Abstract
Background/Aims
To identify factors predictive of post-management secondary glaucoma in eyes with iris melanoma.
Methods
Patients with iris melanoma who were conservatively managed on the Ocular Oncology Service, Wills Eye Hospital from 1970 to 2016 were included. Charts were retrospectively reviewed, and binary logistic regression analysis was performed. Main outcome measures were factors predictive of post-management glaucoma, defined as intraocular pressure (IOP) > 22 mmHg following melanoma treatment.
Results
Of 271 patients with iris melanoma, melanoma-related glaucoma was identified in 40 (15%) at presentation and post-management glaucoma developed in 75 (28%) at a mean of 103.7 months (range:1.0-120.0). Comparison (post-management glaucoma vs. no glaucoma) revealed patients with post-management glaucoma presented with worse visual acuity (20/50-20/150) (17% vs. 5%, p = 0.001), increased mean tumour basal diameter (5.1 mm vs. 4.3 mm, p = 0.004), greater melanoma-related increased IOP on presentation (24.1 mmHg vs. 16.2 mmHg, p < 0.001), diffuse tumour shape (9% vs. 4%, p = 0.01), American Joint Committee on Cancer (AJCC) T4 category (7% vs. 2%, p = 0.03), and extraocular tumour extension (7% vs. 2%, p = 0.03). Risk factors for post-management glaucoma identified by multivariate analysis included melanoma-related increased IOP at presentation (OR:1.1, [1.08–1.22] per 1-mmHg increase, p < 0.001), increased mean tumour basal diameter (OR:1.17, [1.02–1.33] per 1-millimetre increments, p = 0.03), advanced AJCC clinical T subcategory (OR:1.23, [1.04–1.46] per 1-subcategory increments, p = 0.02) and plaque radiotherapy treatment (OR:2.32, [1.13–4.75], p = 0.02).
Conclusion
Features of iris melanoma that predicted post-management glaucoma included melanoma-related increased IOP on presentation, advanced AJCC clinical T subcategory, increased mean tumour basal diameter, and plaque radiotherapy treatment.
Similar content being viewed by others
Introduction
Uveal melanoma, which includes iris, ciliary body, and choroidal melanoma, is the most common primary intraocular cancer in adults, with a mean age-adjusted incidence of 5.1 cases per million per year [1]. Iris melanoma is relatively rare, comprising only 4% of all uveal melanoma cases [2], and tends to affect younger individuals [3]. Tumour features of iris melanoma including tumour size, extent, invasion of the angle or iris stroma, and the presence of melanoma-related glaucoma have implications for tumour management. While localized nodular tumours without signs of seeding can be managed with local resection or plaque radiotherapy, eyes with extensive multinodular or diffuse-type tumours require transcorneal plaque radiotherapy or enucleation [4].
Melanoma-related glaucoma at presentation is recognized in approximately 14% to 40% of affected eyes and can be mediated through several mechanisms including direct tumour infiltration of the angle, seeding of tumour into the angle through pigment dispersion, iris and angle neovascularization, and hyphema [5,6,7,8,9,10,11]. Post-management glaucoma includes melanoma-related glaucoma plus additional treatment factors that lead to elevated intraocular pressure (IOP). Melanoma-related glaucoma has been associated with a 4.5 times increased risk of metastasis (HR: 4.51 [1.92–10.60], p < 0.001) [12]. Meanwhile, post-management glaucoma has been associated with worse ocular and systemic outcomes, related to an 11 times increased risk for melanoma recurrence (HR:11.36, [2.39–54.0], p = 0.002) [6].
In this analysis, we longitudinally monitored patients with iris melanoma who were treated to characterize the incidence of and risk factors for post-management glaucoma.
Materials and methods
Patients with a diagnosis of primary iris melanoma based on American Joint Committee on Cancer (AJCC) classification 8th edition criteria [13], and managed at the Ocular Oncology Service at Wills Eye Hospital, Philadelphia, Pennsylvania between August 25, 1970, and November 30, 2016, were included in this analysis. Diagnosis of iris melanoma required documented enlargement of a melanocytic iris tumour over a period of 5 years or less or fine-needle aspiration biopsy-proven iris melanoma [14]. The Institutional Review Board of the Wills Eye Hospital approved this study, which adheres to the tenets of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. As all data were de-identified, informed consent was not required.
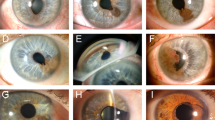
Data were collected retrospectively and included demographic information: age at presentation, sex, race, and ocular history. Ophthalmoscopic examination findings including initial visual acuity, IOP, iris colour, and anterior segment exam findings were documented. Tumour characteristics, quadrantic tumour epicentre, anteroposterior tumour epicentre, anterior tumour margin, posterior tumour margin, configuration, shape, tumour colour, tumour surface, iris stromal and angle seeding, AJCC Classification 8th edition primary tumour category [13], and anterior chamber findings were recorded. Associated features were also documented. Tumour dimensions were measured using slit lamp biomicroscopy and were aided by ophthalmic ultrasound. In all cases, anterior segment optical coherence tomography was performed. In cases where ciliary body involvement was suspected, ultrasound biomicroscopy was performed. Findings of fine needle aspiration biopsy and intravenous fluorescein angiography, when available, were recorded.
The primary reason for choice of treatment was recorded. Treatment other than enucleation, including observation, local resection, and plaque radiotherapy, was considered as conservative management. Observation was reserved for eyes with iris melanoma that received treatment elsewhere, were small (<3 mm basal diameter) in asymptomatic patients, or based on the patient’s preference. Periodic photographic documentation was performed. Local resection (iris, iris and trabecular meshwork, iris, and ciliary body) was generally performed in small iris melanoma with documented growth or when tumours were of limited size and extent. Plaque radiotherapy was the selected treatment if the malignancy was too large or ill-defined for resection (>4 clock hours of iris involvement) or if there was tumour seeding (>2 clock hours) on the iris stroma or in the anterior chamber angle. This study utilized iodine-125 plaque radiotherapy, which was custom-designed on the basis of tumour characteristics and necessary radiation dosimetry to achieve a target dose of 8000 centigray to the tumour apex [6]. Enucleation was the treatment of choice in the presence of uncontrollable or painful melanoma-related glaucoma (>40 mmHg on maximal medications), diffuse (not localized) or extensive (>5 mm) extrascleral extension of melanoma, or anticipated poor compliance.
Complete ophthalmic examination was performed by one of the senior authors (C.L.S., J.A.S.), and photographic documentation was performed with anterior segment and posterior segment photography, gonioscopic images, anterior segment optical coherence tomography, fluorescein angiography, and ultrasound biomicroscopy. Follow-up examinations were conducted at 4- to 6-month intervals during the first 5 years and then at 6- to 12-month intervals. Our centre recommended systemic surveillance with medical oncology specialists for all patients to monitor for metastatic disease with abdominal MRI, CT, or combined PET-CT every 6 months after ocular treatment.
Melanoma-related glaucoma was defined as ocular hypertension with IOP > 22 mmHg at initial presentation. Post-management glaucoma was defined as glaucoma following melanoma treatment with ocular hypertension with IOP > 22 mmHg in the follow-up period. Structural or functional damage typically associated with glaucoma was evaluated by glaucoma specialists. The main outcome measures included factors predictive of post-management glaucoma in eyes with iris melanoma. The time interval for each outcome was recorded.
Statistical analysis
Statistical analysis was performed using SPSS Statistics Software (Version 26; SPSS Inc.). Continuous variables were expressed as mean (median, range). The one-sample Kolmogorov-Smirnov test was used to assess normality of distribution. Comparison between groups (post-management glaucoma vs. no glaucoma) was performed using the one-way ANOVA test for continuous variables with normal distribution and Mann-Whitney U test for continuous variables without normal distribution. Comparison of categorical variables was performed using the Chi-square test and Fisher’s exact test when indicated. Kaplan-Meier analysis was used to determine the time to post-management glaucoma development over a 10-year period. Cox proportional hazards regression was performed to identify the risk of post-management glaucoma development with each type of treatment. Binary logistic regression analysis was performed to identify factors predictive of post-management glaucoma. Independent variables that showed significance in association testing were included in the logistic regression. Variables found to be significant in univariate analysis at a level of p < 0.05 were entered into multivariate regression models using the forward stepwise Wald method. Odds ratios and 95% confidence intervals were generated for both univariate and multivariate regression models. A p-value <0.05 was considered statistically significant for the results of multivariate regression.
Results
Over the study duration, 432 patients met AJCC classification 8th edition criteria17 for primary iris melanoma.
Primary management for iris melanoma included enucleation in 62 (14%) and conservative management in 370 (86%). Conservative management included observation in 81 (22%), local resection in 216 (58%), and plaque radiotherapy in 73 (20%). Observation was performed in small tumours, those that were previously treated elsewhere, or per patient preference. Prior management in each group was as follows: of those observed at our practice (n = 81), management elsewhere was observation in 43 (53%), local resection/biopsy in 7 (9%), plaque radiotherapy in 1 (1%), and none/unknown in 30 (37%); of those who underwent local resection at our practice (216 patients), management elsewhere was observation in 113 (52%), local resection/biopsy in 11 (5%), plaque radiotherapy in 1 (<1%), and none/unknown in 91 (42%); of those who underwent plaque radiotherapy at our practice (73 patients), management elsewhere was observation in 31 (43%), local resection/biopsy in 14 (19%), and none/unknown in 28 (38%). Follow-up data were available in 362 (84%) patients. Mean follow-up duration was 83.0 months (61.0, range: 1.0–412.0) with 304 patients followed for at least 1 year, 238 for at least 3 years, 186 for at least 5 years, and 91 for at least 10 years. Information on melanoma-related glaucoma at presentation and the development of post-management glaucoma in the follow-up period was available in 271 patients. Melanoma-related glaucoma was identified in 40 (15%) patients on presentation, and post-management glaucoma developed in 75 (28%) patients. 35 patients who had melanoma-related glaucoma also had elevated IOPs post-management. Management modalities are listed in Table 1. Comparison (post-management glaucoma vs. no glaucoma) revealed patients who had post-management glaucoma had a lower frequency of local resection (49% vs. 66%, p = 0.01) and higher frequency of plaque radiotherapy (41% vs. 16%, p < 0.001). Observation as a management strategy did not lead to a statistically significant higher incidence of post-management glaucoma development.
Mean time to the development of post-management glaucoma was 103.7 months (range: 1.0–120.0). Results of Kaplan-Meier analysis are represented in Fig. 1a. Comparison of management options (observation vs. local resection vs. plaque radiotherapy) revealed an increased 10-year rate of post-management glaucoma after plaque radiotherapy (16% vs. 14% vs. 35%; p = 0.002). Cox proportional hazards regression analysis revealed increased risk of post-management glaucoma development after plaque radiotherapy compared to local resection at 10 years (HR: 3.19, [1.51–6.72], p = 0.002). As compared to observation, local resection was not associated with increased risk of post-management glaucoma development at 10 years. There was an increased 10-year rate of vision loss of 3 lines or greater after plaque radiotherapy (34% vs. 45% vs. 73%; p < 0.001) (Fig. 1b). Cox proportional hazards regression revealed vision loss of 3 lines or greater was more likely in the plaque radiotherapy group at 10 years (HR: 4.58, [1.95–10.78], p < 0.001). Recurrence, metastasis, and enucleation were not associated with treatment type (Supplemental Fig. 1, 2, 3).
a Kaplan–Meier analysis of the development of post-management glaucoma based in eyes with iris melanoma receiving conservative management, including observation, local resection, and plaque radiotherapy. A comparison (observation vs. local resection vs. plaque radiotherapy) at 10 years demonstrated that plaque radiotherapy was associated with more frequent development of post-management glaucoma (16% vs. 14% vs. 35%; p = 0.002). b Kaplan–Meier analysis of visual acuity loss ≥ 3 lines based on iris melanoma conservative management, including observation, local resection, and plaque radiotherapy. A comparison (observation vs. local resection vs. plaque radiotherapy) at 10 years demonstrated that plaque radiotherapy was associated with more frequent development of post-management glaucoma (34% vs. 45% vs. 73%; p < 0.001).
Demographic features are listed in Table 1. Comparison (post-management glaucoma vs. no glaucoma) revealed patients who developed post-management glaucoma presented with mean older age (56.6 vs. 49.7 years, p = 0.004). There was no difference with regard to sex, race or involved eye.
Clinical, tumour, and associated features at presentation are listed in Table 2. Comparison (post-management glaucoma vs. no glaucoma) revealed patients who developed post-management glaucoma presented with lower frequency of Snellen visual acuity 20/20-20/40 (79% vs. 91%, p = 0.01), higher frequency of Snellen visual acuity 20/50-20/150 (17% vs/ 5%, p = 0.001), melanoma-related increased IOP on presentation (24.1 mmHg vs. 16.2 mmHg, p < 0.001), increased mean tumour basal diameter (5.1 mm vs. 4.3 mm, p = 0.004), higher frequency of diffuse tumour shape (9% vs. 4%, p = 0.01), higher frequency of AJCC T4 category (7% vs. 2%, p = 0.03), and higher frequency of extraocular tumour extension (7% vs. 2%, p = 0.03).
Results of binary logistic regression analysis determining factors predictive of post-management glaucoma are listed in Table 3. On univariate analysis, factors predictive of post-management glaucoma development included advanced age at presentation (OR: 1.02, [1.01–1.04], per 1-year increase, p = 0.01), Snellen visual acuity 20/50-20/150 (OR: 3.88, [1.62–9.31], p = 0.002), melanoma-related increased IOP at presentation (OR: 1.19, [1.12–1.25] per 1 mmHg increase, p < 0.001), advanced AJCC clinical T subcategory (OR: 1.44, [1.24–1.68] per 1 subcategory increment, p < 0.001), larger mean tumour basal diameter (OR: 1.17, [1.04–1.33] per 1 mm increase, p = 0.01), diffuse tumour shape (OR: 7.83, [1.79–34.35], p = 0.01), extraocular extension (OR: 4.60, [1.07–19.73], p = 0.04), and treatment with plaque radiotherapy (OR: 5.14, [1.99–13.30], p = 0.001). Treatment with local resection was associated with decreased risk of post-management glaucoma development (OR: 0.51, [0.30–0.87], p = 0.01).
On multivariate analysis, 3 models were created to determine factors predictive of post-management glaucoma development. In model 1, demographics and clinical features were utilized. Melanoma-related increased IOP at presentation (OR: 1.17, [1.10–1.24] per 1 mmHg increase, p < 0.001) and advanced AJCC clinical T subcategory (OR: 1.23, [1.04–1.46] per 1 subcategory increment, p = 0.02) were associated with increased risk. Model 2 utilized intrinsic tumour features, associated tumour features, and treatment type. Increased mean tumour basal diameter (OR: 1.17, [1.02–1.33] per 1 mm increase, p = 0.03) and treatment with plaque radiotherapy (OR: 3.55, [12.14–15.00], p < 0.001) were associated with increased risk. The results of models 1 and 2 were combined to form model 3, which found melanoma-related increased IOP at presentation (OR: 1.15, [1.08–1.22] per 1 mmHg increase, p < 0.001) and treatment with plaque radiotherapy (OR: 2.32, [1.13-4.75], p = 0.02) to be associated with increased risk of post-management glaucoma development. Advanced AJCC clinical T subcategory and larger mean tumour basal diameter were no longer significant in the final model. Model 3 (Nagelkerke R2 = 0.34) explained the greatest variance in post-management glaucoma development [vs. models 1 (Nagelkerke R2 = 0.32) and 2 (Nagelkerke R2 = 0.14)], making it the best fit model. Of the 60 patients requiring post-management glaucoma treatment, 49 (81.7%) were managed on topical medications alone, 4 (6.7%) underwent trabeculectomy, 3 (5.0%) underwent glaucoma drainage device implantation, 3 (5.0%) underwent cyclophotocoagulation, and 1 (1.7%) underwent laser trabeculoplasty.
Visual acuity and tumour outcomes between the post-management glaucoma and no glaucoma groups are listed in Table 4. Comparison (post-management glaucoma vs. no glaucoma) at the last-follow-up visit revealed lower Snellen visual acuity (CF vs. 20/70, p < 0.001), greater proportion with visual acuity loss of 3 lines or greater (77% vs. 40%, p < 0.001), higher incidence of tumour recurrence (20% vs. 7%, p = 0.003), and greater need for enucleation (16% vs. 6%, p = 0.01) in the group with post-management glaucoma. There was no statistically significant difference in the incidence of metastasis and death.
Discussion
This case series found that 28% of iris melanoma eyes develop post-management glaucoma, which is in keeping with prior reports [5,6,7,8,9,10,11]. Additionally, we identified melanoma-related increased intraocular pressure at initial visit, advanced American Joint Committee on Cancer clinical T subcategory, increased mean tumour basal diameter, and treatment with plaque radiotherapy as risk factors for the development of post-management glaucoma in eyes with iris melanoma. In addition to visual disability associated with glaucomatous disease, iris melanoma-associated glaucoma and post-management glaucoma are associated with greater need for enucleation [12], and greater tumour recurrence [6], and systemic metastasis [5, 8, 12]. Given the relatively good prognosis of iris melanoma overall and poor prognostic factors associated with post-management glaucoma, early identification of this condition could be associated with more favourable outcomes.
Prior studies by Shields et al. reported a greater likelihood of flat tumours (diffuse iris melanoma) with seeding on the iris stroma and into the angle [6] and greater frequency of AJCC category T4 vs. T1 [12] in patients with iris melanoma-related glaucoma on presentation. In the present study, by multivariate analysis, the only tumour features found to be predictive of post-management glaucoma were advanced AJCC clinical T category and increased mean tumour basal diameter. Additionally, we found that while those with post-management glaucoma were more likely to have a diffuse tumour shape and extraocular extension, these findings were not significant in the multivariate analysis. A likely reason for this difference is that prior studies have assessed melanoma-related glaucoma on presentation, while our report is on post-management glaucoma. In the majority of cases, treatment of iris melanoma leads to change in tumour morphology, which may result in regression of tumour infiltration into the angle with decrease in IOP. Alternatively, treatment could lead to an increase in necrotic debris in the anterior chamber angle or trabecular fibrosis, each leading to increase in IOP. Furthermore, those with post-management glaucoma were older and had moderately poor visual acuity at initial visit, but these were not independent risk factors for this condition.
In a combined model including demographics, clinical features, tumour features, associated features, and treatment, melanoma-related increased IOP at presentation and treatment with plaque radiotherapy were associated with increased risk of post-management glaucoma. Eyes selected for plaque radiotherapy treatment typically have more extensive tumour spread than those that undergo local resection or those that are observed; therefore, it is not possible to randomize treatment across tumour sizes. Bechrakis et al. provided retrospective data on 152 cases of uveal melanoma and accounted for this bias by matching 54 of the studied patients in treatment groups by tumour size, and found that the incidence of post-management glaucoma after transscleral tumour resection was significantly lower at 5.6% as compared to 33.3% after plaque radiotherapy (p = 0.03) [15]. Our study supports these results by establishing a 2.3 times increased risk of post-management glaucoma following plaque radiotherapy as compared to local resection, while adjusting for various baseline characteristics, including tumour size. When compared to the study by Bechrakis et al., the present study reported a higher rate of post-management glaucoma after local resection and plaque radiotherapy at 22% and 50%, respectively. This may be due to the inclusion of all uveal melanoma types in the prior study, while our report is exclusively on iris melanoma, the location and spread of which is more likely to lead to post-management glaucoma than choroidal melanoma [6, 7, 12]. Additionally, the present study found that every 1 mmHg increase in IOP at baseline was predictive of the presence of post-management glaucoma. Thus, patients who presented with melanoma-related increased IOP need to be monitored more closely.
This retrospective analysis has several limitations. First, this large database was gathered from data at a tertiary referral centre, which may receive advanced cases that present with greater likelihood of melanoma-related glaucoma at presentation. Additionally, treatment was based on tumour extent, infiltrative features, and presence of melanoma-related glaucoma on presentation. Iris melanoma and its treatment can both affect IOP and the susceptibility of the nerve to glaucoma. As this was an observational study, treatment was not randomized. Furthermore, differences in sample size in the no glaucoma and post-management glaucoma cohorts and among various management modalities may have led to inadequately powered analyses. Our definition of post-management glaucoma was based on an IOP cutoff, and characteristic optic nerve structural damage and functional damage by visual field testing either (1) were evaluated by glaucoma specialists outside of the Ocular Oncology Service, or (2) could not be evaluated due to media opacities obscuring the view of the fundus. IOPs were measured using Tono-Pen XL (Lombart Instrument, Inc; Norfolk, VA) or applanation tonometry. Given that 50% of those with primary open-angle glaucoma are missed by using an IOP cutoff of >21 mmHg [16] and that elevated IOP without glaucoma damage is a disease entity, it is possible that our study under- or overestimated the number of individuals with post-management glaucomatous damage. Studies by our group [6] and other centres [17, 18] evaluating melanoma-related or post-management glaucoma have used similar IOP-dependent criteria. Finally, it is possible that different types of plaque therapy may be associated with varying risks of glaucoma. While our study utilized only iodine-125 plaques, ruthenium plaques may be associated with lower radiation-induced side effects such as elevated IOP [19].
Patients with iris melanoma-related increased IOP on presentation and those that undergo plaque radiotherapy should be monitored closely for signs of post-management glaucoma, which may be associated with a more aggressive disease course [5, 6, 8, 12]. In those with post-management glaucomatous optic neuropathy or elevated IOPs, treatment with IOP-lowering medications or laser procedures should be initiated, especially given that iris melanoma tends to affect young individuals and has a favourable ocular and systemic prognosis. Incisional glaucoma surgery in an eye with active iris melanoma is an absolute contraindication to prevent egress of tumour from the eye. In an eye with regressed iris melanoma but persistent glaucoma refractory to topical therapy, laser trabeculoplasty, or laser cyclophotocoagulation, glaucoma filtration surgery can be performed after a minimum period of 6 months of tumour regression [20]. Preservation of vision by preventing the development or worsening of post-management glaucomatous optic neuropathy is an important adjunctive goal. Glaucoma specialists participating in the care of secondary glaucoma associated with all ocular tumours should work in collaboration with ocular oncologists in determining the safest treatment strategies for these complex eyes.
Summary
What was known before
-
Iris melanoma-related glaucoma has been associated with a 4.5 times increased risk of tumour metastasis. Glaucoma following the management of iris melanoma has been associated with worse ocular and systemic outcomes, related to an 11 times increased risk for melanoma recurrence.
What this study adds
-
Twenty-eight percent eyes in our cohort of 432 eyes with iris melanoma developed post-management glaucoma. We identified melanoma-related increased intraocular pressure at initial visit, advanced American Joint Committee on Cancer clinical T subcategory, increased mean tumour basal diameter, and treatment with plaque radiotherapy as risk factors for the development of post-management glaucoma in eyes with iris melanoma. Our study found a 2.3 times increased risk of post-management glaucoma following plaque radiotherapy as compared to local resection, while adjusting for various baseline characteristics, including tumour size.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology 2011;118:1881–5. https://doi.org/10.1016/j.ophtha.2011.01.040.
Shields CL, Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR, et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009;127:989–98. https://doi.org/10.1001/archophthalmol.2009.208.
Shields CL, Kaliki S, Furuta M, Mashayekhi A, Shields JA. Clinical spectrum and prognosis of uveal melanoma based on age at presentation in 8,033 cases. Retina 2012;32:1363–72. https://doi.org/10.1097/IAE.0b013e31824d09a8.
Shields CL, Shields JA, De Potter P, Singh AD, Hernandez C, Brady LW. Treatment of non-resectable malignant iris tumours with custom designed plaque radiotherapy. Br J Ophthalmol. 1995;79:306–12. https://doi.org/10.1136/bjo.79.4.306.
Shields CL, Kaliki S, Shah SU, Luo W, Furuta M, Shields JA. Iris melanoma: features and prognosis in 317 children and adults. J AAPOS. 2012;16:10–6. https://doi.org/10.1016/j.jaapos.2011.10.012.
Shields CL, Shah SU, Bianciotto CG, Emrich J, Komarnicky L, Shields JA. Iris melanoma management with iodine-125 plaque radiotherapy in 144 patients: impact of melanoma-related glaucoma on outcomes. Ophthalmology 2013;120:55–61. https://doi.org/10.1016/j.ophtha.2012.06.053.
Shields CL, Shields JA, Shields MB, Augsburger JJ. Prevalence and mechanisms of secondary intraocular pressure elevation in eyes with intraocular tumors. Ophthalmology 1987;94:839–46. https://doi.org/10.1016/s0161-6420(87)33537-7.
Shields CL, Shields JA, Materin M, Gershenbaum E, Singh AD, Smith A. Iris melanoma: risk factors for metastasis in 169 consecutive patients. Ophthalmology 2001;108:172–8. https://doi.org/10.1016/s0161-6420(00)00449-8.
Khan S, Finger PT, Yu GP, Razzaq L, Jager MJ, de Keizer RJ, et al. Clinical and pathologic characteristics of biopsy-proven iris melanoma: a multicenter international study. Arch Ophthalmol. 2012;130:57–64. https://doi.org/10.1001/archophthalmol.2011.286.
Fernandes BF, Krema H, Fulda E, Pavlin CJ, Payne DG, McGowan HD, et al. Management of iris melanomas with 125Iodine plaque radiotherapy. Am J Ophthalmol. 2010;149:70–6. https://doi.org/10.1016/j.ajo.2009.08.007.
Shields CL, Materin MA, Shields JA, Gershenbaum E, Singh AD, Smith A. Factors associated with elevated intraocular pressure in eyes with iris melanoma. Br J Ophthalmol. 2001;85:666–9. https://doi.org/10.1136/bjo.85.6.666.
Shields CL, Di Nicola M, Bekerman VP, Kaliki S, Alarcon C, Fulco E, et al. Iris melanoma outcomes based on the American Joint Committee on Cancer Classification (Eighth Edition) in 432 Patients. Ophthalmology 2018;125:913–23. https://doi.org/10.1016/j.ophtha.2017.11.040.
Kivelä T, Simpson ER, Grossniklaus HE, et al. Uveal mekanoma. In: AJCC Cancer Staging Manual. 8th ed. New York: Springer; 2017. p. 805e817.
Shields CL, Kaliki S, Hutchinson A, Nickerson S, Patel J, Kancherla S, et al. Iris nevus growth into melanoma: analysis of 1611 consecutive eyes: the ABCDEF guide. Ophthalmology 2013;120:766–72. https://doi.org/10.1016/j.ophtha.2012.09.042.
Bechrakis NE, Bornfeld N, Zoller I, Foerster MH. Iodine 125 plaque brachytherapy versus transscleral tumor resection in the treatment of large uveal melanomas. Ophthalmology 2002;109:1855–61. https://doi.org/10.1016/s0161-6420(02)01273-3.
Tielsch JM, Katz J, Singh K, Quigley HA, Gottsch JD, Javitt J, et al. A population-based evaluation of glaucoma screening: the Baltimore Eye Survey. Am J Epidemiol. 1991;134:1102–10. https://doi.org/10.1093/oxfordjournals.aje.a116013.
Kim EA, Salazar D, McCannel CA, Kamrava M, Demanes DJ, Lamb J, et al. Glaucoma after Iodine-125 Brachytherapy for Uveal melanoma: incidence and risk factors. J Glaucoma 2020;29:1–10. https://doi.org/10.1097/IJG.0000000000001393.
Puusaari I, Heikkonen J, Kivela T. Ocular complications after iodine brachytherapy for large uveal melanomas. Ophthalmology 2004;111:1768–77. https://doi.org/10.1016/j.ophtha.2004.03.027.
Karimi S, Arabi A, Shahraki T. Plaque brachytherapy in iris and iridociliary melanoma: a systematic review of efficacy and complications. J Contemp Brachytherapy. 2021;13:46–50. https://doi.org/10.5114/jcb.2021.103586.
Kaliki S, Eagle RC, Grossniklaus HE, Campbell RJ, Shields CL, Shields JA. Inadvertent implantation of aqueous tube shunts in glaucomatous eyes with unrecognized intraocular neoplasms: report of 5 cases. JAMA Ophthalmol. 2013;131:925–8. https://doi.org/10.1001/jamaophthalmol.2013.828.
Acknowledgements
Accepted for paper presentation at the Annual Meeting of the American Academy of Ophthalmology from November 13–15, 2020.
Funding
Eye Tumor Research Foundation, Philadelphia, PA (CLS) and the American Glaucoma Society’s Mentoring for the Advancement of Physician Scientists Grant (AGS). The funders had no role in the design and conduct of the study, in the collection, analysis and interpretation of the data, and in the preparation, review or approval of the manuscript. No conflicting relationship exists for any author. Aakriti G. Shukla, M.D. has had full access to all the data in the study and takes responsibility for the integrity of the data.
Author information
Authors and Affiliations
Contributions
AGS: conceptualization, methodology, writing - original draft, supervision. SV: conceptualization, methodology, formal analysis, visualization, writing -reviewing and editing. AY: conceptualization, methodology, writing-reviewing and editing. MDN: investigation, writing-reviewing and editing. SK: investigation, writing—reviewing and editing. EF: investigation, writing-reviewing and editing. JSM: writing-reviewing and editing. JAS: writing- reviewing and editing, funding acquisition. CLS: conceptualization, methodology, writing-reviewing and editing, funding acquisition, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shukla, A.G., Vaidya, S., Yaghy, A. et al. Iris melanoma: factors predictive of post-management secondary glaucoma in 271 cases at a Single Ocular Oncology Centre. Eye 37, 938–946 (2023). https://doi.org/10.1038/s41433-022-02051-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02051-0