Abstract
We aimed to understand the risks and benefits of post-inflatable penile prosthesis (IPP) implantation drainage and optimal duration. Our patients were divided into 3 groups: Group 1 (n = 114) had no drain placed, Group 2 had a drain placed for 24 h (n = 114) and Group 3 had a drain placed for 72 h (n = 117). Postoperative scrotal hematoma and prosthesis infection rates were compared between the groups. The patients from Group 3 demonstrated a statistically significant lower incidence of hematoma on the 10th postoperative day: (n = 1, 0.9%) compared to Group 2: (n = 11, 9.6%) and Group 1: (n = 8, 7%), (p = 0.013). However, on the 3rd postoperative day, there was a statistically significant lower incidence of hematoma in both Groups 3 and 2: (0.9% and 6.1%, respectively) vs. Group 1: (11.4%), (p = 0.004). Hematoma rates followed the same group order after the first day of surgery: 1.7% (n = 2), 5.3% (n = 6), and 8.8% (n = 10), respectively, (p = 0.05). Five patients (4.4%) in Group 1 and four patients (3.5%) in Group 2 developed an IPP associated infection, opposed to only a single patient (0.85%) in Group 3, (p = 0.210). We concluded that prolonged scrotal drainage for 72 h after virgin IPP implantation significantly reduces hematoma and infection rates.
Similar content being viewed by others
Introduction
To date, inflatable penile prosthesis (IPP) implantation remains the gold standard treatment for erectile dysfunction refractory to medical treatment and is associated with the highest rates of patient satisfaction [1,2,3]. The last 50 years have been characterized by continuous advances in design and technology of penile implants and by a constant amelioration of surgical techniques and this has significantly improved overall surgical outcomes [4].
One of the most common complications of IPP implantation is postoperative bleeding and hematoma formation [5]. The loose nature and dependency of the scrotal tissues make the scrotum prone to the collection of blood around the pump and in the soft dartoic tissues. A number of measures have been introduced in order to minimize the risk of hematoma formation, spanning from proper patient selection and preparation and meticulous intraoperative hemostasis to adequate postoperative management. Postoperative measures include close suction drainage and the application of a compressive dressing such as the Mummy Wrap on the genitalia. To date, the decision on whether to leave a drain or not remains controversial [6,7,8]. The arguments in favor of close drain insertion include the lower risk of hematoma formation, which translates into a quicker and less uncomfortable recovery for the patient and an earlier activation of the device [9, 10].
Surgeons in favor of close drain insertion claim that this practice is not associated with an increased risk of infection [7, 11,12,13]. On the other hand, opponents regard drain insertion as a potential source of infection [14].
Our aim was to add to the body of evidence supporting the benefit of IPP implantation drainage as well suggest the optimal duration of drainage. Until an adequately designed prospective randomized controlled study is conducted to assess the potential benefits of inserting a drain during implantation of IPP, the current series suggests that closed drainage insertion after IPP implantation is associated with a significant reduction of hematoma and infection rates.
Methods
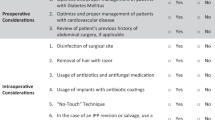
We conducted a multicenter prospective nonrandomized pilot study. Surgery was carried out by four European and one Australian high-volume surgeons at five different centers of excellence. Only virgin IPP cases were included in the series. Patients with Peyronie’s disease or severe fibrosis after priapism were not included. Patients on prophylactic anticoagulation were bridged prior to surgery. The patients that could not be bridged were excluded. All procedures were performed through the penoscrotal access and following the same surgical steps according to the Kiel protocol for IPP implantation. For stay sutures, overlapping stay stitches were utilized to achieve water tight closure of the corporotomies after implant placement. Our drain of choice was a 12 French closed suction drain routing below the corporotomies and behind the pump in all the patients. For closure, Dartos and skin layers were closed by interrupted sutures in a locking fashion for wound sealing. All patients received the same perioperative antibiotic prophylaxis. Devices were left partially inflated (75%) and a mummy wrap was applied for all the patients for 24 h. The urethral catheter was removed after 48 h and all patients were discharged after the 3rd postoperative day. Patients were divided into 3 groups. No drain was inserted in Group 1 patients (n = 114); a drain was inserted for 24 h in Group 2 (n = 114) and for 72 h in Group 3 (n = 117). Out of the surgical outcomes the presence or absence of postoperative scrotal hematoma and infection were the focus of our study. They were evaluated and compared between the three groups. We defined hematoma as a scrotal swelling correlated with ultrasonographic evidence of scrotal free-floating fluid. An US scan was carried out on day 1, 3 and 10 postoperatively. Patients were followed up for 80 days postoperatively. This study was approved by the ethical committee of the Christian Albrecht’s University of Kiel, Germany (D 444/19).
Statistical analysis
Using SPSS version 26 for windows, data was entered, coded and analyzed. All variables were categorized where they were described as numerical and percentage. Chi squared and Exact tests were used when required (referred in the tables). Binary logistic regression analysis was used to compare the prevalence of complications in the 3 different Groups. A p value < 0.05 was considered significant.
Results
Table 1 demonstrates that there was no statistically significant difference among the 3 groups with regards to age, BMI, comorbidities, type of implant utilized and operative time. (Table 1) After the first day of surgery, the no-drain group ranked highest in hematoma incidence [8.8%], followed by the 24 h group [5.3%] and the 72 h group [1.7%] (p = 0.05). On the 3rd postoperative day, both drained groups (24 and 72 h drain) demonstrated a statistically significant lower incidence of hematoma in [6.1% and 0.9%, respectively] vs. the no-drain group [11.4%] (p = 0.004). Nevertheless, when we separately compared the no-drain group to the 24 h drain group (p = 0.157) and the 24 h to the 72 h drain group (p = 0.031), this difference, although may be clinically significant, wasn’t statistically significant. It was statistically significant only when we compared the 72 h group with the no-drain group (p = 0.001). On the 10th day after surgery, we identified a statistically significant lower incidence of hematoma in patients who had a drain for 72 h [0.9%] compared to the 24 h group [9.6%] and the no-drain group [7%], (p = 0.013). There was also a statistically significant lower incidence of hematoma when we separately compared patients in the no-drain group with the 24-group (p = 0.017) and patients in the 24 h group with 72 h group (p = 0.003). However, the difference wasn’t statistically significant when we compared the no-drain group with the 24 h group (p = 0.477). (Table 2 and Fig. 1).
Hematoma rates were highest in the no-drain group 24 h after surgery [8.8%], followed by the 24 h group [5.3%] and lowest in the 72 h group [1.7%] (p = 0.05). Although hematoma rates failed to demonstrate a statistical difference on the 3rd postoperative day comparing the no-drain to the 24 h drain group [11.4% and 6.1%, respectively] (p = 0.157) and the 24 h to the 72 h, separately [6.1% and 0.9 %, respectively] (p = 0.031), the hematoma rates were significantly different comparing the 2 drained groups vs. the no-drain group (p = 0.004). On the 10th day post-surgery, we identified a statistically significant lower incidence of hematoma with prolonged drainage [0.9%] compared to short term drainage [9.6%] and non-drainage [7%], (p = 0.013).
The stratification of the groups by surgical time (under or above 60 min) did not affect our results regarding the incidence of hematoma with superiority remaining for the 72 h drain group.
Early postoperative infection rates were highest in the no drain group [4.4%] followed by the 24-drain group [3.5%] and lowest in the 72 h group [0.9%]. Despite the clinical significance of such differences, there were no significant statistical differences (p = 0.210). Interestingly, the only significant factor associated with the increased incidence of postoperative infection was the occurrence of a hematoma at 24 h after surgery (p = 0.01). The presence of a drain was not found to be a risk for infection. This was demonstrated after adjusting for age, presence of diabetes and intraoperative time, in the presence of a drain for 24 and 72 h, and the presence of hematoma at 24 h (Table 3).
Discussion
Minimizing hematoma formation after IPP insertion is paramount to reduce patient discomfort, to allow for a quicker healing and activation of the device, and possibly, to reduce the risk of infection of the device. In a series of 917 patients, Wilson et Al. assessed the efficacy of closed drain insertion and compressive dressing at preventing the formation of scrotal hematomas. In particular, he subdivided his patients in 3 groups. In the first group (163 patients) only a pressure dressing to the genitalia was applied while in the second group (255 patients) a drainage and pressure dressing were used. In the third group instead (555 patients) a combination of insertion of a drain, application and a compressive dressing and partial inflation of the cylinders (70% inflation) were attempted with the aim of reducing hematoma formation. The overall risk of hematoma formation, which was the highest in group 1, was 3.6% in the second group and 0.9% in the third group [8].
In another series of 600 patients where CSD was placed for 24 h with partial inflation of the devices without any pressure dressing, the reported prevalence of delayed hematoma was 0.5% (>5 days postoperative). According to Garber et al., hematoma formation was related to premature administration of anticoagulants or early vigorous physical activity [15].
Apoj et al. used a combination of pressure dressing, full inflation of devices and drainage placement for 24 h. The authors reported no incidence of hematoma or infection in 169 IPP undergoing patients [16].
Sadeghi-Nejad et al. evaluated the rate of infection and hematoma formation using closed suction drain in 425 patients after IPP implantation through a penoscrotal approach. Nonantibiotic impregnated non-hydrophilic devices were used in this study. The rate of infection was 3.3%, while the rate of hematoma was 0.7%. Drainage was removed after the first 24 h. They concluded that the placement of a closed suction drain did not increase the rate of infection and was associated with a lower incidence of hematoma formation [7].
The hypothetical relation between the utilization of a scrotal drain and IPP infection is questionable, although the theoretical risk of retrograde migration of organisms from the point of insertion of the drain to the scrotal cavity may be considered. In order to shed more light on this concept, Wallen assessed cultures obtained from the proximal and distal end of 130 drains placed for 48 or 72 h after IPP surgeries. Only 1.5% grew bacteria, but none of them developed a clinical infection. The rate of hematoma formation was 1.5% in the same study [17]. Similar results were reported by Rojas-Cruz et Al. in a series of 63 patients were, although drain cultures were positive in 6% of patients none of these patients developed a clinical infection. The rate of hematoma formation was 1.5%. Based on these findings, they concluded that there was no relation between using CSD and IPP infections [18].
Meng et al. compared brief (<24 h) vs. prolonged (average duration 4.7 days) closed suction drain insertion after IPP surgery. They failed to identify any significant difference in infection rates between the two groups (0.9% vs. 1.7%, respectively, p = 1), although hematoma formation rate was significantly lower in the prolonged drainage group 14.4% vs. 26% (p = 0.02). In this series infection rates did not increase in the prolonged drainage group suggesting that the retrograde migration of organisms theory was unlikely [19].
In a multicenter prospective study (PROPPER study), 1348 patients were stratified into drain 634 (47%), and no-drain 714 (53%) groups. The study group observed hematoma formation only in the drain group (0.006%) while none in the no-drain group (p = 0.034) possibly because drains were more likely used in the more complex (and more likely to bleed) cases. Even in this series drainage usage was not associated with higher infection rates [16].
In our study the surgical outcome in patients post IPP without drainage (Group 1- 114 patients), with short term drainage (Group 2- 114 patients, 24 h) and prolonged drainage (Group 3- 117 patient, 72 h) were evaluated. On the tenth follow up day, the prevalence of hematoma was the lowest in Group 3 [0.9%] and highest in Group 1 [9.6%], (p = 0.013). The incidence of infection requiring device removal was highest in Group 1 [4.4%], followed by Group 2 [3.5%] and lowest in Group 3 [0.9%] (p = 0.210). The findings of the current series support our previous conclusion that prolonged drainage reduces the risk of hematoma formation without increasing the risk of infection [20].
We are aware of the strengths and limitations in our study. Although we studied a large cohort yet population distribution was not randomized. Preoperative counseling and postoperative management of the patients may be heterogeneous owing to the multicentric nature of our study.
Conclusions
Prolonged drainage for up to 72 h after virgin IPP implantation significantly reduces hematoma formation and the risk of infections regardless of surgical time.
Due to the nature of this series, its results need to be confirmed by larger randomized trials, which can be possible only after the establishment of the European Registry.
Data availability
The dataset on which this paper is based is securely retained with the corresponding author. Documentation and methods used to support this study are available via the corresponding author.
References
Barton GJ, Carlos EC, Lentz AC. Sexual Quality of Life and Satisfaction With Penile Prostheses. Sex Med Rev. 2019;7:178–88.
Bettocchi C, Palumbo F, Spilotros M, Lucarelli G, Palazzo S, Battaglia M, et al. Patient and partner satisfaction after AMS inflatable penile prosthesis implant. J Sex Med. 2010;7:304–9.
Govier FE, Gibbons RP, Correa RJ, Pritchett TR, Kramer-Levien D. Mechanical reliability, surgical complications, and patient and partner satisfaction of the modern three-piece inflatable penile prosthesis. Urology. 1998;52:282–6. https://pubmed.ncbi.nlm.nih.gov/9697795/.
Habous M, Tal R, Tealab A, Aziz M, Sherif H, Mahmoud S, et al. Predictors of Satisfaction in Men After Penile Implant Surgery. J Sex Med. 2018;15:1180–6.
Köhler TS, Hellstrom WJG. Using wound drains for the uncomplicated penile prosthesis. J Urol. 2011;186:1187–9. https://pubmed.ncbi.nlm.nih.gov/21849194/.
Kramer A, Goldmark E, Greenfield J. Is a Closed-Suction Drain Advantageous for Penile Implant Surgery? The Debate Continues. J Sex Med. 2011;8:601–6.
Sadeghi-Nejad H, Ilbeigi P, Wilson SK, Delk JR, Siegel A, Seftel AD, et al. Multi-institutional outcome study on the efficacy of closed-suction drainage of the scrotum in three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2005;17:535–8. https://pubmed.ncbi.nlm.nih.gov/15988544/.
Wilson S, Cleves M, Delk JI. Hematoma formation following penile prosthesis implantation: to drain or not to drain. J Urol. 1996;634A:55.
Perito PE. Minimally invasive infrapubic inflatable penile implant. J Sex Med. 2008;5:27–30. https://pubmed.ncbi.nlm.nih.gov/18173764/.
Grande P, Antonini G, Cristini C, De Berardinis E, Gatto A, Di Lascio G, et al. Penoscrotal versus minimally invasive infrapubic approach for inflatable penile prosthesis placement: a single-center matched-pair analysis. World J Urol. 2018;36:1167–74.
Kim YH, Cho SH, Kim RS. Drainage versus nondrainage in simultaneous bilateral total hip arthroplasties. J Arthroplasty. 1998;13:156–61.
Garber BB. Mentor alpha 1 inflatable penile prosthesis: Patient satisfaction and device reliability. Urology. 1994;43:214–7.
Parker MJ, Livingstone V, Clifton R, McKee A. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. 2007;2007:CD001825 https://doi.org/10.1002/14651858.CD001825.pub2.
Cruse PJE, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206–10. https://pubmed.ncbi.nlm.nih.gov/4719566/.
Garber BB, Bickell M. Delayed Postoperative Hematoma Formation after Inflatable Penile Prosthesis Implantation. J Sex Med. 2015;12:265–9.
Karpman E, Brant W, Kansas B, Bella A, Christine B, Jones L, et al. 120 Drain Use During Penile Prosthesis Surgery, Results From The PROPPER Study. J Sex Med. 2018;15:S28 http://www.jsm.jsexmed.org/article/S1743609517317022/fulltext.
Wallen J, Beilan J, Emtage J, Bickell M, Martinez D, Carrion R, et al. 062 “Just the Tip” Closed Suction Drain Cultures after Implantation of Penile Prosthesis. J Sex Med. 2016;13:S30 http://www.jsm.jsexmed.org/article/S1743609516002083/fulltext.
Rojas-Cruz C, Sarquella J, Vazquez A. Drain cultures in penile prosthesis implants. J Urol. Vol. 181, No. 4, Supplement, Monday, April 27, 2009.
Meng Y, Song DG, Brown S, Vetter JM, Bullock AD. 255 Prolonged closed suction drains lowered hematoma rates and facilitated early pump operation after inflatable penile prosthesis implantation. J Sex Med. 2018;15:S224 http://www.jsm.jsexmed.org/article/S1743609518304922/fulltext.
Osmonov D, Bannowsky A, Juenemann KP. PO-01-079 Prospective evaluation of the surgical outcome in patients without drain, with a 24-hour drain, and with prolonged drain after inflatable penile prosthesis implantation. J Sex Med. 2019;16:S69 http://www.jsm.jsexmed.org/article/S1743609519306794/fulltext.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
DO, AR: idea of the project, study design. DO, AR: creation of the paper. TP, GL, AE: data collect. CB, KvR, HP, EC: editing and advice. MTF, AGM: statistics. GG, SKW: English grammar check, editing. KPJ, SKW: supervising.
Corresponding author
Ethics declarations
Competing interests
DO is consultant of Coloplast Porgés, Rigicon. KvR is consultant of Coloplast Porgés, Boston Scientific. CB is consultant of Boston Scientific. AR is consultant of Coloplast Porgés. GG is consultant of Boston Scientific. EC is consultant Coloplast Porgés, Rigicon. SW is consultant of Rigicon.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Osmonov, D., Ragheb, A.M., Petry, T. et al. Value of prolonged scrotal drainage after penile prosthesis implantation: a multicenter prospective nonrandomized pilot study. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00710-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00710-8
This article is cited by
-
Erectile device insertion following phalloplasty in transgender and non-binary individuals assigned female at birth: a narrative review
International Journal of Impotence Research (2023)
-
Commentary: Value of prolonged scrotal drainage after penile prosthesis implantation: a multicentre prospective nonrandomized pilot study
International Journal of Impotence Research (2023)
-
Risk of unfavorable outcomes after penile prosthesis implantation – results from a national registry (INSIST-ED)
International Journal of Impotence Research (2023)