Abstract
Identifying germline BRCA1/2 mutation carriers is vital for reducing their risk of breast and ovarian cancer. To derive a serum miRNA-based diagnostic test we used samples from 653 healthy women from six international cohorts, including 350 (53.6%) with BRCA1/2 mutations and 303 (46.4%) BRCA1/2 wild-type. All individuals were cancer-free before and at least 12 months after sampling. RNA-sequencing followed by differential expression analysis identified 19 miRNAs significantly associated with BRCA mutations, 10 of which were ultimately used for classification: hsa-miR-20b-5p, hsa-miR-19b-3p, hsa-let-7b-5p, hsa-miR-320b, hsa-miR-139-3p, hsa-miR-30d-5p, hsa-miR-17-5p, hsa-miR-182-5p, hsa-miR-421, hsa-miR-375-3p. The final logistic regression model achieved area under the receiver operating characteristic curve 0.89 (95% CI: 0.87–0.93), 93.88% sensitivity and 80.72% specificity in an independent validation cohort. Mutated gene, menopausal status or having preemptive oophorectomy did not affect classification performance. Circulating microRNAs may be used to identify BRCA1/2 mutations in patients of high risk of cancer, offering an opportunity to reduce screening costs.
Similar content being viewed by others
Introduction
Hereditary breast and ovarian cancer (HBOC) is the most common hereditary cancer syndrome, and the two most commonly mutated genes in HBOC, BRCA1 and BRCA2, both play critical roles in mediating DNA repair through homologous recombination (HR)1. Germline mutations in BRCA1/2 account for 10–15% of ovarian cancers, 5–10% of breast cancers, and 3–5% of pancreatic and prostate cancers2,3,4,5,6,7. Loss of HR, known as HR deficiency (HRD), impairs the ability of cells to repair double-strand DNA breaks, leaving cells vulnerable to mutagenesis from ionizing radiation and oxidative stress8. Identification of BRCA1/2 mutation carriers is an essential component of cancer risk-reduction strategies and presents opportunities for cascade testing of other family members9. Mutation carriers have several opportunities for cancer prevention or interception, including risk-reducing salpingo-oophorectomy or mastectomy, hormonal chemoprevention, and enhanced surveillance protocols, such as MRI-based breast cancer screening10,11,12,13,14,15,16.
Prevention or early detection of BRCA1/2-related cancers is predicated on the identification of BRCA1/2 mutation carriers. At present, genetic testing for BRCA1/2 is only recommended for individuals with a known personal or familial history of breast, ovarian, tubal, or primary peritoneal cancer or for persons descending from populations with high mutational prevalence (e.g., Ashkenazi Jewish)17. However, more than half of all carriers with BRCA1/2 mutations have no family history of cancer, which would prompt a referral for genetic testing18. Among the estimated 1 million BRCA1/2 mutation carriers in the United States, only 10% are aware of their carrier status19.
While universal genetic testing might not be feasible or desirable, a functional screen for “BRCAness” could improve the efficiency of cancer early detection and prevention efforts. Such a test could focus genetic counseling and testing among those individuals with the highest pretest probability of having a pathogenic mutation, regardless of personal or family history. We suggest microRNAs (miRNAs) might play a role in developing such a tool. Our teams and others have shown that miRNAs are directly linked to BRCA-mediated DNA repair20,21,22,23,24. HBOC-related tumors are characterized by distinct miRNA profiles from sporadic disease25,26,27,28,29. Furthermore, miRNAs circulate in blood, and circulating miRNAs are characterized by surprising stability and reproducibility, making them attractive circulating biomakers30,31. Previously, using sera from subjects with unknown BRCA status, we reported and validated a test based on circulating miRNA that produced both high positive and negative predictive values for discriminating ovarian cancers from benign pelvic masses32. Other groups subsequently reported similar findings33,34. We undertook the present study to investigate whether circulating miRNAs might vary by BRCA1/2 mutational status. We hypothesized that circulating miRNAs profiles could be used to identify germline BRCA1/2 mutations among otherwise healthy individuals without cancer.
In this work, we show that a panel of miRNAs can be used to identify BRCA1/2 mutation carriers among healthy women with high genetic risk of ovarian or breast cancer. The serum miRNA-based test may provide a cheap first-line screening, guiding further efforts for genetic counseling and improving cancer prevention and early detection.
Results
Characteristics of the study population
The study population characteristics are summarized in Table 1. In total, samples were collected from 653 study subjects from six separate cohorts (Fig. 1). Among the study population, 350 (53.6%) subjects had BRCA1 or BRCA2 mutations (BRCA-mt), and 303 (46.4%) were BRCA1/2—wild-type (BRCA-wt). Summary clinical characteristics of each group are presented in Supplementary Table 1. A small number of participants (75/653; 11.5%) had undergone risk-reducing salpingo-oophorectomy prior to blood collection because of BRCA-associated cancer risk, which was accounted for in the differential expression analysis.
a Overview of datasets. BWH Brigham and Women’s Hospital, CCGP Center for Cancer Genetics and Prevention at DFCI, DGO Department of Gynaecological Oncology, Tata Medical Center, Kolkata, India, IHCC International Hereditary Cancer Center of the Pomeranian Medical University, Poland, DFCI DFCI/BWH biobank, UPenn University of Pennsylvania. b Scheme of statistical analysis design.
Identification of miRNAs associated with germline BRCA mutations
Unsupervised, linear and non-linear dimensionality reduction with PCA and UMAP were used to examine the effects of BRCA1/2 deficient status and that of the batch (Fig. 2a, b and Supplementary Fig. 1). The batch effect clearly separated the groups. However, within both observed batches, the BRCA status strongly affected expression profiles (Fig. 2a). We aimed to identify differentially expressed (DE) miRNAs according to germline BRCA1/2 mutations by superimposing the results after two strategies of data preprocessing—on raw data (Fig. 2c and Supplementary Data 1) and after batch adjustment (Fig. 2d and Supplementary Data 2). Nineteen miRNAs were convergent (P < 0.01 with |log2(FC) | > 0.5 in the same direction in both variants, ratio of FCs from two analysis variants between 0.8 and 1.25) regardless of the data preprocessing strategy (purple markings in Fig. 2c, d). Unsupervised hierarchical clustering of all subject samples from the 5 groups used for miRNA selection and model development showed that the samples clustered based on the BRCA1/2 mutations (Fig. 2e) with no evident preference towards BRCA1 or BRCA2 mutations. Notably, in the validation group composed of UPenn samples, the 19 miRNAs also clearly separated BRCA-mt and BRCA-wt samples confirming the robustness of their selection (Supplementary Fig. 2).
UMAP representation of BRCA-mt and BRCA-wt samples from all evaluated cohorts without (a) and after (b) batch adjustment (N = 653). Volcano plots showing differentially expressed miRNAs between BRCA-mutated and wild-type samples without (c) and after (d) batch adjustment (N = 521); red markings represent miRNAs with P < 0.01 and FC > 1.5 or <0.66; purple markings denote ones that were significant in both comparisons. Limma package was used for between-group miRNA expression comparison, presented unadjusted P values, and FCs were calculated by limma algorithm. e Heatmap of 19 miRNAs with convergent BRCA-mt; BRCA-wt profiles regardless of data preprocessing. Clustering primarily by BRCA status with no clear pattern of BRCA1 or BRCA2 or interference by prior oophorectomy (N = 521). Euclidean distance and complete linkage were used to determine cluster structure.
Using miRNAs to predict BRCA mutation status
Having preselected 19 miRNAs with consistent capability of separating BRCA-mt from BRCA-wt samples, we used OmicSelector-based development of models to differentiate between BRCA-mt and wild-type samples based on batch-adjusted log2 (TPM) expression values. Feature sets derived from the training set (Supplementary Data 3) were used for modeling using four different approaches. The best predictive performance was achieved by a logistic regression model with parameters shown in Supplementary Table 2 based on 10 miRNAs: hsa-miR-20b-5p, hsa-miR-19b-3p, hsa-let-7b-5p, hsa-miR-320b, hsa-miR-139-3p, hsa-miR-30d-5p, hsa-miR-17-5p, hsa-miR-182-5p, hsa-miR-421, and hsa-miR-375-3p (Supplementary Data 4). This set of miRNAs was selected using feature ranking based on ROC AUC and a minimal description length (MDL) discretization algorithm on the training set balanced with the Synthetic Minority Oversampling Technique (SMOTE)35.
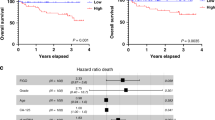
The final model achieved 82.35% accuracy, 84.51% sensitivity, and 79.39% specificity on the original training set. The training AUC ROC (Fig. 3a) was 0.89 (95% CI: 0.87–0.93). This model achieved 84.62% accuracy, 95.33% sensitivity, and 83.64% specificity on the testing set and 85.61% accuracy, 93.88% sensitivity, and 80.72% specificity in the external validation set comprised of the UPenn group. Confusion matrices for the separate sets are available in Supplementary Table 3. Predicted probabilities of BRCA-mt in the context of true BRCA status are presented in Fig. 3b. Menopausal status (Fig. 3c and Supplementary Table 4) or having preemptive oophorectomy before blood sample draw (Fig. 3d) did not affect classification performance. Case-wise prediction for all available samples with clinical data and miRNA expression for all 19 miRNAs are presented in Supplementary Data 5. The presented diagnostic performance was calculated for the cutoff established on the basis of optimal accuracy. However, to better evaluate the utility of the proposed test we present the estimated positive and negative predictive values of different thresholds (based on the results from the whole patient cohort) for populations of varying prevalence of mutations in genes associated with homologous recombination pathway of DNA repair (Supplementary Fig. 3). Although data on accurate age at testing was provided for 52% of subjects, with a predominance of controls, we did not observe any correlation between the model’s predicted probabilities in both BRCA-mt (r = 0.14; P = 0.33) and BRCA-wt (r = 0.01; P = 0.88) individuals (Supplementary Fig. 4). The model’s performance remained constant throughout the whole range of age categories (Supplementary Table 5).
a Training (sample size N = 391) ROC curve of the final logistic regression model; the area under the curve equaled 0.89 (95% CI: 0.87–0.93); b predicted BRCA1/2 mutation probability in training, testing, and validation sets according to reference mutational status; c predicted BRCA1/2 mutation probability in the context of menopausal status; d predicted BRCA1/2 mutation probability in the context of having ovaries at the time of testing. c, d show that both menopausal status and lack of ovaries did not influence predicted BRCA1 or BRCA2 mutation probability. In boxplots median is marked as central line, boxes indicate the first and third quartile and whiskers present 1.5× IQR. b–d present all N = 653 samples, statistics were derived using all samples in respective subgroups.
Discussion
In this study, we analyzed serum profiles of miRNA expression of a large (N = 653) group of healthy participants from six international cohorts to obtain a signature associated with BRCA1/2 mutations. This is a clinically relevant finding because these individuals are at increased lifetime risk of developing BRCA-deficiency-related cancers. We used RNA sequencing for unbiased miRNA quantification and developed classification models to discriminate samples from subjects with BRCA mutations (N = 350) from those who are BRCA wild-type (N = 303). This work is distinct from previous studies which have either evaluated biomarker performance of circulating miRNAs directed at cancer diagnosis33, focused on differences in miRNA-based BRCA1/2 mutation signatures in the context of hereditary breast and ovarian cancers, or limited analyses to expression measured in formalin-fixed paraffin-embedded (FFPE) tumor tissues29,36. The present study is therefore a large-scale, comprehensive analysis of circulating miRNAs in healthy patients to identify those likely at high risk of hereditary cancers.
The presented test may serve as a balance to the United States Preventative Service Task Force recommendation against risk assessment, genetic counseling, or genetic testing for women “whose family history is not associated with an increased risk for harmful mutations in the BRCA1/2 genes17.” The argument to restrict testing derives from estimates that pathogenic mutations in BRCA1/2 only occur in 0.2–0.3% of women in the general population37 and a negative test result offers no gain in life expectancy nor eliminates the need for regular mammograms38. Despite falling costs for genetic testing, a cost-effectiveness investigation found that universal testing for the general population remains cost-prohibitive at about $1 million USD per quality-adjusted life year gained38. On the other hand, among patients referred for genetic testing based on family or personal cancer history, BRCA1/2 mutations are identified in up to 25%39. The application of the miRNA-based test to identify patients at the highest risk offers an opportunity to reduce the costs of screening, which is particularly important in resource-limited settings.
Mechanistically, it has been shown by us20 and other groups40 that miRNAs regulate expression of DNA repair genes and may impact DNA repair capacity and sensitivity to poly (ADP-ribose) polymerase inhibitors (PARPi). The well-established dysregulation of miRNA expression in cancer, together with the contribution of miRNAs to tumorigenesis and the fact that in BRCA1/2 mutation carriers, the genetic alterations are present in all body cells, offers a probable explanation for a distinct circulating miRNA signature. Haploinsufficiency of BRCA1 or BRCA2 gene for the suppression of replication stress instigated by environmental and endogenous factors was demonstrated, despite different biological functions of their encoded proteins41,42,43. This is supported by a recent observation of increased levels of soluble EGFR and increased thymidine kinase 1 activity in the sera of mutation carriers of either BRCA1 or BRCA244. Whether alterations in the levels of these miRNAs are an adaptive response to genomic instability or they function as messengers between cells remains to be established in future studies.
Homologous recombination haploinsufficiency is characterized by increased risks of ovarian, breast, pancreatic and prostate cancer as well as sensitivity to DNA damaging agents and PARPi. Although this phenotype, broadly termed BRCAness, is most commonly associated with germline mutations in BRCA1/2, evidence from basic and clinical studies suggest that other genetic and epigenetic alterations may have similar effects on cancer risk, tumor molecular features, and drug sensitivity45. It is possible that a BRCAness assay could help identify high-risk individuals with functional equivalency to BRCA1/2 mutations who would not be identified by routine genetic tests, such as those with loss of BRCA1/2 function through large-scale genomic rearrangements, promoter methylation, or mutations in less commonly mutated genes also in the HR repair pathway46. The matter of deploying the proposed test in clinical practice would also need to consider calibrating its cutoff to specific needs of the tested population. For the general population with the prevalence of germline BRCA1/2 mutations in the range of ~0.4%, the negative predictive value (NPV) corresponding to a cutoff probability of 0.25 would be 99.6% and the positive predictive value (PPV) would be 8.7%, In other words, in a hypothetical population of 10,000 patients with low risk of mutations, our test with cutoff p set at 0.25 with 94.3% sensitivity and 58.1% specificity would correctly identify 38 of 40 patients with germline BRCA1/2 mutations, while sparing 5787 of 9960 patients without mutations from costly genetic testing. For patients with higher risk of such variants—10.7% of mutations in HR genes that is observed in populations of patients diagnosed with breast cancer47—the same cutoff would yield an NPV of 98.8% and PPV of 21.2%. Individual-level decisions on using the test in prioritizing patients for genetic testing, however, could be made on the basis of the clinician’s experience, patient’s preference, available resources and screening programs. Currently, existing tests beyond germline mutation analysis, including ‘genomic scar’ assays, tissue transcriptional profiles, and functional HRD assays such as RAD51 foci quantification48, fail to consistently identify these patient populations of interest. A test based on circulating miRNA expression has two important advantages: it is feasible to perform in the clinical setting without the need for tissue biopsy and it may provide a dynamic readout of the HR proficiency status49. We hope to test this in future work.
The current study has several important strengths. First, the miRNA test approach enriches a population at the highest risk for ovarian and other BRCA haploinsufficiency-related cancers. Individuals with a positive screen would still require genetic testing to confirm predisposition to cancer, thus reducing risks from false positive results. Likewise, patients screening negative but with a strong family history could still opt for genetic testing, minimizing the number of false negative results. The availability of a confirmatory test minimizes harm while ensuring that most at-risk patients are identified. Second, the resulting model, a logistic regression based on the expression of ten miRNAs, yielded 85.6% accuracy in the hold-out validation set, which we consider to be acceptable performance for an assay designed as a first-pass screen. However, as the data presented at this stage are generated through high throughput sequencing which would likely have to be downscaled to a simpler and cheaper method, the key issue at this stage was not to prioritize the performance of the model itself, but rather to identify variables with the best potential for class separation through any possible means. Additionally, the relatively uncomplicated structure of this model facilitates its explanation, avoiding the unexplainability problem suffered by more complex machine learning and artificial intelligence approaches. Third, the model was developed using data from 6 distinct groups from three continents covering different ethnicities and mutations both in BRCA1 and BRCA2, which represents a more diverse group than our prior study and increases the likelihood that the results are generalizable. The wide range of study subject profiles further ensures that model performance was not affected by menopausal status or previously performed preventive surgery.
We also acknowledge the study’s weaknesses. First, the presented models rely on next-generation sequencing (NGS). While the costs of this tool are coming down, and the use of NGS has entered some clinical applications (e.g., cell-free DNA for prenatal testing), other platforms, such as qRT-PCR, might be more efficient. Considerable batch effects related mainly to the application of different sequencing platforms is an issue that cannot be ignored as a potential obstacle in the translation of our results. Although its impact was largely mitigated by selection of miRNAs consistently dysregulated regardless of using batch correction, similar problems may arise in the future with application of other sequencing platforms and reagents. Finally, we have not investigated these models in patients with other types of DNA repair defects, such as Lynch Syndrome, nor conducted sensitivity analyses across various racial and ethnic subpopulations. Indeed, metadata (age, menopausal status) were not available for a large number of samples. While we did not see variations in model performance across these subgroups, we cannot completely exclude the possibility that these factors may be confounders in a larger sample size. These studies will be needed to examine the generalizability of the approach. Finally, BRCA1 and BRCA2 have distinct functions in the HR repair pathway, yet the haploinsufficiency of either gene gives us a common circulating miRNA signature. We speculate that haploinsufficiency in HR-mediated repair and consequent genomic instability is a potential cause of this miRNA-based signal in serum. However, we need to validate this idea with serum miRNA analysis from individuals with HR gene haploinsufficiency caused by genetic factors other than mutations of BRCA1 or BRCA2.
In summary, we show that circulating miRNA levels can be used to stratify individuals as likely or unlikely to harbor a BRCA1/2 mutation. This extends our prior finding that a diagnostic circulating miRNA model can help distinguish ovarian cancer cases from benign adnexal masses or controls32. The approach supplements our previous effort by providing a means to identify individuals at elevated risk for ovarian cancer who require careful monitoring and may be advised to undergo risk-reduction surgery. The result raises the potential for directing identified patients to serial assessment of ovarian cancer risk designed for high-risk populations, an approach under assessment in a nationwide prospective observational study known as the microRNA Detection (MiDe) Study (www.midestudy.org).
Methods
The study was approved by the following ethical committees: Tata Medical Center—Institutional Review Board (approval number 2018/TMC/117/IRB6), Institutional Review Board of Dana-Farber Cancer Institute (#13–325), Institutional Review Board of University of Pennsylvania (#816688), Ethics Committee of the Pomeranian Medical University in Szczecin (BN-001/174/05).
Samples
The study group was assembled from six serum biorepositories (Fig. 1a) based at: Brigham and Women’s Hospital (BWH; Boston, MA; N = 87), Dana-Farber Cancer Institute (DFCI; Boston, MA; N = 200), a separate sample set from the Center for Cancer Genetics and Prevention at DFCI (CCGP; Boston, MA; N = 162), Tata Medical Center (DGO; Kolkata, India; N = 20), Pomeranian Medical University (IHCC; Szczecin, Poland; N = 52), and University of Pennsylvania (UPenn; Philadelphia, PA; N = 132). Samples from patients with genetically confirmed BRCA1/2 status were included in the study. Patients with ovarian cancer history or other cancer diagnosed within 1 year from sampling were excluded. Patients with benign adnexal masses were included. Patients with missing diagnoses or BRCA status were excluded. All study samples were collected under locally approved institutional review board protocols after obtaining informed consent from study subjects. Sample-level data are presented in Supplementary Data 6. The sequencing methods and NGS panels used for genetic diagnostics of BRCA mutations changed over time but the methods used were CLIA-validated (or certified by respective national boards of laboratory diagnostics or genetics in Poland and India) and the geneticists responsible for determining the pathogenicity of BRCA mutations adhered to the guidelines of the American College of Clinical Genetics current at the time of testing50,51,52.
Next-generation sequencing
Total RNA was extracted, followed by size-selection, adapter ligation, and library preparation as previously described32. All miRNA sequencing data were mapped to the reference miRNA database (miRBase version 22.1) using nf-core/smrnaseq version 1.1.0, a uniform, standardized bioinformatic pipeline developed and published as a part of the Nextflow project53. Reads unmapped to miRbase were subsequently mapped to human genome GRCh38. The sequencing protocol was set as QIAseq, Illumina or Nextflex, as appropriate to each sample set (QIAseq miRNA sequencing in BWH, IHCC, DFCI and UPenn; Illumina miRNA sequencing in CCGP and NEXTFLEX small RNA sequencing in DGO). All parameters of the pipeline were kept at the default values recommended by the code authors to assure reproducibility. Raw sequencing data in FASTQ files are deposited in Sequence Read Archive under BioProject number PRJNA898621. Derived expression data are available in Supplementary Data 7 and deposited in Gene Expression Omnibus (GEO) under the accession number GSE226445.
Data integration and miRNA selection
miRNAs were filtered for species detected in at least 33% of the samples in each group at a minimum detection threshold of >=10 transcripts per million (TPM). After filtering, 227 of the initial 2621 miRNAs were retained. Principal Component Analysis (PCA) was used to visualize the presence of batch effects (Supplementary Fig. 1). After voom normalization and mean-variance trend removal (model formula used for voom: ~0 + brcaStatus + havingOvaries + group, Supplementary Dataset 8), ComBat was used to combine data from all subject groups (Supplementary Data 9, with the UPenn group serving as reference (model formula used for ComBat: ~brcaStatus + havingOvaries)54,55. As different technologies were used to quantify the miRNA content in different subject groups, use of an empirical Bayes framework (ComBat) was a necessary step to combine data from all subject groups while accounting for technical heterogeneity55. However, to limit the potential confounding influence of ComBat on the effect of interest, we performed two versions of differential expression analysis (Fig. 1b): with and without batch adjustment and compared the results to identify miRNAs detected in both variants. Differential expression analysis was performed using limma56. The model formula for limma included the following effects: BRCA1/2 mutation and the effect of prior bilateral salpingo-oophorectomy (~0 + brcaStatus + havingOvaries). Visualization of the samples in reduced dimensionality space was performed using uniform manifold approximation projection (UMAP)57. The settings were as follows: number of neighbors for representation: 10 for batch-adjusted data and 5 for unadjusted, minimal distance: 0.2 for batch-adjusted data and 0.9 for unadjusted, distance metric: Euclidean in both cases. Hierarchical clustering was performed using the Ward method for linkage, Euclidean distance metric for samples (columns) and correlation distance metric for miRNAs (rows)58. DE was performed in R (version 3.6.3) with limma (3.42.2), edgeR (3.28.1), sva (3.34.0) and reticulate (1.26), while results’ visualization and part of preprocessing was done in Python (version 3.8.10) with pandas (1.3.0), numpy (1.20.0), sklearn (1.0.2), statsmodels (0.11.1), matplotlib (3.3.0), and seaborn (0.11.1).
Model development and statistical analysis
In this step, to assure the strict external validation, the dataset was divided into training (N = 391, 75% of cases from all groups except UPenn, random split), testing (N = 130, 25% of cases from all groups except UPenn, random split) and validation (N = 132, only UPenn group) sets. Model development and validation were conducted using in-house OmicSelector software (version 1.0; https://biostat.umed.pl/OmicSelector59). Briefly, OmicSelector tests 94 feature selection approaches based on 25 distinct variable selection methods. OmicSelector-based feature selection followed initial consistency-based preselection as described above. Feature sets with more than 10 miRNAs were filtered out. Selected feature sets were ranked using 4 modeling techniques (logistic regression, conditional decision trees, recursive partitioning trees, and artificial neural networks with 1 hidden layer) with hyperparameter optimization (2000 random hyperparameter sets) and hold-out validation on the testing set. The number of modeling techniques was reduced to assure low complexity of resulting models, and thus reduce the chance of overfitting. The best model was chosen based on the highest validation accuracy.
To assess model performance, the training area under the ROC was analyzed, and a cutoff value for BRCA status prediction was chosen based on the highest Youden index60. This cutoff was applied for prediction on testing and validation sets. Accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV)61 were calculated for all sets. Where indicated, the alpha level for statistical significance was set at <0.05. Supplementary Code 1 contains the RDS object containing Caret wrapper for final model.
All analyses were performed in R.
Statistics and reproducibility
Statistical methods applied in the study are described above. Differential expression analysis can be reproduced using code, data and instructions available at our departmental self-hosted GitLab repository https://git.btm.umed.pl/ZBiMT/brca-mirna and on Zenodo at https://doi.org/10.5281/zenodo.7817763. Code and data for the classification model are available on GitHub at https://github.com/kstawiski/brca-classifier and on Zenodo at https://doi.org/10.5281/zenodo.7817845.
No statistical method was used to predetermine sample size. Inclusion and exclusion criteria are specified in the Samples subsection. BRCA status and other available clinical data were known to researchers responsible for feature selection and models development with exception of BRCA1/2 status in validation set that was unknown to the researcher developing models. Models were developed with the use of results of genetic testing for BRCA status; thus, modeling outcomes were unknown when those tests were performed. All hypothesis tests were two-sided. Randomization was not applicable to this clinical study as no clinical intervention was performed.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Raw sequencing data are publicly available in the Gene Expression Omnibus under accession numbers PRJNA898621 and GSE226445 Source data are provided with this paper.
Code availability
The code for differential expression analysis was deposited at https://git.btm.umed.pl/ZBiMT/brca-mirna and https://doi.org/10.5281/zenodo.7817763; code for the classification model is available at https://github.com/kstawiski/brca-classifier and https://doi.org/10.5281/zenodo.7817845.
References
Shulman, L. P. Hereditary breast and ovarian cancer (HBOC): clinical features and counseling for BRCA1 and BRCA2, Lynch syndrome, Cowden syndrome, and Li-Fraumeni syndrome. Obstet. Gynecol. Clin. North Am. 37, 109–133 (2010).
Peretti, U. et al. Germinal BRCA1-2 pathogenic variants (gBRCA1-2pv) and pancreatic cancer: epidemiology of an Italian patient cohort. ESMO Open 6. https://doi.org/10.1016/j.esmoop.2020.100032 (2021).
Casolino, R. et al. Homologous recombination deficiency in pancreatic cancer: a systematic review and prevalence meta-analysis. J. Clin. Oncol. 39, 2617–2631 (2021).
Pritchard, C. C. et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N. Engl. J. Med. 375, 443–453 (2016).
Salo-Mullen, E. E. et al. Identification of germline genetic mutations in patients with pancreatic cancer. Cancer 121, 4382–4388 (2015).
Swisher, E. Ovarian cancer associated with inherited mutations in BRCA1 or BRCA2. Curr. Women’s Health Rep. 3, 27–32, https://europepmc.org/article/med/12521547 (2003).
Hemel, D. & Domchek, S. M. Breast cancer predisposition syndromes. Hematol. Oncol. Clin. North Am. 24, 799–814 (2010).
Hoeijmakers, J. H. J. Genome maintenance mechanisms for preventing cancer. Nature 411, 366–374 (2001).
Randall, L. M. et al. Multi-disciplinary summit on genetics services for women with gynecologic cancers: a Society of Gynecologic Oncology White Paper. Gynecol. Oncol. 146, 217–224 (2017).
Warner, E. et al. Breast cancer mortality among women with a BRCA1 or BRCA2 mutation in a magnetic resonance imaging plus mammography screening program. Cancers 12, 3479 (2020).
Visvanathan, K. et al. Use of pharmacologic interventions for breast cancer risk reduction: American society of clinical oncology clinical practice guideline. J. Clin. Oncol. 31, 2942–2962 (2013).
Guindalini, R. S. C. et al. Intensive surveillance with biannual dynamic contrast-enhanced magnetic resonance imaging downstages breast cancer in BRCA1 mutation carriers. Clin. Cancer Res. 25, 1786–1794 (2019).
Domchek, S. M. et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. J. Am. Med. Assoc. 304, 967–975 (2010).
Dullens, B. et al. Cancer surveillance in healthy carriers of germline pathogenic variants in BRCA1/2: a review of secondary prevention guidelines. J. Oncol. https://doi.org/10.1155/2020/9873954 (2020).
Marchetti, C. et al. Risk-reducing salpingo-oophorectomy: a meta-analysis on impact on ovarian cancer risk and all cause mortality in BRCA 1 and BRCA 2 mutation carriers. BMC Women’s Health 14, 1–6 (2014).
Nelson, H. D., Fu, R., Zakher, B., Pappas, M. & McDonagh, M. Medication use for the risk reduction of primary breast cancer in women: updated evidence report and systematic review for the US preventive services task force. J. Am. Med. Assoc. 322, 868–886 (2019).
Owens, D. K. et al. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer: US preventive services task force recommendation statement. J. Am. Med. Assoc. 322, 652–665 (2019).
King, M. C., Levy-Lahad, E. & Lahad, A. Population-based screening for BRCA1 and BRCA2: 2014 lasker award. J. Am. Med. Assoc. 312, 1091–1092 (2014).
Drohan, B., Roche, C. A., Cusack, J. C. & Hughes, K. S. Hereditary breast and ovarian cancer and other hereditary syndromes: using technology to identify carriers. Ann. Surg. Oncol. 19, 1732–1737 (2012).
Moskwa, P. et al. MiR-182-mediated downregulation of BRCA1 impacts DNA repair and sensitivity to PARP inhibitors. Mol. Cell 41, 210–220 (2011).
Choi, Y. E. et al. MicroRNAs down-regulate homologous recombination in the G1 phase of cycling cells to maintain genomic stability. eLife https://doi.org/10.7554/ELIFE.02445 (2014).
Meghani, K. et al. Multifaceted impact of microRNA 493-5p on genome-stabilizing pathways induces platinum and PARP inhibitor resistance in BRCA2-mutated carcinomas. Cell Rep. 23, 100–111 (2018).
Srinivasan, G. et al. MiR223-3p promotes synthetic lethality in BRCA1-deficient cancers. Proc. Natl Acad. Sci. USA 116, 17438–17443 (2019).
Poh, W. et al. BRCA1 promoter methylation is linked to defective homologous recombination repair and elevated miR-155 to disrupt myeloid differentiation in myeloid malignancies. Clin. Cancer Res. 25, 2513–2522 (2019).
Danza, K. et al. TGFbeta and miRNA regulation in familial and sporadic breast cancer. Oncotarget 8, 50715–50723 (2017).
Brouwer, J. et al. Small RNA sequencing reveals a comprehensive miRNA signature of BRCA1-associated high-grade serous ovarian cancer. J. Clin. Pathol. 69, 979–985 (2016).
Gu, Y. et al. The BRCA1/2-directed miRNA signature predicts a good prognosis in ovarian cancer patients with wild-type BRCA1/2. Oncotarget 6, 2397–2406 (2014).
Tommasi, C. et al. Biological role and clinical implications of microRNAs in BRCA mutation carriers. Front. Oncol. 11, 3555 (2021).
Murria Estal, R. et al. MicroRNA signatures in hereditary breast cancer. Breast Cancer Res. Treat. 142, 19–30 (2013).
Chen, X. et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 18, 997–1006 (2008).
Mitchell, P. S. et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl Acad. Sci. USA 105, 10513–10518 (2008).
Elias, K. M. et al. Diagnostic potential for a serum miRNA neural network for detection of ovarian cancer. eLife 6 https://doi.org/10.7554/eLife.28932 (2017).
Yokoi, A. et al. Integrated extracellular microRNA profiling for ovarian cancer screening. Nat. Commun. 9, 1–10 (2018).
Pan, C. et al. Exosomal microRNAs as tumor markers in epithelial ovarian cancer. Mol. Oncol. 12, 1935–1948 (2018).
Chawla, N. V., Bowyer, K. W., Hall, L. O. & Kegelmeyer, W. P. SMOTE: synthetic minority over-sampling technique. J. Artif. Intell. Res. 16, 321–357 (2002).
Tanic, M. et al. MicroRNA expression signatures for the prediction of BRCA1/2 mutation-associated hereditary breast cancer in paraffin-embedded formalin-fixed breast tumors. Int. J. Cancer 136, 593–602 (2015).
Nelson, H. D. et al. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: a systematic review to update the U.S. preventive services task force recommendation. Ann. Intern. Med. 160, 255–266 (2014).
Long, E. F. & Ganz, P. A. Cost-effectiveness of universal BRCA1/2 screening: evidence-based decision making. JAMA Oncol. 1, 1217–1218 (2015).
Melchor, L. & Benítez, J. The complex genetic landscape of familial breast cancer. Hum. Genet. 132, 845–863 (2013).
Crosby, M. E., Kulshreshtha, R., Ivan, M. & Glazer, P. M. MicroRNA regulation of DNA repair gene expression in hypoxic stress. Cancer Res. 69, 1221 (2009).
Pathania, S. et al. BRCA1 haploinsufficiency for replication stress suppression in primary cells. Nat. Commun. 5, 1–15 (2014).
Tan, S. L. W. et al. A class of environmental and endogenous toxins induces BRCA2 haploinsufficiency and genome instability. Cell 169, 1105–1118.e15 (2017).
Ogony, J. et al. Immune cells are increased in normal breast tissues of BRCA1/2 mutation carriers. Breast Cancer Res. Treat. 197, 277–285 (2023).
Nisman, B. et al. Comparison of diagnostic and prognostic performance of two assays measuring thymidine kinase 1 activity in serum of breast cancer patients. Clin. Chem. Lab. Med. 51, 439–447 (2013).
Lord, C. J. & Ashworth, A. BRCAness revisited. Nat. Rev. Cancer 16, 110–120 (2016).
Pennington, K. P. & Swisher, E. M. Hereditary ovarian cancer: beyond the usual suspects. Gynecol. Oncol. 124, 347–353 (2012).
Tung, N. et al. Frequency of germline mutations in 25 cancer susceptibility genes in a sequential series of patients with breast cancer. J. Clin. Oncol. 34, 1460–1468 (2016).
Hoppe, M. M., Sundar, R., Tan, D. S. P. & Jeyasekharan, A. D. Biomarkers for homologous recombination deficiency in cancer. JNCI: J. Natl Cancer Inst. 110, 704–713 (2018).
Miller, R. E. et al. ESMO recommendations on predictive biomarker testing for homologous recombination deficiency and PARP inhibitor benefit in ovarian cancer. Ann. Oncol. 31, 1606–1622 (2020).
Kazazian, J., Boehm, C. D. & Seltzer, W. K. ACMG recommendations for standards for interpretation of sequence variations. Genet. Med. 2, 302–303 (2000).
Richards, C. S. et al. ACMG recommendations for standards for interpretation and reporting of sequence variations: Revisions 2007. Genet. Med. 10, 294–300 (2008).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405 (2015).
di Tommaso, P. et al. Nextflow enables reproducible computational workflows. Nat. Biotechnol. 35, 316–319 (2017).
Law, C. W., Chen, Y., Shi, W. & Smyth, G. K. Voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol. 15, 1–17 (2014).
Zhang, Y., Jenkins, D. F., Manimaran, S. & Johnson, W. E. Alternative empirical Bayes models for adjusting for batch effects in genomic studies. BMC Bioinforma. 19, 1–15 (2018).
Ritchie, M. E. et al. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47–e47 (2015).
Becht, E. et al. Dimensionality reduction for visualizing single-cell data using UMAP. Nat. Biotechnol. 37, 38–44 (2018).
Ward, J. H. Hierarchical grouping to optimize an objective function. J. Am. Stat. Assoc. 58, 236–244 (1963).
Stawiski, K. et al. OmicSelector: automatic feature selection and deep learning modeling for omic experiments. Preprint at bioRxiv https://doi.org/10.1101/2022.06.01.494299 (2022).
Youden, W. J. Index for rating diagnostic tests. Cancer. 3, 32–35 (1950).
Fardy, J. M. & Barrett, B. J. Evaluation of diagnostic tests. Methods Mol. Biol. 1281, 289–300 (2015).
Acknowledgements
This work was supported by the Developmental Research Program of the Dana-Farber/Harvard Cancer Center Ovarian Cancer SPORE (Di.C. and K.E.) from the National Institutes of Health and the National Cancer Institute (grant 1P50CA240243-01A1, Di.C.), the Massachusetts Life Sciences Center Bits to Bytes Program (K.E.), the Deborah and Robert First Family Fund (K.E.), the Honorable Tina Brozman Foundation (K.E. and Di.C.), the V Foundation (Di.C.) and the Mighty Moose Foundation (Di.C.) and the DST-UKIERI grant no DST/INT/UK/P-134/2016 (A.M.). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Dr. K.E., Dr. W.F., and Dr. Di.C. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: K.E., W.F., and Di.C. Acquisition, analysis, or interpretation of the data: J.L., H.S., S.D., D.C.C., Do.C., A.M., J.G., J.K., C.L., W.F., Z.N., K.S., U.S., and J.W. Drafting of the manuscript: W.F., K.S., K.E., Z.N., and U.S. Critical revision of the manuscript: K.E., Di.C., J.C., P.K., J.G., and S.D. Statistical analysis: U.S., K.S., W.F., and J.W. Supervision: K.E., W.F., and Di.C.
Corresponding authors
Ethics declarations
Competing interests
K.E., W.F., K.S., and Di.C. are co-inventors of patent US201762444085P/EP3565903A1 (title “Circulating microrna signatures for ovarian cancer”), which relates to the use of circulating miRNAs for ovarian cancer diagnosis. Dr. Elias, Dr. Fendler, and Dr. Chowdhury acknowledge research funding from Aspira Women’s Health. K.E. reports research funding from Abcam, Inc. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Cong Zhou, Kishore Challagundla and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elias, K., Smyczynska, U., Stawiski, K. et al. Identification of BRCA1/2 mutation female carriers using circulating microRNA profiles. Nat Commun 14, 3350 (2023). https://doi.org/10.1038/s41467-023-38925-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-023-38925-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.