Abstract
Objectives Asylum seekers and refugees (ASRs) encounter barriers when accessing oral health care (OHC). A qualitative systematic review was conducted to understand the perceptions, attitudes, behaviours and experiences of ASRs regarding their OHC. Themes were extracted to identify the barriers and facilitators ASRs face when accessing OHC.
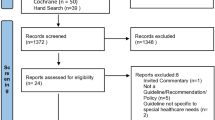
Data sources PubMed, APA PsycInfo, Cochrane Database, Web of Science and CINAHL were searched on 4 and 5 October 2022.
Data selection Primary studies including ASRs of any age or nationality were included. Qualitative data of ASRs' lived experiences of oral health (OH) and accessing OHC were extracted. The Critical Appraisal Skills Programme quality appraisal tool was applied.
Data synthesis Data findings were extracted and meta-aggregation performed using inductive reasoning. A total of 13 primary qualitative studies were included. Three barriers were identified, including difficulty accessing treatments and appointments, cultural and language changes, and ASRs' lack of OHC knowledge or incongruous beliefs surrounding OH. Two facilitators were identified as good OH education and support from care providers or government.
Conclusions Decision-makers should adapt policy to facilitate access to OHC and educate ASRs on OH. More research is needed to understand the barriers and facilitators to OHC for other people groups who experience health inequalities.
Key points
-
This review was the first to focus on the lived experience of asylum seekers and refugees in relation to oral health care access in host countries.
-
Financial support (that is, insurance-based care or complete coverage) could significantly increase oral health standards. Funds should be available for indirect costs, including transport, toothbrushes and toothpaste.
-
Collaboration between policymakers, local government and the third sector may better equip local authorities with the knowledge and tools to care for the specific needs of asylum seekers and refugees. Oral health care staff should be trained in how to tailor care, including cultural competency, communication and an understanding of care pathways and entitlements. Practices should give information in the appropriate language or provide translators.
Similar content being viewed by others
Introduction
Refugees have fled their country of origin and are unable to return due to fear of persecution because of race, religion, nationality, or association with a particular social or political group. These people have been recognised as refugees by the country they are seeking refuge in accordance with the 1952 UN Convention.1 Where an individual has fled their country but has not yet been granted refugee status they are referred to as an asylum seeker.2
Poor oral health disproportionately affects refugees.3 Oral diseases are painful, reduce quality of life, cause a loss of schooling or workdays, cause family disruption and are linked to broader social determinants of health and socioeconomic statement.4
Several factors affect the accessibility of primary health care for asylum seekers and refugees (ASRs), such as care eligibility, the cost of care, psychological social and financial stress, low availability of translators or interpreters and poor access to other areas of health (mental health and maternity care).5 They also experience inequalities in health outcomes.6
ASRs are vulnerable to poor oral health care (OHC),7 with poor access to OHC services and a wide prevalence of oral disease. Newly arrived ASRs and their children often suffer from poorer OHC than ASRs that have been in the host country longer,8 suggesting barriers to OHC may weaken over time.
This review will aim to explore and synthesise the existing evidence regarding ASRs perceptions, attitudes, behaviours and experiences when accessing OHC.
Methods
Prior to conducting the systematic review, a rapid scoping search was conducted to identify the narrative on ASR oral health (OH) and identify keywords from the existing literature.
Where applicable, this was set out according to the PRISMA 2020 framework, and the Joanna Briggs Institute protocol for qualitative systematic reviews was followed.9
Search strategy
The search terms were ((Refugee*) OR (Asylum*)) AND ((Oral*) OR (Dent*)). Boolean operators were changed according to the requirements of each database. Using the advanced search function, five databases across different scientific faculties were searched: CINAHL, Web of Science, APA PsycInfo via Ovid, PubMed and Cochrane Database. This search was conducted on 4 and 5 October 2022. A broad search, with no geographical or temporal restrictions, was applied to allow identification of variation across countries and time periods. No language restrictions were applied.
Eligibility
Participants
-
Refugees: people who have fled their home country and been recognised as refugees by the country they are seeking refuge
-
Asylum seekers: people who have fled their country but have not yet been granted this refugee status.
Any ASRs meeting the above definitions, at any stage of their resettlement journey, with no restrictions, were included in this study. Where ‘migrants' or ‘displaced person' were used, full texts of the papers were read to ascertain whether the participants were ASRs. Any relevant papers with mixed data of ASRs and other groups of vulnerable persons, such as migrants, were included but only the data regarding ASRs were analysed.
Phenomena of interest
This review focused on the barriers and facilitators of OHC access. It considered the experiences, beliefs and perspectives of ASRs and looked at individual, systemic and institutional factors that affected OH and OHC.
Context and types of studies
Any type of primary study was included. Secondary data-based studies including, but not limited to, systematic reviews or protocols were excluded. However, their reference sections were scrutinised and any additional relevant papers added to the process. Only studies with qualitative data were included. Papers with mixed quantitative and qualitative data where the qualitative data were accessible and relevant were included.
Quality appraisal of selected studies
Quality appraisal using the Critical Appraisal Skills Programme checklist10 was undertaken by two reviewers (NW, OP) independently and discrepancies were discussed and resolved.
Extraction of data
Study characteristics were extracted by NW, including authors, title, publication year, study aim, hosting country, number of participants, method of primary data retrieval and the study setting. Data relevant to the phenomenon of interest were extracted from the finalised papers and presented as originally published.
Data synthesis and analysis
Meta-aggregation was used to synthesise the extracted qualitative data. This approach is grounded in pragmaticism and transcendental phenomenology.11 All data were considered and findings and papers were coded through repeated reading of the full text. Findings were further grouped into themes through the identification of similar concepts. A subset of papers was analysed by OP and compared to ensure consistency and validity of the themes identified.
Results
After removing duplicates, the search yielded 1,477 titles; however, only 13 met the inclusion criteria (Fig. 1).
Included studies
All 13 included studies were published between 2009 and 2021. In total, 417 participants were included. All studies presented qualitative data and used interviews, focus groups or both. Four studies occurred in Canada,12,13,14,15 five in Australia,16,17,18,19,20 one in Germany,21 one in Turkey,22 one in the UK23 and one in the USA.24 The studies occurred across various settings, including community centres, mobile dental clinics and online. Three studies included only female ASRs, two of which explored parental perceptions of their children's OH,16,22with the other exploring pregnant women's access to OHC.20 One paper utilised mixed methods, but only the qualitative data were extracted (see online Supplementary Information).22
Methodological quality of included studies
The 13 studies included in this review were of good methodological quality, with 10/13 scoring at least 9/10.10 All papers had appropriate aims, methodology and research design. The full quality appraisal table can be found in the online Supplementary Information.
Thematic analysis
From the included papers, five themes (three barriers and two facilitators) emerged. These were composed of eight barrier sub-themes and four facilitator subthemes (see Figure 2). Many of the findings were unequivocal, while others occasionally acted as both barriers and facilitators, depending on the individual's experience. Quotations supporting each sub-theme can be found in the online Supplementary Information.
Barrier 1: accessing effective OHC provision is difficult for ASRs
The direct and indirect costs of accessing dental health care and maintaining good OH acted as a barrier (Theme 1.1). ASRs expressed an inability to pay for care and treatment,12,20,21 often resulting in reduced or no care.13 This was reinforced by insufficient governmental finance schemes13 and health insurance.15,19 Many ASRs were willing to or had sought overseas dental care, often in their country of origin. Paying for the flight and the care transnationally was perceived to be cheaper, and people favoured health care professionals they already know and speak the same language as.13,15,20
Indirect monetary costs of care were also a barrier in seeking OHC. These included an inability to afford OH tools (for example, toothbrushes)17,22 transport costs (often public), time off work, child carers21 and fresh food (versus sugary alternatives).16
ASRs found that dental practices had poor availability (Theme 1.2). Dental practices often ran at capacity17 with long waiting times, which lead to non-attendance.13,15,19,20ASRs described appointment-making as excessively difficult and bureaucratic20 and transportation to and from appointments insufficient or non-existent.19 Appointments were often during working hours and inflexible.21
OH providers and the institutions that support them were viewed as unhelpful and sometimes inadequate (Theme 1.3). ASRs complained of unfair treatment due to their background or refugee status21 and poor communication between themselves and service providers. Training for staff concerning how to treat ASRs effectively, kindly, and how to present their rights to care and funding where applicable, was often lacking.17,20 This resulted in mixed messages regarding ASRs' care, entitlements and eligibility, with ASRs having little say in their care.16,20,21
Barrier 2: cultural changes and acculturation affect OH and inhibit effective care
This barrier demonstrates how OHC practices and cultural beliefs from home countries can clash with the norms and values of the new hosting culture (Theme 2.1). Considering previous trauma and other resettlement priorities, such as housing, food and education, caring for one's teeth was often not a priority for ASRs until they felt safe and settled.17,18,21
Toothbrushing and other OH practices may be unfamiliar for ASRs and their children.16 Parents may not see OHC as necessary for their children and this merging and imparting of ‘Western' culture can feel threatening, creating a mismatch of practices and values in individuals and families.19
Language differences and insufficiencies exacerbated the adverse effects of cultural assimilation (Theme 2.2). A lack of translators and interpreters was frequently reported.13,17 This communication challenge was described throughout the OHC journey: understanding the ask,15 form completion,13 informed consent and post-treatment follow-up needs.21 Follow-up needs communication can lead to dentists misunderstanding the issue, which can lead to incorrect treatments and misinformation.21 This leads to feelings of being misunderstood and humiliated by OHC providers.15
Barrier 3: ASR behaviours, perceptions and knowledge modulate OHC
Individuals having their own behaviours, practices, beliefs, perceptions and knowledge of OH and OHC acted as barriers to care. This does not force blame onto ASRs, rather it acknowledges the importance of understanding the factors that may negatively impact their health. That is that ASRs may unknowingly put themselves at increased need of OHC through changes in behaviours, that is, that OHC access is directly related to OHC need.
Numerous behaviours and traditions that ASRs practise affected their OH (Theme 3.1). OHC was not routinely prioritised15 and there was poor attendance at routine check-ups, perhaps due to differing ‘cultural perceptions of time'.15,21
Drinks consumed by ASRs varied. Some perceived the tap water in their host country to be ‘dirty', which led to people consuming soft drinks and juices regularly.16,17 Other ASRs filtered their tap water or added cordial to improve the taste,17 with little understanding of fluoridation.16
An increase in sugar in everyday foods and an increased availability of sugary sweets was cited as problematic.24 Low-sugar foods were harder to access and high-sugar foods were perceived as tastier and more nutritious.16,21 Mothers also often struggled not to give their children sugary foods during the weaning process. This included giving children juices or sugar mixed with water as alternatives to formula.17
Smoking, drug use and hazardous behaviours that impact the teeth were also a barrier to good OH. Smoking ‘chelam' and sucking ‘naswar' were referenced as traditional tobacco agents that affect the teeth.18 Other behaviours included ‘breaking nuts' with their teeth and chewing ‘khat leaves',24 which are bitter and so often drank with sweetened tea.24 The stress of fleeing their home country often leads to chronically dry mouths and the conflict, persecution or torture that may have occurred previously can leave ASRs with severely damaged and missing teeth.18
Further, multiple traditional cleaning sticks from plants were referenced, including ‘aday' and ‘miswak'.16,17,18,24 These trusted tools were used regularly for prayer ablution and ASRs had cultural attachments to them. ASRs even froze or imported these plants so they can be used for longer.21 Other substances used for OHC included bicarbonate soda, sage and carnation flowers.16 ‘Takhak', aspirin, saltwater, antiseptics, cloves, ‘derum' bark, the spice blend ‘berbere' and garlic were also used to treat pain or bad breath.13,18,21,24
Poor understanding of determinants of OH acted as a barrier to preventative OHC (Theme 3.2). ASRs lacked knowledge on the causes of oral diseases and sometimes had false beliefs on the causes of poor OH.12 This was intertwined with poor education on OH.18 Mothers had a knowledge gap concerning their children's OH and the causes of caries.16,20 Further, a lack of understanding of OH terminology caused confusion.16,20 ASRs tended to seek information from family members, information which may not be reliable and can lead to further confusion.14,15
This lack of education was exacerbated by low rates of help-seeking.19 For example, help-seeking for oral caries only appeared to occur when there was a problem12 or pain,14,18,19 the latter of which was consistently the main driver for dental consultations. This lack of routine care may suggest insufficient preventative dental behaviours, meaning problems were discovered when it was already too late.
ASRs had negative and incongruous beliefs and perceptions surrounding OHC (Theme 3.3), often manifesting as fear. Many ASRs avoided seeking dental care and treatment due to fear, past experiences of pain,21 or lingering pain after a procedure.24 Fears also extended to their safety during dental care, especially in pregnant people20 and for some in whom it was triggering of prior dental torture.17
Associated with this fear was a lack of trust in the system, the motivations of dentists and the efficacy of local methods and tools.21 There was a sense of loss in their locus of control over their own and their children's OHC.14,16
Facilitator 1: positive drivers for individuals seeking and achieving good OH
This theme explored the factors that drive effective help-seeking.
Understanding the importance of OH was a prominent facilitator (Theme 4.1), enabling help-seeking and good OH practice.13 An appreciation of OH and its association with general health, knowledge of the causes of poor OH, what good OH is and how to maintain it were all beneficial.12,16,21
Teaching of OH practices and its importance in schools, in addition to a greater knowledge of English language, often resulted in younger ASRs having better OH and more effective OH practices.19 Promotion and education of OH were also effective through GP surgeries and community centres.14 Although pain was often caused by caries, it can increase engagement with OHC as ASRs acknowledged the issue, sought help, and changed their behaviour post-treatment.19
Social influence in the form of conforming to peers, acculturation and faith-related influence all facilitated good OH (Theme 4.2). ASRs may conform to ‘Western' beauty standards and seek care for themselves or their children in order to have straight, white and healthy teeth.21 There was a desire to be attractive17 and a belief that conforming to these physical standards increased employment prospects.12 Maintaining good OH also occurred through faith-based promotion, for example, Islam encourages teeth cleaning before every prayer.19
Facilitator 2: effective, accessible services and institutions lead to thriving OH.
This theme acknowledged the positive effect that care providers, communities and government schemes had on ASRs OHC when they work effectively.
Health care providers can be important facilitators for ASRs accessing OHC (Theme 5.1). Supplying helpful information on finding clinics, transportation, providing information in the ASRs' first language/providing interpreters and making appointments accessible greatly increased care satisfaction and high-quality, personalised care.15,17 Compassionate, kind and informative staff also increased care quality, calming ASRs' fears concerning OH, thus increasing their trust in the care provided.15 This contributed to positive perceptions of dentists and care providers21 and positive experiences encouraged individuals to bring other ASRs to seek care at that practice.21 Educating midwives and doctors on ASRs' OHC access was also important.15,16
Wider support was a powerful facilitator for accessing effective care (Theme 5.2). Community members supported one another, shared information and acted as interpreters during dental consultations.19 Health professionals also translated and distributed information on OH and how to access care.20 Organisations collaborating to share information made it easier for ASRs to access care.17 Financial support from governments enabled some access to OHC for ASRs, which may otherwise be inaccessible.15
Discussion
This systematic review identified three barriers and two facilitators to ASRs' OH and OHC access. No significant variations between the barriers or facilitators identified from the papers were due to the country of origin, the year of study, or the setting.
This review is unique to others in terms of the phenomenon of interest and approach taken. It both supports and contrasts the current literature on ASRs' OHC. Synonymous to the findings of this review, Paisi et al.25 identified several barriers to OHC access for ASRs, including the unaffordability of care, communication difficulties, poor knowledge of OHC and poor experiences. The need for the diversity of the ASR population to be recognised and for cultural competency to be implemented into care services is clear.25 Other reviews and primary studies also support the current findings, identifying some of the same barriers and facilitators to care.26,27,28,29
However, a review conducted by Batra et al.30 identified that some barriers varied with country of origin. Although this discrepancy may be genuine, it could also be attributed to the inclusion of migrants, who may have different OH experiences and barriers than ASRs - the focus of the current review.
Intervention-based papers conducted by Reza et al.8 and Keboa et al.3 employed education courses to increase knowledge of OHC, the effect of targeting newcomers after arrival, trialling mobile dental clinics and community-based interventions. These were found to be helpful in improving the OH status of ASRs.3,8 The aim of many of the interventions trialled are based on facilitators that this study identifies or resolve barriers to care.
A number of prior studies have attempted to devise frameworks for access;31 however, our review suggests that the needs of ASRs were related to a much smaller number of more nuanced factors. This review identified factors that previous reviews have not considered in depth. Papers acknowledge that traditional beliefs and cultural differences affect OHC; however, none have yet identified the role of acculturation in both motivating and inhibiting OHC. On one hand, it can be confusing and can create incorrect beliefs surrounding OHC. On the other hand, assimilation and social influence can lead to a shift in priorities, encouraging good oral hygiene and regular dental appointments. It is important to understand these issues so tailored practice and policy can be implemented to sustain good OH behaviours.
A strength of this review is that the included studies generally had high methodological quality. Further, title, abstract and full-text screening, as well as quality appraisal, were conducted by two independent reviewers, decreasing the chance of bias. However, four papers that got through title and abstract screening were not available at the full-text screening stage, indicating there is potential data that may have been missed, which may have altered the findings of this review.
The potential limitation of this review is the combining of all ASRs at all stages of their resettlement journey. This was necessary in part because of the paucity of published literature on the topic and because many manuscripts did not separate AS and Rs and journey stage. In reality, this had likely had a limited impact, as all studies were conducted in Western countries and likely reflected final destinations. A common limitation of qualitative systematic reviews is that they can only include what has been presented by prior authors where minor themes may have been omitted from the final published manuscripts. We have tried to mitigate the impacts of this by including a wide range of study designs and by coding the manuscripts rather than reliance on the previously identified themes. Furthermore, due to the subjective nature of qualitative research, there was a risk of undue researcher influence on the findings. This was mitigated as far as possible by utilising an established methodology, dual independent coding and transparency of conflicts of interest.
This review only explored the experiences of ASRs, so findings may not be generalised to migrants or other vulnerable persons. Additionally, it was unclear in the literature who was an ASR or a migrant as per the definition. Further, the two main hosting countries in this review were Australia and Canada, but many refugees settle in developing countries, where facilitators and barriers to OHC may differ. Turkey and Pakistan host more refugees than all EU countries combined;2 however, research is difficult in developing countries, especially in camps. Finally, the timing of this review means that the impacts on Ukrainian refugees following the war starting in 2022 were not included. The barriers to OHC experienced by Ukrainian refugees may differ to those faced by ASRs from the Middle East, which may not yet be reflected in the literature. This is an avenue for future research.
The findings from this review identify a need for OHC staff to be trained in how to tailor care for ASRs, including cultural competency, clear communication and an understanding of care pathways and entitlements.17,20 Practices should give information in the ASRs' language or provide translators and give clear information about finance and appointment timings. Together, this can reduce confusion and increase attendance, care satisfaction compliance and trust.15,17
Given that ASRs are protected by international law and cannot be deported to their country of origin,32 host countries cannot ignore them. ASRs encounter uniquely complex health needs, which are determined by their health on leaving their country of origin, modulators during transit and adapting to the host country.33 Taking this into consideration, authorities could integrate OHC for ASRs with other physical/mental health offers, as many barriers and facilitators likely carry over. For example, advertisements in the locality of large populations of ASRs, which explain where, why and how to access oral and other health care. Recommendations should be made to dental practices so they are easier to access and local or mobile clinics specifically for ASRs could be implemented to meet the demand for OHC and other needs.
Finally, if provided, financial support in the form of insurance-based care or complete coverage could significantly increase OH standards. This is an obvious approach to reducing inequalities.15 Furthermore, providing support to ASRs to aid housing, nutrition and employment so that resettlement priorities shift from the basic requirements of living to integrating into society and thriving could further improve OH. Implementing these changes may reduce barriers to care while facilitating greater access and maintenance of oral and general health.
Conclusion
This review provides a greater understanding of a complex yet important issue and contributes to the wider discussion on reducing health inequalities. It also acts as a springboard for future research on ASRs' access to OHC.
References
British Medical Association. Who are refugees or asylum seekers? 2023. Available at https://www.bma.org.uk/advice-and-support/ethics/refugees-overseas-visitors-and-vulnerable-migrants/refugee-and-asylum-seeker-patient-health-toolkit/who-are-refugees-or-asylum-seekers (accessed March 2024).
Amnesty International. Refugees, asylum seekers and migrants. 2024. Available at https://www.amnesty.org/en/what-we-do/refugees-asylum-seekers-and-migrants/#definitions (accessed March 2024).
Keboa M T, Hiles N, Macdonald M E. The oral health of refugees and asylum seekers: a scoping review. Global Health 2016; 12: 59.
Peres M A, Macpherson L M, Weyant R J et al. Oral diseases: a global public health challenge. Lancet 2019; 394: 249-260.
Spike E A, Smith M M, Harris M F. Access to primary health care services by community-based asylum seekers. Med J Aust 2011; 195:188-191.
Watt R G, Venturelli R, Daly B. Understanding and tackling oral health inequalities in vulnerable adult populations: from the margins to the mainstream. Br Dent J 2019; 227: 49-54.
UK Government. Inequalities in oral health in England. 2021. Available at https://www.gov.uk/government/publications/inequalities-in-oral-health-in-england (accessed March 2024).
Reza M, Amin M S, Sgro A et al. Oral health status of immigrant and refugee children in North America: a scoping review. J Can Dent Assoc 2016; 82: 3.
Lockwood C, Porritt K, Munn Z et al. Chapter 2: Systematic reviews of qualitative evidence. In Aromataris E, Munn Z (eds) JBI Manual for Evidence Synthesis. JBI, 2020.
Critical Appraisal Skills Programme. CASP Checklists. Available at https://casp-uk.net/checklists/casp-qualitative-studies-checklist-fillable.pdf (accessed March 2024).
Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc 2015; 13: 179-187.
Keboa M, Nicolau B, Hovey R et al. A qualitative study on the health of humanitarian migrants in Canada. Community Dent Health 2019; 36: 95-100.
Nurelhuda N M, Keboa M T, Lawrence H P, Nicolau B, Macdonald M E. Advancing our understanding of dental care pathways of refugees and asylum seekers in Canada: a qualitative study. Int J Environ Res Public Health 2021; 18: 8874.
Prowse S, Schroth R J, Wilson A et al. Diversity considerations for promoting early childhood oral health: a pilot study. Int J Dent 2014; 2014: 175084.
Keboa M T, Hovey R, Nicolau B, Esfandiari S, Carnevale F, Macdonald M E. Oral healthcare experiences of humanitarian migrants in Montreal, Canada. Can J Public Health 2019; 110: 453-461.
Riggs E, Gibbs L, Kilpatrick N et al. Breaking down the barriers: a qualitative study to understand child oral health in refugee and migrant communities in Australia. Ethn Health 2015; 20: 241-257.
Nicol P, Al-Hanbali A, King N, Slack-Smith L, Cherian S. Informing a culturally appropriate approach to oral health and dental care for pre-school refugee children: a community participatory study. BMC Oral Health 2014; 14: 69.
Lamb C E, Michaels C, Whelan A K. Refugees and oral health: lessons learned from stories of Hazara refugees. Aust Health Rev 2009; 33: 618-627.
Due C, Aldam I, Ziersch A. Understanding oral health help-seeking among Middle Eastern refugees and asylum seekers in Australia: An exploratory study. Community Dent Oral Epidemiol 2020; 48: 188-194.
Riggs E, Yelland J, Shankumar R, Kilpatrick N. ‘We are all scared for the baby': promoting access to dental services for refugee background women during pregnancy. BMC Pregnancy Childbirth 2016; 16: 12.
Kidane Y S, Ziegler S, Keck V et al. Eritrean Refugees' and Asylum-Seekers' Attitude towards and Access to Oral Healthcare in Heidelberg, Germany: A Qualitative Study. Int J Environ Res Public Health 2021; 18: 11559.
Pani S C, Al-Sibai S A, Rao A S, Kazimoglu S N, Mosadomi H A. Parental perception of oral health-related quality of life of Syrian refugee children. J Int Soc Prevent Community Dent 2017; 7: 191-196.
Kang C, Tomkow L, Farrington R. Access to primary health care for asylum seekers and refugees: a qualitative study of service user experiences in the UK. Br J Gen Pract 2019; 69: 537-545.
Adams M J, Young M S, Laird L D et al. The cultural basis for oral health practices among Somali refugees pre- and post-resettlement in Massachusetts. J Health Care Poor Underserved 2013; 24: 1474-1485.
Paisi M, Baines R, Burns L et al. Barriers and facilitators to dental care access among asylum seekers and refugees in highly developed countries: a systematic review. BMC Oral Health 2020; 20: 337.
Bhusari S, Ilechukwu C, Elwishahy A, Horstick O, Winkler V, Antia K. Dental caries among refugees in Europe: a systematic literature review. Int J Environ Res Public Health 2020; 17: 9510.
Amin M S, Elyasi M, Schroth R J et al. Improving the oral health of young children of newcomer families: a forum for community members, researchers, and policy-makers. J Can Dent Assoc 2014; 80: 64.
Riggs E, Rajan S, Casey S, Kilpatrick N. Refugee child oral health. Oral Dis 2017; 23: 292-299.
Paisi M, Baines R, Wheat H et al. Factors affecting oral health care for asylum seekers and refugees in England: a qualitative study of key stakeholders' perspectives and experiences. Br Dent J 2022; DOI: 10.1038/s41415-022-4340-5.
Batra M, Gupta S, Erbas B. Oral health beliefs, attitudes, and practices of South Asian migrants: A systematic review. Int J Environ Res Public Health 2019; 16: 1952.
Levesque J-F, Harris M F, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health 2013; 12: 18.
UN Refugee Agency. ‘Refugee' vs ‘migrant' - Which is right?2015. Available at https://www.unrefugees.org/news/refugee-or-migrant-which-is-right/ (accessed March 2024).
British Medical Association. Unique health challenges for refugees and asylum seekers.2023.Available at https://www.bma.org.uk/advice-and-support/ethics/refugees-overseas-visitors-and-vulnerable-migrants/refugee-and-asylum-seeker-patient-health-toolkit/unique-health-challenges-for-refugees-and-asylum-seekers (accessed March 2024).
Author information
Authors and Affiliations
Contributions
The primary author, Nathan E. Wainman, completed the literature search and screening process and wrote the first draft of the manuscript, with revisions from Olivia R. Phillips and Joanne R. Morling. Olivia R. Phillips also aided with the screening process.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
The Ethics Committee of the Faculty of Medicine and Health Sciences, University of Nottingham advised that approval from the ethics committee was not required for systematic review studies due to the use of existing published data.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Supplementary Information
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2024
About this article
Cite this article
Wainman, N., Phillips, O. & Morling, J. Facilitators and barriers to asylum seeker and refugee oral health care access: a qualitative systematic review. Br Dent J (2024). https://doi.org/10.1038/s41415-024-7235-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-024-7235-9