Abstract
Short-term outcome of myeloablative (MAC) and reduced intensity (RIC) conditioning in the prospective randomized international EBMT RICMAC study in patients with myelodyplastic syndrome (MDS) was comparable but longer follow up is lacking. Patients with MDS aged 18–65 years were randomized to receive MAC (N = 64) with busulfan/cyclophosphamide or RIC (n = 65) with busulfan/fludarabine followed by stem cell transplantation -(HCT) from HLA matched or mismatched donor. After a median follow-up of 6.2 (0.4–12.5) years, 10-year OS and RFS were 54.0% and 43.9% for RIC and 44.4% and 44.2% for MAC (p = 0.15 and p = 0.78), respectively. Since the first report, 6 patients died on NRM, 4 after RIC, and 2 after MAC. Similarly, 8 patients relapsed (4 in each arm), increasing the number of relapsed patients to 28. The second HCT was performed in 18 pts, 8 in the MAC, and 10 in the RIC arm. In a multivariate analysis, ECOG status and chemotherapy prior to HCT were independent risk factors for OS and RFS, ECOG and low cytogenetic risk for NRM and chemotherapy prior to HCT for RI. Patients with low cytogenetic risk had better OS [p = 0.002], RFS [p = 0.02], and NRM (p = 0.015) after RIC as compared to MAC.
Similar content being viewed by others
Introduction
Myelodysplastic neoplasm (MDS) is a molecularly and morphologically heterogeneous disease presenting mainly in older patients with a median age of 76 years [1, 2]. Following new insights into the biology of the disease, exciting new treatment concepts become available, such as hypomethylating agents, molecular therapies, and growth hormones. While novel therapies have been shown to prolong survival, allogeneic hematopoietic cell transplantation (HCT) remains the treatment with the highest curative potential.
HCT after myeloablative conditioning (MAC) has been considered for decades the golden standard for younger patients and used with increasing frequency. From the early century, the use of HCT after reduced intensity conditioning (RIC) or non-myeloablative (NMA) conditioning opened the potential of curative treatment to elderly patients, the population with the highest incidence. However, the optimal conditioning regimen in younger patients has still to be defined. Several retrospective studies described similar results after HCT with RIC or MAC conditioning, but significant age differences were noted in both groups, and selection biases were assumed. Therefore, a randomized study comparing MAC and RIC [3] using a uniform protocol and GVHD-prophylaxis was performed in patients up to the age of 64 years. The short-term results of up to 24 months were published previously [3]. In the following analysis, we present a nonpreplanned analysis of long-term results with a follow-up period of up to 10 years investigating a possible higher late relapse rate after RIC or differences in the outcome of subgroups of patients with different disease risks. The clinical trial was registered as NCT01203228.
Patients and methods
In this prospective, multicenter, open-label randomized phase III study, patients were randomly assigned to receive a MAC regimen that consisted of busulfan (16 mg/kg orally or 12.8 mg/kg intravenously total dose) and cyclophosphamide (120 mg/kg total dose) or a RIC regimen consisting of busulfan (8 mg/kg orally or 6.4 mg/kg intravenously total dose) and fludarabine (150 mg/m2 total dose) followed by allogeneic HCT from a related or unrelated (matched or 1 mismatch) donor. Detailed characteristics of patients and events (including events after 24 months) are listed in Table 1.
Inclusion criteria were reported previously [3]. Recruitment started in 2004 and finished in 2012. Major inclusion criteria were cytologically proven MDS and sAML with <20% of blasts at HCT, a matched or one mismatch related or unrelated donor, age 18–60 years (amended to 65 in February 2006) for unrelated donors and age 50–65 years for related donors. Eighty-five percent of chemotherapies before transplantation were administered in advanced MDS (chronic myelomonocytic leukemia, refractory anemia with excess of blasts, and sAML) to reduce the number of blasts, whereas only 15% of chemotherapies were administered to less advanced MDS (refractory anemia, refractory anemia with ringsideroblasts, and refractory anemia with multilineage dysplasia). Other inclusion criteria were adequate hepatic, renal, pulmonary, and cardiac functions. Graft-versus-host disease (GVHD) prophylaxis consisted of cyclosporine and a short course of methotrexate (10 mg/m2 on days +1, +3, +6, and +11) for both arms. In the case of an unrelated donor, antilymphocyte globulin (Fresenius, Graefelfing, Germany) at a cumulative dose of 30 to 60 mg/kg or antithymocyte globulin (Thymoglobulin; Sanofi, Paris, France) at a cumulative dose of 6–10 mg/kg was administered divided on days −3, −2, and −1 according to center policy.
The primary endpoint for the long-term follow-up was overall survival (OS), and secondary endpoints were relapse-free survival (RFS), relapse incidence (RI), non-relapse mortality (NRM), and chronic graft-versus-host disease (GVHD) incidence. Furthermore, OS and RFS were analyzed in MDS subpopulations. Chronic GVHD was scored according to Shulman criteria (limited and extensive) [4]. For Random Assignment Procedure, patient enrollment, center and country distribution, definitions of graft failure, engraftment, and acute and chronic GVHD, see previous publication [5].
The RICMAC Study was conducted in accordance with good clinical practice guidelines and the provisions of the Declaration of Helsinki. Protocol approval was obtained from an independent ethics committee at each study site. All patients provided written informed consent. EBMT sponsored the study.
Statistical methods
The main analysis and the landmark (conditional) analysis compared patients according to the randomization arm (Intent-To-Treat principle). In a secondary analysis, we excluded cases (n = 4) with major violations (Per-Protocol analysis). The landmark analysis included all patients alive relapse-free (and cGVHD-free for that endpoint) at 12 months post-allo. Table 1 describes differences in characteristics at baseline, reporting Fisher’s exact and Mann–Whitney tests p-values. OS and RFS were estimated by the Kaplan–Meier method and compared by Log-Rank test in univariable analysis and by Cox regression in multivariable analysis. NRM and relapse were analyzed as mutually competing risks. For Chronic GVHD, relapse or death were considered competing events, and onset was measured from 100 days post-transplant. For endpoints with competing events, we used the proper cumulative incidence estimator, the Gray test for univariable analysis, and Cox regression for the analysis of cause-specific hazards. Stratification factors (donor type, blasts, age), as well as patient and donor gender or gender mismatch, CMV status combination, diagnosis subgroup (sAML vs. other), cytogenetics, International Prognostic Scoring System score, performance status, prior chemotherapy, and use of busulfan (RIC vs. MAC), were considered for inclusion in Cox models with the random assignment arm. Selection was done on the basis of significance, taking into account prior clinical knowledge, the presence of missing values, and aspects related to model validation. Analyses were performed by using SPSS version 25 and R package version 3.3.
Results
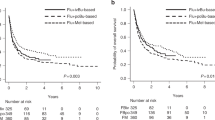
Overall survival
Comparing estimated OS from the initial analysis [5] with the current/updated analysis OS is presented in Fig. 1. The curves are overlapping during the first 24 months and now reach an OS of 50% at 10 years with a follow-up extended from a median follow up of 24 months to 74.9 (4.31–149.6) months (MAC 75.4 vs. RIC 72.2 months; p = 0.8). Median OS time was not reached (CI 95%: 73.6–) months for RIC and 97.3 (CI 95%: 25.4–) months for MAC. There was a trend towards improved OS 54.0 (CI 95%: 38.5–69.4)% of RIC in comparison to MAC 44.4 (CI 95%: 29.3–59.5)% at 10 years (Fig. 2a) without reaching statistical significance. The difference did not reach the 5% level of statistical significance (p = 0.15), and it was more evident in the first 100 days post-allo (HR = 0.31, p = 0.084). A total of 18 patients received a second allogeneic HCT, 8 in the MAC and 10 in the RIC group (Table 1). Interestingly, indications for 2nd HCT were 3 relapses, 4 graft failures, and one poor graft function in the MAC and 8 relapses, one graft failure, and one donor-cell derived MDS in the RIC group. For patients who underwent a second HSCT for relapse, median times to relapse and to transplant were 5.3 (1.0–33.1) and 8.5 (4.6–53.1) months, respectively. In the multivariate analysis, ECOG > 0 and the administration of chemotherapy were associated with OS (HR 2.45 and 2.31, respectively) with p = 0.01 each (Table 2). Time from diagnosis to transplant did not impact the outcome in both arms.
Initial analyses [5] versus updated analyses of overall survival of all patients (n = 129) recruited in the RICMAC study.
Relapse free survival
RFS at 10 years is presented in Fig. 2b and amounts to 44.2 (CI 95%: 29.9–58.6)% for MAC and 43.9 (CI 95%: 29.1–58.8)% for RIC (p = 0.78). Median time of RFS totals 87.4 (CI 95%: 18.4–) for MAC and 86.1 (26.2–) months for RIC. Similar to OS, ECOG > 0 and chemotherapy was an independent determinant for RFS (HR 2.08; p = 0.02 and HR 2.00; p = 0.01, respectively; Table 2).
RI
Cumulative Incidence of relapse at 10 years was 25.2% (CI 95%: 12.3–38.2) after MAC and 25.7% (CI 95%: 13.5–38.0) (p = 0.66) after RIC. Administration of chemotherapy prior to HSCT was associated with a higher RI (HR 3.02; CI 95%: 1.37–6.64; p = 0.006; Table 2).
NRM and chronic GVHD
The non–relapse mortality was 30.5% (CI 95%:19.0-42.0) after MAC and 30.3% (CI 95%:17.2–43.5) after RIC at 10 years (p = 0.50). The only significant predictors for NRM in the multivariate analysis were the low cytogenetic risk group [HR: 4.14 (1.20–14.29) p = 0.02] and ECOG > 0 [HR 3.49 (1.33–9.16), p = 0.01]. A total of 70 patients developed cGVHD (limited n = 15, extensive n = 49, 6-grade unknown) by a median of 6.0 months (range, 3.3–48.9). Five patients had cGVHD following 2nd HCT because of relapse, 3 extensive, and 2 of unknown grade. Chronic GVHD incidence did not differ between the two groups and was 68.2% (CI 95%: 55.0–81.4) for MAC and 65.5% (CI 95%: 53.0–78.0) for RIC (p = 0.70). RIC had evidence for less NRM than MAC in the first 100 days post-HCT, though not reaching significance at the canonical 5% level (HR = 0.30, p = 0.075).
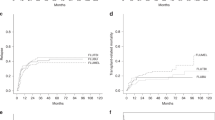
Analysis of landmark 12 months and per protocol
Analyses of OS, RFS, NRM, RI, and incidence of cGVHD were performed as a landmark analysis at 12 months to show the effect without short-term influences of NRM within one year. The difference in OS described above was not seen in the landmark analysis (Fig. 3a), but was confirmed in the analysis per protocol (only 4 patients less in the per protocol analyses). It should be noted that RFS after RIC and MAC overlapped in all three analyses [final analysis (Fig. 2b), landmark (Fig. 3b), and per protocol (data not shown]. RI (Fig. 3c), NRM (Fig. 3d), and cGvHD (Fig. 3e) were without statistical difference.
Subgroup analysis
We were interested in looking at particular subgroups of patients that might benefit from one of the two preparative regimens. Among patients with low cytogenetic risk profiles those who received RIC had better outcomes compared to MAC: OS (HR 0.22 (CI 95%: 0.09–0.57); p = 0.002), RFS [HR 0.37 (CI 95%: 0.16–0.86); p = 0.02] and lower NRM [0.29 (CI 95%: 0.1–0.79); p = 0.02] but with no difference in RI (Table 2).
Discussion
In the present long-term follow-up of the multicenter, multinational, randomized phase III RIC-MAC study, we confirmed our previously published results and highlighted new findings. As of to date, the present analysis is based on the longest follow up in a randomized study for HCT in MDS. First of all, HCT leads to a long-term OS of 49% (95% CI: 38.3–60.1) at 10 years, irrespective of the preparative regimen and with similar results following RIC (FluBu2) and MAC (BuCy). Overall RI was around 25.4% (16.5–34.3) and NRM 30.4% (21.6–39.1) at 10 years without statistically significant differences between the two arms. HCT after RIC and MAC display comparable long-term outcomes in patients up to 65 years with MDS. RIC showed a trend for better OS as compared to MAC early after HCT but RFS was overlapping. In general, RIC protocols have been shown to have less morbidity compared to MAC, possibly due to a lower infection rate [6] and faster engraftment with a lower likelihood of bleeding complications [7] and a higher probability of pregnancy [8, 9], but also to less stomatitis and to a trend to overall lower Bearmann grade >1 toxicity in the randomized RICMAC [3] study. Chronic GVHD did not differ between the two arms. Risk factors in a multivariate analysis were ECOG > 0 (OS, RFS, NRM, and RI) and chemotherapy prior to HCT (OS, RFS, and RI). Low-risk cytogenetics was an independent risk factor for OS, RFS, and NRM. Similarly, previous chemotherapy negatively influenced RI, RFS, and OS. This finding is not easily explainable and might represent a selection of high-risk patients needing chemotherapy before HCT or the selection of resistant MDS clones during pre-transplant therapy [10].
RI in our study was lower than published in other studies with 37% for MDS and 51% for AML patients with RIC [11]. NRM was higher than described and could be explained by the earlier recruitment period, where no high-resolution typing was available. There is no data on OS at 10 years available for comparison, but OS compares favorably to 70.2% (95% CI: 51.8–85.7%) for MAC vs. 58.3% (95% CI: 39.2–76.2%) for RIC at 4 years.
Randomized comparisons between MAC and RIC of the BMT–CTN trial were published previously [11, 12]. Here, at 4 years, the NRM was 25.1% for MAC, compared with 9.9% for RIC (p < 0.001), but patients who received RIC had a significantly higher risk of relapse (60.7% vs. 19.8%; [HR], 4.06; 95% CI: 2.59–6.35; p < 0.001). OS was superior for patients who received MAC compared to those who received RIC (HR, 1.54; 95% CI: 1.07–2.2; p = 0.03), but OS in only MDS patients was 70.2% (95% CI: 51.8–85.7%) for MAC versus 58.3% (95% CI: 39.2–76.2%) for RIC and not statistically significantly different (p = 0.366). There are several differences between this analysis and our clinical trial. Scott et al. analyzed patients with AML (n = 218) and MDS (n = 54) in contrast to 125 patients with MDS (including 12 patients with AML) in our study. Furthermore, different conditioning regimens were allowed (RIC: FLU + BU2 or Melphalan; MAC: BU4/CY or FLU+Bu4 or Cy+TBI 12 or 14.2 Gy), and a variety of GVHD regimens and ATG were allowed as decided by each center. In our trial, uniform conditioning of BU4/CY for MAC and FLU/BU2 for RIC and the same GVHD prophylaxis was used. Median follow-up was 75 vs. 51 months. In agreement with the Scott study, OS (primary endpoint in both studies) and RFS of MDS patients were not different in the two studies.
A metaanalysis looking at 31 clinical trials on MDS patients, identified only 2 prospective randomized trials of RIC versus MAC reporting OS, RFS, NRM, relapse, and GVHD [13]. Combined analysis of MDS patients revealed no difference in OS, RFS, and RI.
Our results also compares favorably to the OS and RFS described in another randomized study using busulfan based RIC versus treosulfan [14, 15]. The estimated OS at 36 months were 52.4 (42.2–61.6) for RIC and 62.5 (48.4–73.7) for treosulfan.
The lack of an IPSS-R score, which was not available at the study start may be considered a limitation of the study. The study shows that in younger patients with a median age of 51 years, the OS and RFS did not differ significantly between RIC and MAC. The results presented here refer only to the comparison of FluBu2 as RIC versus BuCy as MAC and not for other RIC (e.g., FluMel) or MAC regimens.
Overall, we report that low risk cytogenetic patients have the highest benefit with RIC for OS and RFS because of lower NRM. Therefore RIC may be considered as equivalent to MAC in younger patients with MDS, but preferentially cytogenetic low risk patients should be treated with RIC.
Data availability
Data can be requested by e-mail to the corresponding author.
References
Ma X. Epidemiology of myelodysplastic syndromes. Am J Med. 2012;125(7 Suppl):S2–5. https://doi.org/10.1016/j.amjmed.2012.04.014.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65. https://doi.org/10.1182/blood-2012-03-420489
Kroger N, Iacobelli S, Franke GN, Platzbecker U, Uddin R, Hubel K, et al. Dose-reduced versus standard conditioning followed by allogeneic stem-cell transplantation for patients with myelodysplastic syndrome: a prospective randomized phase III study of the EBMT (RICMAC Trial). J Clin Oncol. 2017; JCO2016707349. https://doi.org/10.1200/JCO.2016.70.7349.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man: a long-term clinicopathologic study of 20 seattle patients. Am J Med. 1980;69:204–17.
Kroger N, Sockel K, Wolschke C, Bethge W, Schlenk RF, Wolf D et al. Comparison between 5-azacytidine treatment and allogeneic stem-cell transplantation in elderly patients with advanced MDS according to donor availability (VidazaAllo Study). J Clin Oncol. 2021: JCO2002724. https://doi.org/10.1200/JCO.20.02724.
Chen W, Zhao Y, Luo Y, Yu J, Fu H, Lai X, et al. Clinical characteristics, microbiology, and risk factors for mortality of pre-engraftment and post-engraftment bloodstream infection in hematopoietic stem cell transplantation recipients. Infect Drug Resist. 2022;15:6893–905. https://doi.org/10.2147/IDR.S392804.
Kim DH, Seo J, Shin DY, Koh Y, Hong J, Kim I, et al. Reduced-intensity conditioning versus myeloablative conditioning allogeneic stem cell transplantation for patients with myelofibrosis. Blood Res. 2022;57:264–71. https://doi.org/10.5045/br.2022.2022194.
Salooja N, Michonneau D, Tichelli A, van der Werf S, Aljurf M, Browne PV, et al. Conception and pregnancy outcomes after haematopoietic stem cell transplant: a retrospective study from the transplant complications working party of the European Society for Blood and Marrow Transplantation. Blood. 2018;132:2139. https://doi.org/10.1182/blood-2018-99-113643.
Forgeard N, Jestin M, Vexiau D, Chevillon F, Ricadat E, Peffault de Latour R, et al. Sexuality- and fertility-related issues in women after allogeneic hematopoietic stem cell transplantation. Transpl Cell Ther. 2021;27:432.e431–432.e436. https://doi.org/10.1016/j.jtct.2021.02.003.
Jacoby MA, Duncavage EJ, Chang GS, Miller CA, Shao J, Elliott K, et al. Subclones dominate at MDS progression following allogeneic hematopoietic cell transplant. JCI Insight 2018; 3. https://doi.org/10.1172/jci.insight.98962.
Scott BL, Pasquini MC, Logan BR, Wu J, Devine SM, Porter DL, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation for acute myeloid leukemia and myelodysplastic syndromes. J Clin Oncol. 2017;35:1154–61. https://doi.org/10.1200/JCO.2016.70.7091.
Scott BL, Pasquini MC, Fei M, Fraser R, Wu J, Devine SM, et al. Myeloablative versus reduced-intensity conditioning for hematopoietic cell transplantation in acute myelogenous leukemia and myelodysplastic syndromes-long-term follow-up of the BMT CTN 0901 Clinical Trial. Transpl Cell Ther. 2021;27:483.e481–483.e486. https://doi.org/10.1016/j.jtct.2021.02.031.
Rashidi A, Meybodi MA, Cao W, Chu H, Warlick ED, Devine S, et al. Myeloablative versus reduced-intensity hematopoietic cell transplantation in myelodysplastic syndromes: systematic review and meta-analysis. Biol Blood Marrow Transpl. 2020;26:e138–e141. https://doi.org/10.1016/j.bbmt.2020.03.003.
Beelen DW, Stelljes M, Remenyi P, Wagner-Drouet EM, Dreger P, Bethge W, et al. Treosulfan compared with reduced-intensity busulfan improves allogeneic hematopoietic cell transplantation outcomes of older acute myeloid leukemia and myelodysplastic syndrome patients: final analysis of a prospective randomized trial. Am J Hematol. 2022;97:1023–34. https://doi.org/10.1002/ajh.26620.
Beelen DW, Trenschel R, Stelljes M, Groth C, Masszi T, Remenyi P, et al. Treosulfan or busulfan plus fludarabine as conditioning treatment before allogeneic haemopoietic stem cell transplantation for older patients with acute myeloid leukaemia or myelodysplastic syndrome (MC-FludT.14/L): a randomised, non-inferiority, phase 3 trial. Lancet Haematol. 2020;7:e28–e39. https://doi.org/10.1016/S2352-3026(19)30157-7.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Paper writing: CN and NK. Data collection and analysis: all authors. Final approval of the paper: All authors.
Corresponding author
Ethics declarations
Competing interests
The study was funded in part by Pierre Fabre. NK received an honorarium from Novartis, Neovii, Riemser, and BMS. PD consultancy for AbbVie, AstraZeneca, Beigene, BMS, Gilead, Miltenyi, Novartis, Riemser; speakers’ bureau for AbbVie, AstraZeneca, BeiGene, BMS, Gilead, Novartis, Riemser, Roche; research support from Riemser (all to institution). WB received Honoraries and Travel Grants from Medac, Miltenyi, BMS, Janssen, and Novartis. MR received research funding (independent studies) from AbbVie, Novartis, Medac, and Astex. LPM received an honorarium from Pfizer, Gilead Novartis, Amgen, Jazz, and Neovii.KH received research support from Celgene/BMS, Gilead, Incyte, Janssen, Roche, and Sanofi and honorarium from AbbVie, EUSA Pharma, Gilead, Incyte, Novartis, Roche, Beigene, Celgene/BMS, EUSA Pharma, Incyte, Roche, Sanofi. UP received honoraria from Abbvie, Celgene/Jazz, Curis, Geron, and Janssen for consulting or advisory roles from BMS GmbH & Co KG, Celgene/Jazz, and Novartis, research funding from Amgen, BerGenBio, Celgene, Curis, Janssen, and Novartis, and travel sponsoring, accommodations, and expenses from Celgene. DPM received honoraria/consultation fees from Novartis, Jazz Pharma, and partial participation in a company-sponsored bureau (AbbVie, CTI).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Niederwieser, C., Iacobelli, S., Franke, GN. et al. Reduced intensity versus myeloablative conditioning for MDS: long-term results of an EBMT phase III study (RICMAC). Bone Marrow Transplant (2024). https://doi.org/10.1038/s41409-024-02282-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41409-024-02282-7