Abstract
Introduction Team-based learning (TBL) is a dialectic, student-focused method of teaching which has become increasingly popular in international institutions for delivering undergraduate dental education. Despite several dental schools in the UK using dialectic teaching methods, such as problem-based learning, none appear to use TBL.
Aims This scoping review aims to identify the literature investigating the use of TBL compared with other teaching pedagogies in delivering undergraduate dental education.
Methods The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guidelines were adopted. A search strategy was developed using appropriate MeSH (medical subject headings) terms and key words. Medline, Scopus and the Cochrane Databases were searched.
Results Overall, five studies were identified for inclusion. Of these, three studies compared TBL to traditional, didactic teaching methods (such as lectures) and found both student satisfaction and student performance to be greater with TBL. The remaining two studies compared TBL to other dialectic methods of teaching. The results on student performance in these studies were conflicting.
Conclusions There is some limited but promising evidence that TBL is effective at delivering undergraduate dental education; however, the scarcity of research evidence highlights the need for more robust exploration.
Key points
-
There is some evidence that team-based learning used to deliver undergraduate dental education leads to improved student satisfaction and student performance compared to traditional, didactic methods of teaching.
-
There is limited research evidence comparing team-based learning to other dialectic methods of teaching in undergraduate dentistry.
-
More robust research is required to explore the effectiveness of team-based learning in undergraduate dental education compared to other dialectic methods of teaching.
Similar content being viewed by others
Introduction
Traditionally, healthcare pedagogy has been delivered using didactic methods of teaching, centred on the transfer of information from teachers to students (usually in the form of lectures). However, for several decades now, there have been strong calls from both the medical and dental world encouraging transformation and placing the onus of learning on students themselves.1,2 Our healthcare environments today require professionals that are not only competent but are also able to work effectively in interprofessional teams to help deliver high-quality, cost-effective patient care. The widespread availability and use of the internet and digital platforms has revolutionised the progression and dissemination of medical and dental research findings, and our healthcare professionals must now be equipped with the ability to problem solve, critically appraise information, and where possible, ensure they are providing care which is supported by research evidence.1,3 To this effect, we have witnessed a paradigm shift in dental education methods, with learner-centred models, such as problem-based learning (PBL), enquiry-based learning (EBL) and case-based learning (CBL), being introduced.4,5,6,7,8,9An overview of these three pedagogies is outlined in Table 1. While there are numerous similarities between these three pedagogies, there are also subtle differences.10,11,12,13,14 Within the UK, several universities have deployed PBL and EBL teaching methods to aid the delivery of their undergraduate dental curriculums.6,15,16,17 These dialectic methods are fundamentally based on the use of small groups (typically 5-8 students together with a facilitator), to address theoretical and clinical topics, generally supported by appropriately selected clinical cases. Students approach these through a combination of enquiry, independent study, discussion and debate.17 The overall aim is a far more interactive and dynamic form of learning; when compared to lecture-based teaching, PBL, EBL and CBL are active rather than passive educational approaches to teaching. However, despite the perceived advantages of these methods,18,19 they require a relatively high number of facilitators and a large number of small rooms to accommodate groups, which in itself can present a logistical challenge to educational institutions.19 Furthermore, there can be issues with educational quality standardisation, as there may be variation in the ability of small groups to interpret clinical cases and adequately identify the intended learning objectives.19,20 Scenarios can arise where groups learn vastly different content, especially if the facilitator is not adequately trained to guide discussions.19,20 To address some of these drawbacks, attention has now been drawn to an alternative learner-centred teaching model known as team-based learning (TBL).21,22
TBL involves large group classes (which can be several hundred students) divided into smaller teams (typically 5-7), together with a smaller number of facilitators (typically 2-3).21,22 Prior to the session, students are expected to complete pre-reading in preparation for an assessment known as the individual readiness assurance test (iRAT).21,22 This is often in the form of a multiple-choice assessment and is used to evaluate concepts learnt in the pre-reading material. Following completion of the iRAT, the students convene in their allocated teams and answer the questions together in a team/group readiness assurance test (tRAT/gRAT).21,22 Subsequently, the teams are presented with real-life problem scenarios with multiple solutions, which they are able to discuss, rationalise and problem-solve together before the teams are able to debate the solutions that they have synthesised. The final step in the TBL process is peer review, whereby students provide feedback to each other, including their ability to work effectively in a team.21,22 The process of TBL is summarised in Figure 1.
In recent years, TBL has gained popularity in medical education, and there is now evidence emerging that students favour this over methods such as PBL.23 There are studies which have found that medical students prefer the structure and format of TBL sessions and feel these to be more conducive to learning, engagement and participation when compared to PBL.23,24 A recent systematic review exploring the impact of TBL among healthcare professionals found evidence that academic performance was significantly improved among TBL groups when compared to lecture-based teaching groups.25 While the evidence to date supporting the use of TBL in healthcare education is promising, much of this research has been based on the use of TBL in the development of medical, nursing and allied healthcare professionals.25,26,27As such, there is a real need to determine the effectiveness of TBL in delivering undergraduate dental education. The aim of this scoping review is to:
-
Evaluate the current research exploring the effectiveness of TBL versus other teaching pedagogies in delivering undergraduate dental education
-
Identify the strengths and weaknesses within the current evidence base
-
Stimulate discussion on the suitability of TBL in delivering undergraduate dental education within the UK.
Methods
Information sources and search
Scoping reviews provide an ideal tool for determining the nature of literature available in a particular subject area.28 As such, this was the most appropriate research methodology for addressing the objectives of this study. This scoping review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews guidelines.29 The following electronic databases were searched: Medline, Cochrane and Scopus (May 2023). The review was limited to literature published from inception through to 2 May 2023. Two reviewers (BJT and HJ) searched the databases using the MeSH (medical subject headings) terms and key words ‘dentistry' OR ‘dental' AND ‘team-based learning' OR ‘TBL' OR ‘iRAT' OR ‘tRAT'.
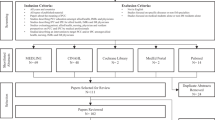
Inclusion criteria
-
Articles written in the English language
-
Dentistry at undergraduate level (any year of study)
-
Studies comparing TBL with any other form of teaching pedagogy.
Exclusion criteria
-
Articles written in any language other than English
-
Studies focusing on postgraduate courses
-
Studies where TBL was not compared to another form of teaching pedagogy.
Screening and data collection
Assessment and screening of studies was completed independently by three authors (BJT, BP and HJ).30 A selection protocol based on the inclusion/exclusion criteria of the review was designed and piloted on the first 50 studies returned from the electronic database search. This was designed and used to provide a consistent method for selecting studies that appropriately addressed the objectives of this study. The selected articles had their full text read by two authors (BJT and HJ) and were assessed for final inclusion. Any discrepancies were planned for resolution through discussion and involvement of a third author (RVR). The reference lists of all included articles were researched for any additional relevant articles.
A data collection sheet was developed using the guidelines described by Free et. al.31 and piloted before implementation. The characteristics and findings of all the studies included in the review were extracted using the data collection sheet. This was conducted independently and in duplicate by two authors (BJT and HJ). Ethical approval was not required because this study retrieved and synthesised data from previously published studies.
Results
Selection and characteristics of source of evidence
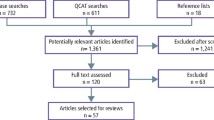
The electronic database searches yielded a total of 780 articles. Following removal of duplicates, 406 articles were returned. Following initial title and abstract screening, 375 articles were removed. A total of 31 full-text articles were reviewed with the eligibility criteria and 26 excluded. In total, five studies were included in this scoping review.32,33,34,35,36 The PRISMA diagram in Figure 2 provides a summary of the selection process.
The included studies are summarised in Table 2. They were conducted in the USA32,33 (n = 2), Japan35,36 (n = 2) and Saudi Arabia (n = 1).34 The effectiveness of TBL in teaching prosthodontics was assessed in three studies,32,35,36 while one study focused on the teaching of oral and systemic topics.33 In one of the studies, it was unclear which discipline of dentistry was being taught.34 Of the selected studies, three compared TBL to traditional methods (lectures),32,34,36 one compared TBL to case-based learning,33 and one compared TBL to flipped classroom (flipped classroom is a blended approach where the student watches a series of videos or digital media before attending a class or workshop).35,37
Although the studies used different outcomes to assess the effectiveness of TBL versus other teaching pedagogies, these outcomes were largely found to fall into two main themes, namely, student satisfaction/perception and examination performance. In four of the studies, examination performance was found to be significantly better in favour of TBL,32,33,34,36 while one study found no statistically significant difference between material taught using TBL versus the flipped classroom method.35
Student perception of TBL was assessed in two of the studies,34,36 both of which found TBL to be perceived more favourably than traditional, lecture-based approaches. Student satisfaction was assessed in a single study which compared TBL with CBL and found student satisfaction to be higher in CBL.33
Discussion
To our knowledge, this is the first scoping review of the literature that has investigated the use of TBL in undergraduate dental education. TBL has gained popularity as a teaching method in allied health professions25 and this review has found some evidence that TBL is gradually being used as a teaching pedagogy in undergraduate dental education. While five studies were identified for inclusion,32,33,34,35,36 there was substantial heterogeneity in both study design and data analysis, which makes direct comparison of the data from each of these studies difficult. Furthermore, the sample size of most of these studies was relatively small and the teaching was limited to isolated, short dental courses, which limits extrapolation of these findings to a full undergraduate dental curriculum.
The results of the studies included in this review suggest that TBL in undergraduate dental education leads to improved student performance when compared to traditional, lecture-based approaches,32,34,36 but there is limited evidence comparing the effectiveness of TBL versus other constructivist-focused pedagogy, such as CBL, PBL or EBL. There were two studies which compared active constructivist approaches, specifically TBL with CBL,33 and TBL with flipped classroom.35 The results of these studies in relation to student performance were conflicting. Where TBL was compared to CBL, the authors reported a statistically significant (p = 0.046) improvement in student performance with TBL.33 However, on close examination, it is clear that this difference is minimal (86% vs 83%) and therefore unlikely to be consequential.33 Where TBL was compared to the flipped classroom approach, there was no significant difference found in examination performance (p = 0.848).35 As such, based on the current evidence to date, we cannot draw any robust conclusions regarding the impact of TBL on student performance when compared to other constructivist teaching pedagogies in undergraduate dental education.
Based on the studies identified for inclusion in the review, it appears that student satisfaction was perceived to be higher for TBL when compared to traditional lecture-based approaches34,36 but inferior when compared to another constructivist learning approach (CBL).33 The single study which compared two constructivist approaches (TBL vs CBL) highlighted a number of issues with TBL, notably a dissatisfaction in TBL rigidity and a preference for smaller group sizes in CBL.33 Overall, there appears to be limited evidence comparing student perceptions/satisfaction of TBL with other teaching pedagogies in undergraduate dental education. That said, however, there are studies which have looked at student satisfaction with TBL in undergraduate dental education and found high levels of satisfaction, but such studies have assessed TBL alone and have failed to compare this to other teaching pedagogies.38,39
In the UK, dentistry is a healthcare modality that has traditionally been provided within the NHS. Over the last 12 months, it has become increasingly publicised that NHS dentistry is in a precarious state, and while several potential solutions have been put forward and discussed on public, professional and political platforms, one potential solution has been to increase the number of undergraduate dental places within our educational institutions.40 While such a change may increase the size of our future dental workforce, it is paramount that institutions are able to accommodate these increasing numbers while still providing high-quality training and ensuring that these increased numbers do not adversely affect the competency and proficiency of graduating dental students. It is therefore pertinent, now more than ever, that we ensure the teaching pedagogies used to deliver undergraduate dental education are effective and make efficient and appropriate use of the resources available within our educational institutions. At present, multiple institutions in the UK utilise constructivist teaching approaches such as PBL and EBL in undergraduate dental programmes,15,17,41 and while these are generally considered more favourable than traditional, lecture-based methods, they are fraught with their own distinct and logistical challenges.19,42,43 These range from lack of educational standardisation to the increasing number of rooms needed to accommodate the small group discussions and the large number of facilitators required. One could argue that in contrast to this, TBL is a teaching pedagogy that maintains the benefits of a constructivist approach to teaching while requiring only a minimal number of expert facilitators. It has the added benefit that every student receives the same level of expert input, and as such, institutions can potentially be more confident about the standardisation of teaching, leading to improved levels of quality assurance.
Conclusion
As outlined above, TBL may have the potential to provide a more effective constructivist teaching methodology for delivering undergraduate dental education. Based on the literature identified in this scoping review, it appears that there is some evidence that TBL may be effective in delivering undergraduate dental education, but this evidence is limited and fraught with several limitations. Overall, most of the studies identified had poor research methodology (there was a lack of randomised controlled trials), were based on small sizes and had delivered TBL to very small portions of the dental curriculum. In addition to this, in most of the studies, the outcomes were focused on a combination of student perception, satisfaction and examination performance, and no regard was given to the perception of educators/institutions. While not entirely conclusive, there is sufficient evidence to support further assessment of TBL in delivering undergraduate dental education using appropriate research methodology and utilising outcomes relevant to all stakeholders.
References
Haden N K, Andrieu S C, Chadwick D G et al. The dental education environment. J Dent Educ 2006; 70: 1265-1270.
Irby D. Educating physicians for the future: Carnegie's calls for reform. Med Teach 2011; 33: 547-550.
Pyle M, Andrieue S C, Chadwick D G et al. The case for change in dental education. J Dent Educ 2006; 70: 921-924.
Werb S B, Matear D W. Implementing evidence-based practice in undergraduate teaching clinics: a systematic review and recommendations. J Dent Educ 2004; 68: 995-1003.
Fincham A G, Shuler C F. The changing face of dental education: the impact of PBL. J Dent Educ 2001; 65: 406-421.
Bassir S H, Sadr-Eshkevari P, Amirikhorheh S, Karimbux N Y. Problem-based learning in dental education: a systematic review of the literature. J Dent Educ 2014; 78: 98-109.
Balos Tuncer B, Sokmen T, Celik B, Tortop T. Perception of dental students towards case-based orthodontic education. J Orofac Orthop 2022; 83: 96-101.
Townsend G C, Winning T A, Wetherell J D, Mullins G A. New PBL dental curriculum at the University of Adelaide. J Dent Educ 1997; 61: 374-387.
Matlin K S, Libert E, McArdle P J, Howell T H. Implementing the problem-based curriculum at Harvard School of Dental Medicine. J Dent Educ 1998; 62: 693-708.
Connolly C, Logue P A, Calderon A. Teaching about curriculum and assessment through inquiry and problem-based learning methodologies: an initial teacher education cross-institutional study. Irish Educ Stud 2023; 42: 443-460.
Thistlethwaite J E, Davies D, Ekeocha S et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med Teach 2012; 34: 421-444.
Savery J R. Overview of Problem-based Learning: Definitions and Distinctions. Interdiscip J Probl Based Learn 2006; 1: 9-20.
Kahn P, O'Rourke K. Understanding Enquiry-Based Learning. In Barrett T, Mac Labhrainn I, Fallon H (eds) Handbook of Enquiry & Problem-Based Learning. Galway: CELT, 2005.
All Ireland Society for Higher Education. An Introduction to Enquiry/Problem-based Learning. Maynooth: All Ireland Society for Higher Education, 2015.
Pau A K, Croucher R. The use of PBL to facilitate the development of professional attributes in second year dental students. Eur J Dent Educ 2003; 7: 123-129.
Fincham A G, Shuler C F. The changing face of dental education: the impact of PBL. J Dent Educ 2001; 65: 406-421.
McHarg J, Kay E J. The anatomy of a new dental curriculum. Br Dent J 2008; 204: 635-638.
Rich S K, Keim R G, Shuler C F. Problem-based learning versus a traditional educational methodology: a comparison of preclinical and clinical periodontics performance. J Dent Educ 2005; 69: 649-662.
Winning T, Townsend G. Problem-based learning in dental education: what's the evidence for and against…and is it worth the effort? Aust Dent J 2007; 52: 2-9.
Glew R H. The problem with problem-based medical education: Promises not kept. Biochem Mol Biol Educ 2003; 31: 52-56.
Michaelsen L K, Sweet M. The essential elements of team-based learning. New Direct Teach Learn 2008; 2008: 7-27.
Parmelee D, Michaelsen L K, Cook S, Hudes P D. Team-based learning: a practical guide: AMEE guide no. 65. Med Teach 2012; 34: 275-287.
Burgess A, Bleasel J, Haq I et al. Team-based learning (TBL) in the medical curriculum: better than PBL? BMC Med Educ 2017; 17: 243.
Burgess A, Bleasel J, Hickson J, Guler C, Kalman E, Haq I. Team-based learning replaces problem-based learning at a large medical school. BMC Med Educ 2020; 20: 492.
Joshi T, Budhathoki P, Adhikari A, Poudel A, Raut S, Shrestha D B. Team-Based Learning Among Health Care Professionals: A Systematic Review. Cureus 2022; 14: 21252.
Reimschisel T, Herring A L, Huang J, Minor T J. A systematic review of the published literature on team-based learning in health professions education. Med Teach 2017; 39: 1227-1237.
Fatmi M, Hartling L, Hillier T, Campbell S, Oswald A E. The effectiveness of team-based learning on learning outcomes in health professions education: BEME Guide No. 30. Med Teach 2013; 35: 1608-1624.
Peters M D, Godfrey C, McInerney P et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth 2022; 20: 953-968.
Tricco A C, Lillie E, Zarin W et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018; 169: 467-473.
Taylor K S, Mahtani K R, Aronson J K. Summarising good practice guidelines for data extraction for systematic reviews and meta-analysis. BMJ Evid Based Med 2021; 26: 88-90.
Free C, Phillips G, Felix L, Galli L, Patel V, Edwards P. The effectiveness of M-health technologies for improving health and health services: a systematic review protocol. BMC Res Notes 2010; 3: 250.
Echeto L F, Sposetti V, Childs G et al. Evaluation of Team-Based Learning and Traditional Instruction in Teaching Removable Partial Denture Concepts. J Dent Educ 2015; 79: 1040-1048.
Haley C M, Brown B, Koerber A, Nicholas C L, Belcher A. Comparing Case-Based with Team-Based Learning: Dental Students' Satisfaction, Level of Learning, and Resources Needed. J Dent Educ 2020; 84: 486-494.
Nawabi S, Bilal R, Javed M Q. Team-based learning versus Traditional lecture-based learning: An investigation of students' perceptions and academic achievements. Pak J Med Sci 2021; 37: 1080-1085.
Nishigawa K, Omoto K, Hayama R et al. Comparison between flipped classroom and team-based learning in fixed prosthodontic education. J Prosthodont Res 2017; 61: 217-222.
Takeuchi H, Omoto K, Okura K et al. Effects of team-based learning on fixed prosthodontic education in a Japanese School of Dentistry. J Dent Educ 2015; 79: 417-423.
Lage M J, Platt G J, Treglia M. Inverting the Classroom: A Gateway to Creating an Inclusive Learning Environment. J Econom Educ 2000; 31: 30-43.
Saadaldin S A, Eldwakhly E, Alaziz S N et al. Team-Based Learning in Prosthodontics Courses: Students' Satisfaction. Int J Dent 2022; DOI: 10.1155/2022/4546381.
Park S E, Salihoglu-Yener E, Fazio S B. Use of team-based learning pedagogy for predoctoral teaching and learning. Eur J Dent Educ 2019; 23: 32-36.
Evans D, Mills I, Burns L, Bryce M, Hanks S. The dental workforce recruitment and retention crisis in the UK. Br Dent J 2023; 234: 573-577.
Zahra D, Bennett J, Belfield L et al. Effect of constant versus variable small-group facilitators on students' basic science knowledge in an enquiry-based dental curriculum. Eur J Dent Educ 2019; 23: 448-454.
Luke A M, Mathew S, Kuriadom S T et al. Effectiveness of Problem-Based Learning versus Traditional Teaching Methods in Improving Acquisition of Radiographic Interpretation Skills among Dental Students - A Systematic Review and Meta-Analysis. Biomed Res Int 2021; DOI: 10.1155/2021/9630285.
Alrahlah A. How effective the problem-based learning (PBL) in dental education. A critical review. Saudi Dent J 2016; 28: 155-161.
Author information
Authors and Affiliations
Contributions
Benjamin James Trill: contributed to conceptualisation, design, conducting the search, data synthesis, data interpretation, and drafted and critically revised the manuscript. Bal Panesar: contributed to conceptualisation, data synthesis, data interpretation, reviewed drafts and critically revised the manuscript. Manas Dave and Reza Vahid Roudsari: contributed to conceptualisation, reviewed drafts and critically revised the manuscript. Hanieh Javidi: contributed to conceptualisation, design, conducting the search, data synthesis, data interpretation and critically revised the manuscript.
Corresponding author
Ethics declarations
Ethical approval was not required because this study retrieved and synthesised data from previously published studies.
The data supporting this study can be obtained from the corresponding author.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2024
About this article
Cite this article
James Trill, B., Panesar, B., Dave, M. et al. Is team-based learning an alternative approach for UK undergraduate dental education? A scoping review of the literature. Br Dent J 236, 52–56 (2024). https://doi.org/10.1038/s41415-023-6615-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-023-6615-x