Was horizontal positioning uninterrupted throughout the BR period?; (6) Was sunlight exposure controlled?; (7) Were measurements scheduled to take place at the same time each day?; and (8) Was the duration of the BR period stated?
Data analysis
A full meta-analysis could not be performed due to the heterogeneity of the extracted data. Means and standard deviations were extracted from the included studies in order to calculate effect sizes based on mean differences of control vs. countermeasure groups pre- and post- BR. Due to the small sample sizes of the included studies, Hedge’s G method was used for correction of bias wherein the quotient of the difference of means is taken from the pooled standard deviation17. As in Sandal et al.17, data were presented in effect size plots with 95% confidence interval bars. Outcomes were grouped by the broad groupings reflecting those used in the search strategy: “cardiopulmonary,” “musculoskeletal performance” and “skeletal anthropometric”. Outcomes were then further grouped by specific variables being measured. The cardiopulmonary grouping included: heart rate (HR), orthostatic tolerance (OT), VO2max and peak power. The musculoskeletal performance grouping included: balance, gait, muscle strength and jump performance. Finally, the skeletal anthropometric grouping included bone mineral density (BMD).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Data extracted from reviewed articles and used for effect size analysis are available upon request.
Code availability
The European Astronaut Center’s Space Medicine Systematic Review Group’s data analysis excel sheet used for data analysis is available upon request.
References
Williams, D., Kuipers, A., Mukai, C. & Thirsk, R. Acclimation during space flight: effects on human physiology. CMAJ 180, 1317–1323 (2009).
Buckey, J. C. Jr. et al. Orthostatic intolerance after spaceflight. J. Appl Physiol. 81, 7–18 (1996).
Otsuka, K. et al. Long-term exposure to space’s microgravity alters the time structure of heart rate variability of astronauts. Heliyon 2, e00211 (2016).
Shen, M. & Frishman, W. H. Effects of spaceflight on cardiovascular physiology and health. Cardiol. Rev. 27, 122–126 (2019).
Reschke, M. F. et al. Posture, locomotion, spatial orientation, and motion sickness as a function of space flight. Brain Res. Rev. 28, 102–117 (1998).
Macaulay, T. R. et al. Developing proprioceptive countermeasures to mitigate postural and locomotor control deficits after long-duration spaceflight. Front. Syst. Neurosci. 15, 658985 (2021).
Blaber, A. P., Goswami, N., Bondar, R. L. & Kassam, M. S. Impairment of cerebral blood flow regulation in astronauts with orthostatic intolerance after flight. Stroke 42, 1844–1850 (2011).
Blaber, A. P., Zuj, K. A. & Goswami, N. Cerebrovascular autoregulation: lessons learned from spaceflight research. Eur. J. Appl. Physiol. 113, 1909–1917 (2013).
Goswami, N. et al. Using the Moon as a high-fidelity analogue environment to study biological and behavioral effects of long-duration space exploration. Planet Space Sci. 74, 111–120 (2012).
Petersen, N. et al. Exercise in space: the European Space Agency approach to in-flight exercise countermeasures for long-duration missions on ISS. Extrem. Physiol. Med. 5, 9 (2016).
Loehr, J. A. et al. Physical training for long-duration spaceflight. Aerosp. Med. Hum. Perform. 86, A14–A23 (2015).
Kramer, A., Gollhofer, A., Armbrecht, G., Felsenberg, D. & Gruber, M. How to prevent the detrimental effects of two months of bed-rest on muscle, bone and cardiovascular system: an RCT. Sci. Rep. 7, 13177 (2017).
Weber, T. et al. Hopping in hypogravity—a rationale for a plyometric exercise countermeasure in planetary exploration missions. PLoS ONE 14, e0211263 (2019).
Convertino, V. A. Exercise as a countermeasure for physiological adaptation to prolonged spaceflight. Med. Sci. Sports Exerc. 28, 999–1014 (1996).
Korth, D. W. Exercise countermeasure hardware evolution on ISS: the first decade. Aerosp. Med. Hum. Perform. 86, A7–A13 (2015).
National Aeronautics and Space Administration. Artemis plan: NASA’s lunar exploration program overview. https://www.nasa.gov/wp-content/uploads/2020/12/artemis_plan-20200921.pdf (2020).
Sandal, P. H. et al. Effectiveness of nutritional countermeasures in microgravity and its ground-based analogues to ameliorate musculoskeletal and cardiopulmonary deconditioning—a systematic review. PLoS ONE 15, e0234412 (2020).
Clement, G. & Pavy-Le Traon, A. Centrifugation as a countermeasure during actual and simulated microgravity: a review. Eur. J. Appl. Physiol. 92, 235–248 (2004).
Rittweger, J. et al. Short-arm centrifugation as a partially effective musculoskeletal countermeasure during 5-day head-down tilt bed rest—results from the BRAG1 study. Eur. J. Appl. Physiol. 115, 1233–1244 (2015).
Bretl, K. N. et al. Tolerable acclimation to the cross-coupled illusion through a 10-day, incremental, personalized protocol. J. Vesti. Res. 29, 97–110 (2019).
Harris, K. M., Petersen, L. G. & Weber, T. Reviving lower body negative pressure as a countermeasure to prevent pathological vascular and ocular changes in microgravity. NPJ Microgravity 6, 38 (2020).
Hargens, A. R., Whalen, R. T., Watenpaugh, D. E., Schwandt, D. F. & Krock, L. P. Lower body negative pressure to provide load bearing in space. Aviat. Space Environ. Med. 62, 934–937 (1991).
Petersen, L. G. et al. Mobile lower body negative pressure suit as an integrative countermeasure for spaceflight. Aerosp. Med. Hum. Perform. 90, 993–999 (2019).
Arbeille, P. et al. Effect of the thigh-cuffs on the carotid artery diameter jugular vein section and facial skin edema: HDT study. J. Gravit. Physiol. 6, P39–P40 (1999).
Keller, D. M., Low, D. A., Davis, S. L., Hastings, J. & Crandall, C. G. Skin surface cooling improves orthostatic tolerance following prolonged head-down bed rest. J. Appl. Physiol. 110, 1592–1597 (2011).
Muir, J., Judex, S., Qin, Y. X. & Rubin, C. Postural instability caused by extended bed rest is alleviated by brief daily exposure to low magnitude mechanical signals. Gait Posture 33, 429–435 (2011).
Berinstain, A., Gregory, P. & Herring, R. Canada’s space protein crystal growth program prepares for ISS. J. Cryst. Growth 232, 450–457 (2001).
Bloomberg, J. J., Reschke, M. F., Clement, G. R., Mulavara, A. P. & Taylor, L. C. Risk of impaired control of spacecraft/associated systems and decreased mobility due to vestibular/sensorimotor alterations associated with space flight. Human Research Program Human Health & Countermeasures No. JSC-CN-34446 (2015).
Sun, X. Q. et al. Effect of lower body negative pressure on orthostatic tolerance and cardiac function during 21 days head-down tilt bed rest. J. Gravit. Physiol. 10, 11–17 (2003).
Sun, X. Q. et al. Effect of lower body negative pressure against orthostatic intolerance induced by 21 days head-down tilt bed rest. Aviat. Space Environ. Med. 73, 335–340 (2002).
Qin, Y.-X., Xia, Y., Muir, J., Lin, W. & Rubin, C. T. Quantitative ultrasound imaging monitoring progressive disuse osteopenia and mechanical stimulation mitigation in calcaneus region through a 90-day bed rest human study. J. Orthop. Transl. 18, 48–58 (2019).
Linnarsson, D. et al. Effects of an artificial gravity countermeasure on orthostatic tolerance, blood volumes and aerobic power after short-term bed rest (BR-AG1). J. Appl. Physiol. 118, 29–35 (2015).
Kramer, A. et al. Daily 30-min exposure to artificial gravity during 60 days of bed rest does not maintain aerobic exercise capacity but mitigates some deteriorations of muscle function: results from the AGBRESA RCT. Eur. J. Appl. Physiol. https://doi.org/10.1007/s00421-021-04673-w (2021).
Custaud, M. A. et al. No effect of venoconstrictive thigh cuffs on orthostatic hypotension induced by head-down bed rest. Acta Physiol. Scand. 170, 77–85 (2000).
Arbeille, P. et al. Influences of thigh cuffs on the cardiovascular system during 7-day head-down bed rest. J. Appl. Physiol. 87, 2168–2176 (1999).
Arbeille, P. et al. Effect on the cardiac function of repeated LBNP during a 1-month head down tilt. Acta Astronaut. 25, 415–418 (1991).
Dupui, P., Montoya, R., Costes-Salon, M. C., Severac, A. & Guell, A. Balance and gait analysis after 30 days -6 degrees bed rest: influence of lower-body negative-pressure sessions. Aviat. Space Environ. Med. 63, 1004–1010 (1992).
Guell, A., Braak, L., Pavy Le Traon, A. & Gharib, C. Cardiovascular deconditioning during weightlessness simulation and use of lower body negative pressure as a countermeasure to orthostatic intolerance. Acta Astronaut. 21, 667–672 (1990).
Millet, C. et al. Adaptations to a 7-day head-down bed rest with thigh cuffs. Med. Sci. Sports Exerc. 32, 1748–1756 (2000).
Smith, S. M. et al. Effects of artificial gravity during bed rest on bone metabolism in humans. J. Appl. Physiol. 107, 47–53 (2009).
Stenger, M. B. et al. Artificial gravity training reduces bed rest-induced cardiovascular deconditioning. Eur. J. Appl. Physiol. 112, 605–616 (2012).
Frost, M. L., Blake, G. M. & Fogelman, I. Quantitative ultrasound and bone mineral density are equally strongly associated with risk factors for osteoporosis. J. Bone Min. Res. 16, 406–416 (2001).
Harm, D. L. et al. Invited review: gender issues related to spaceflight: a NASA perspective. J. Appl. Physiol. 91, 2374–2383 (2001).
Fullagar, H. H. et al. Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med. 45, 161–186 (2015).
Knowles, O. E., Drinkwater, E. J., Urwin, C. S., Lamon, S. & Aisbett, B. Inadequate sleep and muscle strength: implications for resistance training. J. Sci. Med. Sport 21, 959–968 (2018).
Schlesinger, A., Redfern, M. S., Dahl, R. E. & Jennings, J. R. Postural control, attention and sleep deprivation. Neuroreport 9, 49–52 (1998).
Hughson, R. L. Recent findings in cardiovascular physiology with space travel. Respir. Physiol. Neurobiol. 169, S38–S41 (2009).
Baisch, F. et al. Cardiovascular response to lower body negative pressure stimulation before, during, and after space flight. Eur. J. Clin. Invest. 30, 1055–1065 (2000).
Fritsch-Yelle, J. M., Charles, J. B., Jones, M. M., Beightol, L. A. & Eckberg, D. L. Spaceflight alters autonomic regulation of arterial pressure in humans. J. Appl. Physiol. 77, 1776–1783 (1994).
Watenpaugh, D. E. et al. Lower body negative pressure exercise plus brief postexercise lower body negative pressure improve post-bed rest orthostatic tolerance. J. Appl. Physiol. 103, 1964–1972 (2007).
Zhang, L. F. Region-specific vascular remodeling and its prevention by artificial gravity in weightless environment. Eur. J. Appl. Physiol. 113, 2873–2895 (2013).
Durand, S., Cui, J., Williams, K. D. & Crandall, C. G. Skin surface cooling improves orthostatic tolerance in normothermic individuals. Am. J. Physiol. Regul. Integr. Comp. Physiol. 286, R199–R205 (2004).
Stegemann, J., Hoffmann, U., Erdmann, R. & Essfeld, D. Exercise capacity during and after spaceflight. Aviat. Space Environ. Med. 68, 812–817 (1997).
Ade, C. J., Broxterman, R. M., Moore, A. D. & Barstow, T. J. Decreases in maximal oxygen uptake following long-duration spaceflight: role of convective and diffusive O2 transport mechanisms. J. Appl. Physiol. 122, 968–975 (2017).
Iwasaki, K. I., Sasaki, T., Hirayanagi, K. & Yajima, K. Usefulness of daily +2Gz load as a countermeasure against physiological problems during weightlessness. Acta Astronaut. 49, 227–235 (2001).
LeBlanc, A., Rowe, R., Schneider, V., Evans, H. & Hedrick, T. Regional muscle loss after short duration spaceflight. Aviat. Space Environ. Med. 66, 1151–1154 (1995).
Akima, H. et al. Effect of short-duration spaceflight on thigh and leg muscle volume. Med. Sci. Sports Exerc. 32, 1743–1747 (2000).
Costantino, C., Pogliacomi, F. & Soncini, G. Effect of the vibration board on the strength of ankle dorsal and plantar flexor muscles: a preliminary randomized controlled study. Acta Biomed. 77, 10–16 (2006).
Ozcivici, E. et al. Mechanical signals as anabolic agents in bone. Nat. Rev. Rheumatol. 6, 50–59 (2010).
NASA. Artemis Plan: NASA’s Lunar Exploration Program Overview (National Aeroonautics and Space Administration, 2020).
NASA. Risk of Orthostatic Intolerance During Re-exposure to Gravity (National Aeronautics and Space Administration, 2008).
Fu, Q. et al. Impact of prolonged spaceflight on orthostatic tolerance during ambulation and blood pressure profiles in astronauts. Circulation 140, 729–738 (2019).
Tays, G. D. et al. The effects of long duration spaceflight on sensorimotor control and cognition. Front. Neural Circuits 15, 723504 (2021).
Ozdemir, R. A., Goel, R., Reschke, M. F., Wood, S. J. & Paloski, W. H. Critical role of somatosensation in postural control following spaceflight: vestibularly deficient astronauts are not able to maintain upright stance during compromised somatosensation. Front. Physiol. 9, 1680 (2018).
Lee, S. M. C. et al. Efficacy of gradient compression garments in the hours after long-duration spaceflight. Front. Physiol. 11, 784 (2020).
Stenger, M. B., Brown, A. K., Lee, S. M., Locke, J. P. & Platts, S. H. Gradient compression garments as a countermeasure to post-spaceflight orthostatic intolerance. Aviat. Space Environ. Med. 81, 883–887 (2010).
Stenger, M. B. et al. Abdomen-high elastic gradient compression garments during post-spaceflight stand tests. Aviat. Space Environ. Med. 84, 459–466 (2013).
Lee, A. G. et al. Spaceflight associated neuro-ocular syndrome (SANS) and the neuro-ophthalmologic effects of microgravity: a review and an update. NPJ Microgravity 6, 7 (2020).
Mader, T. H. et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology 118, 2058–2069 (2011).
Fiebig, L. et al. Effectiveness of resistive exercise countermeasures in bed rest to maintain muscle strength and power—a systematic review. Front. Physiol. Conference Abstract: 39th ISGP Meeting & ESA Life Sciences Meeting (2018).
Space Biomedicine SR Methods. Space Biomedicine SR Methods. https://sites.google.com/view/sr-methods/aboutcontact (2021).
Ouzzani, M., Hammady, H., Fedorowicz, Z. & Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 5, 210 (2016).
Kim, S. Y. et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J. Clin. Epidemiol. 66, 408–414 (2013).
Winnard, A. et al. Systematic review of countermeasures to minimise physiological changes and risk of injury to the lumbopelvic area following long-term microgravity. Musculoskelet. Sci. Pr. 27, S5–S14 (2017).
Angeer, O., Larina, I. & Cromwell, R. Guidelines for Standardization of Bed Rest Studies in the Spaceflight Context (International Academy of Astronautics, 2014).
Acknowledgements
This project was supported by the ESA Space Medicine Team (HRE-OM).
Author information
Authors and Affiliations
Contributions
T.W. and L.F. conceived of the presented idea. T.W., D.G., and A.W. established the methods and tools used for data extraction, analysis, and quality assessment of reviewed articles. S.A., T.W., and L.F. conducted the updated literature search and screening of articles based on criteria established by T.W. and L.F.. S.A. conducted data extraction, data analysis, and quality assessment of reviewed articles and wrote the manuscript with supervision from N.G., A.S., and T.W. Revisions were completed with by S.A. with supervision from N.G., A.S., and T.W. All authors provided critical feedback for shaping of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. T.W. is employed by KBR GmbH on behalf of the European Space Agency. The funder KBR GmbH provided support in the form of salaries for the authors D.G. and T.W. but did not have any role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript. All authors declare that the research was conducted in the absence of any commercial, financial, or non-financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, S.S., Goswami, N., Sirek, A. et al. Systematic review of the effectiveness of standalone passive countermeasures on microgravity-induced physiologic deconditioning. npj Microgravity 10, 48 (2024). https://doi.org/10.1038/s41526-024-00389-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41526-024-00389-1