Abstract
Background/objectives
There is an ongoing debate on whether encircling scleral buckling (SB) procedure for the treatment of rhegmatogenous retinal detachment (RRD) may cause an impairment in choroidal blood flow. The aim of this study was to compare choroidal vascularity index (CVI) and subfoveal choroidal thickness (CT) between eyes that had undergone encircling SB with unoperated fellow eyes (FEs).
Subjects/methods
Thirty patients treated with encircling SB for unilateral RRD were included. Demographic and clinical characteristics as well as enhanced depth imaging—optical coherence tomography scans were retrospectively collected. Images were binarised using ImageJ software, total choroidal area along with luminal and stromal area (respectively, TCA, LA and SA) were segmented and the CVI was computed as the ratio of LA/TCA. In addition, CT was evaluated.
Results
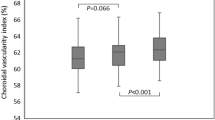
The mean follow-up interval between surgery and examination was 25.5 ± 16.8 months. Choroidal thickness, TCA, LA and SA were significantly increased in the operated eyes compared to FEs (respectively, 271.7 ± 78.0 µm vs. 238.5 ± 83.4, P = 0.001; 1.804 ± 0.491 mm2 vs. 1.616 ± 0.496, P = 0.001; 1.199 ± 0.333 mm2 vs. 1.067 ± 0.337, P < 0.001 and 0.605 ± 0.171 mm2 vs. 0.550 ± 0.171, P = 0.001). Conversely, CVI did not significantly differ between the two groups (66.4 ± 3.6 vs. 65.9 ± 3.2, P = 0.490).
Conclusions
In conclusion, eyes treated with encircling SB for RRD presented increased LA, SA and CT compared with FEs, but showed no difference in CVI.
Similar content being viewed by others
Introduction
Rhegmatogenous retinal detachment (RRD) is a sight-threatening condition caused by the passage of fluid from the vitreous cavity into the subretinal space through one or more retinal breaks, leading to the separation of the neurosensory retina from the underlying retinal pigment epithelium [1]. Encircling scleral buckling (SB) represents an effective and well-established surgical technique for the treatment of selected cases of primary or recurrent RRD. The positioning of an encircling element around the circumference of the eye provides the reduction of vitreoretinal traction and the closure of the retinal defect(s), allowing retinal re-attachment [1]. Although uncommon, complications, such as anterior and posterior segment ischaemia and serous choroidal detachment could occur postoperatively [2]. The mechanical force exerted by the encircling band induces changes in anatomical and functional parameters of the eyeball, such as axial length, anterior chamber depth and corneal biomechanics [3,4,5]. Moreover, previous studies disclosed an impaired ocular circulation, reporting post-operative changes in both choroidal and retinal blood flow [6,7,8,9,10,11,12,13,14]. These findings suggest that a subclinical ischaemia may exist in more cases than reported.
The advancements in spectral domain optical coherence tomography (SD-OCT) technology made it possible to visualise the choroidal structure in great detail, and allowed the accurate calculation of different quantitative parameters [15]. In particular, choroidal thickness (CT) has been used to investigate vascular changes after encircling SB. Although there seems to be some agreement that the encircling element affects CT, the results are somewhat contradictory [13, 16,17,18,19].
The recent introduction of binarisation algorithms on enhanced depth imaging SD-OCT (EDI SD-OCT) images allows to separately investigate the vascular and stromal choroidal components [20].
In particular, choroidal vascularity index (CVI), which is the proportion of the luminal area (LA) to the cross-sectional choroidal area, represents a novel choroidal biomarker that has been used to monitor choroidal status in several chorioretinal disorders [21,22,23,24,25]. Compared to CT, CVI seems to be less influenced by biological variables, such as axial length, intraocular pressure and diurnal variation [26].
The aim of this study was to compare CVI between eyes that had undergone encircling SB for RRD and fellow eyes (FEs), and to further investigate possible correlations with clinical parameters.
Subjects and methods
Study design and patients
This retrospective cross-sectional study included patients treated for RRD at a single tertiary referral centre (S.Orsola-Malpighi University Hospital, Bologna, Italy) between January 2016 and December 2019. The study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the local Institutional Review Board. Written informed consent was obtained from all subjects included in the study. Consecutive patients underwent uneventful SB for RRD in one eye were screened for enrolment. SB was performed by the same surgeon (PGT) in phakic patients with RRD due to single retinal break or small confluent multiple breaks without significant lens opacification. Eyes with SB were included as the study eyes and the FEs served as controls. Exclusion criteria were any previous ocular surgery except for SB in one eye, history of retinal diseases (e.g. choroidal neovascularization, diabetic retinopathy, retinal dystrophy and central serous chorioretinopathy), glaucoma, spherical equivalent ≥6 dioptres (D), anisometropia ≥1.5 D, poor image quality and missing data from medical records.
The following data were extrapolated from medical records: age, sex, preoperative status of the macula, post-operative BCVA in logMAR, postoperative fundus examination and spectral domain EDI-OCT scan.
Encircling scleral buckling procedure
A 360° limbal conjunctival peritomy incision was made and traction sutures were placed beneath the insertions of the exposed rectus muscles to facilitate positioning the globe. A 2.5 mm wide silicone band (No. 240) was passed around the circumference of the globe and beneath the rectus muscles at a distance of 14 mm from the limbus. The band was anchored with single interrupted suture with bites parallel to the limbus placed in the centre of each quadrant, the ends of the band were then joined in the opposite quadrant of the retinal break(s) with a silicone sleeve. In all cases, drainage procedure was performed by a sclerotomy just below the retinal break(s) then sutured by a single scleral stitch. Ab externo cryotherapy was done in the retinal break(s) location. In order to increase the buckling effect an adjunctive biconvex silicone 9 mm wide element (No. 279) was placed beneath the band above the retinal break(s). In all patients included, their extension ranged from 3 to 5 clock hours. The ends of the encircling silicone band were then pulled until the desired buckle effect was reached. A paracentesis was done and SF6 injection was performed 4 mm posterior to the limbus. There were no intraoperative complications. At the end of the procedure, indirect ophthalmoscopy revealed retinal re-attachment in all patients.
Image analysis
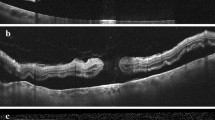
The SD-OCT scans were obtained in all patients using the Spectralis HRA-OCT (Heidelberg Engineering, Heidelberg, Germany). Each session was performed at approximately the same time of the morning, to avoid diurnal variations. Macular OCT images were acquired with EDI mode using a volume scan of 30 × 10° centred on the fovea, with 100 frames averaged in each scan. The OCT scan passing through the central foveal region was chosen for the analysis. The choroid was defined as the space between the outer border of the retinal pigment epithelium and the choroidal–scleral junction. The subfoveal CT was measured manually by two independent examiners (FB and PRR) using the caliper function tool of the image analysis software. The mean of the two measurements was used for the analysis. The OCT images were binarised and segmented by the same examiners using the public domain software ImageJ 1.51 s (National Institutes of Health, Bethesda, MD), with a semiautomated method previously described [20, 22]. Briefly, the OCT image was opened in ImageJ and the polygon tool was used to select the region of interest across the entire length of the OCT scan. The upper boundary of the region of interest was traced along the choroidal–retinal pigment epithelium junction and the lower boundary along the choroidal–scleral junction to identify the total choroidal area (TCA) (Fig. 1, part A). After conversion to an 8-bit image, Niblack’s auto local threshold was applied to binarise the image and demarcate the LA and stromal area (SA) (Fig. 1, part B). The image was converted back to a red, green, blue image, and the colour threshold tool was used to select the dark pixels, representing the LA (Fig. 1, part C). The TCA and LA were measured. The SA was calculated by subtracting LA from TCA. The CVI, defined as the LA divided by the TCA, was then computed. The choroidal parameters calculation was performed separately by two investigators, both blinded for patients’ characteristics (FB and MP), and the mean value for each parameter calculated was used for the statistical analysis.
A Choroidal boundaries are traced to identify the total choroidal area (orange lines). B The image is binarised with Niblack’s auto local threshold. C The colour threshold tool is used to select the dark pixels, representing the luminal area (yellow lines). The choroidal vascularity index is obtained dividing luminal area by total choroidal area.
Statistical analysis
The R studio software, version 1.2.5042, (http://www.r-project.org) was used for data analysis. Values are expressed as mean ± standard deviation. The Shapiro–Wilk test was used to determine the normality of data. The Student’s t-test was used to compare normally distributed continuous variables between operated eyes (OEs) and FEs, whereas the Wilcoxon signed-rank test was used for not normally distributed variables. The correlations of choroidal parameters with demographic and clinical parameters were examined using the Pearson correlation analysis with a Bonferroni correction for multiple comparisons. A P value < 0.05 was considered statistically significant.
Results
Thirty-nine patients treated with SB for RRD were initially identified. Of these, nine patients did not satisfy the inclusion/exclusion criteria and were excluded from the final analysis. In particular, two presented high myopia, three had previous eye surgery in both eyes, one had glaucoma, one was lost to follow-up and two presented poor OCT scans quality. Finally, 30 patients were enroled in the study. Mean age was 61.7 ± 6.1 years (range 51–75 years), and 19 of the patients (63.3%) were male. Eighteen patients (60%) presented macula off RRD at the time of the procedure. The mean time interval between the surgery procedure and the follow-up visit was 25.5 ± 16.8 months (range 4–59 months). Mean BCVA was 0.05 ± 0.07 logMAR in the OEs. Macular pucker was present in nine of the OEs (30%) at follow-up visit. Choroidal parameters in eyes treated with encircling SB for RRD and FEs are reported in Table 1. CT, TCA, LA and SA were significantly increased in the OEs compared with FEs (respectively, 271.7 ± 78.0 µm vs. 238.5 ± 83.4, P = 0.001; 1.804 ± 0.491 mm2 vs. 1.616 ± 0.496, P = 0.001; 1.199 ± 0.333 mm2 vs. 1.067 ± 0.337, P < 0.001 and 0.605 ± 0.171 mm2 vs. 0.550 ± 0.171, P = 0.001). On the contrary, CVI did not significantly differ between the two groups (66.4 ± 3.6% vs. 65.9 ± 3.2, P = 0.490). No significant correlations between choroidal parameters and demographical and clinical parameters, including follow-up period, were found (always P > 0.05).
Discussion
In the present study, we investigated the choroidal structure in eyes treated with encircling SB after a relatively long-term follow-up. The evaluation was made using a previously validated technique, which allows to evaluate separately the stromal and the luminal choroidal components [20]. We found that both LA and SA were increased in the OEs compared with FEs. Interestingly, the CVI, which represents the ratio of LA to TCA, was not different between the two groups, suggesting that both LA and SA increased without changing their proportions.
It has been speculated that the mechanical force exerted by encircling and buckling elements could determine a venous drainage obstruction, inducing an increased vascular resistance and thus, a decreased ocular blood flow [6]. Previous studies investigated ocular blood flow after SB procedure using different techniques, including ocular pulse measurements, bidirectional laser Doppler, laser speckle flowmetry and colour Doppler imaging, disclosing an impaired chorioretinal circulation [6,7,8,9,10,11,12,13,14]. However, mixed results on its changes over time have been reported. Some studies showed that the reduction of chorioretinal blood flow still persisted after a long-term follow-up and improved only after the removal of the encircling band [6, 9,10,11]. Our results could support this hypothesis, since the increase in LA had previously been interpreted as an indirect marker of blood flow stasis secondary to an impaired circulation [24]. Conversely, others reports showed a post-operative reduction in choroidal blood flow that returned to baseline values 3 to 6 months after surgery [12, 14]. It is difficult to compare the results of these studies because they differ in terms of surgical technique, follow-up period and measurement methods.
Recently, CT has been evaluated in patients after SB as a surrogate marker of choroidal blood flow [13, 16,17,18,19]. Previous studies indicated that segmental SB procedure, characterised by the placement of a local buckling element, induces a temporary increase of subfoveal CT that returns to baseline values from 1 to 3 months after surgery [13, 18, 19]. Conversely, the use of encircling band in addition to the local buckling element seems to lead to a long-term increase in CT [17, 27].
Several factors might be related with the development of choroidal changes, including the material of the buckling element and its extent (length, width and thickness), along with the use of cryotherapy, which can induce a post-operative inflammatory response [13, 19]. We found that OEs showed an increased CT along with a greater TCA compared with FEs. These results are consistent with Odrobina et al. who disclosed an increased CT in patients treated with a 3.5 mm encircling SB after a mean follow-up of 22 months [17]. These findings suggest that different mechanisms might occur depending on whether an encircling band has been used or not. In fact, it is reasonable to hypothesise that the presence of an encircling element may induce an impairment of choroidal circulation over a longer period of time and may reduce the possibility of choroidal tissue to return to baseline status.
The absence of change in CVI between OEs and FEs could be explained in two different ways: on the one hand, also the stromal component of the choroid might be affected by the placement of the encircling band; on the other hand, an adaptation process of the stromal tissue might occur following vascular changes. However, these hypotheses remain speculative and a prospective study is required to evaluate when stromal change occur.
Interestingly, none of the patients included presented any complication related with vascular impairment following the surgery. Moreover, all of them experienced an overall good prognosis in terms of visual acuity. According to a previous report, although an alteration of the choroidal blood flow seems to be common after encircling SB procedure, patients generally do not experience long-term visual complications. These complications could be related with an individual susceptibility or with the degree of tightness of the encircling band [6].
This study has some limitations that should be taken into account. The main limit is related to its retrospective design, which hampered the evaluation of choroidal parameters before and after encircling SB, as well as the monitoring of their trend over time. In addition, the algorithm used for the calculation of choroidal parameters does not allow the evaluation of the different choroidal layers, namely the choriocapillaris, the medium choroidal vessel layer and the large choroidal vessel layer, thus it was not possible to determine their respective degree of involvement.
In conclusion, eyes treated with encircling SB for RRD show increased luminal and SAs along with a greater choroidal area, compared to FEs. Furthermore, OEs show no difference in CVI compared to FEs, suggesting that the increase in stromal and vascular components maintained their proportion unchanged. These results support the theory that encircling SB induces subclinical changes in choroidal circulation and provide a deeper characterisation of this phenomenon.
Summary
What was known before
-
Scleral buckling procedure leads to impaired choroidal blood flow.
-
Long-term effect of encircling element on choroidal vasculature still remains unclear.
What this study adds
-
Encircling scleral buckling induces an increase in stromal and luminal choroidal area but does not affect choroidal vascularity index.
References
Park SW, Lee JJ, Lee JE. Scleral buckling in the management of rhegmatogenous retinal detachment: patient selection and perspectives. Clin Ophthalmol. 2018;12:1605–15. http://www.ncbi.nlm.nih.gov/pubmed/30214145.
Papakostas TD, Vavvas D. Postoperative complications of scleral buckling. Semin Ophthalmol. 2018;33:70–74.
Bedarkar A, Ranjan R, Khan P, Gupta RC, Kushwaha R, Mohan S. Scleral buckling-induced ocular parameter changes in different age group patients of rhegmatogenous retinal detachment. Taiwan J Ophthalmol. 2017;7:94–99. http://www.ncbi.nlm.nih.gov/pubmed/29018764.
Smiddy WE, Loupe DN, Michels RG, Enger C, Glaser BM, deBustros S. Refractive changes after scleral buckling surgery. Arch Ophthalmol. 1989;107:1469. http://www.ncbi.nlm.nih.gov/pubmed/2803094.
Taroni L, Bernabei F, Pellegrini M, Roda M, Toschi PG, Mahmoud AM, et al. Corneal biomechanical response alteration after scleral buckling surgery for rhegmatogenous retinal detachment. Am J Ophthalmol. 2020;217:49–54.
Ogasawara H, Feke GT, Yoshida A, Milbocker MT, Weiter JJ, Mcmeel JW. Retinal blood flow alterations associated with scleral buckling and encircling procedures. Br J Ophthalmol. 1992;76:275–9.
Eshita T, Shinoda K, Kimura I, Kitamura S, Ishida S, Inoue M, et al. Retinal blood flow in the macular area before and after scleral buckling procedures for rhegmatogenous retinal detachment without macular involvement. Jpn J Ophthalmol. 2004;48:358–63.
Nagahara M, Tamaki Y, Araie M, Eguchi S. Effects of scleral buckling and encircling procedures on human optic nerve head and retinochoroidal circulation. Br J Ophthalmol. 2000;84:31–36.
Yoshida A, Feke GT, Green GJ, Goger DG, Matsuhashi M, Jalkh AE, et al. Retinal circulatory changes after scleral buckling procedures. Am J Ophthalmol. 1983;95:182–8.
Ito Y, Sasoh M, Ido M, Osawa S, Wakitani Y, Uji Y. Effects of scleral buckling without encircling procedures on retrobulbar hemodynamics as measured by color doppler imaging. Arch Ophthalmol. 2005;123:950–3.
Yoshida A, Hirokawa H, Ishiko S, Ogasawara H. Ocular circulatory changes following scleral buckling procedures. Br J Ophthalmol. 1992;76:529–31.
Sugawara R, Nagaoka T, Kitaya N, Fujio N, Takahashi J, Takahashi A, et al. Choroidal blood flow in the foveal region in eyes with rhegmatogenous retinal detachment and scleral buckling procedures. Br J Ophthalmol. 2006;90:1363–5.
Iwase T, Kobayashi M, Yamamoto K, Yanagida K, Ra E, Terasaki H. Change in choroidal blood flow and choroidal morphology due to segmental scleral buckling in eyes with rhegmatogenous retinal detachment. Sci Rep. 2017;7.
Yokota H, Mori F, Nagaoka T, Sugawara R, Yoshida A. Pulsatile ocular blood flow: changes associated with scleral buckling procedures. Jpn J Ophthalmol. 2005;49:162–5.
Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147:811–5. http://www.ncbi.nlm.nih.gov/pubmed/19232559.
Montezuma SR, Tang PH, Miller CJ, Kelly A, van Kuijk FJGM, Drayna P, et al. The effect of scleral buckling surgery on choroidal thickness measured by enhanced depth optical coherence tomography: a cross-sectional study. Ophthalmol Ther. 2016;5:215–22.
Odrobina D, Laudańska-Olszewska I, Gozdek P, Maroszyński MAM. Influence of scleral buckling surgery with encircling band on subfoveal choroidal thickness in long-term observations. Biomed Res Int. 2013;2013:586894.
Miura M, Arimoto G, Tsukahara R, Nemoto R, Iwasaki T, Goto H. Choroidal thickness after scleral buckling. Ophthalmology. 2012;119:1497–8.
Kimura M, Nishimura A, Yokogawa H, Okuda T, Higashide T, Saito Y, et al. Subfoveal choroidal thickness change following segmental scleral buckling for rhegmatogenous retinal detachment. Am J Ophthalmol. 2012;154:893–900.
Agrawal R, Salman M, Tan KA, Karampelas M, Sim DA, Keane PA, et al. Choroidal vascularity index (CVI) - a novel optical coherence tomography parameter for monitoring patients with panuveitis? PLoS ONE. 2016;11.
Iovino C, Pellegrini M, Bernabei F, Borrelli E, Sacconi R, Govetto A, et al. Choroidal vascularity index: an in-depth analysis of this novel optical coherence tomography parameter. J Clin Med. 2020;9:595.
Giannaccare G, Pellegrini M, Sebastiani S, Bernabei F, Moscardelli F, Iovino C, et al. Choroidal vascularity index quantification in geographic atrophy using binarization of enhanced-depth imaging optical coherence tomographic scans. Retina. 2020;40:960–5.
Pellegrini M, Giannaccare G, Bernabei F, Moscardelli F, Schiavi C, Campos EC. Choroidal vascular changes in arteritic and nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol. 2019;205:43–49.
Pellegrini M, Veronese C, Bernabei F, Lupidi M, Cerquaglia A, Invernizzi A, et al. Choroidal vascular changes in multiple evanescent white dot syndrome. Ocul Immunol Inflamm. 2019;7:1–6.
Iovino C, Au A, Chhablani J, Parameswarappa DC, Rasheed MA, Cennamo G, et al. Choroidal anatomical alterations following photodynamic therapy for chronic central serous chorioretinopathy: a multicenter study. Am J Ophthalmol. 2020;217:104–13.
Agrawal R, Gupta P, Tan KA, Cheung CMG, Wong TY, Cheng CY. Choroidal vascularity index as a measure of vascular status of the choroid: measurements in healthy eyes from a population-based study. Sci Rep. 2016;6.
Tsen CL, Sheu SJ, Chen SC, Wu TT. Imaging analysis with optical coherence tomography angiography after primary repair of macula-off rhegmatogenous retinal detachment. Graefe’s Arch Clin Exp Ophthalmol. 2019;257:1847–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bernabei, F., Pellegrini, M., Taroni, L. et al. Choroidal vascular changes after encircling scleral buckling for rhegmatogenous retinal detachment. Eye 35, 2619–2623 (2021). https://doi.org/10.1038/s41433-020-01307-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01307-x
This article is cited by
-
Postoperative Choroidal Vascular Biomarkers in Eyes with Rhegmatogenous Retinal Detachment-Related Giant Retinal Tears
International Journal of Retina and Vitreous (2023)
-
Choroidal vascular changes in silicone oil-filled eyes after vitrectomy for rhegmatogenous retinal detachments
BMC Ophthalmology (2023)