Abstract
In June 2022 the United States Supreme Court issued a ruling in the case Dobbs v. Jackson that overturned Roe v. Wade, the 1973 ruling establishing a federally protected right to abortion in the United States. Anecdotal reports suggested increased vasectomy volume following this event; however, no published data exist. We sought to describe trends in vasectomy consultation before and after the Dobbs v. Jackson ruling (referred to as pre- and post-Dobbs herein). Following IRB approval, we reviewed charts of all adults seeking vasectomy consultation in July–August 2021 and July–August 2022 at a large healthcare organization. We then aggregated vasectomy procedural billing data from 2018 to present. The primary outcome was volume of vasectomy consultation appointments and the secondary outcome was number of vasectomies performed. In July–August 2021 (Pre-Dobbs), 116 men attended vasectomy consultation versus 142 men in July–August 2022 (Post-Dobbs). Median age Post-Dobbs was significantly younger than Pre-Dobbs (35 vs 38 years, respectively, p = 0.01) with a significant increase in Post-Dobbs men under 30 seeking vasectomy (p = 0.005). A total of 16.9% (24/142) of Post-Dobbs men were childless, compared to 8.6% (10/116) of Pre-Dobbs men (p = 0.05). Of those with children, median number of offspring was unchanged at 2. Billing data showed a significant increase in vasectomy procedural volumes Post-Dobbs. While overturning Roe v Wade directly impacted female reproductive rights, number of vasectomy consultations and procedures increased significantly following this decision. Younger men, especially those under 30, as well as childless men were significantly more likely to seek consultation Post-Dobbs compared to the prior reproductive legal climate. While longer-term data are needed, findings indicate that men are invested in maintaining reproductive autonomy for themselves and their partners.
Similar content being viewed by others
Introduction
On June 24, 2022, the United States Supreme Court issued a 6–3 ruling in Dobbs vs. Jackson Women’s Health Organization, with Justice Alito writing the majority opinion that “procuring an abortion is not a fundamental constitutional right because such a right has no basis in the Constitution’s text or in our Nation’s history” [1]. The ruling, which was leaked in draft form 2 months prior, overturned the landmark 1973 Roe v. Wade decision that established a federally protected right to abortion during the first two trimesters of pregnancy and gave each state the power to set its own abortion laws [2]. A review of Gallup polls dating back to 1989 found that almost 60% of Americans have consistently supported federal protection for abortion rights across three decades and through multiple generations [3]. Until June 2022, reproductive autonomy protections had been the law of the land for all reproductive-age women living in the United States.
While this legal decision directly impacted the reproductive rights of females and their bodily autonomy, the decision appears to have exerted profound effects on men too. There have been multiple media outlets reporting on anecdotal increases in the number of men seeking permanent contraception following this event [4,5,6]. Despite these assertions, no peer-reviewed published data yet exist on this phenomenon.
We sought to describe for the first time the trends in vasectomy consultation and completion at a large healthcare organization by comparing men presenting for vasectomy consultation in the Pre-Dobbs era compared to the Post-Dobbs era. Because there is a delay in completing the procedures due to provider availability and insurance restrictions, our primary outcome of interest was the number of vasectomy consultations and our secondary outcome included the number of vasectomy procedures performed.
Methods
Following institutional IRB approval, we performed a retrospective review of all adult patients seeking consultation for vasectomy in July–August 2021 compared to July–August 2022 at a large midwestern academic healthcare system including 13 community hospitals. The follow-up period for patients seen in July–August 2022 (the “Post-Dobbs” cohort) was 3 months, while the July 2021 (the “Pre-Dobbs cohort”) was 16 months but was truncated to 3 months for the purposes of statistical analysis. In parallel, we also obtained the billing data for all patients at our institution who underwent vasectomy (Current Procedural Terminology code 55250) between 2018 and 2022.
Demographic data including age, ethnicity, marital status and number of children were extracted from the medical record, aggregated, and analyzed using descriptive statistics. Comparisons were performed between patients attending consultation in July–August 2021 versus July–August 2022 with regard to age, race, number of children, marital status and vasectomy completion with t-test and χ2 tests where appropriate. The average vasectomy procedural volume for July to September 2018–2021 was compared to the average vasectomy procedural volume for July to September 2022. Threshold for statistical significance was set a priori at p ≤ 0.05. Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp.
Results
The primary analysis of vasectomy consultation volume focused on the July–August 2021 (Pre-Dobbs) and July–August 2022 (Post-Dobbs) cohorts. In the Pre-Dobbs cohort, 123 men initiated requests for vasectomy consultation and 116 men actually attended the appointment with a urology provider. In the Post-Dobbs cohort, 166 men initiated requests for vasectomy consultation and 142 men actually attended an appointment. The visit attendance rate in 2021 was higher than in 2022 (94.3% vs 85.5%, p = 0.02), although 17 Post-Dobbs appointments were scheduled 3 or more months out and had not taken place at the time of data collection. Overall, there was a 35.0% increase in vasectomy consultation requests and a 22.4% increase in vasectomy consultations from Pre-Dobbs to Post-Dobbs.
The median age of the Post-Dobbs cohort was significantly younger at 35 years old (IQR 10) compared to 38 years old (IQR 9) in the Pre-Dobbs cohort (p = 0.01) and there was a significant increase in Post-Dobbs men under 30 seeking vasectomy versus pre-Dobbs (23.9% vs 10.3%, p = 0.005). The self-reported race of men seeking vasectomy in 2022 versus 2021 is shown in Table 1. The proportion of white men seeking consultation significantly increased in July 2022 (83.8% vs 70.7%, p = 0.01).
Seventy-two percent of men in the Post-Dobbs cohort were married compared to 78% in the prior year (p = 0.29). There was also a significant increase in childless men seeking vasectomy Post-Dobbs at 16.9% (24/142) vs 8.6% (10/116) men (p = 0.05). The median number of offspring for each patient seeking vasectomy consultation was 2 in both groups (IQR 1).
At 3-month follow-up, 58.6% (68/116 consultations) of Pre-Dobbs men had completed their vasectomy versus 66.2% (94/142 consultations) of Post-Dobbs men (p = 0.21). At 16-month follow-up, the vasectomy completion rate for men initially seen in July–August 2021 was 79.3% (92/116).
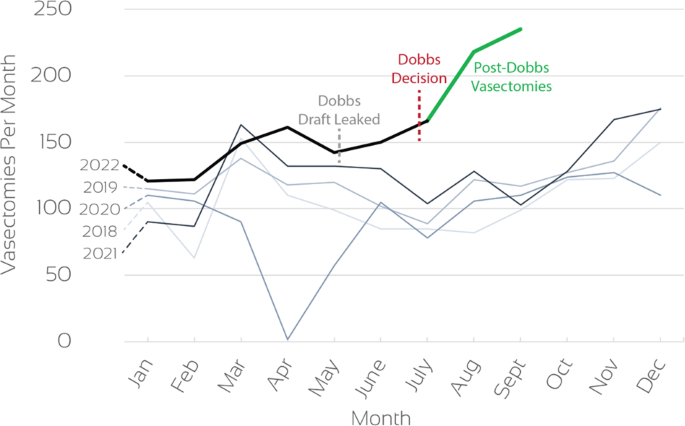
In order to further examine our secondary endpoint, billing data for all patients who underwent vasectomy within our healthcare system from 2018 to August 2022 was extracted. Our results showed a significant increase in median (IQR) vasectomy procedural volume following the 2022 Dobbs decision, increasing from 104 (24) vasectomies per month to 218 (35) vasectomies per month (p = 0.03, Fig. 1).
Discussion
Permanent contraception for premenopausal women typically involves abdominal surgery to ligate or occlude the fallopian tubes. While overall safe, this is still a procedure with inherent risks such as pain, transfusion risk, infection, damage to abdominal strictures and risks of general anesthesia [7].
In contrast, permanent contraception for men via vasectomy involves a straightforward minimally invasive procedure in the scrotum [8]. Despite the fact that vasectomy is less invasive and safer, tubal ligation has historically accounted for the majority of surgeries performed for permanent contraception in the United States [8, 9]. Approximately 16% of women undergo tubal ligation as a sterilization technique compared with only 6% of men who undergo vasectomy [10]. In fact, one study even demonstrated a decrease in the number of vasectomies performed from 2007 to 2015 in the United States across all ages and geographic locations [11].
While women appear to have historically taken on more responsibility regarding the decision to avoid future offspring, the overturning of Roe v. Wade in June 2022 has changed the landscape of family planning for male partners as well. Multiple news organizations covered stories about non-published reports of more men seeking vasectomies all across the country [4,5,6]. We hypothesized that increased discussion around reproductive rights and a strong desire by some couples to avoid legal jeopardy may have contributed to assertive decision making among single and partnered individuals, some of whom may have already considered pursuing elective sterilization but had not yet found the impetus to do so.
In this manuscript, we report clinical data from a high-volume academic medical institution showing a significant increase in vasectomy procedural volumes following Dobbs (Fig. 1). While the overall increase in procedural volume includes patients who had initiated consultation prior to the ruling, the legal decision may have prompted many to actually schedule vasectomy rather than putting it off. Within the short interval after this decision, our hospital network also experienced a rise in new vasectomy consultation requests of 35.0% and vasectomy consultation visits of 22.4% compared to the same time period the year prior. Interestingly the rate of men who actually attended their appointment was lower in 2022, showing that some men ultimately did not feel compelled to pursue vasectomy after initial fact-searching. However, when examining the preliminary 3-month follow-up period after consultation in the July–August cohorts, we found that men were proceeding with the vasectomy procedure at a similar rate, indicating that patients who came to appointments were truly interested in acting.
There were multiple other notable findings in our analysis. After Roe v Wade was overturned in June 2022, men seeking vasectomy were significantly younger (35 vs 38 years, p = 0.01) and far more likely to be under the age of 30 (23.9% vs 10.3%, p = 0.005). The median age of men undergoing vasectomy has previously been described at approximately 37 or 36 years of age depending on urban versus rural location [12]. This surge of younger men choosing to undergo permanent contraception half a decade earlier than historical rates should not be dismissed as expected change over time. The immediacy with which this change was seen indicates that the Post-Dobbs generation has already been significantly affected by the legal climate and the population-based consequences of this decision will continue to be seen in multiple ways for decades to come.
Interestingly there was no change in the proportion of single or married men pursuing vasectomy pre and post Roe v Wade overturning. However, there was a significant increase in childless men pursuing vasectomy after the legal ruling. We hypothesize that both single and partnered men who have decided not to have further offspring now feel it necessary to take reproductive autonomy into their own hands. The invasiveness of female permanent contraception may have some bearing on this decision, but changes in the rates of tubal ligation for women Post-Dobbs have yet to be described.
Prior studies have described racial and ethnic differences in men seeking vasectomy in the United States [10]. Consistent with the published literature, we also found that the majority of men in our study self-identified as white for both years. There was a significantly higher percentage of white men seeking vasectomy after Roe v Wade was overturned, and a significant decrease in African American men (Table 1). The reasons for this are likely multifactorial in nature, and could include uneven access to healthcare, and differing perceptions of the reproductive legal climate. However, larger numbers would be needed in order to accurately assess for these factors.
One limitation of our study is the short duration of follow-up for the July/August 2022 cohort. In order to minimize the risk of bias in interpreting results such as surgical scheduling, we compared the 3-month vasectomy completion rate in both the 2021 and 2022 cohorts and found these to be similar. In addition, our procedural volume also reflects the increase in consultation, which further strengthens the conclusion that vasectomy interest rose post-Dobbs. Another limitation is the single-institutional nature of our study. However, as our institution is a large quaternary referral center including a network of 13 community hospitals serving our racially diverse region in both urban and rural settings, the database used is likely representative of the greater population. It is also important to note that this study was carried out in Ohio, a state that activated a “heartbeat bill” (Ohio Revised Code, 2919.195) very soon after Roe v Wade was overturned. At the time of writing this manuscript, an Ohio state judge temporarily blocked this law from taking effect based on a challenge from the Ohio American Civil Liberties Union and further deliberations are pending. A strength of our study is that comparison of the same months (July–August) in two different years limits the inherent variability in surgery consultation and scheduling, as patients consider multiple factors when making medical appointments that are unrelated to the legal landscape [4]. One unique factor that has affected elective medical appointment scheduling over recent years is the COVID-19 pandemic, and it is important to note that during the July–August 2021 time period compared, there was no active national or Ohio-wide surge in cases which would have decreased our volumes. Further study regarding vasectomy consultation and scheduling across the country should be encouraged and is ongoing at our institution.
Conclusion
While the loss of the federally protected right to abortion directly impacted the reproductive rights of women, we demonstrate for the first time that biological males with the potential to cause pregnancy have also been deeply affected as reflected by their reproductive healthcare decisions. An increase in vasectomy consultation visits was seen post-Dobbs, especially among younger men and childless men. Our overall vasectomy procedural volume also demonstrated a significant rise after July 2022 as compared to past years.
While longer-term and multi-institutional data are needed to study this phenomenon, it is clear from our findings that men remain engaged with reproductive autonomy for themselves and for their partners and are capable of rapidly acting when prompted by external stimulus. Legal rulings on reproductive health can have an impact far beyond the boundaries of gender. Policymakers should keep this in mind when discussing issues concerning healthcare and medical decision making.
Data availability
The original data can be made available via the corresponding author upon reasonable request.
References
United States Reports. Dobbs, State Health Officer of the Mississippi Department of Health et al. v. Jackson Women’s Health Organization et al. Vol. 597. 2022.
United States Reports. Roe et al. v. Wade, District Attorney of Dallas County. Vol. 410. 1973. p. 113.
Saad L. Where Do Americans Stand on Abortion? The Gallup Organization; June 15, 2022.
Dzhanova Y. “I just don’t want children”: some American men are turning to vasectomies after the Supreme Court’s decision to overturn Roe. Business Insider. 2022. https://www.businessinsider.com/how-roe-v-wade-affects-men-american-vasectomies-abortion-2022-8. Accessed 9 Jan 2023.
Taylor S. Why men as young as 23 are choosing vasectomies in post-Roe America. Bloomberg. 2022. https://www.bloomberg.com/news/articles/2022-07-08/vasectomy-interest-surges-among-men-after-roe-v-wade-decision?leadSource=uverify wall. Accessed 9 Jan 2023.
Ducharme J. Vasectomies are going viral after the Roe v. Wade leak, but they aren’t a solution to abortion bans. Time Magazine. 2022. https://time.com/6178287/vasectomy-sterilization-roe-v-wade/. Accessed 9 Jan 2023.
Huber AW, Mueller MD, Ghezzi F, Cromi A, Dreher E, Raio L. Tubal sterilization: complications of laparoscopy and minilaparotomy. Eur J Obstet Gynecol Reprod Biol. 2007;134:105–9.
Velez D, Pagani R, Mima M, Ohlander S. Vasectomy: a guidelines-based approach to male surgical contraception. Fertil Steril. 2021;115:1365–8.
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin No. 208: benefits and risks of sterilization. Obstet Gynecol. 2019;133:194–207.
Eisenberg ML, Henderson JT, Amory JK, Smith JF, Walsh TJ. Racial differences in vasectomy utilization in the United States: data from the national survey of family growth. Urology. 2009;74:1020–4.
Ostrowski KA, Holt SK, Haynes B, Davies BJ, Fuchs EF, Walsh TJ. Evaluation of vasectomy trends in the United States. Urology. 2018;118:76–9.
Machen GL, Bird ET, Kavoussi PK. Analysis of urban vs. rural vasectomy demographics: a multi-institutional, retrospective comparison. Transl Androl Urol. 2018;7:931–4.
Author information
Authors and Affiliations
Contributions
RB, SDL, EP, PB, NP and SCV conceived and designed the work, acquired data and interpreted results. RB, SDL, EP, PB, NP and SCV drafted or revised the manuscript. RB, SDL, EP, PB, NP and SCV approved the final version and RB, SDL, EP, PB, NP and SCV agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bole, R., Lundy, S.D., Pei, E. et al. Rising vasectomy volume following reversal of federal protections for abortion rights in the United States. Int J Impot Res 36, 265–268 (2024). https://doi.org/10.1038/s41443-023-00672-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-023-00672-x
This article is cited by
-
The percentage of men counseled by urologists who received a vasectomy mildly increased after the publication of the AUA vasectomy guideline
International Journal of Impotence Research (2024)
-
Uncovering the interhospital price variations for vasectomies in the United States
International Journal of Impotence Research (2024)