Abstract
Study design
A cross-sectional study.
Objective
To investigate the correlations between gut microbiota and metabolic parameters in people with different levels of chronic spinal cord injury (SCI).
Setting
An SCI-specialized rehabilitation facility in a university hospital.
Methods
Forty-three participants with chronic SCI were recruited. Blood samples of each participant were collected for analysis of metabolic parameters. Feces were collected after the bowel opening method the patient routinely uses to evaluate fecal bacterial microbiota using quantitative RT-PCR. Body composition was examined using dual-energy x-ray absorptiometry (DEXA). Data were analyzed to evaluate the correlations between gut microbiota and other parameters.
Results
Of the 43 participants, 31 people (72.1%) were paraplegic and 12 people (27.9%) tetraplegic. Thirty-two people (74.4%) were diagnosed with obesity using the percentage of body fat (% body fat) criteria. The mean (SD) ratio of Firmicutes:Bacteroides (F/B), which represents the degree of gut dysbiosis, was 18.3 (2.45). Using stepwise multivariable linear regression analysis, both having tetraplegia and being diagnosed with obesity from % body fat evaluated by DEXA were independent positively-correlating factors of F/B (p < 0.001 and p = 0.001, respectively), indicating more severe gut dysbiosis in people with tetraplegia than paraplegia.
Conclusion
In people with chronic SCI, having tetraplegia and being diagnosed with obesity from % body fat evaluated by DEXA are independent positive-correlating factors of gut dysbiosis. These results indicate a significant association between gut microbiota and the characteristics of SCI as well as metabolic parameters.
Similar content being viewed by others
Introduction
Currently, cardiovascular disease (CVD) is the most common cause of death in people with chronic SCI [1]. Compared with the age-matched general population, people with chronic SCI also have a higher prevalence of CVD and its metabolic risk factors, including obesity, hypertension, diabetes, obesity, and metabolic syndrome (MetS), especially those with tetraplegia [2]. Recently, gut dysbiosis or abnormal gut microbiota, the small microorganisms living in human intestines, has been shown to be associated with the development of obesity in able-bodied people [3,4,5,6]. Gut dysbiosis is described by an increase in the ratio of gram-positive bacteria in the phylum Firmicutes to gram-negative bacteria in the phylum Bacteroidetes (F/B) [7]. This is in addition to an increase in the percentage of gram-negative lipopolysaccharide (LPS)-producing bacteria in the family Enterobacteriaceae of the phylum Proteobacteria [8]. Previous studies have demonstrated that people with SCI have alterations in gut microbiota in comparison to able-bodied age-matched controls [9, 10]. Another study demonstrated an association between gut microbiota and serum lipid profiles [11], and another found a correlation between the microbiota and neurogenic bowel parameters [12] in males with SCI.
Control of bowel function depends on both the enteric and autonomic nervous systems [13]. The autonomic nervous system controls the enteric nervous system by fine-tuning, not by directly affecting motility and secretory functions [13, 14]. After SCI, axons that normally control spinal sympathetic neurons are damaged, resulting in abnormalities in gut motility, mucosal secretions, vascular tone, and immune function [15]. This impaired homeostasis can disrupt the ecological balance of microorganisms in the gut, resulting in gut dysbiosis [16]. Interestingly, pre-clinical evidence from an investigation in a mouse model demonstrated that sympathetic tone of the body was a factor affecting gut dysbiosis [17]. Therefore, it could be proposed that people with tetraplegia (neurological level of injury [NLI] at or above C8), who totally lose the sympathetic control of the entire body, should have a greater increase in gut dysbiosis when compared with people with paraplegia (NLI at or below T1), who partially lose the sympathetic control of the entire body. A previous clinical study investigating gut microbiota profiles in acute SCI patients also demonstrated that the level of SCI was positively correlated with the degree of gut dysbiosis [18]. However, to date there have been no clinical studies to investigate the effect of the level of SCI (for example having tetraplegia or high paraplegia) on gut microbiota in people with chronic SCI. Therefore, the hypotheses of this study were that 1) people with tetraplegia have more severe gut dysbiosis when compared with people with high and low paraplegia, and 2) the level of SCI is an independent factor showing a positive correlation with gut dysbiosis after adjusting for other demographic and lifestyle parameters, and also metabolic status in people with chronic SCI.
Methods
Study design
This is a cross-sectional etiologic study with prospective data collection. The study protocol was approved by the Institutional Ethics Committee of the Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand (study number REH-2561-06025).
Participants
We included participants who: 1) were diagnosed with traumatic spinal cord injury; 2) were aged between 18-65 years; 3) were able to communicate; 4) had onset of SCI for more than 1 year. Exclusion criteria were: people who were diagnosed with or had a history of diagnosis of the condition which could potentially disturb gut microbiota status, including coronary artery diseases, cerebrovascular diseases, peripheral arterial diseases, antibiotic-associated colitis, inflammatory bowel diseases, irritable bowel syndrome, and malignancy of gastrointestinal tract, having a history of steroid drug use in any context within the month prior to enrolment, or currently using antibiotic drugs within the 28 days prior to the stool collecting date. After performing a pilot study with 6 paraplegic and 4 tetraplegic people, the mean (SD) of F/B of paraplegic and tetraplegic people was 20.12 (10.05) and 38.23 (20.34), respectively. Therefore, the recommended sample size for testing two independent means [19], was at least 12 people per group.
Study protocol
After informed consent, epidemiologic and medical history data of the participants were collected in line with the International Spinal Cord Injury (ISCI) Basic Data Set [20]. Neurogenic bowel dysfunction type and bowel management data were determined using the ISCI Bowel Data Set [21]. Since a previous study demonstrated that using rectal enema affected gut microbiota profiles [22], participants were also categorized into an enema-using group (including both large volume and mini-enema), and a non-enema-using group (voluntary defecation or manual evacuation). Since diet and physical activity are known to affect the gut microbiota, a specific questionnaire intending to explore these two factors was designed and used (Supplementary Data). Anthropologic parameters, including height and body weight, were measured then a body mass index was calculated. Metabolic parameters, including fasting plasma glucose (FPG), lipid profile (triglycerides, total cholesterol, HDL-C and LDL-C), were evaluated. Feces of each participant were collected from samples from the bowel opening method the patient routinely uses to evaluate fecal bacterial microbiota. Body composition was examined using dual-energy x-ray absorptiometry (DEXA) within 24 h after the blood and the feces were collected.
Gut microbiota analysis
Feces of each participant were collected then bacterial genomic DNA was extracted using a commercial genomic DNA isolation kit (QIAGEN, Germany). Briefly, the fecal sample (0.25 g) was homogenized in QIAGEN ASL lysis buffer using a Minibeadbeater (BioSpec Products, Bartlesville, USA). The extraction of bacterial genomic DNA was carried out following the manufacturer’s instructions. The fractions of the bacterial microbiota population were quantified using real-time quantitative reverse transcription PCR (qRT-PCR) as described previously [23]. Briefly, extracted bacterial genomic DNA was diluted at 1:10 and 0.04 mL was used as the template for SYBR-Green-based (SensiFAST SYBR Lo-ROX kit, Bioline, Taunton, MA) real-time polymerase chain reaction using the corresponding primers. The gene copy numbers of each bacterial population were determined based on standard curves that were generated from fragments of bacterial 16 S rRNA genes; Eubacteria: Ruminococcus. productus (ATCC 27340 D), Clostridiales: Ruminococcus. productus (ATCC 27340 D), Lactobacillales/Bacillales: Lactobacillus acidophilus (ATCC 4357 D), Bacteroidetes/Actinobacteria: Bacteroides fragilis (ATCC 25285 D), and Enterobacteriaceae: Escherichia coli K-12 (TOP10) cloned into pCR2.1 (TOPO TA cloning kit, Invitrogen, Carlsbad, CA) as templates [23]. The percentage of Firmicutes was calculated from qPCR as a combination between Clostridiales and Lactobacillales/Bacillales using standard curves that were generated by pSW192 and pSW193. The percentage of each bacterial phylum was determined by dividing the gene copy number of each bacterial phylum by the total gene copy number determined using the universal primers previously described [23].
Dual-energy X-ray absorptiometry
The Nebula model of Hologic DEXA machine (Marlborough, Massachusetts, USA) was used to measure body composition in all participants. Every effort was taken to mimic the positioning of the original participants on the scanner for all measurements [24]. Obesity was diagnosed using the following criteria: % body fat ≥ 25% in males or % body fat ≥ 32% in females [25].
Diagnosis of metabolic syndrome
In accordance with the American Heart Association (AHA)/The National Cholesterol Education Program (NCEP) III Guidelines for Diagnosis of Metabolic Syndrome, MetS was diagnosed when three or more of the following criteria were met: hypertension (blood pressure [BP] more than or equal to 130/85 mmHg, or using antihypertension medication), central obesity [waist circumference > 40 inches/102 cm in men or > 35 inches/88 cm] in women, impaired fasting glucose [FPG more than or equal to 100 mg/dl, or use of medication for treating hyperglycemia], fasting hypertriglyceridemia TG more than or equal to 150 mg/dl, and low high-density lipoprotein cholesterol [HDL-C < 40 mg/dl in men or < 50 mg/dl in women] [26]. In males, central obesity was also diagnosed using the SCI-specific cut-off level (86.5 cm), which was proposed by Gill, et al. (2020) [27]. MetS was also diagnosed using data of central obesity categorized using the SCI-specific criteria.
Statistical analysis
Categorical variables were described using frequency and percentages. Normally-distributed numerical variables were presented using arithmetic means and standard deviations (SD). Non-normally distributed variables were modified by taking a natural logarithm and then were presented using geometric mean and SD. The correlations between gut microbiota (continuous parameters) and each demographic, SCI-related, metabolic parameter were determined using univariable linear regression analysis. The multivariable linear regression analysis was then used to determine whether being tetraplegic is an independent correlating factor of gut microbiota by controlling all other demographic, SCI-related, and metabolic confounding metabolic parameters. Statistical analyses were performed using SPSS version 24.0 for Windows (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Results
Demographic parameters of all participants
Table 1 shows the demographic data of the participants. Out of the 60 people with chronic SCI preliminarily recruited in this study, 43 people had complete data of all the blood and stool samples, and from DEXA testing. Therefore, only data from these 43 people were analyzed. Of the 43 participants, 28 people (65%) were male; the mean (SD) age was 44.4 (11.1) years; the median (IQR) duration of the SCI of the participants was 13 (19) years and 25 (58%) people had been living with SCI for more than 10 years. Regarding the characteristics of SCI, 31 people (72%) had paraplegia and 12 people (28%) had tetraplegia. Thirty-two people (74%) had complete SCI and 11 people (26%) had incomplete SCI. Comparison of the participants with tetraplegia and those with paraplegia, showed that the tetraplegic group was younger, and the duration of having SCI was shorter. In addition, there were more people with complete injury in the tetraplegic group when compared with the paraplegic group.
Lifestyle parameters
Table 1 shows lifestyle parameters including the neurogenic bowel dysfunction status of the participants. Regarding the type of neurogenic bowel dysfunction, 28 people (66.1%) had a reflexic bowel and 15 people (34.9%) had the areflexic type. Twenty-four (56%) used a rectal mini enema for bowel opening management, whereas 17 participants (40%) used voluntary defecation or manual evacuation, and 2 participants (5%) had a colostomy. No participants used suppository medication as a bowel opening method. Regarding the use of oral laxatives, 10 participants (23%) regularly used senna laxative medications at least once a week, whereas 33 participants (77%) did not. No participant reported using other laxative medication. With regard to the frequency of bowel opening, 15 people (35%) opened their bowels every day whereas 28 people (69%) did not. Focusing on diet consumption, the most common type of diet the participants consumed was carbohydrate-based (45.2%), followed by protein (22.9%), vegetables and fruits (22.4%), and fat (9.4%). Regarding independent mobility, 27 participants (63%) could be independently mobile, as indicated by being able to walk independently or manually propel a wheelchair, whereas 16 participants (37%) could not. Predictably, there was a significantly higher frequency in the paraplegic group with lower motor neuron type neurogenic bowel dysfunction in comparison to the tetraplegic group.
Metabolic parameters
Table 2 shows the metabolic parameters of the participants. The mean % body fat of the participants was 31.8% (SD = 7.4). According to the guidelines for the diagnosis of obesity from % body fat, 32 people (74%) were diagnosed as obese (75% male and 73% female participants). The mean (SD) body mass index of the participants was 21.05 (4.34). According to the guidelines for the diagnosis of obesity from the BMI in people with chronic SCI (BMI more than 22.0 kg/m2) [28], 15 people (35%) were diagnosed with obesity. According to the AHA/NCEP III Guidelines for Diagnosis of Metabolic syndrome, 5 people (12%) were diagnosed with hypertension, 11 people (26%) were diagnosed with central obesity, 9 people (21%) were diagnosed with impaired fasting glucose, 8 people (19%) were diagnosed with fasting hypertriglyceridemia, 17 people (40%) were diagnosed with low HDL cholesterol, and 10 people (23%) were diagnosed with MetS. When using the SCI-specific cut-off level for diagnosing central obesity in males, 13 participants (30%) were diagnosed with central obesity and 12 participants (28%) were diagnosed with MetS. It is noteworthy that there are no detectable differences in metabolic parameters between the tetraplegic group and the paraplegic group.
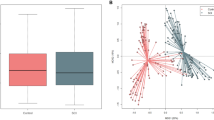
Profiles of gut microbiota and their correlations to the other parameters
The most prevalent gut microbiota of people with chronic SCI in this study was Firmicutes (mean percentage = 83.9%, SD = 6.3), followed by Bacteroides (mean percentage = 7.7%, SD = 6.2). The geometric mean (SD) of the ratio between Firmicutes:Bacteroides (F/B) was 18.3 (2.45). The geometric mean (SD) of the percentage of the Enterobacteriaceae-family bacteria was 0.017 (0.013)%. Focusing on the correlations between F/B and other parameters, using univariable analysis, people with tetraplegia had significantly higher F/B when compared with those with paraplegia (p = 0.003; linear regression analysis) (Fig. 1). People with chronic SCI and obesity indicated by % fat from DEXA (% body fat ≥ 25% in males or % body fat ≥ 32% in females [25]) also had significantly a higher F/B when compared with those without obesity (p = 0.003; linear regression analysis) (Fig. 2). People who regularly used laxative medications had significantly higher F/B when compared with those who did not use them (p = 0.015; linear regression analysis). Physically inactive people had significantly higher F/B when compared with those who were physically active (p = 0.009; linear regression analysis). There were no significant correlations between F/B and age, or with percentage of fats, carbohydrates, proteins, and fruit/vegetable intake (all p > 0.05; linear regression analysis). No significant difference in F/B was found between each of the following comparisons: 1) males and females with chronic SCI; 2) those who had a complete and incomplete lesion; 3) those who had reflexic and areflexic type of neurogenic bowel dysfunction; 4) those who used rectal enema and did not use on; 5) those who had a colostomy and did not have one; 6) those who opened their bowel every day against less frequent than every day; 7) those who had SCI less than or equal to 10 years against more than 10 years; 7) those who were diagnosed and who were not diagnosed with hypertension, impaired fasting glucose, fasting hypertriglyceridemia, low HDL cholesterol, or central obesity, and who were diagnosed with MetS and were not diagnosed with MetS by both the AHA/NCEPIII and the SCI-specific criteria (p > 0.05; linear regression analysis in each comparison). Focusing on the correlations between the percentage of the Enterobacteriaceae-family bacteria and the other parameters, no significant correlation was found (all p > 0.05, linear regression analysis). Table 3 demonstrates the correlations between F/B and demographic, lifestyle, and metabolic parameters.
Using a stepwise multivariable linear regression analysis adjusted for sex, age, level of SCI, the completeness of SCI, type of neurogenic bowel dysfunction, use of oral laxative medications, being physically inactive, using rectal enema as a bowel opening method, diagnosis of hypertension, impaired fasting glucose, fasting hypertriglyceridemia, low HDL cholesterol, central obesity, obesity by using BMI criteria, and MetS by both the NCEPIII and the SCI-specific criteria, having tetraplegia was still an independently positive-correlating factor of F/B (p < 0.001), together with being diagnosed with obesity from % body fat by DEXA (p = 0.001) (Unstandardized coefficient [B] = 0.93 with 95% CI 0.44–1.41; standardized coefficient [β] = 0.470 and B = 0.88 with 95% CI 0.38–1.374; β = 0.433, respectively).
Discussion
The major findings of this study were that, in people with chronic SCI, the level of the injury (having tetraplegia or paraplegia) is an independent positive-correlating factor of gut dysbiosis indicated by an increased fecal F/B after adjusting for all demographic and lifestyle parameters, as well for metabolic status. A second factor is being diagnosed with obesity from % body fat by DEXA. These results indicate a significant relationship between gut microbiota and the characteristics of SCI as well as metabolic parameters. However, some interesting points need to be discussed before translating these findings into daily clinical practices.
The correlation between the level of SCI and profiles of gut microbiota
We found that having tetraplegia was positively correlated with a higher F/B, which indicates a higher degree of gut dysbiosis. To all our knowledge, our study is the first study to demonstrate this correlation in people with chronic SCI. Our findings are compatible with those results from a previous clinical study which demonstrated the severity of SCI, using the level and American Spinal Injury Association (ASIA) Impairment Scale (AIS) to be subcategorized as severe SCI (motor complete tetraplegia and motor complete high paraplegia) and less severe SCI (motor complete low paraplegia and motor incomplete SCI), was correlated with gut microbiota profiles [18]. We have also subcategorized the participants into 4 groups, specifically complete tetraplegia, incomplete tetraplegia, complete paraplegia, and incomplete paraplegia. However, the sample size of 3 out of the 4 groups is very small (7 for complete tetraplegia, 5 for incomplete tetraplegia, 26 for complete paraplegia, and 5 for incomplete paraplegia). Therefore, no significant difference in F/B between those with complete and incomplete tetraplegia, as well as those with complete and incomplete paraplegia could be confidently accepted (p > 0.05; one-way ANOVA followed by Turkey post-hoc analysis). Increasing the sample size in each group would be essential in any future study to confirm the present findings. We propose two rationales to explain our findings. First, there is a significant difference in physical activity between those with tetraplegia and paraplegia. Evidence shows that the level of physical activity showed a negative correlation with the degree of gut dysbiosis, indicated by increased F/B [29, 30]. However, when adjusted by the physical activity factor using specific criteria (independently mobile - walking or manual propelling a wheelchair as a main mobility method), having tetraplegia was still an independently positive-correlating factor of F/B. Therefore, levels of physical activity alone could not be completely responsible for the effect having tetraplegia had on gut dysbiosis. Noteworthy in this study is we did not directly assess the level of physical activity and using the term independently mobile might be confounded by the completeness of injury factor since people with incomplete SCI have a higher probability of being able to walk independently when compared with those with complete SCI. Another possible explanation of this result is the difference in the loss of sympathetic control of the entire body, which is compatible with the results of the pre-clinical evidence [17]. Since we investigated only some parameters of gut microbiota (e.g., F/B) and did not compare gut microbiota profiles between people with SCI and able-bodied subjects, our results should not be over-interpreted as there was no gut dysbiosis in people with paraplegia.
The correlation between metabolic parameters and profiles of gut microbiota
Secondly, the positive correlation between the obesity and F/B is comparable with the results from previous studies in both animal [31] and clinical models [7, 32]. For example, Kolida et al. (2017) demonstrated that people in the general population who had F/B more than or equal to 1 had a significantly higher risk of being overweight with an odds ratio of 1.33 [7]. Previous in vivo studies also demonstrated an increase in the Firmicutes:Bacteroides ratio in feces from high-fat diet-induced obese-insulin resistant rats when compared with those from non-obese rats [31]. However, to our knowledge, our study is the first to demonstrate a correlation between obesity and gut dysbiosis in people with chronic SCI.
Although the correlations between the percentage of Enterobacteriaceae and metabolic parameters are indicated in studies in able-bodied subjects, there is no correlation between the percentage of Enterobacteriaceae and metabolic parameters, as well as SCI characteristics in this study. The cause of these surprising findings is unknown, but it might be due to the confounding factors which are presented exclusively in people with SCI. For example, a previous study showed increased colonization of Klebsiella pneumoniae, which is a member of the Enterobacteriaceae Family, in the urethra and perineum of people with chronic SCI [33]. This abnormal translocation of gut microbiota might change the characteristics of the Enterobacteriaceae gut microbiota resulting in an absence of the correlation between Enterobacteriaceae and other parameters in people with SCI. In addition, the present study has only the results of bacterial phylum, a further metagenomic study to investigate the details of profiles in gut microbiota at levels of families, genus, orders, and species of bacteria is warranted to confirm these findings.
With regard to the mechanisms explaining the positive correlation between F/B and obesity, this might be due to the difference in energy production properties between Firmicutes and Bacteroides bacteria. Previous studies demonstrated that Firmicutes had a more pronounced ability for metabolizing undigested, non-absorptive carbohydrates into absorptive, energy-rich molecules such as short-chain fatty acids (SCFAs) than Bacteroides [34, 35]. Since Firmicutes and Bacteroides are the two most common phyla of bacteria in the gut, responsible for 80–90% of the colonic microbiota [36], a change in the ratio between them might produce a pronounced effect on the host metabolism.
Limitations
The limitations of this study are the relatively small sample size, the interview bias, and the cross-sectional study design but also, as previously mentioned, we only evaluated gut microbiota to phylum level, which would potentially have too low a sensitivity to detect a change in family, order, or genus level. A further study investigating gut microbiota at family, order, or genus level by using more advanced technology such as sequencing targeting the V3-V4 region of the 16 S ribosomal RNA (rRNA) gene or metaproteomics [10, 37], might bring us further understanding of the function of microbes to develop targeted microbiome treatments in clinical settings. Previously, Zhang, et al. reported a significant correlation between defecation time and gut microbial community structure [11], as well as describing a significant correlation between serum lipid profile and the gut microbiota genera Faecalibacterium, Megamonas, and Prevotella, and between glucose levels and the gut microbiota genus Lactobacillus in males with SCI [10]. Differences in the study populations (both sexes in this study compared with solely males in the other studies), as well as differences in the levels of gut microbiota detection (phylum level in this study vs genus level in the other studies), might be responsible for any inconsistency.
Another limitation of this study is the questionable accuracy of the tools for detecting dietary and physical activity data, which might be responsible for an absence of the significant correlations between dietary lifestyles and gut microbiota profiles despite being described in many studies [31, 38, 39]. There are validated tools for the evaluation of dietary data [40], and physical activity [41, 42]. Since dietary and physical activity data are affected by cultures, some parameters (such as choices of diet) in the Western country-developing questionnaires are not understandable in a Thai context, as well as some parameters being missed. At present, there has been no validated cross-cultural translation of these standard tools for evaluation of dietary and physical activity in our language. Therefore, we decide to refrain from using these standard questionnaires and use our specifically developed questionnaire for the collection of dietary data, as well as using more observable data (having the ability to walk independently or manually propel a wheelchair) and report them as the ability to be independently mobile. Although this parameter was not a valid surrogate outcome for detecting physical activity levels, it was the only parameter related to physical activity, which is one of the determining factors of gut microbiota in this study.
Next, gut dysbiosis is only a surrogate outcome of cardiovascular and metabolic problems, not a true clinical endpoint. Further prospective cohort studies, aiming to compare gut microbiota, rate, and time to developing cardiovascular events between people with SCI and a control group of able-bodied people matched for other characteristics, are needed especially in people with tetraplegia who are at the highest risk of developing CVD and gut dysbiosis. Also, further studies are needed to investigate whether these correlations contribute to the premature development of cardiovascular and metabolic diseases in people with SCI.
Clinical Implications
Gut dysbiosis can be defined as an increase in the ratio of gram-positive bacteria in the phylum Firmicutes to gram-negative bacteria in the phylum Bacteroidetes (F/B) [7]. Our study demonstrated an increased F/B in people with SCI who lived with tetraplegia or were diagnosed with obesity. Therefore, among the chronic SCI population, people with chronic tetraplegia have the highest risk of gut dysbiosis, which might contribute to the premature development of cardiovascular risk factors and diseases. Another risk of gut dysbiosis demonstrated in this study is obesity. Therefore, people with SCI, especially those with tetraplegia should act appropriately to prevent and treat obesity to avoid additional risks of gut dysbiosis. Other risks of gut dysbiosis, including alcohol intake, smoking, and antibiotic overuse [43], should also be avoided in people with SCI who live with tetraplegia with or without obesity. Future studies to prove the efficacy of available treatment, such as the use of probiotics and prebiotics, for attenuating gut dysbiosis and/or the development of cardiovascular risks and events in the SCI population are needed.
Conclusion
In people with chronic SCI, being tetraplegic and being diagnosed with obesity from % body fat by DEXA are independent positively-correlating factors of gut dysbiosis indicated by increased F/B. These results indicate a significant association between gut microbiota and the characteristics of SCI as well as metabolic parameters.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. 2005;43:408–16.
Myers J, Lee M, Kiratli J. Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med rehabilitation. 2007;86:142–52.
Shen J, Obin MS, Zhao L. The gut microbiota, obesity and insulin resistance. Mol Asp Med. 2013;34:39–58.
Fei N, Zhao L. An opportunistic pathogen isolated from the gut of an obese human causes obesity in germfree mice. ISME J. 2013;7:880–4.
Vrieze A, Van Nood E, Holleman F, Salojarvi J, Kootte RS, Bartelsman JF, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143:913–6.e7.
Fukuda S, Ohno H. Gut microbiome and metabolic diseases. Semin Immunopathol. 2014;36:103–14.
Koliada A, Syzenko G, Moseiko V, Budovska L, Puchkov K, Perederiy V, et al. Association between body mass index and Firmicutes/Bacteroidetes ratio in an adult Ukrainian population. BMC Microbiol. 2017;17:120.
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–72.
Gungor B, Adiguzel E, Gursel I, Yilmaz B, Gursel M. Intestinal microbiota in patients with spinal cord injury. PLoS ONE. 2016;11:e0145878.
Lin R, Xu J, Ma Q, Chen M, Wang L, Wen S, et al. Alterations in the fecal microbiota of patients with spinal cord injury. PLoS ONE. 2020;15:e0236470.
Zhang C, Jing Y, Zhang W, Zhang J, Yang M, Du L, et al. Dysbiosis of gut microbiota is associated with serum lipid profiles in male patients with chronic traumatic cervical spinal cord injury. Am J Transl Res. 2019;11:4817–34.
Zhang C, Zhang W, Zhang J, Jing Y, Yang M, Du L, et al. Gut microbiota dysbiosis in male patients with chronic traumatic complete spinal cord injury. J Transl Med. 2018;16:353.
Durney P, Stillman M, Montero W, Goetz L. A primary care provider’s guide to neurogenic bowel dysfunction in spinal cord injury. Top spinal cord Inj Rehabilitation. 2020;26:172–6.
Mayer EA. Gut feelings: The emerging biology of gut-brain communication. Nat Rev Neurosci. 2011;12:453–66.
Kigerl KA, Hall JC, Wang L, Mo X, Yu Z, Popovich PG. Gut dysbiosis impairs recovery after spinal cord injury. J Exp Med. 2016;213:2603–20.
Kigerl KA, Zane K, Adams K, Sullivan MB, Popovich PG. The spinal cord-gut-immune axis as a master regulator of health and neurological function after spinal cord injury. Exp Neurol. 2020;323:113085.
Robles-Vera I, Toral M, Duarte J. Microbiota and Hypertension: Role of the Sympathetic Nervous System and the Immune System. Am J Hypertens. 2020;33:890–901.
Bazzocchi G, Turroni S, Bulzamini MC, D’Amico F, Bava A, Castiglioni M, et al. Changes in gut microbiota in the acute phase after spinal cord injury correlate with severity of the lesion. Sci Rep. 2021;11:12743.
Dupont WD, Plummer WD Jr. Power and sample size calculations. A review and computer program. Control Clin Trials. 1990;11:116–28.
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
Krogh K, Perkash I, Stiens SA, Biering-Sorensen F. International bowel function basic spinal cord injury data set. Spinal Cord. 2009;47:230–4.
Furuta A, Suzuki Y, Takahashi R, Jakobsen BP, Kimura T, Egawa S, et al. Effects of Transanal Irrigation on Gut Microbiota in Pediatric Patients with Spina Bifida. J Clin Med. 2021;10:224.
Winter SE, Thiennimitr P, Winter MG, Butler BP, Huseby DL, Crawford RW, et al. Gut inflammation provides a respiratory electron acceptor for Salmonella. Nature. 2010;467:426–9.
Gorgey AS, Martin H, Metz A, Khalil RE, Dolbow DR, Gater DR. Longitudinal changes in body composition and metabolic profile between exercise clinical trials in men with chronic spinal cord injury. J Spinal Cord Med. 2016;39:699–712.
Myung J, Jung KY, Kim TH, Han E. Assessment of the validity of multiple obesity indices compared with obesity-related co-morbidities. Public Health Nutr. 2019;22:1241–9.
Grassi G, Seravalle G, Quarti-Trevano F, Dell’Oro R, Bombelli M, Mancia G. Metabolic syndrome and cardiometabolic risk: An update. Blood Press. 2009;18:7–16.
Gill S, Sumrell RM, Sima A, Cifu DX, Gorgey AS. Waist circumference cutoff identifying risks of obesity, metabolic syndrome, and cardiovascular disease in men with spinal cord injury. PLoS ONE. 2020;15:e0236752.
Silveira SL, Ledoux TA, Robinson-Whelen S, Stough R, Nosek MA. Methods for classifying obesity in spinal cord injury: a review. Spinal Cord. 2017;55:812–7.
de Sire A, de Sire R, Petito V, Masi L, Cisari C, Gasbarrini A, et al. Gut-Joint Axis: The role of physical exercise on gut microbiota modulation in older people with osteoarthritis. Nutrients. 2020;12:574.
Motiani KK, Collado MC, Eskelinen JJ, Virtanen KA, LÖyttyniemi E, Salminen S, et al. Exercise training modulates gut microbiota profile and improves endotoxemia. Med Sci Sports Exerc. 2020;52:94–104.
Saiyasit N, Chunchai T, Prus D, Suparan K, Pittayapong P, Apaijai N, et al. Gut dysbiosis develops before metabolic disturbance and cognitive decline in high-fat diet-induced obese condition. Nutrition. 2020;69:110576.
Jasirwan COM, Muradi A, Hasan I, Simadibrata M, Rinaldi I. Correlation of gut Firmicutes/Bacteroidetes ratio with fibrosis and steatosis stratified by body mass index in patients with non-alcoholic fatty liver disease. Biosci Microbiota Food Health. 2021;40:50–58.
Montgomerie JZ, Gilmore DS, Ashley MA, Schick DG, Jimenez EM. Long-term colonization of spinal cord injury patients with Klebsiella pneumoniae. J Clin Microbiol. 1989;27:1613–6.
Krajmalnik-Brown R, Ilhan ZE, Kang DW, DiBaise JK. Effects of gut microbes on nutrient absorption and energy regulation. Nutr Clin Pract: Off Publ Am Soc Parenter Enter Nutr. 2012;27:201–14.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31.
Donaldson GP, Lee SM, Mazmanian SK. Gut biogeography of the bacterial microbiota. Nat Rev Microbiol. 2016;14:20–32.
Allaband C, McDonald D, Vázquez-Baeza Y, Minich JJ, Tripathi A, Brenner DA, et al. Microbiome 101: Studying, Analyzing, and Interpreting Gut Microbiome Data for Clinicians. Clin Gastroenterol Hepatol. 2019;17:218–30.
Ngowi EE, Wang YZ, Khattak S, Khan NH, Sayed Mohamed Mahmoud S, Helmy Y, et al. Impact of the factors shaping gut microbiota on obesity. J Appl Microbiol. 2021;31:2131–47.
Overby HB, Ferguson JF. Gut microbiota-derived short-chain fatty acids facilitate microbiota: Host cross talk and modulate obesity and hypertension. Curr Hypertens Rep. 2021;23:8.
Pannucci TE, Thompson FE, Bailey RL, Dodd KW, Potischman N, Kirkpatrick SI, et al. Comparing reported dietary supplement intakes between two 24-Hour recall methods: The automated self-administered 24-Hour dietary assessment tool and the interview-administered automated multiple pass method. J Acad Nutr Diet. 2018;118:1080–6.
Martin Ginis KA, Phang SH, Latimer AE, Arbour-Nicitopoulos KP. Reliability and validity tests of the leisure time physical activity questionnaire for people with spinal cord injury. Arch Phys Med rehabilitation. 2012;93:677–82.
Ginis KA, Latimer AE, Hicks AL, Craven BC. Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc. 2005;37:1099–111.
El-Sayed A, Aleya L, Kamel M. Microbiota and epigenetics: Promising therapeutic approaches? Environ Sci Pollut Res Int. 2021;28:49343–61.
Acknowledgements
A part of this study was presented at the International Spinal Cord Society (ISCoS) 60th Annual Scientific Meeting (ISCoS 2021: VIRTUAL) on 29 September - 2 October 2021 and was nominated an Early Career Scholar Awardee.
Funding
This work was supported by the Senior Research Scholar grant from the National Research Council of Thailand (SCC), a Thailand Research Fund grant MRG6210062 (SP), an NSTDA Research Chair Grant from the National Science and Technology Development Agency Thailand (NC), a Chiang Mai University Center of Excellence Award (NC), and a Faculty of Medicine Chiang Mai University Research Grant No. 028-2563/0 (SP).
Author information
Authors and Affiliations
Contributions
SP, NC, and SC designed the study and contributed essential materials and reagents; SP, TK, and. NS performed the research; SP, TK, NC, and SC analyzed the data; SP, TK, SC, and NC wrote and revised the manuscript; SC and NC critically reviewed the manuscript. All authors reviewed the final manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Pattanakuhar, S., Kaewchur, T., Saiyasit, N. et al. Level of injury is an independent determining factor of gut dysbiosis in people with chronic spinal cord injury: A cross-sectional study. Spinal Cord 60, 1115–1122 (2022). https://doi.org/10.1038/s41393-022-00832-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00832-8