Abstract
Study design
Prospective multi-center trial.
Objectives
To characterize the complication profile associated with modest systemic hypothermia after acute cervical SCI in a prospective multi-center study.
Setting
Five trauma centers in the United States.
Methods
We analyzed data from a prospective, multi-center trial on the use of modest systemic hypothermia for acute cervical SCI. Patients with acute cervical SCI were assigned to receive modest systemic hypothermia (33 C) or standard of care medical treatment. Patients in the hypothermia group were cooled to 33 C and maintained at the target temperature for 48 h. Complication profile and the rate of complications within the first 6 weeks after injury were compared between the two groups. Multiple regression analysis was performed to determine risk factors for complications after injury.
Results
Fifty patients (hypothermia: 27, control: 23) were analyzed for this study. Median age was significantly lower in the hypothermia arm (39 vs 59 years, p = 0.02). Respiratory complications were the most common (hypothermia: 55.6% vs control: 52.2%, p = 0.81). The rate of deep vein thrombosis was not significantly different between the two groups (hypothermia: 14.8% vs control 17.4%, p = 0.71). The rate of complications was not statistically different between the two groups.
Conclusion
In this prospective multi-center controlled trial, preliminary data show that modest systemic hypothermia was not associated with increased risk of complications within the first 6 weeks after acute cervical SCI.
Trial information
The study is registered on clinicaltrials.gov NCT02991690. University of Miami IRB (Central IRB) approval No.: 20160758. Emory University IRB #IRB00093786.
Similar content being viewed by others
Introduction
Systemic hypothermia is a neuroprotective technique that reduces secondary injury to the central nervous system [1]. Pre-clinical studies show that systemic hypothermia reduces metabolic activity and energy consumption in tissues [2] as well as ameliorates local inflammation and oxidative stress after injury [3]. In the central nervous system, hypothermia can reduce glutamate toxicity as well as the release of inflammatory cytokines [4]. Together, systemic hypothermia demonstrates a promising role in the treatment of central nervous system injury, such as acute spinal cord injury (SCI).
Modest systemic hypothermia (32–34 C) after acute traumatic cervical SCI is feasible in the clinical setting [5,6,7]. Hypothermia can be initiated within a few hours of the injury and surgical interventions, if needed, can be performed during hypothermia [5]. Adverse events associated with systemic hypothermia after acute cervical SCI have been described from a single center with extensive experience with this technique [5,6,7]. Data from a prospective, multi-center case control study is necessary to determine the unique adverse event profile of therapies for SCI [8]. This may help physicians better anticipate clinical challenges associated with systemic hypothermia for acute cervical SCI, and improve our ability to counsel patient families.
In this study, we describe the adverse events associated with systemic hypothermia for patients enrolled in a multi-center trial evaluating the use of modest systemic hypothermia after acute cervical SCI.
Methods
Data from a prospective, multi-center, non-blinded case-controlled trial were analyzed for this study. The study aims to evaluate the efficacy of modest (33 C) systemic hypothermia for acute cervical SCI. The primary and secondary outcomes of the study, which include changes in AIS grades and FIM scores, respectively, at 12 months, will be analyzed and presented in a separate manuscript. The study began recruitment in August 2017 and is actively recruiting with a planned enrollment of 120 patients. Inclusion criteria are adults aged 18–70 years, AIS grade A-C, admission Glasgow Coma Scale ≥14, non-penetrating SCI and patients in whom hypothermia treatment can start within 24 h of injury. Patients with hyperthermia on admission (>38.5 °C), severe systemic injury, bleeding, coagulopathy, pregnancy, and cord transection are excluded. Informed consent was provided by each participant or participant family. The study protocol is approved by a central Institutional Review Board for 4 centers and one center has approval from its own Institutional Review Board.
Study design
This trial is recruiting patients with acute cervical SCI from 5 trauma centers across the United States. Patients are assigned to receive hypothermia or standard of care medical treatment. To maximize patient enrollment, the study employs a cross-over design with two centers providing hypothermia for the first 2 years, while the other centers provide standard of care (control) treatment. After 2 years, the centers switch the treatment assignments. This study design was chosen since some centers do not have experience with systemic hypothermia and these centers will enroll controls initially. The study design helps these centers get familiarized with the hypothermia protocol and learn from the more experienced centers. In addition, we anticipated that some centers will have an infrequent and unpredictable rate of enrollment of acute SCI subjects, and the time it would take to randomize subjects at the time of enrollment would make it impractical to initiate the hypothermia protocol in a timely fashion. There was no difference in the selection criteria for subjects at hypothermia and non-hypothermia sites.
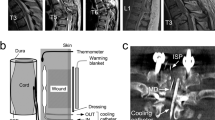
Systemic hypothermia is initiated within 24 h of injury using intravascular cooling catheters (Zoll, Chelmsford, MA, USA), inserted into the femoral vein using a sterile technique in the emergency room, intensive care unit or operating room. Patients are cooled at a maximum rate of 2–2.5 C/h till they reach the target temperature of 33 C (modest hypothermia). Modest hypothermia is maintained for 48 h and then rewarming at 0.1 C/h is performed till normothermia (37 C). If required, surgical procedures are performed concurrently with the hypothermia protocol. All patients are admitted to the ICU during the hypothermia protocol. Mean arterial blood pressure is maintained above 90 mm Hg at all times. If sedated and intubated, sedation is stopped at 12 h post-injury to obtain a neurological exam. Nutrition is initiated via a nasogastric or orogastric tube in intubated patients. Daily clinical exams, serum electrolyte, and blood counts are performed. Chemoprophylaxis for deep vein thrombosis is started as early as possible, when deemed safe by the treating physician. After termination of the hypothermia protocol, the cooling catheter is removed a venous doppler of the lower limbs is performed to evaluate for deep vein thrombosis. Routine doppler of the lower limbs is not performed for patients in the control group. All adverse events during the hospitalization are diagnosed, investigated and treated by the treating team. All complications documented in the patient’s medical chart are recorded and monitored by the data safety monitoring board (DSMB) of the study. Complications within the first 6 weeks of the injury were analyzed in this study.
Descriptive statistics were performed to analyze baseline demographic and clinical data. Chi-square test and Fisher’s exact test (if cell count <5) were performed for categorical variables. Mann–Whitney U test was used to compare continuous variables. For the purpose of this study, complications were categorized into complication groups based on the organ system affected.
Results
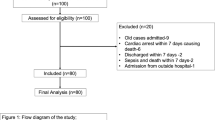
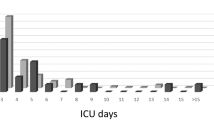
A total of 51 acute cervical spinal cord injury patients have been enrolled in the study between August 2017 and January 2021 (Table 1). Twenty-seven patients were assigned to the hypothermia arm and twenty four patients were assigned to the control arm. One patient in the control group withdrew from the study and data for this subject was not included in the analysis. For the hypothermia group, patients were enrolled at 2 sites (site 1 = 20, site 3 = 7). For the control group, patients were enrolled at 4 different sites (site 1 = 5, site 2 = 13, site 4 = 1, site 5 = 3, site 7 = 2).
Demographic and clinical data
The median age was significantly lower in patients undergoing hypothermia (p = 0.02, Table 1). The majority of patients in both arms were AIS C with a neurological level at C4. The most common mechanism of injury was motor vehicle accident (n = 13) in the hypothermia group and fall from standing/height (n = 11) in the control group. All patients in the hypothermia arm underwent spinal surgery. Twenty-four patients (88.9%) in the hypothermia group underwent surgery within 24 h of the injury. Of the 3 patients who underwent delayed surgical decompression, one patient underwent surgery during the cooling phase of the hypothermia protocol at 28 h after injury. The other 2 patients underwent delayed surgical decompression at 153 and 411 h after injury. One control patient underwent surgery within 24 h but the exact time of surgery was not available. All control patients underwent surgical decompression within 24 h except 3 patients who underwent surgery at 25.1, 38.9 and 40 h. The median time interval between injury and surgery was not significantly different between the two groups (p = 0.34, Table 1).
Chemoprophylaxis for deep vein thrombosis was started in all patients in the hypothermia group (enoxaparin (n = 24), heparin (n = 2)). Data was not available for one patient in the hypothermia group. Chemoprophylaxis was started in 21 patients in the control group (enoxaparin (n = 12), heparin (n = 9)). In the hypothermia group, chemoprophylaxis was started on post-injury day 0 (n = 3), day 1 (n = 14), day 2 (n = 5), day 3 (n = 2),day 7 (n = 1) and day 21 (n = 1). In the control group, chemoprophylaxis was started on post-injury day 0 (n = 3), day 1 (n = 7), day 2 (n = 10), and day 3 (n = 1). There was no statistical significance between timing of chemoprophylaxis between the two groups (Chi-square 8.7, p = 0.07). The rates of deep vein thrombosis (hypothermia: n = 4 (14.8%) vs control: n = 4 (17.4%), p = 0.71) and pulmonary embolism (hypothermia: n = 3 (11.1%) vs control: n = 2 (8.7%), p = 1.0). Tracheostomy was performed in 9 patients (33.3%) in the hypothermia group and 8 patients (34.7%) in the control group (p = 0.76). One patient in the control group did not have available data on estimated blood loss, chemoprophylaxis or tracheostomy status. Twenty-six patients (96%) in the hypothermia group and 21 patients (91.3%) in the control group had 6 week follow-up data available. Follow-up data on change in AIS grade will be reported in a separate manuscript.
Complication profile
Respiratory complications were the most common complication in both the hypothermia group and control group (Fig. 1). Respiratory failure (n = 15, 55.6%), and pneumonia (n = 10, 37%) were the most common respiratory complication in the hypothermia group. Cardiac complications, particularly, bradycardia was seen in 7 patients (25.9%) in the hypothermia group. In the control group, respiratory failure was seen in 12 patients (52.2%) and pneumonia in 5 patients (21.7%). Bradycardia was seen in 5 patients (21.7%) in the control group. There was no significant difference in the incidence of any complication between the two groups (Table 2). No significant difference in the incidence of a particular complication group (Table 3) was noted between the two groups.
Description of select complications in the hypothermia group.
Cardiac arrest
This patient was admitted with C4 AIS A and improved to AIS B by 6 weeks. At 7 weeks after injury, this patient sustained a cardiac arrest twice, and EEG showed anoxic brain injury, after which the patient was discharged to palliative care and expired. The cardiac arrest was not attributed to hypothermia as the hypothermia protocol was completed successfully and safely within first 4 days of the SCI, while the cardiac arrest took place 53 days later.
Stroke
This patient presented with vertebral artery dissection and developed vertebral artery occlusion leading to the cerebellar stroke.
Do not resuscitate (DNR)
This patient presented with history of bipolar disorder and AIS A, C4 SCI. After hypothermia protocol was completed, the patient recovered from AIS A to AIS B. One week after the SCI, acute, unspecified encephalopathy was reported by the ICU team as the patient’s respiratory status also declined. As re-intubation was deemed necessary, it was discussed with the patient who declined. After psychiatric evaluation, a DNR order was signed and subject expired.
Thrombocytopenia
Thrombocytopenia was reported as a complication in the medical record for a single subject in the hypothermia group. The DSMB reviewed this but did not attribute it to the hypothermia protocol.
Acute renal failure
The patient who developed acute renal failure had a complicated course of in-patient stay. This included pneumothorax, rhabdomyolysis, acute liver injury, upper limb deep vein thrombosis, bradycardia, and urinary tract infection. Since the multi-system injury potentially contributed to the renal failure, it was determined that renal failure was not attributable to the hypothermia.
Discussion
The majority of previous studies on complications after acute SCI have been retrospective reviews of SCI patient data [9,10,11,12,13]. Grossman et al. [8]. published a prospective, multi-center study using the North American Clinical Trials Network database, and showed that 57.8% of patients had at least one complication after acute SCI. Given that acute SCI is associated with several systemic complications, the authors highlighted the need for prospective data with a control group to evaluate complications specifically associated with the therapeutic intervention. Our study design adheres to these recommendations provides a reference for the expected complication rate and profile when using systemic hypothermia for acute cervical SCI. This study includes prospective multi-center data with a comparative control group and a larger number of subjects compared to prior studies describing complications with systemic hypothermia for acute SCI [5,6,7]. Respiratory complications were the commonest complication in the hypothermia group. Systemic hypothermia was not independently associated with an increased risk of complications in the first 6 weeks after acute cervical SCI.
Pulmonary complications, particularly respiratory failure, are common after acute cervical SCI and are an important contributor to morbidity and mortality [14]. Jackson and Groomes [15] evaluated prospectively collected data from five SCI care systems and found the incidence of respiratory complications to be 67% after acute SCI. Grossman et al. [8]. showed that the pulmonary complications were seen in 38.4% of patients with acute SCI (cervical and thoracic), excluding pneumonia. Pulmonary complications are more common after acute cervical SCI [15, 16], particularly with an injury level of C4 and above [14, 15]. We found the rate of at least one pulmonary complication (including pneumonia) in the first 6 weeks was higher in the hypothermia group (74.1%) compared to the control group (60.9%), however, the difference was not statistically significant (Table 3). Chest wall injuries and pulmonary contusions sustained during trauma can also contribute to respiratory complications after acute SCI. However, severe systemic injury was an exclusion criterion in this study, and therefore patients with substantial associated injuries were excluded from this study. Similar to prior studies, we found that SCI patients with more complete injury had a higher risk of pulmonary complications [14]. In prior studies [5,6,7], pulmonary complications were seen in 83% of patients and pneumonia was seen in 57–60% of acute cervical SCI patients receiving systemic hypothermia. These studies, however, included only patients with AIS A cervical SCI, and completeness of injury is known to be associated with a higher rate of pulmonary complications after acute SCI [14].
Cardiac adverse events are a known complication for patients undergoing systemic hypothermia. Similar to a prior study [5], bradycardia (n = 7, 26%) was a common complication in the acute period during the systemic hypothermia protocol. Animal studies have shown that therapeutic hypothermia can cause systolic and diastolic dysfunction [17], possibly related to persistently high intracellular myocardial calcium concentration during the cooling phase [18]. Systemic mild or moderate hypothermia can produce transient arrythmias [19, 20]. Profound cardiac side effects are more associated with deep hypothermia (<=30 C) [21], however, we employed a modest hypothermia (33 C) protocol in this study. Additionally, no patient in this study required interruption of the hypothermia protocol due to bradycardia or arrythmia.
Endovascular cooling catheters have been associated with an increased risk of deep vein thrombosis [22, 23]. The rates of deep vein thrombosis was not significantly higher in the hypothermia group in this study, despite doppler assessments after catheter removal in the hypothermia group. The cooling catheter was removed as soon as the cooling phase was completed to reduce the risk of deep vein thrombosis. Differences in choice of chemoprophylaxis agent reflect practice variations across institutions in this multi-center study, and more patients in the hypothermia group received enoxaparin. Systemic hypothermia has also been shown to cause coagulopathy and thrombocytopenia [24, 25]. However, we found no increased risk of hemorrhage or thrombocytopenia in the hypothermia group. Surgical decompression in the hypothermia group was performed during the cooling phase in 25 patients (92.6%), and the estimated blood loss was not significantly higher in the hypothermia group.
The effect of systemic hypothermia on neurological outcomes will be published in a separate manuscript. In this manuscript, we present preliminary results on complications associated with modest systemic hypothermia after acute cervical SCI in a multi-center controlled study. This the most complete set of data available in this study, and we believe that one of the challenges of recruiting subjects for the study is the small number of centers with the capability or willingness to perform systemic hypothermia for acute SCI. The aim of this manuscript was to detail the complication profile of systemic hypothermia in acute SCI using prospective, multi-center data. Our expectation is that this manuscript will address safety concerns with systemic hypothermia and increase adoption of the technique by other centers. Additionally, this manuscript represents a considerable improvement since prior published research in this area.The study is, however, limited by the small number of patients and the unequal distribution of patients across study sites. The complication rates are similar between the hypothermia and control group despite the younger age and lower number of AIS A subjects in the hypothermia group. Although this may point to an unexpectedly higher rate of complications in the hypothermia group, we could not come to this conclusion due to the limited data we had on systemic injuries. Since high impact injuries were more common in the hypothermia group (motor vehicle accidents [48.1% vs 39.1%] and sports injuries [18.5% vs 8.7%]), while falls were the most common injury in the control group (47.8%), it is possible that systemic injuries contributed to the unexpectedly higher rate of complications in the hypothermia group. Again, we anticipate the differences in age, AIS grade and injury mechanism to reduce as we enroll more subjects in the trial.
The difference in age between the two groups was unanticipated and we expect that the difference in median age between the two groups will lessen as more subjects are enrolled in the study. Since the inclusion criteria for this study were fairly strict, the complication profile may not be generalizable to all acute SCI patients. As one of the first prospective, multicenter controlled studies to use modest systemic hypothermia for acute cervical SCI, this study describes an acceptable adverse event rate for modest systemic hypothermia that is not greater than that seen with standard of care.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Alzaga AG, Cerdan M, Varon J. Therapeutic hypothermia. Resuscitation. 2006;70:369–80.
Kaibara T, Sutherland GR, Colbourne F, Tyson RL. Hypothermia: depression of tricarboxylic acid cycle flux and evidence for pentose phosphate shunt upregulation. J Neurosurg. 1999;90:339–47.
Morino T, Ogata T, Takeba J, Yamamoto H. Microglia inhibition is a target of mild hypothermic treatment after the spinal cord injury. Spinal Cord. 2008;46:425–31.
Friedman LK, Ginsberg MD, Belayev L, Busto R, Alonso OF, Lin B, et al. Intraischemic but not postischemic hypothermia prevents non-selective hippocampal downregulation of AMPA and NMDA receptor gene expression after global ischemia. Brain Res Mol Brain Res. 2001;86:34–47.
Levi AD, Green BA, Wang MY, Dietrich WD, Brindle T, Vanni S, et al. Clinical application of modest hypothermia after spinal cord injury. J Neurotrauma. 2009;26:407–15.
Levi AD, Casella G, Green BA, Dietrich WD, Vanni S, Jagid J, et al. Clinical outcomes using modest intravascular hypothermia after acute cervical spinal cord injury. Neurosurgery. 2010;66:670–7.
Dididze M, Green BA, Dietrich WD, Vanni S, Wang MY, Levi AD. Systemic hypothermia in acute cervical spinal cord injury: a case-controlled study. Spinal Cord. 2013;51:395–400.
Grossman RG, Frankowski RF, Burau KD. Incidence and severity of acute complications after spinal cord injury. J Neurosurg Spine. 2012;17:119–28.
Boakye M, Patil CG, Santarelli J, Ho C, Tian W, Lad SP. Laminectomy and fusion after spinal cord injury: national inpatient complications and outcomes. J Neurotrauma. 2008;25:173–83.
New PW, Jackson T. The costs and adverse events associated with hospitalization of patients with spinal cord injury in Victoria, Australia. Spine. 2010;35:796–802.
Tator CH, Duncan EG, Edmonds VE, Lapczak LI, Andrews DF. Complications and costs of management of acute spinal cord injury. Paraplegia. 1993;31:700–14.
Krassioukov AV, Furlan JC, Fehlings MG. Medical co-morbidities, secondary complications, and mortality in elderly with acute spinal cord injury. J Neurotrauma. 2003;20:391–9.
Furlan JC, Kattail D, Fehlings MG. The impact of co-morbidities on age-related differences in mortality after acute traumatic spinal cord injury. J Neurotrauma. 2009;26:1361–7.
Aarabi B, Harrop JS, Tator CH, Alexander M, Dettori JR, Grossman RG, et al. Predictors of pulmonary complications in blunt traumatic spinal cord injury. J Neurosurg Spine. 2012;17:38–45.
Jackson AB, Groomes TE. Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil. 1994;75:270–5.
Fishburn MJ, Marino RJ, Ditunno JF. Atelectasis and pneumonia in acute spinal cord injury. Arch Phys Med Rehabil. 1990;71:197–200.
Espinoza A, Kerans V, Opdahl A, Skulstad H, Halvorsen PS, Bugge JF, et al. Effects of therapeutic hypothermia on left ventricular function assessed by ultrasound imaging. J Am Soc Echocardiogr Publ Am Soc Echocardiogr. 2013;26:1353–63.
Wold RM, Kondratiev T, Tveita T. Myocardial calcium overload during graded hypothermia and after rewarming in an in vivo rat model. Acta Physiol Oxf Engl. 2013;207:460–9.
MacKenzie MA, Aengevaeren WR, Hermus AR, Van Der Werf T, Pieters GF, Smals AG, et al. Electrocardiographic changes during steady mild hypothermia and normothermia in patients with poikilothermia. Clin Sci Lond Engl 1979. 1992;82:39–45.
Ilia R, Ovsyshcher I, Rudnik L, Gueron M. Atypical ventricular tachycardia and alternating Osborn waves induced by spontaneous mild hypothermia. Pediatr Cardiol. 1988;9:63–5.
Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009;37:S186–202.
Maze R, Le May MR, Froeschl M, Hazra SK, Wells PS, Osborne C, et al. Endovascular cooling catheter related thrombosis in patients undergoing therapeutic hypothermia for out of hospital cardiac arrest. Resuscitation. 2014;85:1354–8.
Andremont O, du Cheyron D, Terzi N, Daubin C, Seguin A, Valette X, et al. Endovascular cooling versus standard femoral catheters and intravascular complications: a propensity-matched cohort study. Resuscitation. 2018;124:1–6.
Patt A, McCroskey BL, Moore EE. Hypothermia-induced coagulopathies in trauma. Surg Clin North Am. 1988;68:775–85.
Schubert A. Side effects of mild hypothermia. J Neurosurg Anesthesiol. 1995;7:139–47.
Acknowledgements
Zoll (Chelmsford, MA, USA) provided access to catheters and machines but did not financially support the study.
Funding
United States Department of Defense: CDMRP-AR150187- Award No. W81XWH-16-1-0756. Miami CTSI 1UL1TR000460. University of Miami.
Author information
Authors and Affiliations
Contributions
AV: study design, data analysis, interpretation of results, writing the report. GJ: data collection, data analysis, interpretation of results. JH: data collection, interpretation of results, manuscript review and feedback. LA: data collection, administrative assistance. FIA: data collection, interpretation of results, manuscript review and feedback. RKM: data collection, interpretation of results, manuscript review and feedback. JBJ: data collection, interpretation of results, manuscript review and feedback. RBR: data collection, interpretation of results, manuscript review and feedback. ADL: study conception, study design, interpretation of results, final review of manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
We certify that all applicable institutional regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vedantam, A., Jimsheleishvili, G., Harrop, J.S. et al. A prospective multi-center study comparing the complication profile of modest systemic hypothermia versus normothermia for acute cervical spinal cord injury. Spinal Cord 60, 510–515 (2022). https://doi.org/10.1038/s41393-021-00747-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00747-w