Abstract
The COVID-19 pandemic and the ensuing widespread lockdown measures have had a negative impact on the mental health of children and adolescents. We thus conducted a meta-analysis of the worldwide prevalence of sleep disturbances in children and adolescents during the COVID-19 pandemic. We performed a systematic literature search of the major international (PubMed, PsycINFO, Web of Science) and Chinese (Chinese Nation Knowledge Infrastructure (CNKI) and WANFANG) databases from their commencement dates to 27 December 2022. Altogether, 57 articles covering 206,601 participants were included in the meta-analysis. The overall prevalence of sleep disturbances was 34.0% (95% confidence interval (CI): 28–41%). The prevalence of parent-reported sleep disturbances during the COVID-19 pandemic was significantly higher than that of self-reported (p = 0.005) sleep disturbances. Epidemiological studies jointly conducted across Asia and Europe had a higher prevalence of sleep disturbances compared to those conducted in Asia, Europe, America, Oceania, or South America alone (p < 0.001). Children had a significantly higher prevalence of sleep disturbances compared to adolescents alone or a mixed cohort of children and adolescents (p = 0.022). Meta-regression analyses revealed that mean age (p < 0.001), quality evaluation score (p < 0.001), and percentage of men (p < 0.001) showed negative associations, while time of survey (B = 1.82, z = 34.02, p < 0.001) showed a positive association with the prevalence of sleep disturbances. Sleep disturbances were common in children and adolescents during the COVID-19 pandemic.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been declared a pandemic since March 11, 2020 by the World Health Organization (WHO) [1]. As of September 23, 2020, there have been over 230 million COVID-19 cases and more than 4 million deaths caused by COVID-19 [2]. The crucial COVID-19 pandemic preventive measures such as mass lockdowns, social distancing, mask-wearing, frequent hand hygiene, and restriction of school and recreational activities have had a negative influence on the mental health of nearly all populations especially children and adolescents, such as an increased risk of depression, anxiety, post-traumatic stress disorder (PTSD), and sleep problems [3,4,5,6,7,8].
To reduce the negative impact of adverse mental health and allocate appropriate health resources, understanding the epidemiology of mental health problems and their associated factors is important. In the past years, numerous studies on the mental health impacts on children and adolescents, particularly the occurrence of depressive and anxiety symptoms, have been conducted, with mixed findings [9, 10]. A recent meta-analysis revealed that the pooled prevalence estimates of depressive and anxiety symptoms were 25.2% (95% confidence interval (CI): 21.2–29.7%) and 20.5% (95% CI: 17.2–24.4%), respectively in children and adolescents during the COVID-19 pandemic [11]. Sleep disturbances might be associated with increased stress levels, excessive online activities, reduced peer interactions, increased daytime sleep, and disrupted daily routine and sleep/wake schedule, all of which could increase the risk of loneliness, negative affect, lethargy, and napping behaviors [12].
Although many studies focused on sleep disturbances in children and adolescents, the findings varied greatly between studies with very few meta-analyses published. One meta-analysis reported that the prevalence of sleep problems was 35.7% (95% CI: 29.4–42.4%) in the general population during the COVID-19 pandemic [13]. In a recent meta-analysis of major sub-populations [14], the prevalence of sleep disturbances was 45.96% [36.90- 55.30%] (N = 10) among children and adolescents during the COVID-19 pandemic. Another meta-analysis found that the pooled prevalence of sleep disorders alone was 44% (95% CI: 21%- 68%) in children and adolescents during the pandemic [8], but when more broadly defined, those with sleep disturbances were not included. In another meta-analysis examining sleep disturbances in children and adolescents with and without neurobehavioral disorders, the pooled prevalence of any sleep disturbance was 54% during the COVID-19 pandemic (95% CI: 50–57%) [15]. However, the inclusion of neurobehavioral disorders and only a small number of studies (N = 3) might have biased the findings. This gave us the impetus to conduct a meta-analysis on the worldwide prevalence and associated factors of sleep disturbances in children and adolescents during the COVID-19 pandemic.
Material and methods
Search strategy and selection criteria
This meta-analysis was conducted based on the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) [16]. This protocol was registered in the International Platform of Registered Systematic Review and Meta-analysis Protocol (INPLASY) (registration number is INPLASY202190098). Two investigators (HC and PC) independently searched the relevant literature in the major international (PubMed, PsycINFO, and Web of Science) and Chinese databases (Chinese Nation Knowledge Infrastructure (CNKI) and WANFANG) from their commencement dates until 27 December 2022 using the following terms: (Sleep Initiation and Maintenance Disorders [MeSH Terms] OR sleep disturbance OR insomnia OR sleep problem OR sleep disorder OR sleep symptom OR sleep*) AND (adolescent [MeSH Terms] OR child OR children OR preschool OR pediatrics OR infants OR toddlers) AND (2019-ncov* OR 2019ncov* OR 2019n-cov* OR coronaviru* OR corona viru* OR covid OR covid-19 OR covid19* OR novel cov* OR ncov* OR covid-2019 OR covid2019 OR SARS-COV2* OR SARS COV-2* OR SARS COV2* OR SARS COV19 OR SARS COV-19 OR SARS-COV-2019 OR SARS COV 2019 OR SARS COV-2019 OR severe acute respiratory syndrome or severe acute respiratory disease) AND (epidemiology OR prevalence OR rate) (Supplementary Table 1).
Inclusion and exclusion criteria
The inclusion criteria were developed according to the PICOS acronym as follows: Participants: Children and Adolescents; Intervention: not applicable; Control: not applicable; Outcomes: the prevalence of sleep disturbances or data that could generate prevalence of sleep disturbances during the COVID-19 pandemic; and Study design: epidemiological surveys, including cross-sectional surveys and baseline (cross-sectional) data of cohort studies. There were no restrictions on the measures on sleep disturbances used. When more than one paper was published based on the same dataset, only the one with the largest sample was included.
Study selection and data extraction
The same two investigators independently screened the titles and abstracts, and then read the full texts of relevant papers for eligibility. Moreover, the reference lists of the relevant reviews were checked manually to identify any additional studies. Any uncertainty in the literature search was resolved by a discussion with a third investigator (YTX). The literature search procedure is shown in Fig. 1.
The two investigators independently performed data extraction using a standardized form. Study and participant characteristics such as the first author, year of publication, country, time of the survey, study design, sampling method, mean age, total sample size, sample size of males, and scale used for sleep disturbance were recorded.
Study quality assessment
Study quality was assessed using an instrument for epidemiological studies [17, 18], with 8 items as follows: (1) target population was defined clearly, (2) probability sampling or entire population surveyed, (3) response rate was equal or >80%, (4) non-responders clearly described, (5) sample representative of the target population, (6) data collection methods standardized, (7) validated criteria used to measure sleep disturbance, and (8) prevalence estimates given with confidence intervals and detailed by subgroups (if applicable). The total score ranged from 0 to 8. Studies with a total score of “7–8” were considered as “high quality”, “4–6” as “moderate quality” and “0–3” as “low quality” [19]. Any uncertainty in the quality assessment was resolved via a discussion with a third investigator (YTX).
Statistical analysis
This meta-analysis was implemented using the R software [20] and comprehensive meta-analysis (CMA) version 2.0 (Biostat Inc., Englewood, NJ, USA). Due to the different study characteristics between studies, the random-effects model was used to calculate the pooled prevalence of sleep disturbances with their 95% CI. Following previous meta-analyses of epidemiology [21, 22], the raw data were analyzed with the random-effect model. The heterogeneity between studies was assessed with the I2 statistic, and I2 > 50% was considered an indication of high heterogeneity [23]. In addition, τ2 values arising from the random effects model were also used to quantify heterogeneity. The moderating effects of categorical variables (e.g., type of data collection (self-report vs. parent-report), children and/or adolescents, and region classified by the WHO regional classification (Africa/North and South America/Eastern Mediterranean/Europe/South East Asia/Western Pacific) [24]) and continuous variables (e.g., percentage of males, mean age, time of survey and quality evaluation score) on the results were examined using subgroup and meta-regression analyses, respectively. Sensitivity analyses were performed to identify outlying studies by excluding studies one by one. Publication bias was estimated with funnel plots and Begg tests [25]. A p-value < 0.05 was considered statistically significant (two-tailed).
Results
Study and participant characteristics are summarized in Table 1. Out of 4946 articles identified, a total of 57 articles covering 206,601 participants were included in the meta-analysis. The sample size ranged from 28 to 42,077. The mean age of participants ranged from 6.78 to 17.4 years. Study quality assessment scores ranged from 3 to 7; 2 studies were rated as low quality; 51 studies were moderate quality, and 4 were high quality (Supplementary Table 2).
Pooled prevalence of sleep disturbance
In the meta-analysis, 57 studies reported the prevalence of sleep disturbances in children and adolescents. The overall prevalence of sleep disturbance was 34.0% (95% CI: 28–41%, I2 = 100%, τ2 = 0.071) (Fig. 2).
Sensitivity analysis and publication bias
Sensitivity analyses did not find any outlying studies that could significantly change the prevalence of sleep disturbances in children and adolescents during the COVID-19 pandemic. The Funnel plot and Begg test did not find significant publication bias with respect to the prevalence of sleep disturbance (Begg test: z = 0.21, p = 0.83) (Supplementary Fig. 1).
Subgroup and meta-regression analyses
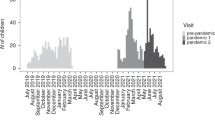
As shown in Table 2, the type of data collection, region, and inclusion of children and/or adolescents was significantly associated with the prevalence of sleep disturbances. The prevalence of parent-reported sleep disturbances during the COVID-19 pandemic were significantly higher than that of self-reported sleep disturbances (Q = 7.948, p = 0.005). Epidemiological studies jointly conducted across Asia and Europe had a higher prevalence of sleep disturbances compared to those conducted in Asia, Europe, America, Oceania, and South America alone (Q = 23,656, p < 0.001). Children had a significantly higher prevalence of sleep disturbances compared to adolescents alone or a mixed cohort of children and adolescents (Q = 7.670, p = 0.022). In contrast, there was no significant difference in the prevalence of sleep disturbances as assessed by different scales on sleep disturbances (Q = 10.281, p = 0.068). Meta-regression analyses revealed that mean age (B = −0.20, z = −53.79, p < 0.001), study quality assessment (B = −19, z = −34.38, p < 0.001) and percentage of men (B = −0.37, z = −16.79, p < 0.001) showed negative associations with the prevalence of sleep disturbances (Supplementary Figs. 2–4). In contrast, the time of the survey (B = 1.82, z = 34.02, p < 0.001) showed a positive association with the prevalence of sleep disturbances (Supplementary Fig. 5).
Discussion
This systematic review and meta-analysis found that the worldwide prevalence of sleep disturbances in children and adolescents was 34% (95% CI: 28–41%) during the COVID-19 pandemic, which is lower than the corresponding figures in two previous meta-analyses which reported 54% (95% CI: 50–57%) [15] and 44% (95% CI: 21%, 68%) [8], respectively. However, it should be noted that in the first meta-analysis [15] children and adolescents with neurobehavioral disorders were included, which could increase the prevalence of sleep disturbances; further, only 5 studies were included which could only provide preliminary findings. In another meta-analysis [8], the prevalence of sleep disorders, rather than sleep disturbances more broadly, was examined. Hence, direct comparisons between studies must be made with caution. In addition, our finding was higher than the corresponding figure (26%; 95% CI: 24–27%) in adolescents [26] and the general population (15%; 95% CI: 12.1–18.5%) [27] in China prior to the COVID-19 pandemic. Possible reasons for increased sleep disturbances in children and adolescents included fear caused by the pandemic and related preventive measures such as closures of school and recreation facilities, social distancing from their peers, and compulsory home quarantine, all of which could increase the risk of mental health problems including sleep disturbances in this population [8, 15].
In this meta-analysis, parent-reported sleep disturbance prevalence was higher than self-reported sleep disturbance by children and adolescents. This is consistent with previous findings [28, 29]. Other research [30] has found that when assessing health/disease status, external raters (e.g. physicians and caregivers) are more likely to focus on patients’ objective symptoms and disease diagnoses, whereas patients tend to focus on their subjective symptoms, functional limitations, and quality of life; consequently, discordances between self-report and external assessments are likely. Hence, sleep disturbances in children and adolescents such as difficulties falling asleep during the pandemic and home isolation were more likely to be identified by their parents. Besides, based on the duration of online activities among adolescents and children during the pandemic [31, 32], parents could also ascertain the sleep disturbances in their children objectively.
Younger children were associated with a higher risk of sleep disturbances, which was the opposite result compared to the findings reported prior to the pandemic [26]. Several factors might account for this finding. Younger children usually spend more time doing outdoor and recreational activities and less time studying than older children and adolescents. During the pandemic, however, young children were relatively more deprived of outdoor activities and social groups compared with adolescents who had spent more time in school [15]. Additionally, children were often more fearful due to their lack of understanding of the COVID-19 pandemic’s effects. All these factors might increase the risk of having mental health problems including sleep disturbances [33].
The prevalence of sleep disturbance was significantly higher in studies jointly conducted across Asia and Europe compared to those conducted in Asia, Europe, America, Oceania, and South America alone. There is an substantial inequalities in health care among children and adolescents across countries due to different country-specific socioeconomic and demographic indicators [34], the severity of the pandemic, and access to child mental health services [35], all of which could result in variations in prevalence of sleep disturbances across the regions.
The prevalence of sleep disturbances has increased in more recent surveys, which is consistent with the findings of prospective studies on insomnia symptoms among college students in China [36] and adults living in the United States [37]. Most of the included studies were conducted in 2020 and the first half of the year 2021, during the first peak of the pandemic wave. The prevalence of insomnia symptoms increased dramatically during the initial months of the pandemic [38]. Most children and adolescents experienced stricter public health measures over this period, such as the change from classroom teaching to online classes and reduced outdoor activities, which could substantially affect their sleep/wake schedules and increase their risk of insomnia symptoms [39].
The meta-analysis also found that girls were more likely to have sleep disturbances than boys, which is consistent with the notion that girls usually have a higher risk of mental health-related problems [11, 40]. Possible reasons for the gender difference may include an increased risk of interpersonal stressors, more experience of violence, increased screen time, and reduced outdoor activities during the COVID-19 pandemic in girls [33, 41].
We found a negative relationship between study quality and sleep disturbance prevalence. High-quality studies are usually associated with random sampling, well-trained interviewers, and well-validated measures, all of which could reduce the likelihood of false detection of sleep disturbances and as such, result in a relatively lower prevalence compared to poor-quality studies. In this meta-analysis, most of the included studies were rated as moderate study quality, and therefore high-quality studies that use random sampling, well-trained interviewers, and well-validated measures should be conducted in the future.
The strengths of this meta-analysis include the large number of studies and pooled sample size from both international and Chinese databases. Considering that COVID-19 was first reported in China and that many of the relevant studies were published in Chinese-language journals, it is important to include studies from Chinese-language databases. Several limitations should be noted. First, most of the studies conducted in the early stage of the pandemic (February–March 2020) were conducted in East Asia. Second, most studies were cross-sectional in nature; therefore, the dynamic changes in sleep disturbance prevalence between different periods could not be examined. Third, convenience sampling was used in most studies, which limits the representativeness of the study sample. Fourth, factors associated with sleep disturbances, such as academic pressure at school and psychiatric comorbidities, were not examined due to insufficient data. Finally, heterogeneity is unavoidable when conducting the meta-analysis of epidemiological studies [42, 43], even if subgroup meta-regression analyses were performed.
In conclusion, sleep disturbances were common in children and adolescents during the COVID-19 pandemic, particularly in children. Considering the negative impact of sleep disturbances on daily life, academic performance, and well-being, appropriate prevention and treatment measures should be implemented for this vulnerable population.
Data availability
The data of the investigation will be made publicly available if necessary.
References
World Health Organization. Coronavirus disease (COVID-19) pandemic. World Health Organization; 2020.
Word Health Organization. COVID-19 reports. Word Health Organization. 2021.
Güner HR, Hasanoğlu İ, Aktaş F. COVID-19: Prevention and control measures in community. Turk J Med Sci. 2020;50:571–7.
Qian M, Jiang J. COVID-19 and social distancing. J Public Health. 2020;30:1–3.
Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Global Health. 2020;5:e002794.
Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020;174:882–9.
Mustafa NM, Selim LA. Characterisation of COVID-19 pandemic in paediatric age group: a systematic review and meta-analysis. J Clin Virol. 2020;128:104395.
Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;293:78–89.
Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord. 2020;275:112–8.
Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264.
Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142–1150.
Bruni O, Malorgio E, Doria M, Finotti E, Spruyt K, Melegari MG, et al. Changes in sleep patterns and disturbances in children and adolescents in Italy during the Covid-19 outbreak. Sleep Med. 2022;91:166–74.
Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17:299–313.
Jahrami HA, Alhaj OA, Humood AM, Alenezi AF, Fekih-Romdhane F, AlRasheed MM, et al. Sleep disturbances during the COVID-19 pandemic: a systematic review, meta-analysis, and meta-regression. Sleep Med Rev. 2022;62:101591.
Sharma M, Aggarwal S, Madaan P, Saini L, Bhutani M. Impact of COVID-19 pandemic on sleep in children and adolescents: a systematic review and meta-analysis. Sleep Med. 2021;84:259–67.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Boyle M. Guidelines for evaluating prevalence studies. Evid-based Ment Health. 1998;1:3.
Loney PL, Chambers LW, Bennett KJ, Roberts JG, Stratford PW. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can. 1998;19:170–6.
Yang C, Zhang L, Zhu P, Zhu C, Guo Q. The prevalence of tic disorders for children in China: a systematic review and meta-analysis. Medicine (Baltimore). 2016;95:e4354.
R: A language and environment for statistical computing. R Core Team; 2020. https://www.R-project.org/.
Çoğaltay N, Karadağ E. Introduction to meta-analysis. In: Leadership and organizational outcomes: meta-analysis of empirical studies. John Wiley & Sons; 2015. pp. 19–28.
Scotti L, Franchi M, Marchesoni A, Corrao G. Prevalence and incidence of psoriatic arthritis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2018;48:28–34.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Chen SJ, Shi L, Bao YP, Sun YK, Lin X, Que JY, et al. Prevalence of restless legs syndrome during pregnancy: a systematic review and meta-analysis. Sleep Med Rev. 2018;40:43–54.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Liang M, Guo L, Huo J, Zhou G. Prevalence of sleep disturbances in Chinese adolescents: a systematic review and meta-analysis. PLoS ONE. 2021;16:e0247333.
Cao X-L, Wang S-B, Zhong B-L, Zhang L, Ungvari GS, Ng CH, et al. The prevalence of insomnia in the general population in China: a meta-analysis. PLoS ONE. 2017;12:e0170772.
Short MA, Gradisar M, Lack LC, Wright HR, Chatburn A. Estimating adolescent sleep patterns: parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nat Sci Sleep. 2013;5:23.
Dayyat EA, Spruyt K, Molfese DL, Gozal D. Sleep estimates in children: parental versus actigraphic assessments. Nat Sci Sleep. 2011;3:115.
Giltay EJ, Vollaard AM, Kromhout D. Self-rated health and physician-rated health as independent predictors of mortality in elderly men. Age Ageing. 2012;41:165–71.
Dong H, Yang F, Lu X, Hao W. Internet addiction and related psychological factors among children and adolescents in China during the coronavirus disease 2019 (COVID-19) epidemic. Front Psychiatry. 2020;11:751.
Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health. 2020;20:1–13.
Francisco R, Pedro M, Delvecchio E, Espada JP, Morales A, Mazzeschi C, et al. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front Psychiatry. 2020;11:1329.
Gariepy G, Danna S, Gobiņa I, Rasmussen M, de Matos MG, Tynjälä J, et al. How are adolescents sleeping? Adolescent sleep patterns and sociodemographic differences in 24 European and North American countries. J Adolesc Health. 2020;66:S81–S88.
Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–24.
Wang D, Zhao J, Zhai S, Huang S, Yang Z, Pan Y, et al. Longitudinal trajectories of insomnia symptoms among college students during the COVID-19 lockdown in China. J Psychosom Res. 2022;157:110795.
Vargas I, Muench A, Grandner MA, Irwin MR, Perlis ML. Insomnia symptoms predict longer COVID-19 symptom duration. Sleep Med. 2023;101:365–72.
Perlis ML, Vargas I, Ellis JG, Grandner MA, Morales KH, Gencarelli A, et al. The natural history of insomnia: the incidence of acute insomnia and subsequent progression to chronic insomnia or recovery in good sleeper subjects. Sleep. 2020;43:zsz299.
Brandão LEM, Martikainen T, Merikanto I, Holzinger B, Morin CM, Espie CA, et al. Social jetlag changes during the COVID-19 pandemic as a predictor of insomnia-a multi-national survey study. Nat Sci Sleep. 2021;39:1711–22.
Riecher-Rössler A. Sex and gender differences in mental disorders. Lancet Psychiatry. 2017;4:8–9.
Aguilar-Farias N, Toledo-Vargas M, Miranda-Marquez S, Cortinez-O’Ryan A, Cristi-Montero C, Rodriguez-Rodriguez F, et al. Sociodemographic predictors of changes in physical activity, screen time, and sleep among toddlers and preschoolers in Chile during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:176.
Long J, Huang G, Liang W, Liang B, Chen Q, Xie J, et al. The prevalence of schizophrenia in mainland China: evidence from epidemiological surveys. Acta Psychiatr Scand. 2014;130:244–56.
Winsper C, Ganapathy R, Marwaha S, Large M, Birchwood M, Singh SP. A systematic review and meta-regression analysis of aggression during the first episode of psychosis. Acta Psychiatr Scand. 2013;128:413–21.
Acknowledgements
The study was supported by the Beijing High Level Public Health Technology Talent Construction Project (Discipline Backbone-01-028$Discipline Backbones 02-38) and the University of Macau (MYRG2019-00066-FHS).
Author information
Authors and Affiliations
Contributions
Study design: YJ, YF, Y-TX. Data collection, analysis, and interpretation: HC, PC, YJ, QZ. Drafting of the manuscript: HC, TC, Y-TX. Critical revision of the manuscript: CHN. Approval of the final version for publication: all co-authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, H., Chen, P., Jin, Y. et al. Prevalence of sleep disturbances in children and adolescents during COVID-19 pandemic: a meta-analysis and systematic review of epidemiological surveys. Transl Psychiatry 14, 12 (2024). https://doi.org/10.1038/s41398-023-02654-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-023-02654-5
This article is cited by
-
Prevalence and correlates of sleep disturbance among adolescents in the eastern seaboard of China
BMC Public Health (2024)