Abstract
Next-generation sequencing (NGS) technologies are now established in clinical laboratories as a primary testing modality in genomic medicine. These technologies have reduced the cost of large-scale sequencing by several orders of magnitude. It is now cost-effective to analyze an individual with disease-targeted gene panels, exome sequencing, or genome sequencing to assist in the diagnosis of a wide array of clinical scenarios. While clinical validation and use of NGS in many settings is established, there are continuing challenges as technologies and the associated informatics evolve. To assist clinical laboratories with the validation of NGS methods and platforms, the ongoing monitoring of NGS testing to ensure quality results, and the interpretation and reporting of variants found using these technologies, the American College of Medical Genetics and Genomics (ACMG) has developed the following technical standards.
Similar content being viewed by others
A. INTRODUCTION
Since the ACMG first published guidance for laboratories performing next-generation sequencing (NGS) testing in 2013,1 the field has witnessed a rapid expansion in the use of this technology. NGS throughput, cost, and accuracy for single-nucleotide variant (SNV) detection are often superior to Sanger sequencing.2 This document describes standards for clinical laboratories that use NGS to perform diagnostic gene panel testing, exome sequencing (ES), and genome sequencing (GS) for constitutional variants. While this document attempts to cover issues essential for the development of any NGS test, it does not address specific technologies in detail, and may not cover all issues relevant to each test application or platform-specific characteristics. Testing for somatic variants, cell-free DNA analysis, infectious disease detection, and RNA applications of NGS are beyond the scope of this document.
A.1. Method for standards development
As part of the 5-year review program of ACMG laboratory guidance documents, a new workgroup was established to review and update the existing document.1 To engage the ACMG membership in the review and development process, the workgroup formulated a survey to query those performing NGS testing for constitutional disorders in clinical laboratories. In February 2018, a survey was sent to 512 individuals identified by ACMG as members board certified by the American Board of Medical Genetics and Genomics (ABMGG) or Canadian College of Medical Geneticists (CCMG) in Clinical Molecular Genetics, by the American Board of Pathology in Molecular Genetic Pathology, or self-identified laboratory genetic counselors. A total of 80 responses were received during the 17-day response window. Survey responses were presented in an open forum session attended by >100 individuals at the ACMG annual meeting in April 2018, during which additional comments were collected from attendee discussion. During the revision of these clinical laboratory standards, the opinions of the survey respondents as well as guidance documents issued by government agencies such as the Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC), and the New York State Department of Health, as well as other professional societies such as the Association for Molecular Pathology (AMP), the College of American Pathologists (CAP), and the Canadian College of Medical Geneticists (CCMG) were considered. This document was finalized through iterative review and editing between the workgroup and the molecular genetics subcommittee of the ACMG Laboratory Quality Assurance Committee, accepted by the ACMG Laboratory Quality Assurance Committee, and approved by the ACMG Board of Directors. A draft document was posted on the ACMG website and an email link was sent inviting ACMG members to provide comments. All comments were assessed by the authors. When appropriate, changes were made to address member comments. Both member comments and workgroup responses were reviewed by a representative of the ACMG Laboratory Quality Assurance Committee and by the ACMG Board of Directors. The final document was approved by the ACMG Board of Directors.
A.2. Definitions
A.2.1. Gene panels examine a curated set of genes associated with a particular phenotype, such as hearing loss, or indication, such as procreative management. The sensitivity and specificity of diagnostic gene panels depend, in part, on the sequence coverage of targeted regions and the types of variants that can be detected. By focusing on a limited set of genes, the cost to achieve appropriate coverage is reduced through efficient utilization of sequencing capacity and reduced computational and data storage requirements. Panel tests can maximize clinical sensitivity by not only evaluating the coding and clinically relevant noncoding regions of targeted genes by NGS, but also incorporating ancillary assays, such as Sanger sequencing, to fill in missing content or other methods to detect copy-number variants (CNVs), predefined complex rearrangements, or other specific variant types3 (section D.1.1.3). The ACMG provides guidance on gene inclusion and technical and reporting considerations for diagnostic gene panels.4 The Clinical Genome Resource (ClinGen; www.clinicalgenome.org) framework for gene–disease associations also provides additional guidance. The PanelApp website represents a crowdsourcing tool to allow gene panels to be shared, downloaded, viewed, and evaluated by the scientific public (https://panelapp.genomicsengland.co.uk/panels/).
A.2.2. Exome sequencing (ES) examines the coding and adjacent intronic regions across the genome and requires enrichment of these regions by capture or amplification methods. The exome is estimated to comprise approximately 1–2% of the genome, yet contains the majority of SNVs and small insertions/deletions currently recognized to cause Mendelian diseases. The depth of coverage for an exome is not uniform, therefore the analytical sensitivity of ES may be lower than some disease-targeted gene panels; however, exome sequencing is still expected to have a higher overall diagnostic yield. While Sanger sequencing and other technologies are commonly used to supplement gene panels, this approach is impractical for ES. Analytical sensitivity and specificity may be compromised by inadequate coverage or quality for certain regions.
A.2.3. Genome sequencing (GS) examines over 90% of the genome and has a number of advantages over diagnostic gene panels and ES. In contrast to ES, GS does not require enrichment methods prior to sequencing; therefore, GS produces more even coverage across the exome. GS data can be produced more rapidly than ES data. GS has increased capacity to simultaneously detect SNVs and CNVs, as well as complex variants such as balanced/unbalanced structural rearrangements (e.g., translocations, inversions, and insertions) and repeat expansions.5 There is value in the coverage of noncoding regions for certain pharmacogenetic variants, and increasing numbers of variants in noncoding regions will likely be found to cause monogenic and complex diseases,6 or become part of polygenic risk scores.7 Mitochondrial genome sequence data are also produced and can be analyzed and interpreted. While coverage is more even with GS, the read depth is generally lower than diagnostic gene panels and ES, and may therefore limit the detection of mosaicism.8 The cost of data generation and storage is higher for GS than for ES.
B. CLINICAL USE OF NGS-BASED TESTING
Choosing an appropriate NGS-based test is the responsibility of the ordering health-care provider. Given the large number of tests (https://www.ncbi.nlm.nih.gov/gtr/) available to the clinician, the clinical laboratory often provides critical advice in test selection. Ordering providers must weigh considerations of sensitivity, specificity, cost, and turnaround time for each clinical situation. The clinical sensitivity and diagnostic yield of these testing approaches continue to be compared.9,10,11,12,13,14,15 Laboratories should be available for phone consultation; provide test definition and intended use for each of their tests, as well as general test-ordering guidance on their website; and publish relevant experience in diagnostic detection rates.
Diagnostic gene panels are optimal for well-defined clinical presentations that are genetically heterogeneous (e.g., congenital hearing loss), for which pathogenic variants in disease-associated genes account for a significant fraction of cases. Secondary/incidental findings should not be encountered, although broad panels (e.g., epilepsy, or pan-cancer panels) may identify clinically significant findings unrelated to the test indication. By limiting the test to those genes relevant to a given disease, the panel can be optimized to maximize coverage of relevant regions of the gene(s).4 If a disease-targeted panel contains genes for multiple overlapping phenotypes, laboratories may provide the option to restrict analysis to a subset of genes associated with a specific phenotype (e.g., hypertrophic cardiomyopathy genes within a broad cardiomyopathy gene panel) to minimize the number of variant(s) of uncertain significance (VUS) reported. Assessing the clinical significance of many VUS is challenging. The number of variants with potential clinical relevance is roughly proportional to the size of the target region analyzed.
In contrast to panels, ES or GS provide a broad approach to match detected variants with the clinical phenotype assessed by the laboratory and health-care provider.16 ES may be performed with the intention of restricting interpretation and reporting to variants in genes with specific disease associations with an option to expand the analysis to the rest of the exome if the initial analysis is nondiagnostic. ES/GS approaches are most appropriate in the following scenarios: (1) when the phenotype is complex and genetically heterogeneous; (2) when the phenotype has unusual features, an atypical clinical course, or unexpected age of onset; (3) when the phenotype is associated with recently described disease genes for which disease-targeted testing is unavailable; (4) when focused testing has been performed and was nondiagnostic; (5) when sequential testing could cause therapeutic delays; or (6) when the phenotype does not match an identified genetic condition, suggesting the possibility of more than one genetic diagnosis, which has been documented in 4–7% of positive cases.17,18,19,20 When ES/GS does not establish a diagnosis, the data can be reanalyzed (section E.6). The potential impact of secondary findings with ES/GS should also be considered (section E.3).
C. NEXT-GENERATION SEQUENCING TECHNOLOGY
C.1. Sample preparation
The NGS process begins with the extraction of genomic DNA from a sample. Any validated sample type can be used as long as the quality and quantity of the resulting DNA are sufficient. The laboratory should specify the allowed sample types and quantities of DNA required (section D.2.1).
C.2. Library generation
At present, short-read platforms are used in most clinical laboratories. A library of short DNA fragments (100–500 bp) flanked by platform-specific adapters is the required input for most of the short-read NGS platforms. Fragmentation of genomic DNA is achieved through a variety of methods, each having strengths and weaknesses. Adapter sequences are ligated to both ends of the fragments. Adapters are complementary to platform-specific sequencing primer(s). Notably, not all technologies rely on a complementary primer.21 Polymerase chain reaction (PCR) amplification of the library may be necessary prior to sequencing.
C.3. Indexing
Indexing refers to the molecular tagging of samples with unique sequence-based codes, enabling pooling of samples, and thereby reducing the per sample sequencing cost. In addition, the same sample can be distributed across several lanes or instruments ameliorating the effects of lane-to-lane and instrument-to-instrument variability. Indexes can be part of the adapters or can be added as part of a PCR enrichment step. Dual indexing is typically recommended to reduce the likelihood of index misassignment.22
C.4. Target enrichment
For gene panels and ES, the genes or regions of interest must be enriched prior to sequencing. The targets can range from a relatively small number of genes chosen for a disease-targeted gene panel to the entire exome. Target enrichment approaches include amplicon-based and solid or in-solution oligonucleotide hybridization-based (capture) strategies. Amplicon-based approaches do not scale beyond a limited number of targets. Strategies for target enrichment have been reviewed.23,24,25,26
An analysis of intronic variants in the ClinVar database (Supplemental Table 1) showed coverage encompassing the −16 position at the splice acceptor site and coverage encompassing the +5 position at the splice donor site would detect >97% of the pathogenic and likely pathogenic intronic variants in the ClinVar database; the bias of this data toward reported variants and current sequencing practices is acknowledged. Targeted regions should minimally include coding exons with sufficient intronic coverage to allow analysis of positions −1_−16 and +1_+5 as well as other regions with reported pathogenic variants (e.g., splice sites of noncoding exons, deep intronic variants). It is suggested that laboratories define pathogenic content outside of the standard coding and intronic flanking regions and design probes to ensure coverage of these regions.
C.5. Sequencing platforms and methods
Current commercial platforms use a variety of processes including sequencing by synthesis or sequencing by ligation with reversible terminators, bead capture, ion sensing, and nucleotide sensing through a nanopore.27,28 Each has the capacity to sequence millions of DNA fragments in parallel. Sequencing platform performance varies in clinically important ways (section D.1.1). Table 1 lists some of the considerations required to choose an appropriate platform.
C.6. Data generation
Extensive bioinformatic support and hardware infrastructure are required for analysis. NGS data generation can be divided into four primary operations: base calling, read alignment, variant calling, and variant annotation. Base calling is the identification of the specific nucleotide present at each position in a single sequencing read; this is typically integrated into the instrument software given the technology-specific nature of the process. Read alignment involves correctly positioning DNA sequence reads in relation to a reference sequence. Variant calling is the identification of sequence differences between the sample and a genome reference. Variant annotation associates the variant with relevant contextual information and annotates zygosity (section D.1.3.3).
D. TEST DEVELOPMENT AND VALIDATION
D.1. General considerations
Test development must consider the variant types that will be detected in the genes or regions of the genome interrogated. The test validation process for an NGS test has been outlined.29 Various combinations of instruments, reagents, and analytical pipelines may be used. A limited number of clinical NGS assays are approved by the FDA (https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/InVitroDiagnostics/ucm330711.htm); therefore, most tests will be laboratory developed tests (LDTs) that require a full validation.30 The laboratory director or equivalent may validate a test using commercially available testing components labeled as analyte specific reagent (ASR), investigational use only (IUO), or research use only (RUO). Depending on the intended clinical application of the components, each may be subject to different levels of validation.30
Clinical laboratories should consider the strengths and limitations of their chosen technology. Short-read advantages include SNV and insertion/deletion (indel) calling accuracy,31,32,33 broad use in current clinical practice, a choice of mature analysis software, availability of control samples and associated short-read data for validation, lower cost per base than long-read technology, and the option to produce a rapid (<48 hours) genome. By estimating the anticipated gigabases required, a laboratory can choose a sequencer with suitable capacity.
Short-read sequencing may be performed as single-end sequencing (genomic DNA fragments are sequenced at one end only) or paired-end sequencing (both ends are sequenced). Paired-end sequencing increases unambiguous read mapping, particularly in repetitive regions, and has the added advantage of increasing coverage and stringency of the assay, as bidirectional sequencing of each DNA fragment is performed. A variation of paired-end sequencing is mate-pair sequencing, which can be useful for structural variant detection.32 Although not ideally suited to base calling in repetitive or nonunique regions, technologies and software are being developed to assess these regions using short-read data.34,35,36
Long-read technology is superior to short-read technology in phasing of variants, which is required to establish whether variants for a recessive disorder are in cis or in trans and to determine pharmacogenomic diplotypes. In addition, long reads allow detection of repeat expansion disorders (e.g., fragile X syndrome), CNVs, structural variants such as insertion–translocations, and variants in regions of high homology containing clinically important genes such as CYP2D6, GBA, PMS2, STRC, and the HLA genes.31,34,35,37,38,39,40 See Table 2 for additional comparisons between short-read and long-read sequencing.
D.1.1. Limitations and alternatives
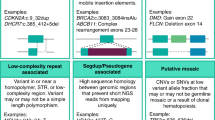
D.1.1.1. Detection of different variant types
Detection of large CNVs, genomic rearrangements, repeat expansions, mitochondrial heteroplasmy, and mosaicism by NGS requires specialized bioinformatic pipelines and highly reproducible, uniform data. Some disease mechanisms such as abnormal methylation require ancillary technologies. It is important to recognize sequence characteristics that may complicate testing or interpretation and when supplementary technologies may be needed to adequately cover the spectrum of pathogenic variants. Detection of mosaicism and heteroplasmic mitochondrial variants requires higher sequence coverage compared to the coverage needed to detect constitutional variants.
D.1.1.2. Regions with technical difficulty
The accuracy of sequence alignment and variant calling can be diminished or biased in genomic regions of high homology or low complexity, as well as repetitive or hypervariable regions.41,42 Hybridization-based enrichment methods used in gene panels and ES cannot avoid capturing homologous regions of targeted genes. The limited length of NGS sequence reads generated by short-read technology can lead to false positive or false negative variant calls when reads are incorrectly aligned to a homologous region. Resources annotating many known regions with high homology have been created (https://www.ncbi.nlm.nih.gov/books/NBK535152/).43 Methods being developed to allow sequencing in problematic regions include:
-
Local realignment after a global alignment strategy
-
Paired-end sequencing to help correct misalignment
-
Informatics tools to force alignment to the region of interest combined with modified variant calling.
Confirmation of variant calls using gene-specific ancillary technology may be necessary. Appropriate caveats specifically addressing potential false negative and false positive results should be reported. Workflows that address accurate, comprehensive diagnostic analysis of genes with known homology issues are available.44,45
D.1.1.3. Ancillary technologies
Clinically relevant genomic regions that cannot be assayed reliably by NGS (e.g., areas with homology, low complexity, methylation) should be considered for testing by ancillary assays.46 Disease-targeted gene panels that include these areas should include appropriate additional methodologies to maximize the clinical sensitivity of the test.4
Sanger sequencing can be used to fill in areas where NGS coverage or quality is insufficient to call variants confidently, but may also be limited by inherent sequencing difficulties (see section D.1.1.2). For ES/GS tests, complete coverage is not expected; however, for gene panel tests the laboratory director or equivalent has discretion to judge the need for Sanger fill-in based on the intended purpose of the test. For diagnostic gene panels, the ACMG provides guidance4 on non-NGS aspects including:
-
Handling of low coverage regions by Sanger fill-in
-
Need for ancillary assays (e.g., CNVs, methylation, repeat expansion) based on the spectrum of pathogenic variants expected for a genetic disorder
-
Disclosures needed at reporting
Projected turnaround times should take into account the time required for these ancillary technologies.
Confirmation of reportable variants using ancillary technologies has been standard practice. Several studies have attempted to determine which metrics could be used to establish parameters for ES/GS approaches, which, when met, would obviate the need for confirmatory testing of SNVs:47
-
Read depth
-
Allele balance
-
Multiple quality scores
-
Strand bias
-
Variant class (e.g., SNV, indel, CNV)
-
Other variant calls nearby
-
Genomic context of the variant (e.g., areas of segmental duplication, homopolymer regions).
Guidance from New York State (NYS) allows SNVs to be reported without orthogonal confirmation once ten SNVs within a gene have been confirmed (https://www.wadsworth.org/regulatory/clep/clinical-labs/obtain-permit/test-approval). However, variants confirmed as true positive (TP) in some samples, can be observed as false positive (FP) in subsequent samples, arguing that prior confirmation alone is insufficient.47 Laboratories should establish and make available a confirmatory testing policy for each variant class, based on a workflow that identifies variants based on laboratory-specific quality metrics drawn from a large and diverse data set as well as visual inspection of read alignments. In the absence of a validated approach, laboratories should continue orthogonal confirmation. For testing involving low allelic fraction variants such as the detection of heteroplasmic mitochondrial variants or germline mosaic variants, other approaches such as replicate testing or testing of additional tissues may be necessary. Identification of large structural variants, such as inversions or gross rearrangements, may require chromosome analysis or fluorescence in situ hybridization (FISH). If the laboratory deviates from their standard practice, for a particular variant, the exception should be noted in the main body of the clinical report.
Laboratory policies should also address instances when the confirmatory test does not support the NGS finding. Confirmatory testing methods such as Sanger sequencing have limitations (e.g., limit of detection, allele drop out). A negative result should not be considered definitive evidence of a FP by NGS.2 Clinical correlation and a second orthogonal test should be considered.
D.1.2. Reference materials
Reference materials (RMs) are used by clinical laboratories for test validation, quality control (QC), and proficiency testing (PT). Initiatives have produced genome-wide RMs for sequence and CNVs. The CDC maintains a list of available RMs here: https://wwwn.cdc.gov/clia/Resources/GETRM/sources.aspx. The Genome in a Bottle Consortium supported by the National Institute for Standards and Technology (NIST) released standardized data for multiple Coriell samples (e.g., NA12878, NA24385, NA24143, NA24149, and NA24631) and two Personal Genome project trios of differing ethnicities.48,49 Additional reference data are appearing regularly.50,51 Long-read sequencing has added to the accuracy of these RMs.37 By comparing internally produced data for these RMs to external data sets, laboratories can more accurately evaluate their test performance. Internal samples assessed by orthogonal methods may also be used as RMs.
While the available RM data is suitable for SNV and small indel performance, robust genome-wide RM data for CNVs, nucleotide repeats, and other genomic variant types are becoming available (https://www.biorxiv.org/content/10.1101/664623v3). A laboratory needs to obtain RMs to represent all appropriate variants or variant classes assessed in their assay.
Note that usage of cell lines as RMs can be limited by genomic stability over time. Genomic DNA extracted from blood is stable, but gathering enough from one individual for long-term, and potentially multilab, use is challenging. Cell lines used as standard RMs for NGS will need to be monitored over time and passages to understand the extent to which instability or usage of amplification techniques impact the samples. Electronic sequences have been computationally generated and can be used as RMs. Simulated sequences are typically designed to address a known issue, such as repetitive sequences, known indels, or SNVs, for which a sample is not available.
D.1.3. Bioinformatic pipelines
Analysis of data generated by NGS platforms is complex and typically requires a multistage data handling and processing pipeline. A wide variety of tools are available and under constant development to improve this process. Analytical pipelines should be developed and optimized separately from the wet lab processes during initial test development by analyzing data containing known sequence variants of various types (e.g., SNVs, small indels, intragenic or large CNVs, structural variants). The optimized pipeline can then be deployed in each end-to-end test validation. When commercially developed software is used, the laboratory should document any validation data provided by the vendor, but must also perform an independent validation of the software. In addition, the laboratory must establish that the bioinformatic pipeline can accurately track sample identity.
The development of standard metrics (section D.3) and well-established RMs (section D.1.2) for performance testing, has significantly improved the capability to perform accurate cross-platform comparisons.48,52 In a joint recommendation by AMP and CAP, standards and guidelines were drafted to aid in validation of bioinformatic pipelines; however, each laboratory must design the appropriate pipeline(s) optimized for its intended clinical use.53 The laboratory should document all hardware, software, databases, including versions used, and additional internally developed systems, and include any modifications or versions if applicable for traceability, that are used in the validated pipeline.54 Basic concepts in the analysis of NGS are outlined below.
D.1.3.1. Base calling
Each NGS platform has specific sequencing biases that affect the type and rates of errors that can occur, including signal intensity decay between the beginning and end of the read and erroneous insertions and deletions in homopolymeric stretches.55 Base-calling software that accounts for technology-specific biases can help address platform-specific issues. The best practice is to utilize a base-calling package that is designed to reduce specific platform-related errors. Generally, an appropriate, platform-specific base-calling algorithm is embedded within the sequencing instrument. Each base call is associated with a quality metric providing an evaluation of the certainty of each call. This is usually reported as a Phred-like score (although some software packages use a different quality metric and measure slightly different variables).
D.1.3.2. Read alignment
Various algorithms for aligning reads have been developed that differ in accuracy and processing speed. Depending upon the types of variants expected, the laboratory should choose one or more read alignment tools to be applied to the data. Several commercially available or open-source tools for read alignment are available that use a variety of alignment algorithms and may be more efficient for certain types of data than for others.56,57,58,59 Alignments are typically stored in standard binary alignment map (BAM) format, although newer compressed and/or secured file formats (CRAM/SECRAM) are also available.60 Proper alignment can be challenging when the captured regions include homologous sequences, but is improved by longer or paired-end reads. In addition, alignment to the full reference genome should be performed, even for ES and disease-targeted testing, to reduce mismapping of reads from off-target capture, unless appropriate methods are used to ensure unique selection of targets.
D.1.3.3. Variant calling and annotation
Increasing sequencing depth and removing duplicate reads increases the accuracy of single or multiple base variant calling. Specific algorithms may be required to detect insertions and deletions (indels), intragenic or large CNVs, repeat expansions, variants in regions of high homology, mitochondrial variants, and structural chromosomal rearrangements (e.g., translocations, inversions). Local realignment after a global alignment strategy can help more accurately call indel variants.61,62 Large deletions and duplications can be detected by comparing actual read depth of a region to the expected read depth, through paired-end read mapping (independent reads that are associated to the same library fragment), skewed allelic ratios, or apparent non-Mendelian transmission of variants. Paired-end and mate-pair (joined fragments brought from long genomic distances) mapping can also be used to identify translocations and other structural rearrangements.
Variant annotation software uses the fraction of reads to differentiate between heterozygous and homozygous sequence variants; however, an unambiguous zygosity call is not always possible and could reflect mosaicism (section D.2.4). Software annotates the variant with relevant information such as the genomic coordinates, coding sequence nomenclature, protein nomenclature, and position relative to gene(s) (e.g., untranslated region, exon, intron). Ideally, the annotation will also include additional information from external resources (as discussed in section E) that facilitates determination of its analytic validity and clinical significance, such as quality metrics and allele frequency in internal and external data sets. This information may also include the degree of evolutionary conservation of the encoded amino acid and a prediction of its potential impact on protein function, gene regulation, or RNA splicing using in silico algorithms.
D.1.3.4. Phase determination
Two variants that are adjacent or close together are particularly challenging to annotate. While each variant substitution is typically tabulated separately, the consequence of the two substitutions must be considered together. For example, two adjacent changes in the triplet codon for a given amino acid may be different from each change considered separately. Bioinformatic pipelines may be adjusted to account for these scenarios but manual curation may be required. When more than one variant is identified in the same gene, it is important to determine whether they are located on the same chromosome (in cis) or opposite chromosomes (in trans). If the difference in the genomic positions for the variants is less than the read length, it is likely that phase can be determined from standard NGS reads. Phase has traditionally been established by targeted testing of parents or other first-degree relatives or trio analysis, but newer technologies are available for determination of phase from a single individual based on short-read sequencing.63
D.1.3.5. File formats
Many different formats have existed for the export of raw variants and their annotations. Each variant file format typically includes a definition of the file structure and the organization of the data, specification of the coordinate system being used as part of the file generated (e.g., the reference genome to which the coordinates correspond, whether numbering is 0-based or 1-based, and the method of numbering coordinates for different classes of variants), and the ability to interconvert to other variant formats and software. If sequence read data are provided as the product of an NGS test, they should conform to one of the widely used formats (e.g., BAM files for alignments, FASTQ files for sequence reads) or have the ability to be readily converted to a standard format. The variant call format (VCF) is a structured text file format that conveys data about specific positions in the genome as well as meta-information about a given data set. It should be noted that the VCF file format is typically limited to variant calls. Many advocate for the inclusion of reference calls in the VCF format (gVCF file) to distinguish the absence of data from reference sequence. Even within this prescribed format, ambiguities can arise when representing complex genetic variants. These should be addressed in order to implement automated duplicate removal and/or variant filtering.64 The CDC has spearheaded an effort to develop a consensus gVCF file format, with specific recommendations regarding reference sequence alignment, variant caller settings, use of genomic coordinates, and gene and variant naming conventions, with the goal of reducing ambiguity in the description of sequence variants and to facilitate genomic data sharing.65 Many genomic file formats are now maintained by GA4GH as international standards (https://www.ga4gh.org/genomic-data-toolkit/).
D.1.3.6. Variant filtering processes
Variant filtering pipelines use a variety of approaches to streamline and automate the process based on reportable data required for a given test. Initial variant filtration processes should maximize analytical sensitivity and minimize false negatives. Subsequent filtration can then be used to increase specificity. To this end, a laboratory should establish a series of variant inclusion and exclusion filters (i.e., filter in versus filter out) based on conditional properties that will accurately and reliably identify the reportable variants for a given test. While these processes can be automated, it is recommended that manual processes exist to view variants filtered out from a given test when necessary. Suggestions regarding filtering relative to variant interpretation and specificity are discussed in section E.2.1.
D.1.4. Staff qualifications
Given the technical and interpretive complexity of NGS, reporting and oversight of clinical NGS-based testing should be performed by individuals with appropriate professional training and certification. The laboratory director or qualified designee should have ABMGG certification in Clinical Molecular Genetics and Genomics or Laboratory Genetics and Genomics or American Board of Pathology certification in Molecular Genetic Pathology, or a foreign equivalent. Directors should have extensive experience in the evaluation of sequence variation and evidence for disease causation as well as technical expertise in sequencing technologies and bioinformatics. For laboratories offering ES/GS services, the laboratory should have access to broad clinical genetics expertise to evaluate the relationships between genes, variants, and disease phenotypes.
Expertise within the laboratory must include a detailed working knowledge of the analytical procedures, data interpretation, bioinformatics methods, and data management. For in-house developed assays and analysis pipelines, this breadth of knowledge is required to develop and validate a test. If commercial assay designs or analysis software are used, the laboratory must be able to critically evaluate the data produced.
Many laboratories utilize additional staff to assist in curation of literature and other evidence used in variant assessment before the data are reviewed by the laboratory director or designee. These individuals often have postgraduate education (e.g., PhD, master’s degree in genetic counseling or a related field) and/or additional training in gene–disease association and variant interpretation. Ongoing competency assessment of technical and interpretive staff is recommended. The laboratory director is ultimately responsible for the technical evaluation of the data and the professional interpretation of the variants in the context of the subject’s phenotype.
D.2. Analyzing and optimizing data before validation
Once the scope and method of testing have been chosen, iterative cycles of performance optimization typically follow until all assay conditions as well as data analysis settings are optimized. Differences in specimens, platforms, and pipelines can produce variability in the resulting data. During optimization the laboratory must first determine the parameters and minimum thresholds for coverage, base quality, and other test quality metrics that define an acceptable quality sequencing run for each sample type through a systematic evaluation of the NGS assay. This may include analyses at intermediate points during the sequencing run as well as at the completion of the run (e.g., real-time error rate, % of target captured, % of reads aligned, fraction of duplicate reads, average coverage depth, range of insert size). In this phase, the laboratory should track these data over a series of runs that include well-established reference samples with or without synthetic variants. This information is used to establish minimum depth of coverage thresholds for variant calling as well as allelic fraction, as they influence analytical sensitivity and specificity. If pooling of samples is planned, the laboratory should also determine the number of samples that can be pooled per sequencing run to achieve these thresholds. Inability or failure to achieve the quality thresholds and other nontechnical design expectations (e.g., baseline costs, turnaround time projections) of an assay should prompt the laboratory to determine if usage of supplemental procedures or a different assay is required. Before proceeding to test validation, a validation plan and standard operating procedure(s) for the entire workflow should be established.
D.2.1. Specimen requirements
NGS may be performed on any specimen that yields DNA (e.g., peripheral blood, saliva, fresh or frozen tissues, cultured cells, formalin-fixed paraffin-embedded [FFPE] tissues, prenatal specimens). However, performance may vary by sample type (e.g., saliva-derived DNA performs more poorly on GS compared with capture-based NGS due to contaminating bacterial DNA; FFPE samples perform poorly on long-read sequencing methods). The laboratory needs to establish the types of specimens and the minimum amount of input DNA required for the particular NGS assay and platform that will be used. The quality of DNA and variant detection requirements will likely differ by specimen type and as such, the laboratory will need to determine acceptable parameters for each type (e.g., volume, amount of tissue, collection device).
Previously extracted genomic DNA may be accepted for testing; however, the original source of the DNA (e.g., blood, saliva) should be determined given the potential differential impact on testing as described above.
D.2.2. DNA requirements and processing
The laboratory should establish the minimum DNA requirements to perform the test. Considerations include how much DNA may be required for confirmatory and follow-up procedures. The laboratory should have written protocols for DNA extraction and quantification (e.g., fluorometry, spectrophotometry) to obtain adequate quality, quantity, and concentration of DNA. In general, the lower limit of detection (LLoD, the lowest amount of DNA acceptable for a test) is calculated as the lowest quantity of an analyte that will generate at least 95% of the positive calls among all true positives.46,66 To identify an initial LLoD as well as an upper LoD (ULoD) that yield data within the established quality metrics, serial dilutions of varying DNA input from multiple specimen types can be assessed.
In addition, the lab must determine the LLoD and ULoD for each anticipated variant type including specimens with mixed content (e.g., mosaicism, chimerism, mitochondrial heteroplasmy). Cell line mixing studies of two well-characterized reference samples (i.e., mixing two pure DNA samples at varying percentages) can aid in these initial evaluations.66 At a minimum, the final LLoD for input in combination with mixed content should be represented by samples in the analytic validation to ensure that quality metrics and performance parameters are maintained across the final assay specifications.
D.2.3. Coverage
Generally, variant calls are more reliable as the depth of coverage from high-quality sequence reads increases for a given position. Low depth of coverage increases the risk of missing variants (false negatives) and increases the risk of assigning incorrect allelic states (zygosity), especially in the presence of amplification bias. Low coverage decreases the ability to effectively filter out sequencing artifacts leading to false positives. Laboratories should establish a minimum depth of coverage necessary to call variants and report analytical performance related to the minimum threshold that is guaranteed for the defined targeted genes or regions.
To call germline heterozygous variants, a minimum base-calling quality of Q ≥ 20 and a minimum depth of 10× for all nucleotides in the targeted region have been suggested;67 https://www.wadsworth.org/regulatory/clep/clinical-labs/obtain-permit/test-approval; however, a 10× depth of coverage may not be sufficient for all variants in all regions. Data suggest that a test intended to detect genetic diseases characterized by a high rate of mosaicism requires 30–50× depth of coverage to detect mosaicism at a level of 10–15%.68 Further increased depth will increase confidence in the call.69,70 Detection of mitochondrial heteroplasmy will also require significantly increased coverage depth to ensure detection of variants down to ~5% allele fraction.71
The average depth of coverage is a readily obtainable surrogate for overall assay performance. For example, to ensure that at least 95% of bases reach at least 10× coverage, an assay may require a minimum mean depth of coverage of 75–100× for ES or 30× for GS. Note that the desired coverage of the region to be sequenced will impact the number of samples that can be pooled in a sequencing run. It is also important to note that minimum coverage is highly dependent on many aspects of the platform and assay including base call error rates, quality parameters such as how many reads are independent versus duplicate, and other factors such as analytical pipeline performance.72 Therefore, it is not possible to recommend a specific minimum threshold for overall coverage. Laboratories will need to choose minimum coverage thresholds in accordance with quality metrics necessary for analytical validity. Estimating the required depth of coverage based on a laboratory’s specific performance parameters is discussed in Jennings et al.66
Other data quality metrics that are useful include the percentage of reads aligned to the genome, the percentage of reads that are unique (prior to removal of duplicates), the percentage of bases corresponding to targeted sequences, the uniformity of coverage, and the percentage of targeted bases with no coverage. Coverage limitations, such as regions of the genome that are difficult to sequence (section D.1.1.2), should be reported as a technical limitation of the test. Ancillary technologies may complement a final test offering to reduce the impact of these limitations on clinical sensitivity.
D.2.4. Allelic fraction and zygosity
Germline heterozygous variants are expected to be present in 50% of the reads; however, capture, amplification, or sequencing bias as well as coverage can lead to variability. Laboratories must determine allelic fraction ranges to distinguish true calls from false positive calls, which typically have a low allelic fraction; assign zygosity; and detect mosaicism or heteroplasmy. The laboratory should understand how zygosity is defined by the bioinformatics pipeline, how it is presented, and establish a range of allele fractions needed to make a final zygosity call based on empirical data. Allele fractions should be investigated by orthogonal methods to clarify ambiguous zygosity or potential mosaicism (section D.1.1.3). Coverage of homozygous calls should be reviewed to distinguish true homozygosity from potential hemizygosity due to deletion of the second allele. The performance of different types of variants should be analyzed separately as their performance may vary. For example, coverage and allelic fraction for indels can be lower when the alignment tool(s) discards indel-containing reads. Finally, laboratories should be aware of genes for which variation in blood may often be confined to blood-forming cells (e.g., TP53, ASXL3),73 even if appearing constitutional, and consider reporting any detected variation in healthy individuals with a warning of possible mosaicism or clonal hematopoiesis of indeterminate potential (CHIP).
D.2.5. Other factors impacting data quality
The lab must identify the factors that occur in clinical samples which will reduce the quality or quantity of the resulting sequence data. Different NGS library preparation approaches, sequencing chemistries, and platforms carry intrinsic error rates; however, systematic evaluations suggest these rates are extremely low for most (section D.1).74,75 In addition, interfering contaminants can reduce the amount of genomic sequence available for analysis, for example, reducing the number of reads that will map to the human reference genome. Methods to detect, reduce, and monitor these interfering substances and improve the analytical specificity of an assay have been studied previously.76,77,78 If significant interoperator variability is observed during initial optimization, the assay may not be ideal for clinical production.
D.3. Establishing quality control metrics and performance parameters before validation
The laboratory must develop quality control (QC) metrics based on established performance parameters during preliminary assay development to be applied to the validation as well as in production. QC metrics should be chosen to monitor sample and data integrity. Selected QC metrics should demonstrate that each assay meets the required coverage depth and quality for the targeted regions (i.e., genome, exome or panel) and variant types identified in the test design.
Examples of metrics used to monitor sample and data integrity:
-
Sample preparation failures
-
Sequencing run failures
-
Cross contamination
-
Cluster cross-talk
-
Sample identity including familial relationships, if applicable
Examples of metrics used to monitor sample and data integrity per sample and over time:
-
Total data yield (gigabases)
-
Raw cluster density
-
Mean coverage
-
Median coverage
-
Percent (%) bases ≥Q30 (Phred-scale)
-
Percent (%) aligned bases (reference/target dependent)
-
Percent (%) duplicate paired reads
-
Target coverage at varying depths (10×, 20×, etc.)
-
SNV Het/Hom/Hemi/unknown zygosity ratio
-
SNV transition/transversion ratio
-
Deviations in expected allele fraction
Laboratories should choose, develop, and validate metrics to monitor performance as appropriate for their assays. If necessary, metrics for each sample can also be individually assessed using case-level metrics (sections D.2.3–D.2.5) with respect to the specific test ordered by the provider.
Overall, the laboratory must document that the NGS assay can correctly identify known variants of multiple types. To extrapolate the ability of an assay to detect novel variants, it is necessary to compare internal data to known truth sets representing different variant types within the targeted regions. Maximizing the number of variants of different types in the targeted regions can establish the confidence and reliability of the assay. It has been suggested that 59 variants of each type (e.g., substitutions, indels, CNVs) be evaluated to confirm that regions covered by the assay can be analyzed with 95% confidence and 95% reliability (section D.4.1).66,79 Detection of variants can be influenced by local sequence context and therefore a uniformly high sensitivity will not be possible for every possible variant. Nevertheless, the greater the number of variants tested and the larger and more diverse the genomic loci included in this cumulative analysis, the higher the confidence that the assay is detecting variants accurately.80 Variants included in this type of analysis do not need to be pathogenic as this has no bearing on their detectability. However, it could be argued that the absence of large numbers of established pathogenic variants in test development and validation may result in an unanticipated shortcoming of the assay.
There are limitations to using truth sets as they contain the most easily assessed variants and may contain false positive variants. The definition of a truth set may also be influenced by cross-platform ascertainment bias or other technical limitations in variant detection (e.g., some regions may have no or low sequence coverage in one NGS assay design versus another).81 It is important to track and investigate discrepancies where there is absent, conflicting, or ambiguous data between the assay under development and the truth set to accurately define the limitations of the assay.
The following performance parameters should be assessed and met during the optimization phase and formally documented during validation: (1) accuracy, (2) precision/reproducibility/robustness, (3) analytical specificity, (4) analytical sensitivity, (5) limit of detection, and (6) clinical sensitivity for each type of variant that the laboratory plans to report. These performance metrics should be completed for the entire assay as a whole, as well as each reported variant type and potentially size, when appropriate (e.g., SNVs, CNVs, insertions and deletions). While parameters may be calculated at the NGS technology level initially, the final reported parameters should be relevant to the full test if multiple technologies are utilized. For example, tests may include both NGS and ancillary technologies, including steps to confirm variants and/or Sanger fill-in for missing data. Some regulatory agencies may require additional validation components.
D.3.1. Accuracy
The accuracy of detection for the different variant types, including different size events within a variant type, should be measured by calculating the positive and negative predictive values based on a given truth set, with confidence intervals included. For example, >99% should be expected for SNVs; however, a range of >95–98% has been used by some laboratories for all variant types. For variant types for which there is no truth set data (e.g., Genome in a Bottle)48,81 then FDA recommendations for accuracy should be followed.46
D.3.2. Precision/reproducibility/robustness
The laboratory should document the assay’s precision (repeatability and reproducibility) based upon truth sets. For example, the laboratory should run a single library or sample preparation on 2–3 lanes or wells within the same run (repeatability, within-run variability) as well as 2–3 different runs (reproducibility, between-run variability). Other meaningful measures of reproducibility are instrument-to-instrument variability (running samples on 2–3 different instruments if available) and interoperator variability. Complete concordance of results is unlikely for NGS technologies; however, the laboratory should establish parameters for sufficient repeatability and reproducibility. Depending on the complexity of the assay, some number of differences in calls is expected; however, all differences in calls between runs should be investigated and explained as part of the validation.
An assay’s robustness (likelihood of assay success) should be monitored and have adequate QC measures in place to assess success at critical points such as library preparation and immediately following sequencing (section G).
D.3.3. Analytical specificity and sensitivity
In the genomic area, analytical specificity is the proportion of variants correctly identified as the same variant compared with the reference in a particular sample. During the validation, truth sets should be analyzed to determine the analytic specificity of the assay. The FP rate can be calculated as 1 – specificity. If variant calls are confirmed by an ancillary method, the technology-specific FP rate is less critical unless it generates a significant amount of confirmatory testing per sample that is not sustainable for the laboratory. In general, the specificity of the assay should at a minimum be >98%.
Analytical sensitivity is the proportion of variants correctly identified as different from the reference sequence in a particular sample. The false negative rate can be calculated as 1 – sensitivity. In general, the sensitivity of the assay should at a minimum be >98%.
D.3.4. Minimum input DNA requirement and limit of detection of the test
LoD and LLoD were discussed in section D.2.2. When possible, the use of samples with known allelic imbalances that are confirmed by orthogonal methods should be assessed to provide validation of the LoD. Note that some licensing entities including CAP require patient sample inclusion in LoD validation (CAP MOL.36118). The LLoD value is used to help set limits for the detection of mosaicism, chimerism, or mixed specimens as well as thresholds for sample admixture or cross-talk associated with automated pipetting instruments and sample indexing.
D.3.5. Clinical sensitivity/specificity
For disease-specific targeted panels, the lab should establish the estimated clinical sensitivity of the test based upon a combination of analytical performance parameters and the known contribution of the targeted set of genes and types of variants detectable for that disease. Clinical specificity can be maximized by limiting or excluding genes with limited or disputed evidence related to the phenotype, thereby minimizing detection of VUS. For ES/GS of individuals with undiagnosed (and possibly nongenetic) disorders, it is not feasible to calculate a theoretical clinical sensitivity or specificity for the test given its dependency on the applications and indications for testing.19,20,82,83
D.4. Test validation
Once test content, assay conditions, and pipeline configurations have been established as outlined in D.2 and D.3, a validation plan should be prepared and executed from start to finish on all permissible sample types. Assay performance characteristics including analytical sensitivity and specificity, accuracy, and precision should meet thresholds predetermined in the validation plan (section D.3).66,80,84
D.4.1. Sample consideration for validation
Performance data across tests using the same platform can be combined to establish a cumulative “platform” performance. By maximizing the number and types of variants tested across a broad range of genomic regions across all acceptable specimen types, confidence intervals can be established. Because the size of NGS tests make validation of every base impossible, this approach enables extrapolation of performance parameters to novel variant discovery within the boundaries of the established regions.
For example, when using standard short-read technologies that produce ~150 bp reads, the common types of variants required to be evaluated can be grouped relative to the methodology used for variant calling. Although there will be overlap, typically an “indel” would be an event within the targeted capture probe and sequencing read length, whereas a “CNV” would be an event that spans more than a single capture probe and exceeds the sequencing read length. Detection of larger indels or CNVs is highly dependent on sequence context with deletions typically being easier to detect than duplications. Since performance of specific events cannot be predicted, testing a variety of events (e.g., type, size, position in captured region) across different genes or regions of interest is important. Alternatively, long-read technologies may allow for larger indel events (>100 bp) to be detected by variant calling methods and validation samples would need to reflect this.
If the spectrum of genomic variation related to a specific disease includes types of variation outside those covered by NGS testing, then ancillary methods should be employed to capture these. Issues related to accurate sequencing of highly homologous regions should be addressed when one or more genes within the test have known pseudogenes or other homologous loci. If high clinical sensitivity is based on the ascertainment of particular common pathogenic variants, these should be included in the validation. Alternatively the test report can note a limitation if ancillary methods are not used.
The first test developed by a laboratory generally requires a more comprehensive validation than subsequent tests developed on the same platform using the same basic bioinformatics pipeline design. In practice this may entail sequencing a larger number of samples in order to test a sufficient number of each variant type (section D.3). Note that current “truth” sets of a few samples (e.g., Genome in a Bottle samples)48,81 often encompass most of these variant types across the genome and are recommended to be included. Importantly, they are a renewable resource that can aid in monitoring test performance over time and after modifications (section D.1.2). Additionally, specific licensing entities may require a minimum number of samples for validation. For example, NYS guidelines require that initial NGS validations for a laboratory include at least 25 samples (NYS NGS20). In an effort to ensure regulatory compliance, CAP and AMP have created spreadsheet resources to guide laboratories through the test validation process3 (https://www.cap.org/member-resources/precision-medicine/next-generation-sequencing-ngs-worksheets).
D.4.2. Bioinformatics
The bioinformatic pipeline must produce the expected results, starting from the data produced by the sequencing equipment. The laboratory should establish the reproducibility of a chosen analytic pipeline, such that a given standard input should produce the same output each time it is run. Additional limitations of the pipeline, such as lack of precision in repetitive regions, may be identified during validation and should be discussed in the validation summary.
D.4.3. Evaluation of quality metrics
QC metrics established in the prevalidation stage for each assay (see section D.3) should be monitored throughout the validation. Deviations from expected values should be investigated to determine whether procedural changes should be implemented during the test validation phase. These deviations should be discussed in the validation summary.
D.4.4. Transfer to production
Final assessment of all established performance parameters must be summarized to support the transfer of a clinical test into production. Any deviations or additional limitations to the test’s performance identified during the validation should be described in the validation summary and reflected in the final approved version of the test. If a test fails multiple performance parameters, reoptimization and subsequent validation studies may be necessary. Once a test is validated for production, it is recommended that 2–3 test samples be initiated through the production workflow to identify any unanticipated issues.
D.5. Validating modified components of a test or platform
D.5.1. Version control
Improvements and adjustments to a test are expected over time, but must be validated and documented through version control. The version control system should record the dates and times that changes are implemented in order to accurately track clinical test performance. Versions of the test and/or its components should be represented in the methods section of the clinical report (section E.4.2).
D.5.2. Modified assay conditions, reagents, instruments, and analytical pipelines
Changes in reagents, hardware, and software that can alter the accuracy of the final test result (e.g., new sequencing chemistry, new instruments, new lots of capture reagents, new software versions) must be validated before they are put into production. The process may require an end-to-end test validation with previously analyzed specimens or well-characterized controls. Ideally, the same, renewable, well-characterized samples (e.g., a HapMap sample, Genome in a Bottle NIST sample) should be used. Determination of the analytical performance and other parameters, such as coverage, should be carried out as outlined in the prior sections. New reagent lots and shipments should be compared with previous reagent lots or with suitable reference material before, or concurrent with, their use in production. Software changes may use the laboratory’s existing data for validation obviating the need for an end-to-end validation.
While data storage is expensive, additional or nonstandard analysis of historic data is recommended to identify the strengths and weaknesses of the analytical pipelines over time and can aid in future test development. Note that any alterations or improvements of the pipeline should prompt revalidation; however, the extent of the validation can be commensurate with the complexity or magnitude of the changes. For example, changes in alignment and base calling would warrant a more extensive validation than updates to versions of downloaded databases.
D.5.3. Added/modified test content
When modifying the content of a validated test, an abbreviated end-to-end or in silico validation (3–10 samples) may be sufficient. Such modifications include adding the analysis of genes in a gene panel test using a previously validated capture library, platform, and pipeline design; employing a new capture library using a validated platform and pipeline design; and updating the equipment or assay (e.g., reagents, bioinformatics, or software updates) in a previously validated panel. Separate validation documentation should be generated and the date of implementation into production must be documented. Gene content of panels should be examined every 6 months to determine whether new data suggest the addition of new genes or the removal of others4 (section A.2.1).
D.6. Considerations for a distributive testing model
Some components of a laboratory test may be performed by an outside entity (e.g., sequencing is performed by one laboratory, but the analysis and reporting are performed by a different laboratory). Laboratories should ensure that the outside entity has similar accreditation (CAP/CLIA) and licensure, uses aligned validation and quality metrics, and provides a mechanism through which to report procedural and quality deviations. Per CAP guidance, the validation of any test using this model should include an integrated validation including wet bench and bioinformatics. Any distributive testing should be addressed in the laboratory’s quality management (QM) plan, and should include the types of data to be transferred as well as a system for monitoring trends in the data.
E. REPORTING STANDARDS
E.1. Turnaround times
The laboratory should have written standards for NGS test prioritization and turnaround times (TATs) that are transparent and readily accessible. These TATs should be clinically appropriate and allow for rapid testing when warranted. Laboratories should also have a notification plan in place to alert the ordering providers when a result is expected to be significantly delayed.
E.2. Data filtering and interpretation
E.2.1. Variant filtering
In traditional disease-targeted testing, the number of identified variants is typically small enough to allow for the individual assessment of all variants in each sample, once common benign variants are curated. However, ES identifies tens of thousands of variants and GS identifies several million, making this approach to variant assessment impossible. A filtering approach must be applied for ES/GS studies. Laboratories may need to employ autoclassification strategies for very large disease-targeted panels. Laboratories must also balance overfiltering that could inadvertently exclude causative variants with underfiltering that presents too many variants for expert analysis. A stepwise approach is generally necessary. For example, an initial filter-step identifies benign variants and those that are obviously disease-causing followed by other filtering driven by phenotypic associations and inheritance patterns. Regardless of the approach, laboratories should describe their methods of variant filtering and assessment, including the limitations of each method.
The filtering algorithm design may differ across case types, and requires a high level of expertise in genetics and disease diagnosis. This expertise should include a full understanding of the limitations of the databases against which the individuals’ results are being filtered as mentioned previously and the limitations of both the sequencing platform and multiple software applications being used to generate the variants analyzed. Individuals leading these analyses should have extensive experience in the evaluation of sequence variation and evidence for disease causation, as well as an understanding of the molecular and bioinformatics pitfalls that are encountered.
E.2.1.1. Known and benign variant filtering
Sources of broad population frequencies that can be used for autoclassification of benign variation include dbSNP (www.ncbi.nlm.nih.gov/projects/SNP), the National Heart, Lung, and Blood Institute (NHLBI) Exome Sequencing Project (ESP, evs.gs.washington.edu/EVS), the 1000 Genomes Project (1000 K, www.1000genomes.org), and the Genome Aggregation Database (gnomAD, http://gnomad.broadinstitute.org/). To account for statistical variance in the gnomAD populations due to the control sample size, precomputed frequency estimates designated as a filtering allele frequency (FAF) have been made available. FAFs represent a statistical estimate of a variant’s allele frequency in a given population at either a 95% or 99% confidence interval.85 The laboratory can utilize allele frequencies to determine if a variant’s presence in these populations exceeds the maximum credible disease allele frequency. Determining the maximum credible disease allele frequency requires extensive knowledge of all related disease prevalence, inheritance patterns, pathogenic variant (i.e., allelic) heterogeneity, and other factors for a given gene. Moreover, frequency thresholds should be assessed conservatively to account for the possibility of undocumented reduced penetrance at the gene or variant level, and the possible inclusion of individuals who have not been phenotyped, who have asymptomatic or undiagnosed disease, or who have a known disease. Examples assessing these frequency cutoffs, which can enable rapid autoclassification of benign variants, have been published.86,87
Variants previously associated with disease either in general variant databases such as ClinVar, publications, or locus-specific databases are generally flagged for further assessment regardless of population frequencies. The DECIPHER database (https://decipher.sanger.ac.uk/browser) can provide a general overview of a gene, with graphical representation of protein domains and the distribution of reported population and disease-associated variants. While several expert curated databases exist (e.g., ENIGMA, INSiGHT, CFTR2), laboratories should not assume that they have correctly assessed pathogenicity as few are curated to a clinical grade with strict evidence-based consensus assessment of supporting data.88 The FDA has recognized the ClinGen human variant data set through their Human Variant Database program (https://www.fda.gov/news-events/press-announcements/fda-takes-new-action-advance-development-reliable-and-beneficial-genetic-tests-can-improve-patient). This recognition signifies that the ClinGen variant data set (inclusive of the curated evidence and assertions of pathogenicity) is recognized as a scientifically valid evidence source. As such, the data and assertions can be utilized by test developers to support the clinical validity of their tests. Note that the intent of the FDA’s human variant database program is to support test development. However, laboratories are expected to independently assess the pathogenicity of every reported variant, and not rely solely on external databases and other resources, especially given the ongoing evolution of variant knowledge. Users can access the ClinGen variant data set via ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) and can access the evidence supporting those assertions via the ClinGen Evidence Repository (https://erepo.clinicalgenome.org/evrepo/).
E.2.1.2. Additional patient-centric filtering of ES/GS data
The ordering health-care provider must provide detailed phenotypic information to assist the laboratory in the analysis and interpretation of test results. This step is most important for panels that include a large number of genes as well as ES/GS. The interpretation and prioritization of variants by the laboratory may be enhanced by an iterative process with health-care providers to reassess the individual for specific clinical features of potential diagnoses suggested by the sequence data. Conversely, as laboratorians consider the phenotype while prioritizing variants, health-care providers should interact with the lab if the ES/GS is nondiagnostic. A discussion of the individual’s phenotype may guide the reporting of variants with questionable phenotypic fit.89 This is especially relevant in young children who may not manifest all the diagnostic features of a syndrome. For a detailed discussion of this topic, please review the ACMG statement regarding the dissemination of phenotypes in the context of clinical genetic and genomic testing.16
To accurately employ phenotypic-centric filtering, laboratories should maintain and regularly update lists of genes with associated levels of evidence (https://www.clinicalgenome.org/) connecting them to discrete phenotypes and/or conditions using a structured ontology (e.g., Human Phenotype ontology, OMIM disease ID, MedGen). These lists should be examined at least every 6 months.4 Storage of patient phenotypes with structured ontology is also recommended to promote more rapid analysis of data using phenotype-centric filtering. In addition, utilizing external collaborative resources such as Matchmaker Exchange (www.matchmakerexchange.org) can help identify and refine disease–condition relationships.90
When reviewing genes with more poorly defined disease–condition relationships, the laboratory must apply additional strategies for variant filtering. While it is generally assumed that causative variants for Mendelian disorders will be rare and highly penetrant,91 the range of penetrance and expressivity continues to expand. Successfully identifying the molecular basis for a rare disorder may depend on the indication for testing and alternative analysis strategies, such as choosing appropriate family members for comparison given a suspected mode of inheritance. The ultimate goal is to reduce the number of variants related to the clinical phenotype needing examination by a skilled analyst. Variants may be included or excluded based on factors including presence in a phenotype-associated gene list, presumed inheritance pattern in the family (e.g., biallelic if recessive or hemizygous if X-linked), variant types (e.g., truncating, copy number), presence or absence in control populations, observation of de novo occurrence (if the phenotype is sporadic in the context of a dominant disorder), rare homozygous variants, gene expression pattern, algorithmic scores for in silico assessment of protein function or splicing impact, and biological pathway analysis.
E.2.2. Variant classification
Classification of medically relevant sequence variants is not a fully automated process and requires specialized training in evaluating gene–disease association and variant evidence (section D.1.4). Potential clinically relevant variants should be evaluated and classified according to best practices as outlined in the ACMG/AMP guidelines.92 Additional general guidance documents developed by ClinGen (https://clinicalgenome.org/working-groups/sequence-variant-interpretation/) and gene- and disease-specific specifications may be applied to refine variant classifications and reduce discrepant classifications among laboratories (https://clinicalgenome.org/docs/?doc-type=publications#list_documentation_table). Variant evaluation should include an evidence-based assessment of the pathogenicity of the variant as well as its potential role in the individual’s phenotype. The evidence for clinical validity of the particular gene in the patient’s disease, as documented by resources such as OMIM (https://www.omim.org/) and ClinGen (https://clinicalgenome.org/curation-activities/gene-disease-validity/), should also be considered when weighing potential clinical significance. For tests that cover a broad range of phenotypes (e.g., cardiomyopathy or intellectual disability), as well as ES/GS, correlation between phenotypes known to be associated with the variant and the individual’s phenotype should be assessed. If multiple variants of potential clinical significance are identified, the interpretation should discuss the likely relevance of each variant to the phenotype, including the possibility of concurrent diagnoses, resulting in a potential blended phenotype, and prioritize variants accordingly. Individualized clinical interpretation of laboratory findings goes beyond the standard technical analysis of results and classification of analytical findings. Development of an individualized clinical interpretation may require communication with the ordering health-care provider to obtain and review relevant medical and/or family history information.
Laboratories should deposit interpreted variants with supporting evidence and the criteria applied for assessment into the ClinVar database (http://www.ncbi.nlm.nih.gov/clinvar). The public deposition of this information enables the identification of interpretation differences and ability to rapidly share and build knowledge that can improve diagnosis and care.93,94,95,96,97 Laboratories should have policies consistent with emerging professional guidance for the reporting of variants in genes with limited or no known disease association that aligns with the intended use of the test (e.g., a diagnostic gene panel versus4,93 ES/GS) (https://clinicalgenome.org/docs/?doc-type=curation-activity-procedures&curation-procedure=gene-disease-validity).
E.3. Reporting of secondary or unanticipated findings
ES/GS tests may generate sequence information that is not immediately associated with the individual’s phenotype and family history as provided. The terms “incidental” or “secondary” findings, depending on the intent to identify, are used to describe these unexpected clinically significant variants. Reporting recommendations have been published.98,99,100 While laboratories are not limited to the genes recommended by ACMG, deviations from this gene list should be disclosed. Laboratories should carefully consider which variants to report as secondary findings.101,102 Guidance documents suggesting how laboratories should proceed after detection of unanticipated findings such as consanguinity and misattributed parentage have also been published.103,104
E.4. Written report
Creating reports for audiences of different backgrounds is challenging. A report for a health practitioner may be different from the report for a lay audience.105 All laboratory reports should adhere to federal (42 CFR § 493.1291), state, and regulatory (CAP, CLIA) standards. Primary findings in a diagnostic test should appear as a succinct interpretive result at the beginning of the report indicating the presence or absence of variants consistent with the phenotype. Laboratories may choose to use statements like “positive,” “abnormal,” or “clinically important finding” to describe detection of a variant that explains the clinical findings (primary findings), or a medically actionable variant. “Negative” would indicate that no variants were identified that are relevant to the phenotype. “Uncertain” or “see report” would signal that there is uncertainty regarding the connection between the phenotype and the variant(s) reported. Variants should be prioritized according to their relevance to the phenotype. When reporting a gene associated with a treatable genetic disorder the laboratory should consider the addition of a reference to the treatment in the report.106 This is currently recommended in cancer testing reports.107 Any additional findings (e.g., secondary findings, carrier status, pharmacogenomics variants) may be included in separate sections as appropriate. If other family members are tested to assist with the interpretation of the variants found in the proband (e.g., trio analysis), only the minimum amount of information required to interpret the variants and comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations should be provided in the proband’s report. Specific names and detailed phenotypic descriptions should be avoided. As an example, the following statements would be appropriate: “Parental studies demonstrate that the variants are on separate copies of the gene, with one inherited from each parent” or “Segregation studies showed consistent inheritance of the variant with the disease in three additional affected family members.” Sample reports are included in the Supplemental Material as examples of some ways to provide the content recommended above. The details in these reports are provided as examples only. All report details are ultimately left to the discretion of the laboratory director.
E.4.1. Variant reporting
All reports must include a list of clinically significant variants identified, annotated according to Human Genome Variation Society nomenclature (varnomen.hgvs.org) and classified according to ACMG/AMP guidelines.92 Aspects of HGVS nomenclature may be difficult to incorporate into a clinical report in a way that is meaningful to a health-care provider. In the interest of clarity, abbreviated nomenclature with additional information provided in a methods or reference section of the report may be most appropriate. Gene names should adhere to the approved HUGO Gene Nomenclature Committee (HGNC) nomenclature (www.genenames.org). The following elements should be included for each variant within a gene: genomic coordinate with genome build, gene name, reference transcript, zygosity, complementary DNA (cDNA) nomenclature, nucleotide change, nomenclature for the predicted or known protein impact when appropriate, and variant classification or clinical assertion as noted above. The choice of transcript is at the discretion of the laboratory director as there are currently no established guidelines. The following elements should be included for each variant outside of the coding regions: genomic coordinates (with genome build such as GRCh37 or more complex alternate contig such as GRCh37.p13 chr 6 alt locus HSCHR6_MHC_APD_CTG1), nucleotide change, zygosity, and variant classification or clinical assertion as noted above. Other aspects of variant reporting are under development (https://loinc.org/53037-8/, http://reg.clinicalgenome.org/redmine/projects/registry/genboree_registry/landing, Matched Annotation from the National Center for Biotechnology Information [NCBI] and European Bioinformatics Institute [EMBL-EBI] [MANE], http://www.hl7.org/fhir/uv/genomics-reporting/history.cfml).
Laboratories should document the supporting evidence used to classify variants with respect to their known or potential role in disease. There are increasing examples of variants for which understanding of pathogenicity may differ depending on a specific disease association (e.g., GBA variants in the context of Gaucher disease vs. Parkinson disease).108,109 The laboratory should connect each reported variant with the indication for testing in the interpretative report. For variants that potentially explain the patient’s phenotype, the name of the disorder or phenotype should be included using a standardized nosology such as OMIM, MONDO, or ICD10. Additional information regarding a variant unrelated to the primary clinical indication may be included in the report. Laboratories should have a clear policy describing which variants are excluded from the report. For example, it is typical for laboratories to report only pathogenic variants and likely pathogenic variants for carrier or risk assessment tests in healthy individuals, yet include VUS when they are in genes with an established or plausible role in the patient’s phenotype or family history.110 This policy should be detailed in the material supplied to ordering providers and in the individual’s report. Providers may request that specific gene(s) be evaluated in a gene panel or ES/GS testing. Unreported benign variants, likely benign variants, and additional VUS should be available upon provider or patient request.
E.4.2. Methods reporting
Reports should include a summary of the validated methodology and all limitations of the test (section D.3) including appropriate versioning of databases and informatics pipelines. For disease-targeted gene panels, at a minimum, the report should include the genes analyzed, key coverage metrics, and a list of the analyzed genes without full coverage. Actual coverage should be reported when full coverage is not obtained. The laboratory should also report any limitations in analysis of specific genes or variant types (such as CNVs) if the method of analysis does not include all genes or variant types related to the indication for testing. If not included in the NGS test, comprehensive intragenic deletion and duplication analysis via an ancillary methodology is recommended.
For ES/GS testing, a description of the process of data analysis should be provided in the report. The sample-specific average and/or minimum coverage depth of the exome or genome should be provided. Laboratories should make available average and/or minimum depth of coverage statistics across their testing cohort. For GS, in addition to genome coverage, a separate coverage value for the exome should be available upon request with the laboratory’s definition of exome content. In addition, if the laboratory is explicitly asked to perform an analysis of a particular gene, the gene coverage as well as any additional limitations related to the analytical detection of variants in that gene should be reported. The laboratory may analyze variants in genes with limited or no known disease association, candidate genes, or so-called genes of uncertain significance (GUSs). If the laboratory chooses to report a variant in a GUS (e.g., a de novo variant in a constrained gene without a reported disease association), then the lack of disease association should be noted and it should be reported as a VUS in a section separate from the primary findings. A variant in a GUS should never be classified as pathogenic or likely pathogenic.4,92
E.5. Data release for patient request
To comply with the US Department of Health and Human Services rule 45CFR § 164.524 (https://www.govinfo.gov/app/details/CFR-2018-title45-vol1/CFR-2018-title45-vol1-sec164–524/summary), clinical laboratories (HIPAA covered entities) must provide completed test reports to individuals upon request.111 Additional guidance has specified the extent of data release to include “the full gene variant information generated by the test” including the raw sequencing data (https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html#newlyreleasedfaqs). Laboratories should have a disclosure policy that defines the data elements provided, noting that the variant data will likely include benign variants, previously unreported rare variants, false positive variants, and other potential secondary/incidental findings. The rule does not require laboratories to provide interpretation for the variant data or explanations in language appropriate for a lay person. Laboratories have discretion to set appropriate fees to cover the labor and material costs to supply this information.
E.6. Variant reclassification and data reanalysis
With the rapidly evolving variant knowledge base, high rates of variant reclassification have been reported.112,113,114 Therefore, it is recommended that laboratories offer reanalysis of data from previously reported genetic tests generated in their laboratory. Reanalysis policies should include a description of variant-level reclassification and case-level reanalysis procedures, whether additional charges will apply, as well as a statement about reanalysis in their test description statements and individual reports. Laboratories should suggest periodic inquiry by health-care providers to determine whether knowledge regarding a previously reported variant has changed resulting in reclassification, such as a VUS reclassified as pathogenic. If the laboratory initiates variant reclassification, the laboratory should develop approaches to ensure timely communication of these updates (e.g., through amended reports, especially for significant changes such as a pathogenic variant downgraded to VUS, and submission to ClinVar or direct database access). In turn, the ordering provider should make reasonable efforts to recontact the individual if the change is felt to be medically relevant for the individual or family.115 A document detailing the points to consider when laboratories are establishing these policies has previously been published.112
For reanalysis to be performed, the current bioinformatics pipeline must be validated to accommodate any differences in the data structure since the original analysis (e.g., capture library, sequencer). Given technology improvements, resequencing may be superior to reanalysis of old data and should be considered when data were generated on outdated platforms with reduced accuracy.
F. DATA STORAGE, SECURITY, AND TRACEABILITY OF REPORTS
NGS generates a massive amount of data. Laboratories must ensure that data storage is HIPAA compliant and allows traceability of data whether using on-site storage or cloud storage. Due to the multistep nature of NGS informatics, intermediate files with differing content and sizes will be generated. Laboratories may employ widely heterogeneous sequence alignment and variant calling algorithms; thus, the types of files generated in the process of NGS differ between laboratories. Laboratory policy should explicitly indicate which file types are retained and what length of time each type will be retained. Policies for retention of records and materials must comply with national, federal, state, and local laws and regulations. Regulations and laws related to testing minors (under the age of 21) may differ from adults. CLIA regulations (section 493.1105) require storage of analytic systems records and test reports for at least 2 years. We recommend that the laboratory consider a minimum of 2-year storage of a primary file type (e.g., BAM or FASTQ files with all reads retained). This permits reanalysis with improved analytic pipelines. In addition, laboratories should consider retention of the VCF and final test report for 5 years, given the likelihood of a future request for reanalysis. Storage for longer periods of time is acceptable. International requirements for both storage and destruction may be at odds with state and US federal regulations. Laboratories should maintain an internal database of variants analyzed and classified using the ACMG/AMP standards.92
G. ONGOING QUALITY MANAGEMENT (QUALITY ASSURANCE/QUALITY CONTROL)
Monitoring preanalytical, analytical, and postanalytical variables should be part of the laboratory’s quality assurance and quality improvement programs. Such variables may include quality of the specimen received, number of NGS run failures, TAT, detection rate/positive rate, customer satisfaction, variant detection parameters, etc. A QM program must be in place in accordance with all applicable regulatory agencies. This program is expected to support the routine analysis, interpretation, and reporting of NGS cases including periodic assessment of data trends. Laboratories should monitor and assess deviations from predetermined QC metrics (section D.3) for every sample and run. Bioinformatic pipeline version, instrument, and reagent lots should be documented for each test and correlated with any deviations in quality. Laboratories are expected to document any deviation from the standard procedures established during the validation process. Regular meetings of a quality management team can facilitate these tasks.
G.1. Control samples
Similar to Sanger-based sequencing, positive controls do not need to be tested concurrently with each clinical test.116 Methods to evaluate and control for possible contamination at various points in the procedure are critical, including the use of no template controls during enrichment or library preparation. This type of control does not need to be carried through to final sequencing. Periodic reassessment of a well-characterized control used in validation, such as NA12878, is also recommended to look for drift in sensitivity and specificity. Alternatively, a lab may run a low level of a control such as a synthetic DNA standard mixed with each sample.117
G.2. Within-run QC
Generally, QC stops should be established prior to the sequencing run, within the sequencing run itself, and at the end of the run prior to executing data analysis. Examples of QC stops include determining the success of initial DNA fragmentation (incompletely sheared genomic DNA will result in suboptimal data), monitoring error rates during the sequencing run (enabling abortion of the run if necessary), and preanalysis assessment of the read quality (e.g., percent of bases above a predetermined quality threshold, QC alignments) (monitoring errors in sequencing: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5026502/; https://www.omicsonline.org/open-access/computational-errors-and-biases-in-short-read-next-generationsequencing-jpb-1000420.php?aid=85469).
G.3. Sample integrity assurance
Given the complexity of the procedures and likelihood of manual steps, procedures should be developed to prevent sample switches and cross-talk when multiplexing is employed (https://www.wadsworth.org/regulatory/clep/clinical-labs/obtain-permit/test-approval). Orthogonal confirmatory testing may require additional sample preparation and storage considerations such as separate extractions from the primary blood sample. Laboratories may use a variety of techniques to ensure the integrity of sample identity including Sanger confirmations, familial (trio) analysis, short tandem repeat (STR) analysis, single-nucleotide polymorphism (SNP) arrays, or the inclusion of tracers. Monitoring SNV allele ratios for an excess of ambiguous zygosity calls could reveal an issue with sample integrity.
G.4. Suboptimal samples/data
Ideally, suboptimal samples should be rejected, and new samples requested. In the absence of a new sample, the referring provider should be consulted to determine which testing option would result in the highest clinical sensitivity. Similarly, if the data obtained from a test is limited in scope but of sufficient quality, the laboratory may consult with the referring provider to discuss options of partial or limited reporting. Any limitations or deviations should be addressed in the final report (section E.4.2).
G.5. Bioinformatics and data sources
A quality assurance (Q/A) program for the bioinformatics process or pipeline should be developed to support the analysis, interpretation, and reporting of NGS data. The laboratory should establish the reproducibility of a chosen analytic pipeline; a given standard input should produce the same output each time it is interrogated by the pipeline. Pipelines should be versioned and revalidated when updated (section D.5.1). A system must be developed that allows the laboratory to track pipeline versions, the specific changes each version incorporates, and the date the new version was implemented on clinical samples. A Q/A program should be developed to monitor specific metrics, defined in the program, for both reference files and sources (as these are frequently updated) and output files (as changes to reference files may have unanticipated consequences) for each step of the process to ensure optimal performance. Such metrics may include:
-
Alignment and base calling are consistent with previous analyses
-
Analysis is complete and without errors
-
Expected variant annotations are made
-
Changed or improved processes have intended outcome
The Q/A program should also document corrective measures that have been put in place by the laboratory to report and resolve any deviation from the developed pipeline during the testing process. The Q/A program may also monitor concordance of variant classifications with external sources such as ClinVar, and examine the frequency of variant reclassifications within the laboratory. Laboratories should have a policy regarding the frequency of external data source updates (e.g., ClinVar, OMIM, gnomAD).
H. PROFICIENCY TESTING
Proficiency testing protocols must be established and executed according to laboratory licensing/accrediting agencies (CLIA, CAP). Many licensing/accrediting agencies require participation in formal proficiency testing programs that include specific samples and/or testing kits that are graded. When a formal proficiency testing program for a panel or single gene is not available, alternative assessments such as sample exchanges must be used to demonstrate ongoing proficiency. Proficiency testing should reflect the entire testing process from sequencing through analysis and reporting. CLIA requires proficiency testing or alternative assessments to be performed twice per year for each assay offered clinically. For NGS, the definition of the assay may be a gene panel, exome, or genome analysis. Several formal proficiency programs are available through the CAP for NGS-based testing including ES/GS, selected gene panels, and some single-gene disorders and also include analysis/bioinformatics-only and interpretation-only options.
I. SUMMARY
Identifying disease etiologies for genetic conditions with substantial genetic heterogeneity has been a longstanding and challenging diagnostic hurdle. NGS overcomes many of the scalability obstacles for DNA sequencing in the clinical lab. However, along with the capability to produce high-quality sequence data for applications ranging from clinically relevant targeted panels to the genome, NGS brings new technical challenges that must be appreciated and addressed. This updated version of the ACMG Standards for Clinical Next-Generation Sequencing covers a broad spectrum of topics for those already offering diagnostic testing based on this technology as well as those entering this arena. Most of the topics should be familiar to this audience, but are discussed in some detail given the many unique circumstances and demands of NGS. Although key aspects of the clinical implementation of NGS technology have been addressed, additional recommendations regarding specific applications of the technology may be needed in the future. As always, the diagnostic community will collectively benefit by discussing the newest and most pressing NGS issues together. This will require an ongoing dialogue among those already engaged in this pursuit, those determining how to become involved in this new paradigm of molecular testing, and those who will be responsible for ordering and communicating NGS results to patients.
References
Rehm, H. L. et al. ACMG clinical laboratory standards for next-generation sequencing. Genet. Med. 15, 733–747 (2013).
Beck, T. F. & Mullikin, J. C., NISC Comparative Sequencing Program & Biesecker, L. G. Systematic evaluation of Sanger validation of NextGen sequencing variants. Clin. Chem. 62, 647–654 (2016).
Santani, A. et al. Designing and implementing NGS tests for inherited disorders: a practical framework with step-by-step guidance for clinical laboratories. J. Mol. Diagn. 21, 369–374 (2019).
Bean, L. J. H. et al. Diagnostic gene sequencing panels: from design to report-a technical standard of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 22, 453–461 (2020).
Bick, D., Jones, M., Taylor, S. L., Taft, R. J. & Belmont, J. Case for genome sequencing in infants and children with rare, undiagnosed or genetic diseases. J. Med. Genet. 56, 783–791 (2019).
Vaz-Drago, R., Custódio, N. & Carmo-Fonseca, M. Deep intronic mutations and human disease. Hum. Genet. 136, 1093–1111 (2017).
Lambert, S. A., Abraham, G. & Inouye, M. Towards clinical utility of polygenic risk scores. Hum. Mol. Genet. 28, R133–R142 (2019).
Huang, A. Y. et al. MosaicHunter: accurate detection of postzygotic single-nucleotide mosaicism through next-generation sequencing of unpaired, trio, and paired samples. Nucleic Acids Res. 45, e76 (2017).
Clark, M. M. et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genom. Med. 3, 16 (2018).
Lionel, A. C. et al. Improved diagnostic yield compared with targeted gene sequencing panels suggests a role for whole-genome sequencing as a first-tier genetic test. Genet. Med. 20, 435–443 (2018).
Stavropoulos, D. J. et al. Whole genome sequencing expands diagnostic utility and improves clinical management in pediatric medicine. NPJ Genom. Med. 1, 15012 (2016).
Meienberg, J., Bruggmann, R., Oexle, K. & Matyas, G. Clinical sequencing: is WGS the better WES? Hum. Genet. 135, 359–362 (2016).
Saudi Mendeliome Group. Comprehensive gene panels provide advantages over clinical exome sequencing for Mendelian diseases. Genome Biol. 16, 134 (2015).
Belkadi, A. et al. Whole-genome sequencing is more powerful than whole-exome sequencing for detecting exome variants. Proc. Natl. Acad. Sci. U. S. A. 112, 5473–5478 (2015).
Soden, S. E. et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci. Transl. Med. 6, 265ra168 (2014).
Bush, L. W. et al. Professional responsibilities regarding the provision, publication, and dissemination of patient phenotypes in the context of clinical genetic and genomic testing: points to consider-a statement of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 20, 169–171 (2018).
Trujillano, D. et al. Clinical exome sequencing: results from 2819 samples reflecting 1000 families. Eur. J. Hum. Genet. 25, 176–182 (2017).
Posey, J. E. et al. Molecular diagnostic experience of whole-exome sequencing in adult patients. Genet. Med. 18, 678–685 (2016).
Yang, Y. et al. Molecular findings among patients referred for clinical whole-exome sequencing. JAMA. 312, 1870–1879 (2014).
Yang, Y. et al. Clinical whole-exome sequencing for the diagnosis of mendelian disorders. N. Engl. J. Med. 369, 1502–1511 (2013).
Ambardar, S., Gupta, R., Trakroo, D., Lal, R. & Vakhlu, J. High throughput sequencing: an overview of sequencing chemistry. Indian J. Microbiol. 56, 394–404 (2016).
Kircher, M., Sawyer, S. & Meyer, M. Double indexing overcomes inaccuracies in multiplex sequencing on the Illumina platform. Nucleic Acids Res. 40, e3 (2012).
Mamanova, L. et al. Target-enrichment strategies for next-generation sequencing. Nat. Methods. 7, 111–118 (2010).
Kozarewa, I., Armisen, J., Gardner, A. F., Slatko, B. E. & Hendrickson, C. L. Overview of target enrichment strategies. Curr. Protoc. Mol. Biol. 112, 7.21.1–7.21.23 (2015).
Ballester, L. Y., Luthra, R., Kanagal-Shamanna, R. & Singh, R. R. Advances in clinical next-generation sequencing: target enrichment and sequencing technologies. Expert Rev. Mol. Diagn. 16, 357–372 (2016).
Stevens, R. C. et al. A novel CRISPR/Cas9 associated technology for sequence-specific nucleic acid enrichment. PLoS One. 14, e0215441 (2019).
McCombie, W. R., McPherson, J. D. & Mardis, E. R. Next-generation sequencing technologies. Cold Spring Harb. Perspect. Med. 9, a036798 (2019).
Glenn, T. C. Field guide to next-generation DNA sequencers. Mol. Ecol. Resour. 11, 759–769 (2011).
Jennings, L., Van Deerlin, V. M. & Gulley, M. L. & College of American Pathologists Molecular Pathology Resource Committee. Recommended principles and practices for validating clinical molecular pathology tests. Arch. Pathol. Lab. Med. 133, 743–755 (2009).
Monaghan, K. G. et al. ACMG policy statement. Risk categorization for oversight of laboratory-developed tests for inherited conditions. Genet. Med. 15, 314–315 (2013).
Jain, M. et al. Nanopore sequencing and assembly of a human genome with ultra-long reads. Nat. Biotechnol. 36, 338–345 (2018).
Smadbeck, J. B. et al. Copy number variant analysis using genome-wide mate-pair sequencing. Genes Chromosomes Cancer. 57, 459–470 (2018).
Mikheyev, A. S. & Tin, M. M. Y. A first look at the Oxford Nanopore MinION sequencer. Mol. Ecol. Resour. 14, 1097–1102 (2014).
Wong, K. H. Y., Levy-Sakin, M. & Kwok, P. Y. De novo human genome assemblies reveal spectrum of alternative haplotypes in diverse populations. Nat. Commun. 9, 3040 (2018).
Dolzhenko, E. et al. Detection of long repeat expansions from PCR-free whole-genome sequence data. Genome Res. 27, 1895–1903 (2017).
Harewood, L. et al. Hi-C as a tool for precise detection and characterisation of chromosomal rearrangements and copy number variation in human tumours. Genome Biol. 18, 125 (2017).
Wenger, A. M. et al. Accurate circular consensus long-read sequencing improves variant detection and assembly of a human genome. Nat. Biotechnol. 37, 1155–1162 (2019).
Mitsuhashi, S. & Matsumoto, N. Long-read sequencing for rare human genetic diseases. J. Hum. Genet. 65, 11–19 (2020).
Audano, P. A. et al. Characterizing the major structural variant alleles of the human genome. Cell. 176, 663–675 (2019).
Gong, L., Wong, C. H., Idol, J., Ngan, C. Y. & Wei, C. L. Ultra-long read sequencing for whole genomic DNA analysis. J. Vis. Exp. 145, e58954 (2019).
Clark, M. J. et al. Performance comparison of exome DNA sequencing technologies. Nat. Biotechnol. 29, 908–914 (2011).
Sims, D., Sudbery, I., Ilott, N. E., Heger, A. & Ponting, C. P. Sequencing depth and coverage: key considerations in genomic analyses. Nat. Rev. Genet. 15, 121–132 (2014).
Mandelker, D. et al. Navigating highly homologous genes in a molecular diagnostic setting: a resource for clinical next-generation sequencing. Genet. Med. 18, 1282–1289 (2016).
Mandelker, D. et al. Comprehensive diagnostic testing for stereocilin: an approach for analyzing medically important genes with high homology. J. Mol. Diagn. 16, 639–647 (2014).
Gould, G. M. et al. Detecting clinically actionable variants in the 3’ exons of PMS2 via a reflex workflow based on equivalent hybrid capture of the gene and its pseudogene. BMC Med. Genet. 19, 176 (2018).
Food and Drug Administration. Considerations for design, development, and analytical validation of next generation sequencing (NGS)—based in vitro diagnostics (IVDs) intended to aid in the diagnosis of suspected germline diseases. 83 FR 16106 (2018).
Lincoln, S. E. et al. A rigorous interlaboratory examination of the need to confirm next-generation sequencing-detected variants with an orthogonal method in clinical genetic testing. J. Mol. Diagn. 21, 318–329 (2019).
Zook, J. M. et al. Integrating human sequence data sets provides a resource of benchmark SNP and indel genotype calls. Nat. Biotechnol. 32, 246–251 (2014).
Zook, J. M. et al. Extensive sequencing of seven human genomes to characterize benchmark reference materials. Sci. Data. 3, 160025 (2016).
Zook, J. M. et al. An open resource for accurately benchmarking small variant and reference calls. Nat. Biotechnol. 37, 561–566 (2019).
Eberle, M. A. et al. A reference data set of 5.4 million phased human variants validated by genetic inheritance from sequencing a three-generation 17-member pedigree. Genome Res. 27, 157–164 (2017).
Highnam, G. et al. An analytical framework for optimizing variant discovery from personal genomes. Nat. Commun. 6, 6275 (2015).
Roy, S. et al. Standards and guidelines for validating next-generation sequencing bioinformatics pipelines: a joint recommendation of the Association for Molecular Pathology and the College of American Pathologists. J. Mol. Diagn. 20, 4–27 (2018).
Luh, F. & Yen, Y. FDA guidance for next generation sequencing-based testing: balancing regulation and innovation in precision medicine. NPJ Genom. Med. 3, 28 (2018).
Ledergerber, C. & Dessimoz, C. Base-calling for next-generation sequencing platforms. Brief Bioinform. 12, 489–497 (2011).
Xu, C. A review of somatic single nucleotide variant calling algorithms for next-generation sequencing data. Comput. Struct. Biotechnol. J. 16, 15–24 (2018).
Giannoulatou, E., Park, S. H., Humphreys, D. T. & Ho, J. W. K. Verification and validation of bioinformatics software without a gold standard: a case study of BWA and Bowtie. BMC Bioinformatics. 15, S15 (2014).
Berger, B., Peng, J. & Singh, M. Computational solutions for omics data. Nat. Rev. Genet. 14, 333–346 (2013).
Li, H. & Homer, N. A survey of sequence alignment algorithms for next-generation sequencing. Brief Bioinform. 11, 473–483 (2010).
Zhao, Y., Wang, X. & Tang, H. A secure alignment algorithm for mapping short reads to human genome. J. Comput. Biol. 25, 529–540 (2018).
Bohannan, Z. S. & Mitrofanova, A. Calling variants in the clinic: informed variant calling decisions based on biological, clinical, and laboratory variables. Comput. Struct. Biotechnol. J. 17, 561–569 (2019).
DePristo, M. A. et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat. Genet. 43, 491–498 (2011).
Greer, S. U. & Ji, H. P. Structural variant analysis for linked-read sequencing data with gemtools. Bioinformatics. 35, 4397–4399 (2019).
Tan, A., Abecasis, G. R. & Kang, H. M. Unified representation of genetic variants. Bioinformatics. 31, 2202–2204 (2015).
Lubin, I. M. et al. Principles and recommendations for standardizing the use of the next-generation sequencing variant file in clinical settings. J. Mol. Diagn. 19, 417–426 (2017).
Jennings, L. J. et al. Guidelines for validation of next-generation sequencing-based oncology panels: a joint consensus recommendation of the Association for Molecular Pathology and College of American Pathologists. J. Mol. Diagn. 19, 341–365 (2017).
Mahamdallie, S. et al. The Quality Sequencing Minimum (QSM): providing comprehensive, consistent, transparent next generation sequencing data quality assurance. Wellcome Open Res. 3, 37 (2018).
D’Gama, A. M. & Walsh, C. A. Somatic mosaicism and neurodevelopmental disease. Nat. Neurosci. 21, 1504–1514 (2018).
Qin, L. et al. Detection and quantification of mosaic mutations in disease genes by next-generation sequencing. J. Mol. Diagn. 18, 446–453 (2016).
Stosser, M. B. et al. High frequency of mosaic pathogenic variants in genes causing epilepsy-related neurodevelopmental disorders. Genet. Med. 20, 403–410 (2018).
Abicht, A. et al. Mitochondrial and nuclear disease panel (Mito-aND-Panel): combined sequencing of mitochondrial and nuclear DNA by a cost-effective and sensitive NGS-based method. Mol. Genet. Genomic Med. 6, 1188–1198 (2018).
Kumaran, M., Subramanian, U. & Devarajan, B. Performance assessment of variant calling pipelines using human whole exome sequencing and simulated data. BMC Bioinformatics. 20, 342 (2019).
Wei, Z. et al. Whole-exome sequencing identifies novel recurrent somatic mutations in sporadic parathyroid adenomas. Endocrinology. 159, 3061–3068 (2018).
Pfeiffer, F. et al. Systematic evaluation of error rates and causes in short samples in next-generation sequencing. Sci. Rep. 8, 10950 (2018).
Schirmer, M., D’Amore, R., Ijaz, U. Z., Hall, N. & Quince, C. Illumina error profiles: resolving fine-scale variation in metagenomic sequencing data. BMC Bioinformatics. 17, 125 (2016).
Jun, G. et al. Detecting and estimating contamination of human DNA samples in sequencing and array-based genotype data. Am. J. Hum. Genet. 91, 839–848 (2012).
Sehn, J. K. et al. Occult specimen contamination in routine clinical next-generation sequencing testing. Am. J. Clin. Pathol. 144, 667–674 (2015).
Sangiovanni, M., Granata, I., Thind, A. S. & Guarracino, M. R. From trash to treasure: detecting unexpected contamination in unmapped NGS data. BMC Bioinformatics. 20, 168 (2019).
Hume, S. et al. CCMG practice guideline: laboratory guidelines for next-generation sequencing. J. Med. Genet. 56, 792–800 (2019).
Mattocks, C. J. et al. A standardized framework for the validation and verification of clinical molecular genetic tests. Eur. J. Hum. Genet. 18, 1276–1288 (2010).
Chaisson, M. J. P. et al. Multi-platform discovery of haplotype-resolved structural variation in human genomes. Nat. Commun. 10, 1784 (2019).
Lee, H. et al. Clinical exome sequencing for genetic identification of rare Mendelian disorders. JAMA. 312, 1880–1887 (2014).
Retterer, K. et al. Clinical application of whole-exome sequencing across clinical indications. Genet. Med. 18, 696–704 (2016).
Chen, B. et al. Good laboratory practices for molecular genetic testing for heritable diseases and conditions. MMWR Recomm. Rep. 58, 1–37 (2009).
Whiffin, N. et al. Using high-resolution variant frequencies to empower clinical genome interpretation. Genet. Med. 19, 1151–1158 (2017).
Kelly, M. A. et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: recommendations by ClinGen’s Inherited Cardiomyopathy Expert Panel. Genet. Med. 20, 351–359 (2018).
Gelb, B. D. et al. ClinGen’s RASopathy Expert Panel consensus methods for variant interpretation. Genet. Med. 20, 1334–1345 (2018).
Bell, C. J. et al. Carrier testing for severe childhood recessive diseases by next-generation sequencing. Sci. Transl. Med. 3, 65ra4 (2011).
Shashi, V. et al. A comprehensive iterative approach is highly effective in diagnosing individuals who are exome negative. Genet. Med. 21, 161–172 (2019).
Sobreira, N. L. M. et al. Matchmaker Exchange. Curr. Protoc. Hum. Genet. 95, 9.31.1–9.31.15 (2017).
Majewski, J., Schwartzentruber, J., Lalonde, E., Montpetit, A. & Jabado, N. What can exome sequencing do for you? J. Med. Genet. 48, 580–589 (2011).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Strande, N. T. et al. Evaluating the clinical validity of gene–disease associations: an evidence-based framework developed by the Clinical Genome Resource. Am. J. Hum. Genet. 100, 895–906 (2017).
Garber, K. B., Vincent, L. M., Alexander, J. J., Bean, L. J. H., Bale, S. & Hegde, M. Reassessment of genomic sequence variation to harmonize interpretation for personalized medicine. Am. J. Hum. Genet. 99, 1140–1149 (2016).
Harrison, S. M. et al. Clinical laboratories collaborate to resolve differences in variant interpretations submitted to ClinVar. Genet. Med. 19, 1096–1104 (2017).
Rehm, H. L. A new era in the interpretation of human genomic variation. Genet. Med. 19, 1092–1095 (2017).
ACMG Board of Directors. Laboratory and clinical genomic data sharing is crucial to improving genetic health care: a position statement of the American College of Medical Genetics and Genomics. Genet. Med. 19, 721–722 (2017).
Green, R. C. et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet. Med. 15, 565–574 (2013).
American College of Medical Genetics and Genomics. Incidental findings in clinical genomics: a clarification. Genet. Med. 15, 664–666 (2013).
Kalia, S. S. et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet. Med. 19, 249–255 (2017).
Biesecker, L. G. Genomic screening and genomic diagnostic testing-two very different kettles of fish. Genome Med. 11, 75 (2019).
Hagenkord, J. et al. Design and reporting considerations for genetic screening tests. J. Mol. Diagn. 22, 599–609 (2020).
Rehder, C. W., David, K. L., Hirsch, B., Toriello, H. V., Wilson, C. M. & Kearney, H. M. American College of Medical Genetics and Genomics: standards and guidelines for documenting suspected consanguinity as an incidental finding of genomic testing. Genet. Med. 15, 150–152 (2013).
Deignan, J. L. et al. Points to consider when assessing relationships (or suspecting misattributed relationships) during family-based clinical genomic testing: a statement of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 8, 1285–1287 (2020).
Recchia, G., Chiappi, A., Chandratillake, G., Raymond, L. & Freeman, A. L. J. Creating genetic reports that are understood by nonspecialists: a case study. Genet. Med. 22, 353–361 (2020).
Milko, L. V. et al. An age-based framework for evaluating genome-scale sequencing results in newborn screening. J. Pediatr. 209, 68–76 (2019).
Li, M. M. et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J. Mol. Diagn. 19, 4–23 (2017).
Huang, Y., Deng, L., Zhong, Y. & Yi, M. The association between E326K of GBA and the risk of Parkinson’s disease. Parkinsons Dis. 2018, 1048084 (2018).
Zhang, L. et al. Fumarate hydratase FH c.1431_1433dupAAA (p.Lys477dup) variant is not associated with cancer including renal cell carcinoma. Hum. Mutat. 41, 103–109 (2020).
Lu, J. T. et al. Evaluation for genetic disorders in the absence of a clinical indication for testing: elective genomic testing. J. Mol. Diagn. 21, 3–12 (2019).
Centers for Medicare & Medicaid Services (CMS), HHS; Centers for Disease Control and Prevention (CDC), HHS; Office for Civil Rights (OCR), HHS. CLIA program and HIPAA privacy rule; patients’ access to test reports. Final rule. Fed. Regist. 79, 7289–7316 (2014).
Deignan, J. L., Chung, W. K., Kearney, H. M., Monaghan, K. G., Rehder, C. W. & Chao, E. C. Points to consider in the reevaluation and reanalysis of genomic test results: a statement of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 21, 1267–1270 (2019).
SoRelle, J. A., Thodeson, D. M., Arnold, S., Gotway, G. & Park, J. Y. Clinical utility of reinterpreting previously reported genomic epilepsy test results for pediatric patients. JAMA Pediatr. 173, e182302 (2019).
Machini, K. et al. Analyzing and reanalyzing the genome: findings from the MedSeq project. Am. J. Hum. Genet. 105, 177–188 (2019).
David, K. L. et al. Patient re-contact after revision of genomic test results: points to consider-a statement of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. 21, 769–771 (2019).
Maddalena, A., Bale, S., Das, S., Grody, W. & Richards, S. Technical standards and guidelines: molecular genetic testing for ultra-rare disorders. Genet. Med. 7, 571–583 (2005).
Hardwick, S. A., Deveson, I. W. & Mercer, T. R. Reference standards for next-generation sequencing. Nat. Rev. Genet. 18, 473–484 (2017).
Acknowledgements
Members of the working group were reviewed for conflicts of interest by the Board of the ACMG. This work was supported in part by the ACMG Foundation for Genetic and Genomic Medicine.
Author information
Authors and Affiliations
Consortia
Ethics declarations
Competing interests
Funding and support listed below did not support development of this document unless included in Acknowledgements. C.R. reports receiving consulting compensation from Illumina and RTI International. L.J.H.B. is an employee of PerkinElmer, Inc. D.B. receives consulting compensation from The Northwestern Mutual Life Insurance Company and iRepertoire, Inc. and is an uncompensated member of the Genomics England Scientific Advisory Committee. E.C. is employed by Ambry Genetics. W.C. receives an honorarium as a scientific advisory board member of the Regeneron Genetics Center. H.R. is compensated and receives equity as a scientific advisory board member of Genome Medicine and receives grant support from NIH for work that overlaps with this document. V.S. receives consulting compensation from Innovations Research and Training Inc. The other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer
This technical standard is designed primarily as an educational resource for clinical laboratory geneticists to help them provide quality clinical laboratory genetic services. Adherence to this standard is voluntary and does not necessarily assure a successful medical outcome. This technical standard should not be considered inclusive of all proper procedures and tests or exclusive of other procedures and tests that are reasonably directed to obtaining the same results. In determining the propriety of any specific procedure or test, the clinical laboratory geneticist should apply his or her own professional judgment to the specific circumstances presented by the individual or specimen.
Clinical laboratory geneticists are encouraged to document in the patient’s record the rationale for the use of a particular procedure or test, whether or not it is in conformance with this technical standard. They also are advised to take notice of the date any particular technical standard was adopted, and to consider other relevant medical and scientific information that becomes available after that date. It also would be prudent to consider whether intellectual property interests may restrict the performance of certain tests and other procedures.
The Board of Directors of the American College of Medical Genetics and Genomics approved this technical standard on 25 January 2021.
The related article can be found at https://doi.org/10.1038/gim.2013.92.
Supplementary information
Rights and permissions
About this article
Cite this article
Rehder, C., Bean, L.J.H., Bick, D. et al. Next-generation sequencing for constitutional variants in the clinical laboratory, 2021 revision: a technical standard of the American College of Medical Genetics and Genomics (ACMG). Genet Med 23, 1399–1415 (2021). https://doi.org/10.1038/s41436-021-01139-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01139-4
This article is cited by
-
Identification of a novel ATR-X mutation causative of acquired α-thalassemia in a myelofibrosis patient
Egyptian Journal of Medical Human Genetics (2024)
-
Validated WGS and WES protocols proved saliva-derived gDNA as an equivalent to blood-derived gDNA for clinical and population genomic analyses
BMC Genomics (2024)
-
Rapid genomic sequencing for genetic disease diagnosis and therapy in intensive care units: a review
npj Genomic Medicine (2024)
-
Multiscale analysis of pangenomes enables improved representation of genomic diversity for repetitive and clinically relevant genes
Nature Methods (2023)
-
Time to make rare disease diagnosis accessible to all
Nature Medicine (2022)