Abstract
Study design Prospective randomised placebo-controlled clinical trial.
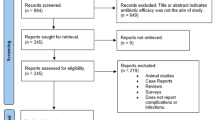
Cohort selection and data analysis Sixty-two healthy adults who underwent single dental implant placement without previous infection of the surgical bed or the need for bone grafting were included in this clinical trial. They were randomly divided into two groups (test and control). The test group was given a single dose of oral clindamycin (600 mg) one hour before surgery and the control group with a placebo. The surgical procedures were carried out by one oral surgeon and all the patients were observed post-operatively on days 1, 7, 14, 28, and 56 by a single observer for clinical, radiological, surgical variables, adverse events, and complications. Statistical analysis was performed with STATA 15 software and the number required to treat or harm (NNT/NNH) was also evaluated.
Results In the test group, the authors observed two implant failures and one patient experienced gastrointestinal disturbances and diarrhoea. They also observed post-operative infections in three patients (two in the control group and one in the test group which eventually failed).
Conclusions The authors concluded that pre-operative clindamycin administration during dental implant surgery in healthy adults may not reduce implant failure or post-surgical complications.
Similar content being viewed by others
A Commentary on
Santamaría Arrieta G, Rodríguez Sánchez F, Rodriguez-Andrés C, Barbier L, Arteagoitia I.
The effect of preoperative clindamycin in reducing early oral implant failure: a randomised placebo-controlled clinical trial. Clin Oral Investig 2022; DOI: 10.1007/s00784-022-04701-9.

GRADE rating
Commentary
Prophylactic antibiotics are commonly recommended before dental implant placement to reduce post-operative infection, risk of infective endocarditis and implant failure. Amoxicillin and amoxicillin-clavulanic acid are the most frequent choices of antibiotics prescribed to patients pre-operatively who undergo dental implant surgery.1 In patients who are allergic to amoxicillin, clindamycin has been the preferred antibiotic of choice.2 The purpose of this prospective randomised placebo-controlled clinical trial was to evaluate the effect of a single 600 mg dose of oral clindamycin administered one hour pre-operatively in reducing early implant failure and post-surgical complications in healthy adults. The study was conducted at the Dental Clinic of the Postgraduate in Oral Implantology and Microsurgery at the University of the Basque Country (Leioa, Spain). Sixty-two adult patients (22 men and 40 women, average 48.6 years of age) who needed single dental implant placement, without any previous surgical site infection or bone graft procedure, were included in the study. The participants were randomly divided into a test group and a control group (31 per group). The test group received two capsules of 300 mg (600 mg) clindamycin and the control group received two capsules of placebo one hour before surgery. All the surgical procedures were performed by a single experienced oral surgeon. All patients received the Straumann Roxolid (TI-Zr) SLActive (sand-blasted large grift acid-etched) (Basel, 4002 Switzerland) dental implants. Overall, 600 mg ibuprofen or 1 g paracetamol for every eight hours was prescribed for post-operative pain management but not more than four days. Post-operative antibiotic regimen included one tablet (875/125 mg) of amoxicillin/clavulanic acid administered every eight hours for seven days whenever needed. One of the inclusion criteria for this study was no allergies to amoxicillin/clavulanic acid; however, no allergy tests were performed on the participants.

© Malorny/Moment/Getty Images Plus
All patients were observed post-operatively on days 1, 7, 14, 28, and 56 by a single trained observer for implant failure (loss or removal of an implant). Secondary outcomes like clinical or radiographic signs indicating infection, peri-implant radiolucency, mobility, post-operative pain, and any adverse reactions were observed. STATA 15 software was used for statistical analysis of the data. In the test group, the authors observed two implant failures and one patient experienced gastrointestinal disturbances and diarrhoea. They also observed post-operative infections in three patients (two in the control group and one in the test group which eventually led to implant failure). The authors concluded that the use of pre-operative clindamycin in dental implant surgery in healthy adults may not be beneficial in reducing implant failures.
The clinical relevance and need for this study and the gap in literature has been well discussed in the introduction section of the article. The study design, patient selection, implant surgery procedures done by a single oral surgeon and post-operative observation by a single observer show that the methods used are valid and appropriate. However, the limitation of the study, as acknowledged by the authors, is the underpowering of the sample size while interpreting the clinical outcomes. The authors also acknowledge that the study participants did not undergo a penicillin allergy test and there was a possibility that some could have been allergic to penicillin. The use of post-operative antibiotic regimen of amoxicillin/clavulanic acid was not clearly explained in the materials and methods section. In the results section, it is mentioned that two of the three patients who had post-operative infections received rescue antibiotic treatment. Both the patients belonged to the control group whereas the third patient who did not receive antibiotic treatment had the implant failure. The authors also acknowledge that the intention-to-treat analysis and the use of rescue antibiotics could have masked the development of a serious infection in these two patients from the control group. The authors conclude that pre-operative clindamycin in dental implant surgery in healthy adults may not be beneficial in reducing implant failure. However, the conclusion of this study needs to be validated with further clinical research in patients who are allergic to penicillin with a stronger sample size. A recent systematic review by the same author group concluded that oral clindamycin is ineffective in preventing infection following third molar extraction surgery and that further clinical research is needed to validate the findings.3 Overall, the study is well conducted and the authors acknowledge the limitations of this study.
References
Bernabeu-Mira J C, Peñarrocha-Diago M, Peñarrocha-Oltra D. Prescription of Antibiotic Prophylaxis for Dental Implant Surgery in Healthy Patients: A Systematic Review of Survey-Based Studies. Front Pharmacol 2020; 11: 588333.
Romandini M, De Tullio I, Congedi F et al. Antibiotic prophylaxis at dental implant placement: Which is the best protocol? A systematic review and network meta-analysis. J Clin Periodontol 2019; 46: 382-395.
Arteagoitia I, Sánchez F R, Figueras A, Arroyo-Lamas N. Is clindamycin effective in preventing infectious complications after oral surgery? Systematic review and meta-analysis of randomized controlled trials. Clin Oral Investig 2022; 26: 4467-4478.
Author information
Authors and Affiliations
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Subramani, K. Does pre-operative clindamycin administration during dental implant surgery reduce implant failure or post-surgical complications?. Evid Based Dent 23, 140–141 (2022). https://doi.org/10.1038/s41432-022-0838-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-022-0838-6