Abstract
Study design
A descriptive, cross-sectional survey of individuals involved in prehospital transportation of neurotrauma patients was performed.
Objectives
Little is known about prehospital care of neurotrauma patients in low- and middle-income countries. This study sought to assess the knowledge of prehospital transporters in Tanzania and propose an educational intervention to help identify patients with severe neurotrauma.
Setting
Dar es Salaam, Tanzania.
Methods
Surveys assessed demographic information and medical knowledge with three outcomes of identifying signs of a deceased, sick, or clinically deteriorating patient. Predictors of increased medical knowledge were investigated with univariate and multivariate logistic regression (MLR).
Results
The survey included 501 participants, who were predominantly young (mean: 36.7 years) and male (84.0%). More than 70% of participants self-reported being able to recognize a deceased or sick patient, yet fewer than 20% correctly listed more than two signs of a deceased, sick, or clinically deteriorating patient. MLR showed that first aid training (Odds ratio (OR): 2.3; 95% confidence interval (CI): 1.3, 3.9; p = 0.002) was predictive of identifying a deceased patient, being employed (OR: 0.5; 95% CI: 0.3, 0.9; p = 0.021) was a negative predictor of identifying a sick patient, and higher education level (OR: 2.3; 95% CI: 1.1, 4.8; p = 0.032) was predictive of identifying a clinically deteriorating patient.
Conclusion
In a survey of prehospital transporters of neurotrauma patients in Tanzania, higher education level and first aid training were associated with higher medical knowledge scores. An educational flier was created to identify severe neurotrauma patients. Additional education of prehospital transporters in Tanzania may improve morbidity and mortality of neurotrauma patients.
Similar content being viewed by others
Introduction
Injuries due to trauma cause more than 5 million deaths each year, nearly 1.7 times the number of deaths from human immunodeficiency virus/acquired immunodeficiency syndrome, malaria, and tuberculosis combined [1]. Every year, more than 5 million treatable neurosurgical injuries occur in low- and middle-income countries (LMICs) yet they do not undergo surgical intervention; traumatic brain injury (TBI) accounts for the greatest proportion of these cases [2]. Traumatic spine injury (TSI), constituting fractures to the vertebral column and spinal cord injury (SCI), is also a major culprit, mostly affecting young, wage-earning males. Though mortality rates of TSI are lower compared to TBI, more patients survive with a permanent disability, losing the ability to live independently and provide income for their families [3]. For LMICs specifically, a study of TSI patients in northeast Tanzania showed that only 20.7% of patients were able to walk unaided at discharge [4]. In addition, in-hospital mortality rates for TSI remain much higher in LMICs like Tanzania (24.1% reported by Rashid et al.), increasing the burden of this devastating injury [5]. For all neurotrauma (both TBI and TSI), access to neurosurgical expertise is limited in many LMICs for a variety of reasons, including a dearth of resources, lack of qualified surgeons, and delays in access to care [2]. While a multi-pronged approach is needed to improve access to neurosurgical care worldwide, one important and potentially fixable area of need is the prehospital care of patients with neurotrauma.
Many LMICs lack formal prehospital emergency medical services (EMS). In Tanzania, most patients are transported by taxi, bus, or private cars. Barriers to EMS implementation include financial limitations, poor infrastructure, and underqualified first responders [6]. Acutely injured patients are often first referred to lower-level facilities and require long travel times to reach tertiary centers, leading to delays in presentation and missed windows of opportunity for intervention [7, 8]. The first hours following TBI are crucial to prevent morbidity and mortality [9], as 50% of mortality from TBI occurs within the first 2 h after injury [10]. However, neurotrauma patients in Tanzania often wait for days to reach a tertiary center [6]. Studies of TSI from Tanzania have shown that patients are admitted approximately 6 days after injury [3], often with complete SCI. An overwhelming majority of patients (87.2%) included in a study of TSI patients at a referral hospital in northern Tanzania were referrals from peripheral centers [5]. A case report of a TSI patient in rural northern Tanzania illustrated specific factors such as extreme distance to hospital (350 km) and suboptimal transport conditions of TSI patients in LMICs that contribute to increased morbidity [11].
Prehospital care is a major need among LMICs. Ensuring safe and timely prehospital transport has the potential to reduce morbidity and mortality among neurotrauma patients. In addressing this public health problem, we must first assess the medical knowledge of transporters and how patients are transported. Using a major East African tertiary referral center located in Dar es Salaam, Tanzania, the objective of the current study was to (1) describe the current practice of transportation of trauma patients, (2) assess the knowledge of individuals transporting trauma patients, and (3) propose potential interventions for prehospital transporters to recognize neurotrauma emergencies. Our aim was to facilitate the development of efficient, safe prehospital transport of neurotrauma patients.
Methods
Study design
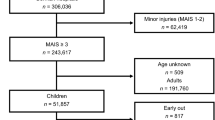
A descriptive, cross-sectional survey was conducted of individuals involved in transporting neurotrauma patients to hospitals. Surveys were administered over a 2-month period in 2016 and distributed within the three municipals of Dar es Salaam—Ilala, Temeke, and Kinondoni—in the 50 km radius from the main hospital (shown in Fig. 1). Since no patient records were accessed, formal institutional review board approval was not required.
Map of Dar es Salaam illustrating three major municipalities [21].
Population surveyed
The intended audience was prehospital transporters, defined as individuals who routinely transport trauma, including neurotrauma, patients from the initial site of injury to Muhimbili National Hospital (MNH) and/or Muhimbili Orthopaedic Institute (MOI). Prehospital transporters were identified at taxi collection areas at major transit points; private car stations including motorcycles and taxi and bus stands; public transport stations; and the Emergency Department at MNH and/or MOI. All individuals interested in or currently involved in transporting trauma patients to hospitals were sampled. Duplication of surveys was protected against by respondents placing initials and phone numbers on the survey and researchers screening for previous survey participation.
Survey questions
The survey was prepared in English and translated into Swahili, which is the primary language used by Tanzanians (Supplementary Appendix). Several demographic variables were collected: age, sex, level of education (none, primary, secondary, tertiary level education), first aid training (yes/no), job title, employment status (self-employed vs. employed), experience transporting an injured patient (yes/no), and frequency of transporting (once vs. more than once). The level of education was then categorized into low (none or primary) or high (secondary or college). First aid training refers to a first aid training that is taught to drivers who receive a special license known as a Class C license. Participants were also asked what they thought could be done to improve the transport of trauma patients. We identified three predictor variables: level of education, first aid training, and employment status.
Several survey questions assessed the medical knowledge of transporters, which we considered the principle outcome of our study. First, participants were asked if they were able to recognize if a patient was deceased, alive, or very sick. Second, participants were asked to list signs of the following scenarios: a deceased patient, a very sick patient, and a clinically deteriorating patient. These signs were then compared to a standardized list of five signs for each category, and the number of signs that a participant listed correctly was recorded. Answers were then dichotomized into high (>2 of 5 signs identified) or low (2 or fewer signs identified) scores. No concrete definition was given for “very sick” or “clinically deteriorating” patients.
Educational intervention
Directed by the survey results, we created an educational flier targeted to prehospital transporters. The objective of these fliers was to provide simple, succinct information that may help transporters recognize emergency neurotrauma situations that require expedient transfer to tertiary centers. These fliers were based on Brain Trauma Foundation guidelines and National Institute for Health and Care Excellence (NICE) pathways focusing on prehospital care for both TBI and SCI [12,13,14,15]. Given the widespread use of Swahili and English in Tanzania and other African countries, fliers were created in both languages (Fig. 2a, b).
Statistical analysis
All continuous data was categorized as mean with standard deviation (SD) and median with range where appropriate. Categorical data was described as n (%). The medical knowledge outcomes were then compared between differences in three predictor variables using Chi-square tests: education level, presence of first aid training, and employment status. Predictors of higher scores on the medical knowledge outcomes were assessed with univariate followed by multivariate logistic regression, controlling for age, sex, and prior experience transporting a patient. We controlled for age and sex due to the chance for different educational opportunities, and prior experience because this could impact medical knowledge. Any variable with p < 0.10 on univariate analysis was entered into the multivariate model, and statistical significance was considered at an alpha level of 0.05. All analyses were performed using Statistical Package for Social Sciences (SPSS) Version 26.0.
Results
Demographics and opinions of transporters
A total of 501 participants were included in the survey. Participants were predominantly young (mean: 36.7 years) and male (84.0%). A majority of participants (59.3%) had a high (secondary or tertiary) education level. Thirty-three percent had first aid training and 39.0% were employed. When asked about how to improve the transport of trauma patients, the most common responses were some form of rapid transport (ambulance, helicopter) (33.0%) and increased education for transporters (26.0%) (Table 1).
Medical knowledge of transporters
Overall, 71.3% of participants reported they were able to recognize a deceased patient, while 73.4% reported they could recognize a sick patient. However, when asked to list signs of a deceased patient, signs of a sick patient, and signs of a clinically deteriorating patient, only 13.2%, 14.6%, and 13.0%, respectively, were able to list more than 2 out of 5 standardized signs (Table 2).
Differences in medical knowledge outcomes
The impact of each of the three predictor variables (first aid training, education level, employment status) on medical knowledge is summarized (Tables 3–6).
For the first outcome of identifying a deceased patient, Chi-square tests showed that there was a statistically significant difference between prehospital transporters with and without first aid training being able to correctly list >2 signs of a deceased patient (p = 0.004). There was no difference associated with education level (p = 0.190) or employment status (p = 0.446). First aid training was a significant factor on univariate analysis (p = 0.005), and after controlling for age, sex, and prior experience transporting a patient, multivariate logistic regression still showed that those with first aid training (Odds ratio (OR): 2.3; 95% confidence interval (CI): 1.3, 3.9; p = 0.002) were more likely to correctly list >2 signs of a deceased patient.
For the second outcome of identifying a sick patient, Chi-square tests showed that there were significant differences in correctly listing >2 signs of a sick patient among all three predictors: between prehospital transporters with and without first aid training (p = 0.016), those with different education levels (p = 0.012), and self-employed vs. employed (p = 0.029). All three predictors of education level (p = 0.013), first aid training (p = 0.017), and employment status (p = 0.031) were significant on univariate analysis. After controlling for these three factors as well as age, sex, and prior experience transporting a patient, multivariate logistic regression showed that employed participants (OR: 0.5; 95% CI: 0.3, 0.9; p = 0.021) were less likely to list >2 signs of a sick patient.
For the third outcome of identifying a clinically deteriorating patient, Chi-square tests showed that there were significant differences in correctly listing >2 signs of a clinically deteriorating patient between prehospital transporters with and without first aid training (p < 0.001) as well as those with different education levels (p < 0.001). Univariate analysis showed that education level (p < 0.001) and first aid training (p = 0.001) were significant factors. After controlling for these as well as age, sex, and prior experience transporting a patient, those with higher education level (OR: 2.3; 95% CI: 1.1, 4.8; p = 0.032) were more likely to identify >2 signs of a clinically deteriorating patient.
Discussion
Prehospital care of trauma patients is lacking in many LMICs. Little is known about the medical knowledge of prehospital transporters in LMICs. We sought to characterize the medical knowledge of these transporters and create an educational flier to improve prehospital transporter knowledge as it relates specifically to neurotrauma. Both receiving first aid training and higher education level were significantly associated with multiple medical knowledge outcomes of identifying sick and clinically deteriorating patients. These results suggest that additional education is an important determinant of being able to identify deceased, sick, and clinically deteriorating patients, more than employment status.
It has been shown in a variety of settings that the implementation of a formal prehospital system or additional training in an informal system leads to improved outcomes for trauma patients. In Londrina, Brazil, Marson et al. reported that the implementation of a formal prehospital trauma care system with firemen trained in basic life support and physicians providing advanced life support was associated with decreased mortality before hospital admission, in the first hour after trauma, and after motor vehicle crashes [16]. Stassen et al. in South Africa utilized a free and open online lecture series that led to increased adherence among prehospital providers to prehospital TBI care guidelines [12]. Transitioning to an LMIC setting, Mock et al. implemented a 6-h basic first aid course for commercial drivers in Ghana, and drivers self-reported improvement in crash scene management (including directing traffic to prevent secondary crashes), airway management, external bleeding control, and splinting of injured extremities [17]. Jayaraman et al. also showed that a 1-day basic prehospital trauma course for police, commercial drivers, and community leaders in Kampala, Uganda resulted in sustained knowledge and skill retention at 6 months [18]. These studies agree with our results in showing that a formal training course can lead to increased medical knowledge and improved patient outcomes. Additionally, prehospital transport in Ghana and Uganda is mainly conducted by nonmedical personnel, much like in Tanzania. Still, these interventions largely focus on trauma patients in general and may have overlooked essential prehospital transport measures as they pertain to neurotrauma. Our educational flier was created to address this void in the literature and provide a preliminary intervention to improve prehospital neurotrauma care.
Educational aids such as our proposed pamphlet could improve medical knowledge of prehospital transporters in Tanzania and hopefully improve patient outcomes, especially neurotrauma victims who require emergent transport to a tertiary hospital. The timely transport of neurotrauma patients to a large referral center was underscored by Ahidjo et al. who found that presentation greater than 24 h after injury and multiple hospital admissions were independent predictors of mortality among SCI patients in Nigeria [19]. Additionally, current evidence-based guidelines recommend the immobilization of all acute SCI patients during transport [20]. We hope that our educational flier will prompt quick assessment and proper transportation of SCI patients to appropriate facilities. Although we propose a potential intervention in the form of a flier, additional improvements in SCI patient morbidity and mortality could be achieved through programs such as first aid classes or prehospital care training sessions. The utility of social networks such as WhatsApp to impart knowledge and help organize these programs should also be considered. Further studies assessing the feasibility and benefits of such programs in Dar es Salaam would be beneficial.
Several limitations should be considered in the current study. As with any survey, these are self-reported responses that are subject to great variability. Additionally, the medical knowledge outcomes of identifying >2 out of 5 signs of deceased, sick, or clinically deteriorating patients form an imperfect method of assessing medical knowledge. It is certainly possible that some survey participants had greater knowledge of how to identify deceased, sick, or clinically deteriorating patients but did not list signs that aligned with the 5 standardized signs included in the survey.
Conclusion
In a survey of potential prehospital transporters involved in neurotrauma care in a major East African city, many participants self-reported that they could identify a deceased or sick patient, but few successfully identified multiple signs of deceased, sick, or clinically deteriorating patients. First aid training and higher education levels were significantly associated with improved medical knowledge outcomes. Therefore, we propose the distribution of an educational flier to prehospital transporters to help with the identification of critically ill SCI patients. Further formal training of prehospital transporters in LMICs may improve morbidity and mortality of SCI patients.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
World Health Organization. Injury and violence: the facts 2014. 2014.
Dewan MC, Rattani A, Fieggen G, Arraez MA, Servadei F, Boop FA, et al. Global neurosurgery: the current capacity and deficit in the provision of essential neurosurgical care. Executive Summary of the Global Neurosurgery Initiative at the Program in Global Surgery and Social Change. J Neurosurg. 2018;130:1039–408.
Leidinger A, Kim EE, Navarro-Ramirez R, Rutabasibwa N, Msuya SR, Askin G, et al. Spinal trauma in Tanzania: current management and outcomes. J Neurosurg. 2019;31:1–154.
Moshi H, Sundelin G, Sahlen K-G, Sörlin A. Traumatic spinal cord injury in the north-east Tanzania—describing incidence, etiology and clinical outcomes retrospectively. Glob Health Action. 2017;10:1355604.
Rashid SM, Jusabani MA, Mandari FN, Dekker MCJ. The characteristics of traumatic spinal cord injuries at a referral hospital in Northern Tanzania. Spinal Cord Ser Cases. 2017;3:17021.
Kuzma K, Lim AG, Kepha B, Nalitolela NE, Reynolds TA. The Tanzanian trauma patients’ prehospital experience: a qualitative interview-based study. BMJ Open. 2015;5:e006921.
Malomo TA, Oyemolade TA, Adeleye AO. Determinants of timing of presentation of neurotrauma patients to a neurosurgical center in a developing country. J Neurosci Rural Pract. 2018;9:545–50.
Ram K, VaraPrasad K, Krishna MK, Kannan N, Sundar V, Joseph M, et al. Prehospital factors associated with discharge outcomes: baseline data from the Andhra Pradesh Traumatic Brain Injury Project. World Neurosurg X. 2019;2:100020.
Cnossen MC, van der Brande R, Lingsma HF, Polinder S, Lecky F, Maas AIR. Prehospital trauma care among 68 European Neurotrauma Centers: results of the CENTER-TBI provider profiling questionnaires. J Neurotrauma. 2018;36:176–81.
Faul M, Xu L, Wald M, Coronado V. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Altanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010.
van Adrichem DC, Ratering MRHA, Rashid SM, Jusabani MA, Poppe VE, Mwaitele HA, et al. Penetrating spinal cord injury causing paraplegia in a bird hunter in rural Tanzania. Spinal Cord Ser Cases. 2019;5:49.
Stassen W, Wylie C, Holgate R. An online learning programme improves traumatic brain injury guideline adherence in a South African Helicopter Emergency Medical Service. Afr J Emerg Med. 2015;5:171–5.
Badjatia N, Carney N, Crocco TJ, Fallat ME, Hennes HM, Jagoda AS, et al. Guidelines for prehospital management of traumatic brain injury, 2nd edition. Prehosp Emerg Care. 2008;12:S1–52.
National Institute for Health and Care Excellence. Spinal injury in the pre-hospital setting. Available from: https://pathways.nice.org.uk/pathways/trauma#path=view%3A/pathways/trauma/spinal-injury-in-the-pre-hospital-setting.xml&content=view-info-category%3Aview-about-menu-responsibilities (2019).
National Institute for Health and Care Excellence. Pre-hospital management for patients with head injury. Available from: https://pathways.nice.org.uk/pathways/head-injury#path=view%3A/pathways/head-injury/pre-hospital-management-for-patients-with-head-injury.xml&content=view-index (2019).
Marson AC, Thomson JC. The influence of prehospital trauma care on motor vehicle crash mortality. J Trauma. 2001;50:917–20.
Mock CN, Tiska M, Adu-Ampofo M, Boakye G. Improvements in prehospital trauma care in an African country with no formal emergency medical services. J Trauma. 2002;53:90–7.
Jayaraman S, Mabweijano JR, Lipnick MS, Caldwell N, Miyamoto J, Wangoda R, et al. First things first: effectiveness and scalability of a basic prehospital trauma care program for lay first-responders in Kampala, Uganda. PLoS ONE 2009;4:e6955.
Ahidjo KA, Olayinka SA, Ayokunle O, Mustapha AF, Sulaiman GA, Gbolahan AT. Prehospital transport of patients with spinal cord injury in Nigeria. J Spinal Cord Med. 2011;34:308–11.
Theodore N, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, Rozzelle CJ, et al. Transportation of patients with acute traumatic cervical spine injuries. Neurosurgery. 2013;72:35–9.
Tanzania GIS User Group. TanRoads PDF overview map of roads in Dar es Salaam. http://www.tzgisug.org/wp/tzgisug-website-a-spatial-data-repositorum-or-not/tanroads_dar_es_salaam_pdf/.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lan, M., Lessing, N.L., Nyamsaya, S. et al. Prehospital care of trauma patients in Tanzania: medical knowledge assessment and proposal for safe transportation of neurotrauma patients. Spinal Cord Ser Cases 6, 32 (2020). https://doi.org/10.1038/s41394-020-0280-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-020-0280-y