Abstract
Introduction
Posterior epidural sequestrated disc is a fairly uncommon condition. We report a case of an unusual presentation of posterior epidural migration with contralateral symptoms. We emphasize a high index of suspicion for early recognition and treatment to promote a good neurological recovery.
Case presentation
A 58-year-old man with a history of severe back pain for 1 week developed sudden right leg weakness while walking. Neurological examination revealed motor and sensory impairments of the right lower extremities (positive right straight leg raising test, right tibialis anterior grade 2/5, right extensor hallucis longus grade 1/5, decreased pinprick sensation of L4-5 dermatome right side) according to the Standards for Neurological Classification of Spinal Cord Injury as Asia Impairment Scale D. Magnetic resonance images showed an acute disc herniation at L4-5 on the left side, cranially migrated and sequestrated to the posterior epidural area, causing severe compression to the cauda equina in the thecal sac. The patient was successfully treated with surgery (transforaminal lumbar interbody fusion) on an urgent basis. We saw significant neurological recovery on the first day after surgery. Motor power recovery was achieved with a minor deficit at 4 weeks. At the follow-up examination at 3 months, the patient had no residual neurological deficits as Asia Impairment Scale E.
Discussion
Posterior epidural sequestrated disc with contralateral radiculopathy is very rare. This case brings a new presentation of posterior epidural sequestrated disc. To our knowledge, this is the first report of a case with an unusual presentation of contralateral radiculopathy.
Similar content being viewed by others
Introduction
Lumbar disc herniation may be classified into protrusion, extrusion, and sequestrum [1]. Normally, the sequestrated pieces can migrate both upward and downward. The migration of sequestered pieces to the anterior, posterior epidural, or intradural spaces can occur, although it is rare [2,3,4,5,6,7,8,9,10,11]. A herniated disc with contralateral symptoms is also rare [12, 13], and the choice of surgical approach side is controversial [14, 15]. Magnetic resonance imaging (MRI) is helpful in the diagnosis and management of a herniated disc with contralateral symptoms [15, 16].
We report a case of an unusual presentation of posterior epidural migration with contralateral symptoms to highlight the diagnostic and treatment challenges it involved.
Case presentation
A 58-year-old man, otherwise healthy, had chronic back pain for 2.5 years without radiating pain. After a long-distance drive, he developed severe back and leg pain and went to the hospital nearby, where MRI revealed an acute disc herniation. Conservative treatment by pelvic traction and medication for 4 weeks was attempted but was unsuccessful. Therefore, he was scheduled for surgery the following week. A few days after the patient initially presented at the hospital, he developed sudden and severe back pain with radiating pain and numbness on the right leg. The pain prevented him from moving his leg, and the right leg motor power worsened. He denied having numbness around the perianal area nor difficulties in urination and defecation.
On examination, the straight leg raising test was positive on the right side, weakness of the right tibialis anterior muscle was grade 2/5 and that of the extensor hallucis longus muscle was grade 1/5, and decreased pinprick sensation was noted at L4 and L5 dermatome on the right side Asia Impairment Scale D.
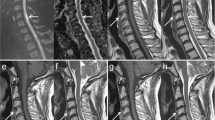
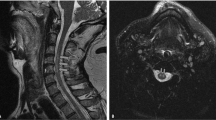
MRI of the L4-5 disc level on the left side demonstrated an iso- to hyposignal intensity mass on sagittal T1-weighted and hypersignal intensity mass on T2-weighted images, with upward migration and sequestration to the posterior epidural area compressing the thecal sac (Fig. 1).
a Sagittal T2-weighted image showing a hypersignal intensity mass at L4-5 on the left side, which has migrated upward and sequestrated to the posterior epidural area, compressing the thecal sac. b Sagittal T1-weighted image showing an iso- to hyposignal intensity mass at L4-5 on the left side. Axial T2-weighted (c) and T1-weighted (d) images showing an acute disc herniation compressing the thecal sac from the left side.
Minimally Invasive Transforaminal lumbar interbody fusion surgery was performed with right side approach. The free disc fragment was found and removed from the left side. The operative finding demonstrated a large mass similar to the sequestrated piece of the L4-5 disc over the thecal sac. This epidural mass was sent to the lab for pathological analysis, and entire fragments of chondroid matrix were found to be interspersing with the intervertebral disc. Pain and motor power improved significantly a few days postoperatively, Right tibialis anterior grade 2/5 to 5/5, right extensor hallucis longus grade 1/5 to 3/5 on day 5 postoperatively. Numbness resolved on day 4 postoperatively. A 1 month follow up, right extensor hallucis longus was return to grade 5/5. Patient was allowed to resume daily activity at 3 months postoperatively Asia Impairment Scale E. Fig. 2
Discussion
For lumbar disc herniation, the incidence of a sequestrated disc has been reported to be 28.6% [1]. Only 1.04% of the sequestratrum migrated to the posterior epidural space [17]. The first report of “posterior epidural migration of disc” in 1973 by Lombardi [18]. Most patients with posterior epidural sequestrated disc present with bilateral symptoms and different degrees of weakness [2,3,4,5,6,7,8,9,10,11, 19,20,21]. Moreover, bowel bladder involvement was not uncommon among patients with posterior epidural sequestrated disc [2,3,4,5,6,7,8,9,10,11, 19, 20]. Nearly half of patients (46.8%) have cauda equina syndrome [17]. The duration of symptoms varies from days to years [14]. The fastest progression of symptoms has been reported to be in 6 h [10], and the longest reported duration of symptoms was 11 years [22].
The case history of similar appearances on MRI is shown in Table 1. Most of the cases showed the posterior epidural mass with hyperintensity on T1-weighted images, iso- or hyperintensity on T2-weighted images, and rim/ring-like enhancement after Gadolinium injection [2,3,4,5,6,7,8,9, 11, 19, 20]. These MRI findings were often indistinguishable from tumor, infection, and hematoma [15].
Treatment of posterior epidural sequestrated disc was mostly surgical (e.g., decompressive laminectomy, hemilaminectomy, discectomy, and transforaminal lumbar interbody fusion) [2,3,4,5,6,7,8,9,10,11, 14, 20, 23]. Only one case was treated conservatively [6].
The recovery from symptoms was considered excellent. Most cases were completely recovered after surgical procedures. Time to complete neurological recovery has been reported from 1 month to 18 months [2, 10, 14, 22, 24].
The mechanism behind herniated disc causing contralateral radiculopathy symptoms in Posterior epidural sequestrated disc remains unclear. However, the literature review confirmed that the phenomenon exists [25]. The series by Sucu and Gelal proved that contralateral disc herniation can be the cause of leg pain. In that study, they operated only on the predominant side of the herniation seen on MRI, and the contralateral symptoms resolved, which shows that sciatica probably was caused by neurological traction rather than by direct compression [22]. However, the explanation of the contralateral symptoms has not yet been established but probably multifactorial [25]. In this case, the different from the previous study as this is not herniated which compressed from the anterior but the epidural disc (compressed from posterior) that caused contralateral symptoms. Mirovsky and Halperin demonstrated five cases of eccentric compression of the spinal canal causing contralateral-side symptoms, and all cases had lesions occupying the space of the spinal canal at or above the herniated level [26]. The pressure applied to the spinal nerve root or the thecal sac may have impaired the intraneural blood flow [27]. Choudhury et al. described three cases with the prominence of spondylotic changes and stenosis contralateral to the side of disc herniation [12]. The absence of the dural ligament (Hoffman’s ligament) was proposed by Kornberg to account for the situation; without the dural ligament, the ipsilateral nerve root can be easily displaced posteriorly, while the contralateral nerve root can be tracted, rather than the ipsilateral nerve root being compressed [13].
In the present case, the patient presented with rare symptoms, namely severe pain and weakness on the right side, while the L4-5 sequestrated disc was found mainly in the epidural area on the left side on MRI. Minimally invasive transforaminal lumbar interbody fusion was performed. Contrary to suggestions by Sucu and Gelal [22] and Mirovsky and Halperin [26] to surgically approach through the side of the compression according to imaging studies, we approached for facetectomy and discectomy as part of Transforaminal Lumbar Interbody Fusion from the side of the main symptoms (contralateral to disc herniation), which was the right side. “Over the top decompression” was not performed. The weakness, pain and paraesthesia of the right leg resolved on early postoperative days. Our findings support the hypotheses that the contralateral side symptoms may be associated with indirect pressure or traction to the contralateral side nerve, rather than direct compression by the disc [22, 26]. Therefore, the approach from the symptom side was suitable for this case.
Our findings are in line with those of a previous study that demonstrates practical value in diagnosis and surgical approach decision [26]. Contralateral herniation is often ignored by surgeons as a coincidental finding on MRI; however, if significant canal compromise is noted at the symptomatic level, we strongly suggest surgical consideration.
Conclusions
We report a rare case of posterior epidural sequestrated disc with an unusual presentation with contralateral radiculopathy. If significant canal compromise is noted at the symptomatic level, we strongly suggest surgical consideration.
References
Brock M, Patt S, Mayer HM. The form and structure of the extruded disc. Spine (Philos Pa 1976). 1992;17:1457–61. https://doi.org/10.1097/00007632-199212000-00003.
Dösoğlu M, Is M, Gezen F, Ziyal MI. Posterior epidural migration of a lumbar disc fragment causing cauda equina syndrome: case report and review of the relevant literature. Eur Spine J. 2001;10:348–51. https://doi.org/10.1007/s005860100300.
Kim H, Kwon BS, Park JW, Lee HJ, Lee JW, Lee EK. et al. Posterior epidural migration of a lumbar intervertebral disc fragment resembling a spinal tumor: a case report. Ann Rehabil Med. 2018;42:621–5. https://doi.org/10.5535/arm.2018.42.4.621.
Kuzeyli K, Cakir E, Usul H, Baykal S, Yazar U, Karaarslan G. et al. Posterior epidural migration of lumbar disc fragments: report of three cases. Spine. 2003;28:e64–7. https://doi.org/10.1097/01.BRS.0000042272.17850.49.
Robe P, Martin D, Lenelle J, Stevenaert A. Posterior epidural migration of sequestered lumbar disc fragments. Report of two cases. J Neurosurg. 1999;90:264–6. https://doi.org/10.3171/spi.1999.90.2.0264.
Tarukado K, Ikuta K, Fukutoku Y, Tono O, Doi T. Spontaneous regression of posterior epidural migrated lumbar disc fragments: case series. Spine J. 2015;15:e57–62. https://doi.org/10.1016/j.spinee.2013.07.430.
Hirabayashi S, Kumano K, Tsuiki T, Eguchi M, Ikeda S. A dorsally displaced free fragment of lumbar disc herniation and its interesting histologic findings. A case report. Spine (Philos Pa 1976). 1990;15:1231–3. https://doi.org/10.1097/00007632-199011010-00026.
Takano M, Hikata T, Nishimura S, Kamata M. Discography aids definitive diagnosis of posterior epidural migration of lumbar disc fragments: case report and literature review. BMC Musculoskelet Disord. 2017;18:151. https://doi.org/10.1186/s12891-017-1516-2.
Teufack SG, Singh H, Harrop J, Ratliff J. Dorsal epidural intervertebral disk herniation with atypical radiographic findings: case report and literature review. J Spinal Cord Med. 2010;33:268–71. https://doi.org/10.1080/10790268.2010.11689706.
Bonaroti EA, Welch WC. Posterior epidural migration of an extruded lumbar disc fragment causing cauda equina syndrome. Clinical and magnetic resonance imaging evaluation. Spine (Philos Pa 1976). 1998;23:378–81. https://doi.org/10.1097/00007632-199802010-00018.
Li K, Li Z, Geng W, Wang C, Ma J. Postdural disc herniation at L5/S1 level mimicking an extradural spinal tumor. Eur Spine J. 2016;25:80–3. https://doi.org/10.1007/s00586-015-4125-5.
Choudhury AR, Taylor JC, Worthington BS, Whitaker R. Lumbar radiculopathy contralateral to upper lumbar disc herniation: report of 3 cases. Br J Surg. 1978;65:842–4. https://doi.org/10.1002/bjs.1800651205.
Kornberg M. Sciatica contralateral to lumbar disk herniation. Orthopedics. 1994;17:362–4.
Theodorou DJ, Theodorou SJ, Kakitsubata Y, Papanastasiou EI, Gelalis ID. Posterior and anterior epidural and intradural migration of the sequestered intervertebral disc: Three cases and review of the literature. J Spinal Cord Med. 2020. https://doi.org/10.1080/10790268.2020.1730110.
Watanabe N, Ogura T, Kimori K, Hase H, Hirasawa Y. Epidural hematoma of the lumbar spine, simulating extruded lumbar disk herniation: clinical, discographic, and enhanced magnetic resonance imaging features. A case report. Spine (Philos Pa 1976). 1997;22:105–9. https://doi.org/10.1097/00007632-199701010-00017.
Chen CY, Chuang YL, Yao MS, Chiu WT, Chen CL, Chan WP. Posterior epidural migration of a sequestrated lumbar disk fragment: MR imaging findings. AJNR Am J Neuroradiol. 2006;27:1592–4.
Akhaddar A, El-Asri A, Boucetta M. Posterior epidural migration of a lumbar disc fragment: a series of 6 cases. J Neurosurg Spine. 2011;15:117–28. https://doi.org/10.3171/2011.3.SPINE10832.
Lombardi VJ. Lumbar spinal block by posterior rotation of anulus fibrosus. Case report. Neurosurg. 1973;39:642–7.
Mugge L, Caras A, Miller W, Buehler M, Medhkour A. A successful outcome despite delayed intervention for cauda equina syndrome in a young patient with a posterior epidural disc extrusion. Cureus. 2019;11:e4645. https://doi.org/10.7759/cureus.4645.
Montalvo Afonso A, Mateo Sierra O, Gil de Sagredo Del Corral OL, Vargas López AJ, González-Quarante LH, Sola Vendrell E. et al. Misdiagnosis of posterior sequestered lumbar disc herniation: report of three cases and review of the literature. Spinal Cord Ser Cases. 2018;4:61.https://doi.org/10.1038/s41394-018-0100-9.
Elsharkawy AE, Hagemann A, Klassen PD. Posterior epidural migration of herniated lumbar disc fragment: a literature review. Neurosurg Rev. 2019;42:811–23. https://doi.org/10.1007/s10143-018-01065-1.
Sucu HK, Gelal F. Lumbar disk herniation with contralateral symptoms. Eur Spine J. 2006;15:570–4. https://doi.org/10.1007/s00586-005-0971-x.
Hawkins JC, Natkha VP, Seibly J. Posterior epidural migration of a lumbar disc herniation causing cauda equina syndrome: a case report. Cureus. 2018;10:e2739. https://doi.org/10.7759/cureus.2739.
Kim JS, Lee SH, Arbatti NJ. Dorsal extradural lumbar disc herniation causing cauda equina syndrome: a case report and review of literature. J Korean Neurosurg Soc. 2010;47:217–20. https://doi.org/10.3340/jkns.2010.47.3.217.
Ruschel LG, Agnoletto GJ, Aragão A, Duarte JS, de Oliveira MF, Teles AR. Lumbar disc herniation with contralateral radiculopathy: a systematic review on pathophysiology and surgical strategies. Neurosurg Rev. 2021;44:1071–81. https://doi.org/10.1007/s10143-020-01294-3.
Mirovsky Y, Halperin N. Eccentric compression of the spinal canal causing dominantly contralateral-side symptoms. J Spinal Disord. 2000;13:174–7. https://doi.org/10.1097/00002517-200004000-00014.
Rydevik B, Brown MD, Lundborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine (Philos Pa 1976). 1984;9:7–15. https://doi.org/10.1097/00007632-198401000-00004.
Acknowledgements
We would like to thank Dr. Khin Myat Myat Lwin, Senior Specialist and Anchana Iam-a-non, research co-ordinator at Bumrungrad International Hospital for the kind co-operation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kesornsak, W., Wasinpongwanich, K. & Kuansongtham, V. Posterior epidural sequestrated disc presenting with contralateral radiculopathy: a very rare case. Spinal Cord Ser Cases 7, 98 (2021). https://doi.org/10.1038/s41394-021-00460-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00460-z
This article is cited by
-
Spinal artery syndrome following kyphoplasty in the setting of a non-compressive extradural cement extravasation: a case report
Spinal Cord Series and Cases (2023)