Abstract
Study design
Systematic review.
Objectives
To evaluate the impact of cannabinoids on neurobehavioral outcomes in preclinical models of nontraumatic and traumatic spinal cord injury (SCI), with the aim of determining suitability for clinical trials involving SCI patients.
Methods
A systematic search was performed in MEDLINE and Embase databases, following registration with PROPSERO (CRD42019149671). Studies evaluating the impact of cannabinoids (agonists or antagonists) on neurobehavioral outcomes in preclinical models of nontraumatic and traumatic SCI were included. Data extracted from relevant studies, included sample characteristics, injury model, neurobehavioural outcomes assessed and study results. PRISMA guidelines were followed and the SYRCLE checklist was used to assess risk of bias.
Results
The search returned 8714 studies, 19 of which met our inclusion criteria. Sample sizes ranged from 23 to 390 animals. WIN 55,212-2 (n = 6) and AM 630 (n = 8) were the most used cannabinoid receptor agonist and antagonist respectively. Acute SCI models included traumatic injury (n = 16), ischaemia/reperfusion injury (n = 2), spinal cord cryoinjury (n = 1) and spinal cord ischaemia (n = 1). Assessment tools used assessed locomotor function, pain and anxiety. Cannabinoid receptor agonists resulted in statistically significant improvement in locomotor function in 9 out of 10 studies and pain outcomes in 6 out of 6 studies.
Conclusion
Modulation of the endo-cannabinoid system has demonstrated significant improvement in both pain and locomotor function in pre-clinical SCI models; however, the risk of bias is unclear in all studies. These results may help to contextualise future translational clinical trials investigating whether cannabinoids can improve pain and locomotor function in SCI patients.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a traumatic event associated with severe disability and mortality [1]. Prevalence of SCI is estimated to be 906 cases per million in the United States and incidence as high as 58 cases per million per year in some European countries [2, 3]. The consequences of SCI encompass motor, sensory and autonomic domains [4]; functional disability, reduced quality of life and high prevalence of affective disorders are common [5]. Chronic neuropathic pain affects up to 75% of people with SCI [5]. Burning and shooting pain as well as hypersensitivity to cutaneous stimuli have detrimental effects on rehabilitation, mood and mental health [6].
The classic model of SCI consists of two phases [1]. The first phase involves direct damage as a result of mechanical trauma. This causes immediate damage and then catalyses the second phase of injury driven by aberrant molecular, cellular and biochemical cascades. Secondary injury constitutes damage caused by ischaemia, ionic derangements, excitotoxicity, free radical damage, oedema, inflammation and apoptosis [7, 8].
Cannabinoid (CB) receptor agonists are a promising pharmacological approach [9]. CBs were first identified as the psychoactive constituents of marijuana [10]. However, an endogenous cannabinoid system also exists, consisting of two CB receptors (CB1 and CB2), natural ligands (endo-CBs) such as anandamide, and enzymes involved in endo-CB synthesis and degradation [11]. Following SCI, local modulation of the endo-CB system has been reported [11]. This involves increased levels of anandamide, upregulation of the synthetic enzyme, and downregulation of the degradative enzyme. Moreover, the endo-CB system has been shown to be important in neuroprotection and immunomodulation after SCI [11], as well after cerebral ischaemia-reperfusion injury [12] and traumatic brain injury [13].
A number of cannabinoids have been shown to downregulate processes thought to be important in the secondary phase of SCI. For example, cannabidiol (CBD) is an exogenous cannabinoid receptor agonist currently being evaluated in a number of clinical trials for multiple medical conditions [14,15,16,17]. CBD has been shown to reduce reactive oxygen and nitrogen species production, chemokine and cytokine release, microglial and astrocyte activation, as well as T cell proliferation [18, 19]. In addition, WIN 55,212-2, a non-selective CB receptor agonist, downregulates central nervous systems neutrophil infiltration and apoptosis in multiple sclerosis [20], promotes neural remyelination in neonatal rats experiencing hypoxia-ischaemia [21] and relieves neuropathic pain following peripheral nerve injury in mice [22].
Given the mechanism of action of cannabinoids and the pathophysiology of SCI, there may be a therapeutic role for cannabinoids in patients following SCI. A recent systematic review of cannabinoid use in human patients with SCI found cannabinoid receptor agonists may be associated with reductions in pain and spasticity, however, the magnitude of these effects and clinical significance was unclear [23]. Furthermore, the overall quality of the included studies was reported as poor [23]. A series of reviews from the International Association for the Study of Pain (IASP) highlighted a similar lack of high-quality pre-clinical or clinical evidence for the use of cannabinoids in pain management specifically [24, 25]. This was the basis for the IASP position statement in March 2021, which stated that the IASP do not endorse the use of cannabinoids and cannabis-based medicine in pain management. Therefore, whilst cannabinoids have showed clinical promise, their clinical use remains limited by the strength of the pre-clinical and clinical evidence base.
This systematic review aims to evaluate the impact of cannabinoids, including cannabinoid receptor agonists, cannabinoid receptor antagonists, and endocannabinoid system modulators, on pain but also locomotor function and anxiolysis in preclinical models of SCI. Cannabinoid agonists are of interest firstly, due to their ability to downregulate processes involved in the inflammatory phase of SCI and secondly, due to reports of beneficial clinical effects following SCI. Furthermore, there exist several cannabinoid receptor agonists licensed for clinical use, and therefore evaluating the effects of cannabinoid agonists is important to gauge whether these drugs could potentially be used in translational clinical trials for patients who have undergone SCI. The effects of cannabinoid receptor antagonists and endocannabinoid system modulators are also of mechanistic interest, as they provide insight into the role of the endo-cannabinoid system following SCI.
This systematic review secondarily aims to offer discussion of the potential underlying mechanisms of action and the potential suitability of cannabinoids for future clinical trials in SCI patients. In this review, we also explore whether cannabinoids are associated with improvements in neurobehavioural outcomes in animal models of SCI and whether there may be merit in using cannabinoids to treat the symptoms experienced by patients following SCI.
The pressing unmet clinical need and scope for this review were identified through the REsearch Objectives and Common Data Elements for Degenerative Cervical Myelopathy (RE-CODE DCM) initiative, an international consortium of key stakeholders in degenerative cervical myelopathy (DCM), which provided consensus on DCM research priorities [26].
Methods
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. [27]
Protocol and registration
The protocol for this review was published on PROSPERO (an international prospective register of systematic reviews) on 3 December 2019 (CRD42019149671).
Eligibility criteria
The inclusion and exclusion criteria used in this review are presented in full in the Supplementary Material.
Population and injury model
This review included only preclinical animal models, and human studies were excluded. SCI models such as traumatic injury, spinal cord ischaemia or cryogenic spinal cord injury were included. Peripheral nerve injury or traumatic brain injury models were excluded.
Intervention and comparison
Studies were included if they used cannabinoid receptor agonists (e.g. WIN 55,212-2), cannabinoid receptor antagonists (e.g. AM251 or AM630) or endocannabinoid system modulators (e.g. acetaminophen or naloxone), administered intravenously, intraperitoneally or intrathecally. To be included, studies required a control treatment group and one or more cannabinoid treatment groups. Studies were not excluded based on drug administration parameters such as frequency or the duration of dosing.
Outcomes
Neurobehavioural outcomes, defined as outcomes of motor and/or sensory function, including pain, were the focus of this review. Studies that assessed neurobehavioural outcomes using tools such as the Basso, Beattie and Bresnahan score for locomotor function and von Frey filaments for mechanical allodynia and hyperalgesia were included. Studies that exclusively assessed other parameters, such as histological or autonomic outcomes, were excluded.
Information sources
To identify articles, a systematic search was performed of MEDLINE and Embase databases on December 14, 2020.
Search
The search strategy was developed with the assistance of a medical librarian at the Cambridge University Medical Library. The terms used to search MEDLINE and Embase are provided in the Supplementary Material. No additional search limits were applied.
Study selection
Duplicates were excluded in Mendeley (Elsevier, London, UK). The abstracts were then screened independently by 14 of the authors using Rayyan software. The abstracts were divided into 7 groups. Each group of abstracts was reviewed by a pair of authors. Disagreements were resolved through discussion between the reviewers until mutual agreement was reached.
Data extraction
The data extracted were: author, year of publication, country of experiments, study characteristics (e.g. number of experimental groups, level of evidence), sample characteristics e.g. size, number of groups, species, strain, age, sex, weight, and comorbidities), intervention (including injury model and the type, dose, frequency and route of drug), the methods and results of any neurobehavioural assessment, and the nature of any relevant statistical analysis performed. Data extraction was performed by one of the authors (FB).
Analysis and reporting
Due to the diverse range of injury models, interventions and outcomes, meta-analysis was not possible and a narrative synthesis using the Synthesis Without Meta-analysis (SWiM) reporting guideline was conducted [28]. A checklist of adherence is provided in the Supplementary Material. Studies were primarily grouped based on outcome measures and secondarily the cannabinoid intervention used. The three broad outcome categories were motor function, pain and anxiolysis. The differences (mean/median/p values) between intervention and control groups reported by individual studies for each outcome measure was initially summarised in a table. Findings were subsequently summarised by transforming the difference measures into standardised metric-direction of effect (positive/negative/no effect) and synthesised in the form of harvest plots by vote-counting based on direction of effects. Combining p values and calculating summary statistics of intervention effect estimates was not possible. Heterogeneity in reported effects was investigated by structuring figures around the injury model, interventions, and outcomes assessed; these are provided in the Supplementary Material. The SYRCLE (Systematic Review Centre for Laboratory Animal Experimentation) tool was used to evaluate the risk of bias of the included studies [29]. Since risk of bias was determined to be ‘unclear’ for all the included studies, it could not be used to prioritise the reporting of certain findings over others, thus study findings were reported equally in the narrative synthesis.
Results
Study selection
The search generated 8714 results. A total of 2062 duplicates were removed using Mendeley (Elsevier, London, UK), resulting in 6652 unique studies. Following the abstract screening, 41 studies were found to meet the inclusion criteria (Supplementary Material). On full-text screening, 23 studies were excluded for the reasons outlined in the Supplementary Material. One additional relevant study was identified in the reference list of an included study. In total, 19 studies were included (Fig. 1).
Study characteristics
Of the 19 included studies, 13 studies used rat models of SCI [30,31,32,33,34,35,36,37,38,39,40,41,42] and 6 used mice models [43,44,45,46,47,48]. Sprague-Dawley rats were used in 10 studies [30, 33,34,35,36,37,38,39,40,41] and Wistar rats in 3 studies [31, 32, 42]. With regards to strains of mice, CD1 mice were used by 3 studies [43, 45, 48] while CB57BL/6J [44], CB57BL/6 [46] and PPAR-αKO mice with litter-mate wildtype controls [47] were each used in 1 study. Male animals were used in 16 studies [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] whilst female animals were used in 1 [46]. 2 studies did not specify the sex of the animals used [47, 48]. The age of mice and rats were not specified in 11 studies [34,35,36,37,38,39,40,41,42, 46, 48]. Of the 8 studies which commented on animal age, 4 studies explicitly specified the age of the animals used [31, 33, 44, 47] and 4 studies stated adult animals were used [30, 32, 43, 45].
The different injury models used are summarised in Fig. 2 and Table 1. Compression models, involving microvascular clips (n = 9) [35,36,37,38,39, 43, 45, 47, 48] and silicon tube insertion into the vertebral canal [44], and contusion models involving spinal cord impaction devices (n = 4) [30, 31, 33, 46] were the most commonly used. Other models used included spinal cord ischaemia via aortic occlusion [40], cryogenic injury using liquid nitrogen [42], spinal cord hemisection [32], ischaemia-reperfusion injury via aortic occlusion [34] and ischaemia-reperfusion injury via aortic clamping [41]. The majority of SCI models used thoracic injury (n = 15) [30, 31, 33, 35,36,37,38,39, 42,43,44,45,46,47,48], whilst one study used cervical level injury (n = 1) [32].
Eight different cannabinoid receptor agonists were used as seen in Fig. 3. WIN 55,212-2 (n = 6) [30, 33, 35, 36, 38, 40] was the most commonly used agonist. Palmitoylethanolamide (PEA) [43, 47] and cannabidiol (CBD) [42, 46] were each used in 2 studies. CP 55,940 [39], JWH [32], N-(2-chloroethyl)−5Z, 8Z, 11Z, 14Z-eicosatetraenamide (ACEA) [44], oxazoline of Palmitoylethanolamide [45] and co-ultramicronised PEA and luteolin [48] were each used in 1 study. Two different inverse cannabinoid receptor agonists were used: rimonabant (n = 2) [38, 39] and hemopressin (n = 1) [38]. Five cannabinoid receptor antagonists were also used, with AM 630 (n = 8) [30, 31, 33,34,35, 37, 40, 41] and AM 251 (n = 7) [30, 33,34,35, 37, 40, 41] being the most commonly used. Other antagonists used included SR 144528 (SR 2) (n = 2) [32, 39] and AM 281(n = 1) [31]. One study used acetaminophen and naloxone [37]; both drugs have been reported to have effects on the endocannabinoid system. Initiation of cannabinoid administration ranged from 20 min [30] to 5 weeks [35] after SCI. The duration of cannabinoid administration ranged from single one-off doses to repeat dosing over 10 weeks [46]. A comprehensive summary of the drugs used in the included studies can be found in the Supplementary Material.
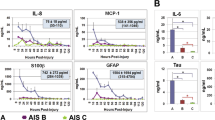
Across the included studies, locomotor function was evaluated by 13 studies, pain perception was evaluated by 8 studies and 1 study explored anxiety. 8 different measures of locomotor function were used (summarised in Fig. 4A). The most commonly used measures of locomotor function were Basso Mouse Scale (BMS) (n = 5) [44,45,46,47,48], Basso, Beattie, Bresnahan (BBB) Locomotor score (n = 4) [31, 33, 42, 43] and 14-point motor deficit index (MDI) score (n = 2) [34, 40]. Beam-walking test [32], CatWalk [32], rodent rotarod) [44], spontaneous open-field locomotor activity [44] and Tarlov scoring system [41] were each used once. Two measures of pain were used (summarised in Fig. 4B), namely the von Frey filament test (n = 5) [31, 35,36,37,38,39] and hind paw withdrawal to thermal stimulus (n = 3) [30, 31, 46]. The elevated plus-maze test [44] was the sole measure of anxiety (n = 1). No studies assessed the sedative effects of cannabinoids. Table 2 summarises all of the scoring systems used to evaluate outcomes. Assessment time points ranged from 30 min [35] to 90 days [31] after cannabinoid administration. Table 3 groups the included studies by neurobehavioural outcome, and summarises the sample features, injury models, interventions, assessment tools and key findings. Figs 2 and 3 investigate the effects of specific cannabinoid interventions and injury model on locomotor and pain, and highlight the heterogeneity of the included studies. Fig. 4 visually represents the overall effects of cannabinoids on locomotor function and pain. Further information relating to individual studies can be found in the Supplementary Material.
Risk of bias
Allocation sequence was adequately generated and applied in 12 out of 19 studies, the remaining studies may have been randomised but did not describe their allocation sequence. Four studies stated that group neurobehavioural characteristics were similar to baseline. No studies stated if the allocation was adequately concealed or if animals were randomly housed during the experiment. No studies stated if animals were selected at random for outcome assessment. The outcome assessor was blinded in 7 out of 19 studies; however, no studies explicitly stated that caregivers or investigators were blinded. One study stated one mouse in the vehicle group died but provided no further information regarding under what circumstances this occurred. A lack of reporting of items on the SYRCLE checklist across the 19 included studies means that accurately determining the risk of bias is challenging. This means that the overall risk of bias remains unclear and all results must be interpreted in the context of this. Full details of risk of bias assessment are provided in the Supplementary Material.
What is the impact of cannabinoids on locomotor outcomes?
13 studies assessed locomotor outcomes of which five assessed BMS [44,45,46,47,48], four assessed BBB locomotor score [31, 33, 42, 43], two assessed 14-point MDI [34, 40]. Rodent rotarod [44], spontaneous open-field locomotor activity [44], beam walking [32], tarlov score [41] and catWalk assessment [32] were each used in one study.
Basso Mouse Scale (BMS) score
Five studies assessed BMS score of which one used ACEA [44], one used CBD [46], two used PEA [47, 48] and one used PEA-OXA [45].
Hong et al. observed that ACEA treated mice had higher BMS scores at 21 days post-SCI compared to vehicle (ACEA = 8 ± 3, vehicle = 5 ± 6, p = 0.02) [44]. By 3 weeks post-SCI most mice in both ACEA and vehicle-treated groups were able to use hindlimbs to support body weight (BMS score >5) [44]. However, a greater number of mice were able to co-ordinate forelimb, hindlimb and tail function (BMS = 9) in the ACEA treated group (5 of 12) compared to the vehicle-treated group (0 of 11) (p = 0.02) [44].
CBD treatment was not shown to produce a significant effect on BMS scores compared to vehicle-treated mice over a period of 10 weeks post-SCI in the study by Li et al. [46].
Of the two studies using PEA [47, 48], 1 used PEA alone and in combination with PPAR-γ and PPAR-δ antagonists GW9662 and GW0660 [47] in wild type (WT) and PPAR-α knock-out (PPAR-αKO) mice. The other used PEA alone, PEA associated with luteolin (flavindoid with antioxidant properties) and a co-ultramicronised composite of PEA and luteolin [48] in WT mice. Both studies induced SCI using microvascular clips and recorded BMS scores daily for 10 days post-SCI. Treatment of WT mice with i.p. PEA (10 mg/kg) exclusively produced a significant increase in BMS scores in one study (p < 0.05) [47]. Pre-treatment with GSK0660 or GW9662 abolished the PEA-induced increase in BMS score [47]. Similarly the genetic absence of the PPAR-α receptor blocked the effect of PEA treatment [47]. In the other study, treatment of WT mice with i.p. PEA (1mg/kg) did not produce a significant increase in BMS scores. Treatment with PEA associated with luteolin also did not improve BMS scores compared to vehicle-treated control mice (p > 0.05) however, treatment with the co-ultramicronised composite of PEA and luteolin significantly reduced motor disturbance after SCI(p < 0.01) [48].
Using PEA-OXA, Impellizzeri et al. found treatment with 10 mg/kg significantly improved BMS scores post-SCI compared to vehicle-treated mice, and the effect was maintained until the end of the 10-day post-SCI experimental period (p < 0.05) [45].
Basso, Beattie, Besnahan (BBB) Locomotor Score
Of the four studies that assessed BBB score, one used PEA [43], one used WIN 55,212-2 alone and in combination with AM 251 or AM 630 [33], one used AM 251 and/or AM 630 [31], and one used CBD [42].
Genovese et al. found pre- or post-treatment with PEA significantly reduced the functional deficits induced by SCI over a 10-day period following SCI (p < 0.05 compared to vehicle-treated controls) [43]. No significant difference was found between PEA administered as a pre- or post-treatment [43]. WIN 55,212-2 was shown to promote functional recovery, measured by BBB score, following SCI [33]. BBB scores of WIN 55,212-2 treated animals continued to improve until 3 weeks following SCI at which point they scored more than 12, whereas BBB scores of control animals plateaued 1 week post-SCI (p < 0.0001) [33]. Significant differences were noted between WIN 55,212-2 and control-treated animals from day 7 to day 28 post-SCI (p < 0.01 at each individual timepoint) [33]. Pre-treatment with AM 630 (CB2 R antagonist) but not AM 251 (CB1 R antagonist) reversed the improvement induced by WIN 55,212-2 treatment (p = 0.0001 and p = 0.1879 respectively) [33]. In the study by Kwiatkoski et al. control rats and CBD treated rats both scored zero on the first day after SCI [42]. However, on day 3 and 7, CBD treated rats obtained higher BBB scores compared to controls (Day 3, CBD treated rats median = 2, vehicle-treated rats median = 0.5; p < 0.05. Day 7, CBD treated rats median = 7, vehicle-treated rats median = 4.5; p < 0.05) [42].
Using the selective CB1 R and CB2 R antagonists, AM 281 and AM 630, Arevalo-Martin et al. found the no difference between the BBB scores of cannabinoid antagonist and vehicle-treated mice at day 7 and 14 post-SCI [31]. At day 30, 60 and 90 cannabinoid antagonist treated mice scored significantly lower that vehicle-treated mice (Day 30: AM630; p < 0.05, AM281 + AM630; p < 0.05. Day 60: AM281; p < 0.05, AM630; p < 0.05, AM281 + AM630; p < 0.001. Day 90: AM281; p < 0.05, AM630; p < 0.05, AM281 + AM630; p < 0.05), with antagonist treated mice reaching a plateau at day 30 compared to vehicle-treated mice which continued to improve until day 60 [31].
The 14-point motor deficit index score
Two studies assessed the 14-point motor deficit (MDI) score [34, 40]. Huo et al. studied the effects of WIN 55,212-2 alone and alongside AM 251 or AM 630 following spinal cord ischaemia [40]. Su et al. investigated the effects of CB1 and CB2 receptor antagonists, AM 251 and AM 630, on the ischaemic tolerance induced by remote ischaemic preconditioning (RIPC) prior to ischaemia/reperfusion injury [34].
Following spinal cord ischaemia, WIN 55,212-2 treatment was observed to reduce the MDI score compared to control treatment (WIN 55,212-2 median = 2.5, interquartile range (IQR) = 1.25, control median = 5, IQR = 2; p < 0.05) [40]. This improvement was noted to be reversed by CB2 receptor antagonism with AM 630 but not by CB1 receptor antagonist with AM 251 (WIN 55,212-2 median = 2.5, IQR = 1.25, WIN 55,212-2 + AM630 median = 5, IQR = 1.25; p < 0.01, WIN 55,212-2 + AM251 median = 2.5, IQR = 1.25; p > 0.05) [40].
Su et al. observed no difference between the MDI scores of rats treated with RIPC, AM 630 + RIPC, and vehicle + RIPC. The MDI scores of rats treated with RIPC was significantly lower than AM 251 + RIPC treated rats (p < 0.05). No significant difference was recorded between the MDI scores of rats treated with AM251 + RIPC, AM 251, AM 630 or vehicle.
Rodent rotarod
One study assessed rodent rotarod performance [44]. Hong et al. found ACEA (3 mg/kg/day) treatment improved rotarod function over the 21 day recovery interval compared to vehicle treatment (p = 0.04) [44].
Spontaneous open field locomotor activity
One study assessed open field locomotor activity of mice treated with ACEA. ACEA was not found to affect spontaneous activity post-SCI [44].
Beam-walking test
Latini et al. found rats treated with either JWH-015, SR2, or saline after lateral cervical spinal cord hemisection all displayed uniform severe motor impairments at day 1 post-SCI [32]. From day 3 post-SCI onwards, rats treated with JWH-015 had better beam-walking scores than saline (p < 0.001) and SR2 (p < 0.0001) treated rats [32]. No differences in score were observed between rats treated with SR2 or saline [32].
CatWalk
Using CatWalk video analysis, Latini et al. found all rats treated with either JWH-015, SR2 or saline to display clear deficits in all parameters on day 7 post-SCI [32]. However, from day 7 to day 60 post-SCI, JWH-015 treated rats achieved significantly better print length (p < 0.001), print width (p < 0.0001), print area (p < 0.001), regularity index (p < 0.0001) and maximum contact area (p < 0.001) than both SR2 and saline-treated rats [32]. No differences were observed between saline and SR2 treated rats [32].
Tarlov scoring system
One study assessed neurological function using the Tarlov scoring system [41]. Jing et al. studied the effect of AM 251 and AM 630 pre-treatment on the neuroprotective effects of RIPC prior to ischaemia/reperfusion injury [41]. At 4 h after reperfusion, AM 251 pre-treatment + RIPC treated rats achieved significantly lower Tarlov scores compared to rats subject to RIPC only (p < 0.05) [41]. The scores of RIPC only, AM630 pre-treatment + RIPC, and vehicle pre-treatment + RIPC treated mice were not significantly different at this time point [41]. At 24 h post-reperfusion, both AM 251 and AM 630 pre-treatment statistically abolished the neuroprotective effect of RIPC as measured by Tarlov scores (p < 0.05) [41].
What is the impact of cannabinoids on pain outcomes?
Eight studies assessed pain outcomes of which seven used the von Frey filament test [31, 35,36,37,38,39, 46] and three assessed hind paw withdrawal thresholds [30, 31, 46].
Von Frey filament test
Of the seven studies assessing mechanical sensitivity using the von Frey filament test, one study used CBD [46], three used WIN 55,212-2 [35, 36, 38], one used CP 55,940 [39], one used hemopressin [38], two used rimonabant [38, 39], one used AM 251 [35, 37], one used AM 281 [31], three used AM 630 [31, 35, 37], and one used SR 144528 [39]. One study used acetaminophen either alone or in combination with gabapentin, memantine, morphine or tramadol [37].
The study by Li et al. found no significant main effect of CBD treatment on right hindpaw von Frey filament scores [46]. Changes in mechanical sensitivity were noted to be variable between mice and between the left and right paw of individual mice, with both increases and decreases in sensitivity observed [46].
Of the two studies that administered WIN 55,212-2 subcutaneously, one administered WIN 55,212-2 as a single dose at 4–5 weeks post-SCI [35] and one administered WIN twice daily for 7 days beginning 4 weeks post-SCI [36]. Both studies found WIN-55,212-2 increased withdrawal thresholds in a dose-dependent manner (p < 0.05 in both studies) [35, 36]. This was observed for 2 h following single WIN 55,212-2 treatment by Hama et al. [35] and 30 min after each WIN 55,212-2 injection by Hama et al. [36]. The antinociceptive effect of WIN was maintained throughout the duration of the 7 day experimental period in the Hama et al.(2009) study [36]. Pre-treatment with AM 251 but not AM 630 was observed to block the antinociceptive effect of subcutaneous WIN 55,212-2 [35].
Hama et al. [38], investigated the effects of centrally mediated CB receptor ligands following SCI [38]. Intrathecal WIN 55,212-2 (57.4 nmol) significantly increased withdrawal thresholds from 30 min post-administration to 120 min post-administration (p < 0.05). Lower doses of intrathecal WIN 55,212-2 were not reported to affect withdrawal thresholds [38]. Intracerebroventricular WIN 55,212-2 produced a dose-dependent antinociceptive effect at 30 min post-administration, but not at any other time point (p < 0.05 at 30 min) [38].
Intrathecally injected hemopressin and rimonabant did not significantly alter hind paw withdrawal threshold [38]. Hemopressin administered either as a pre-treatment intrathecally or as an intracerebroventricular co-treatment with WIN 55,212-2 did not alter the antinociceptive effect of intrathecal WIN 55,212-2 [38]. By contrast intrathecal rimonabant pre-treatment blocked the antinociceptive effect of intrathecal WIN 55,212-2 (p < 0.05 compared to vehicle pre-treatment) [38]. Subcutaneous pre-treatment with rimonabant blocked the antinociceptive effect of intracerebroventricular WIN 55,212-2 (p < 0.05 compared to vehicle pre-treatment) [38].
Arevalo-Martin et al. observed no difference between rats treated with AM 281 (3 mg/kg), AM 630 (3 mg/kg) or a combination AM 281 (3 mg/kg) and AM 630 (3 mg/kg), and rats treated with vehicle following SCI [31].
Hama et al. [39] found CP 55,940 increased withdrawal threshold compared to vehicle in a dose-dependent manner (p < 0.05) [39]. Peak efficacy was not observed until 60–90 min following injection of lower doses (0.03 and 0.1 mg/kg) but was observed rapidly following injection with the highest dose (0.3 mg/kg) [39]. Hama et al. [39] noted the antinociceptive effect of CP 55,940 was maintained at full efficacy with twice-daily dosing over a 7-day observation period [39]. Pre-treatment with the CB1 receptor antagonist rimonabant (p < 0.05) but not the CB2 receptor antagonist SR 144528 (p > 0.05) blocked the effect of CP 55,90 [39].
Hama et al. [37] studied the effects of using acetaminophen alone or in combination with other analgesics on mechanical sensitivity, measured using the von Frey filament score, and presented as a percent maximum possible effect [37]. The maximum possible effect of acetaminophen (100 mg/kg) at 60 and 90 min post-SCI were not significantly different to that of vehicle-treated rats [37]. Combinations of acetaminophen with either gabapentin or morphine produced statistically significant synergy (p < 0.05 compared to effects of drugs used individually) [37]. Combinations of acetaminophen with either memantine or tramadol did not produce any statistically significant synergy (p > 0.05 compared to effects of drugs used individually) [37]. Pre-treatment with AM 251 but not AM 630 significantly attenuated the antinociceptive effect of the acetaminophen + gabapentin combination (AM 251 compared to vehicle pre-treatment; p < 0.05) [37]. Pre-treatment with AM 251 significantly attenuated the antinociceptive effect of the acetaminophen + morphine combination with morphine however, a significant residual antinociceptive effect remained (AM 251 compared to vehicle pre-treatment; p < 0.05) [37]. Similarly, pre-treatment with AM 630 partially decreased the antinociceptive effect of acetaminophen with morphine, leaving a residual antinociceptive effect (AM 630 compared to vehicle pre-treatment; p < 0.05) [37]. Although the acetaminophen + tramadol combination did not produce statistically significant synergy, Hama et al. [37]. found pre-treatment with AM 251 but not AM 630 significantly attenuated the effect of the combination (AM 251 compared to vehicle pre-treatment; p < 0.05) [37]. Pre-treatment with either AM 251 or AM 630 before vehicle treatment did not significantly affect withdrawal thresholds [37].
Hind paw withdrawal to thermal stimulus
Three studies assessed hind paw withdrawal to thermal stimulus [30, 31, 46]. One study treated rats with WIN 55,212-2 alone or in combination with the CB1 or CB2 receptor antagonists AM 251 and AM 630 [30]. One study involved treatment with AM 281 and AM630 alone and in combination. One study treated mice with CBD [46].
Ahmed et al. found that WIN 55,212-2 treatment after SCI (0.2 mg/kg and 2.0 mg/kg) increased withdrawal thresholds from a thermal noxious stimulus, measured on post-injury day 42, in a dose-dependent manner (WIN 55,212-2 0.2 mg/kg increased hindpaw withdrawal latency from 9.5 ± 0.4 s to 11.1 ± 0.5 s on day 42 post injury; p < 0.05. WIN 55,212-2 2 mg/kg increased hindpaw withdrawal latency from = 8.4 ± 0.4 s to 10.7 ± 0.4 s on day 42 post injury; p < 0.0001) [30]. Pre-treatment with AM 630 (3 mg/kg) but not AM 251 (3 mg/kg) was found to significantly decrease the anti-hyperalgesic effect of subsequent WIN 55,212-2 i.p. injection (After AM 630 pre-treatment 9.9 ± 0.6 s, after WIN 55–212,2 post-treatment 8.6 ± 1.0 s; p > 0.05. After-AM 251 pre-treatment 9.7 ± 0.6 s, after WIN 55–212,2 post-treatment 12.0 ± 0.7 s; p < 0.0001) [30].
Arevalo-Martin et al. reported no notable difference in hind paw withdrawal from hot or cold plates when rats were treated with AM 281 (3 mg/kg) and/or AM 630 (3 mg/kg) [31]. A transient increase in hind paw withdrawal time from a cold plate was observed in rats treated with AM 281 or AM 630 at day 60 compared to vehicle-treated rats (p < 0.05) but this was not maintained at day 90 [31].
Li et al. found CBD treatment to be associated with a reduction in thermal sensitivity following thoracic contusion injury [46].
What is the impact of cannabinoids on anxiolysis?
Hong et al. used the elevated plus-maze test to investigate the anxiolytic effects of ACEA post-SCI. No anxiolytic effect of ACEA (3 mg/kg/day) was observed [44].
Discussion
The aim of this systematic review was to evaluate the effect of cannabinoids on neurobehavioral outcomes in preclinical models of SCI. Overall, cannabinoid receptor agonists ACEA, CBD, CP 55,950, JWH-015, PEA, PEA-OXA and WIN 55,212-2 were reported to produce significant improvements across a range of neurobehavioral outcomes assessing locomotion and pain. However, as aforementioned, a lack of adherence to reporting items on the SYRCLE checklist mean that accurately assessing risk of bias is challenging, and therefore the overall risk of bias and validity of the reported outcomes remain unclear. Comparison between studies and drugs are currently limited by heterogeneity in species, strain, age, injury model, dosing, route of administration, and differences in the timing of neurobehavioural assessments.
What is the proposed mechanism of action?
WIN 55,212-2 was observed to improve BBB locomotor score, hind paw withdrawal to thermal stimulus and von Frey filament test scores when administered i.p., s.c. and i.t. [30, 33, 35, 36, 38, 40]. However, improvement was only noted at one time point (30 min post administration) in one study [38].
The effects of WIN 55,212-2 were noted to be blocked by CB1 R antagonists in 2 two studies [30, 35] and CB2 R antagonists in two studies [33, 40]. The endo-CB system is thought to be modulated in two phases following SCI [11]. An initial, acute phase in the first week of SCI is characterised by increased levels of the CB1 receptor-specific endo-CB AEA and high levels of CB1 receptor expression on neurons and oligodendrocytes [11]. This acute phase is considered important for neuronal survival [11]. Two to three weeks after SCI, in the chronic phase post-SCI, levels of the non-specific CB receptor endo-CB agonist 2-AG and CB2 receptors in macrophages and astrocyte like cells increase [11]. Increased IL-10 release from CB2 receptor-expressing macrophages has been proposed as a mechanism for CB2 receptor-mediated analgesia post-SCI [30]. Thus, the effects of WIN 55,212-2 following SCI may be mediated by its actions on both the CB1 and CB2 receptors.
Following spinal cord ischaemia, Huo et al. showed WIN 55,212-2 improved motor function, as measured by the 14-point MDI score, reduced apoptosis and improved survival of neurons [40]. Mechanistically, both Huo et al. and Su et al. showed WIN 55,212-2 treatment blocked nuclear translocation of GAPDH, formation of GAPDH/Siah1complexes and iNOS expression in the spinal cord after spinal cord ischaemia or traumatic SCI [33, 40]. GAPDH/Siah1 activity is correlated with apoptosis after ischaemic injury, thus it is proposed that WIN 55,212-2 improves functional recovery following SCI via inhibition of GAPDH/Siah1 signalling cascades and reduction in iNOS expression [33, 40].
Importantly, Hama et al. found the antinociceptive efficacy of WIN 55,212-2 to be maintained over a twice-daily 7-day treatment regimen, whereas the efficacy of morphine decreased over the same period [36]. Tolerance is a major problem with existing SCI-pain medications, hence the sustained efficacy of WIN 55,212-2 suggests that cannabinoid receptor agonists may be useful in alleviating chronic pain after SCI [36].
Potent anti-inflammatory effects of PEA were demonstrated by Genovese et al. who found that following SCI, PEA reduced the degree of spinal cord damage, neutrophil infiltration, NF-kB activation, IkB-a degradation, nitrotyrosine formation, proinflammatory cytokines production, apoptosis, Bax and Bcl-2 expression and PPAR-a degradation [43]. Paterniti et al. provided further evidence supporting the role of PPARs in the mechanism of action of PEA, finding the anti-inflammatory effects of PEA were antagonised by administration of PPARy and PPARd antagonists, and abolished in PPARa KO mice [47]. Furthermore, another study by Paterniti et al. showed a co-ultramicronised composite of PEA and luteolin restored basal expressions of PPARa, β, δ and γ post SCI [48]. Collectively, these studies suggest a significant anti-inflammatory role of PEA post-SCI.
Impellizzeri et al. found PEA-OXA treatment significantly improved BMS scores and reduced histological alterations post SCI. Mechanistically, PEA-OXA was noted to reduce astrocyte activation and increased neurotrophic factors BDNF, GDNF and NT-3 suggesting PEA-OXA has neuroprotective properties. PEA-OXA, similar to PEA, was observed to have anti-inflammatory effects, reducing degradation of IkB-a (a regulatory protein of NF-kb), and reducing expression of iNOS and COX-2, as well as the release of the pro-inflammatory cytokines TNF-a and IL-1b [45].
ACEA treatment was found to improve both functional and histological outcomes post SCI [44]. Hong et al. identified that ACEA treatment decreased matrix metalloproteinase-9 (MMP-9). MMP-9 is known to be expressed in neurons, reactive astrocytes, infiltrating leucocytes and increased activity results in blood-spinal cord barrier disruption and decreased functional recovery following SCI [49].
Two studies implicated the endo-CB system as having a role in the protective effects of RIPC prior to ischaemia/reperfusion injury [41, 34]. Firstly, RIPC has been observed to increase AEA content in the spinal cord following ischaemia/reperfusion injury [34]. Secondly, both Jing et al. and Su et al. reported cannabinoid receptor antagonists reduced the protective effects of RIPC. Jing et al. found the protective effects of RIPC to be reduced at 4 h post-ischaemia/reperfusion injury by CB1, but not CB2, receptor antagonist pre-treatment [41]. At 24 h post-ischaemia/reperfusion injury pre-treatment with either CB1 or CB2 receptor antagonists abolished the neuroprotective effect of RIPC [41]. This implies involvement of both CB1 and CB2 receptors in the protective effects of RIPC. The findings of Su et al. differed to those of Jing et al.. Su et al. report that the protective effects of RIPC were only reversed by CB1 R antagonists at 24 and 48 h post ischaemia/reperfusion injury, implicating involvement of only the CB1 receptor [34]. Therefore, whilst these findings support the involvement of the endo-CB system in RIPC, it is not clear whether both of the cannabinoid receptors are involved.
Evaluation of pre-clinical evidence base
A large degree of heterogeneity exists in the spinal cord injury models utilised by the included studies, as highlighted in Fig. 2. Each model induces different injuries with different pathophysiology. This is important when considering the potential translation of pre-clinical experiments into human studies. Each model has specific advantages and limitations (summarised in Table 1), and different types of preclinical SCI model may be required to address specific research questions. For example, transection models are a useful method of exploring neuronal regeneration and degeneration, but the pathophysiology of the injury is different to the contusive injury mechanisms more commonly seen in humans [50]. Contusion models are typically regarded as most representative of acute, traumatic SCI, whereas the more chronic injury produced by some compression models may be more representative of conditions such as degenerative cervical myelopathy [51]. The age of animals used provided another source of heterogeneity. Differences in animal age limit interpretation of the included studies as functional behaviours and regeneration after SCI may differ depending on animal age [52]. It is important that future pre-clinical work carefully considers which aspects of human pathology they aim to mimic through animal models, and choose a pre-clinical model and outcomes measures that appropriately reflect this.
There is also heterogeneity amongst the cannabinoid receptor agonists used in the included studies as seen in Fig. 3. WIN 55,212-2 was the most used compound and was noted to produce improvements in both locomotor and pain outcomes [30, 33, 35, 36, 38, 40]. Within those studies that used WIN, various routes of administration were used including intraperitoneal, subcutaneous, intrathecal and intracerebroventricular routes. Furthermore, dosing protocols varied between one off doses and repeat injections. These differences have important clinical implications as some routes of administration (e.g. subcutaneous injection may be easier than others, e.g. intrathecal injection or intracerebroventricular drug administration). The studies included in this review focus primarily on the pharmacodynamics of cannabinoid receptor agonists. However, before clinical trials can be considered, the pharmacokinetics and toxicity of these compounds must also be investigated. Thus, given that multiple compounds have shown improvements in locomotor function and pain scores, future work will need to determine which of these may be most amenable to human translation. This will require essential work investigating pharmacokinetics and distribution, safety and off-target effects, and logistical considerations such as the stability of compounds and shelf-life for use in the clinical environment. Future pre-clinical studies should aim to reach a consensus on lead compounds, explore suitable, clinically relevant dosing regimens, and determine acceptable clinical trade-offs such as the route and frequency of administration.
In our analysis, multiple items from the SYRCLE checklist were not commented on by all 19 studies, including whether animals were randomly selected for outcome assessment, or whether allocation was adequately concealed, and caregivers or investigators were blinded [29]. Due to this, risk of bias remains unclear for the included studies. This appears to be a common problem in the preclinical cannabinoid evidence base. The IASP Presidential Taskforce on Cannabis and Cannabinoid Analgesia identified similar challenges, including the unclear risk of bias due to lack of reporting of methodological criteria [25]. They posit this may be due to reporting of these terms not previously being required by journals for publication [25]. Future pre-clinical trials should be encouraged to follow the ‘Animal Research: Reporting of In Vivo Experiments’ (ARRIVE) guidelines to improve the quality of evidence generated [53].
Opportunities for translational clinical trials
The beneficial effects of cannabinoid agonists on outcomes assessing pain and locomotor function in animal models of SCI strengthens the argument that there may be scope for the endo-cannabinoid system to be harnessed in the treatment of motor and pain-related symptoms seen following human SCI. Despite many of the drugs discussed in this systematic review not being licensed for clinical use, there are now well-tolerated cannabinoid agonists used in clinical practice. These drugs may represent opportunities for translational clinical trials, bypassing the lengthy and costly process of licensing novel drugs. Sativex and Epidolex are two such drugs. Sativex, an oromucosal spray containing tetrahydrocannbinol and cannabidiol has been licensed in the United Kingdom since 2010 for the treatment of spasticity and other symptoms of multiple sclerosis [54]. Epidolex, a 99% pure oral CBD extract, was the first of its kind to be licensed by the FDA in June 2018 for the treatment of Lennox–Gastaut syndrome, Dravet syndrome and other severe forms of epilepsy [55]. A further three synthetic cannabis-related drug products have since been FDA approved, namely Marinol (dronabinol), Syndros (dronabinol), and Cesamet (nabilone). Existing clinical data from Sativex and Epidolex found diarrhoea, fatigue, somnolence, vomiting and pyrexia to be common adverse events but otherwise noted the drugs to be well tolerated [54, 56, 57]. This provides some insight into how these drugs might be tolerated if they were to be delivered following SCI as part of human clinical trials.
Hama et al. similarly investigated whether combinations of currently licensed drugs (i.e. drug repurposing) could be used to treat pain after SCI [37]. In particular combinations involving acetaminophen, which is proposed to act in part by blocking cellular uptake of anandamide [58, 59]. Combinations of acetaminophen with gabapentin or morphine displayed synergy which was attenuated using CB receptor antagonists implying involvement of the CB receptor activation [37]. The benefits of using such existing drugs include the avoidance of long periods of drug development and licensing as well as the ability to use lower doses to avoid side effects that may otherwise limit the use of such drugs.
Whilst these drugs represent promising opportunities, animal to human translation can be unpredictable and key research questions remain. Firstly, consensus must be reached regarding the optimal cannabinoid drug, dose, and determine what would constitute a clinically acceptable route of administration (particularly if repeated dosing is required). The current preclinical evidence base remains heterogenous, and it is difficult to reconcile inconsistencies between studies when variables such as the model of SCI, timing of drug administration, outcome assessment tool and timing of outcome assessment differ from study to study. Similar variation has been reported in a systematic review of the literature on the effects of cannabinoids in patients who have suffered SCI [23]. We echo their call for appropriately powered, randomised controlled studies with standardised outcome measures, which conform to Consolidated Standards of Reporting Trials, to increase the amount of good quality evidence on this topic. Secondly, there is currently little pre-clinical or clinical literature exploring the long-term effects of chronic cannabinoid use following SCI [23], and this would be worthy of further study. Of the studies included in this review, none explored the effects of administering cannabinoids beyond 10 weeks following SCI. Cannabinoids have been associated with addiction, cognitive decline, sedation, and psychotic disorders [60]. Given that SCI patients may need to use cannabinoids for a number of years, long-term longitudinal studies monitoring the incidence of such side-effects will be required if cannabinoids are to be considered in the management of these patients.
Strengths and limitations
Strengths of this review include the following: (1) the search strategy was extensive, (2) each article was independently evaluated for inclusion by 2 reviewers independently evaluated each for eligibility, (3) risk of bias was assessed using the SYRCLE risk of bias tool and (4) the review used the PRISMA guidelines and checklist to structure the review.
This review presents a qualitative, not quantitative, analysis of the existing literature. Meta-analysis was prevented by the low number of studies included and the high degree of heterogeneity in injury model, drug, dose, route of administration, timing of administration, outcome tools, timing of assessment. The overall quality of individual studies was poor due to small sample sizes and failure to satisfy a number of the components of the SYRCLE checklist. Furthermore, due to the relatively small amount of literature on the topic and reliance on what has been reported there is high risk of publication bias. Linking these pre-clinical results to potential clinical findings is difficult given the large differences between animal models of SCI and the injuries seen in patients. Moreover, important side-effects such as sedation and addiction which may have clinical implications were not evaluated in this systematic review. Additional limitations include the exclusion of studies evaluating histological changes and those studies not in English language. Authors of included studies were not contacted to obtain additional information on unpublished or planned studies.
Conclusion
The results of these studies demonstrate that modulation of the endo-cannabinoid system has significant benefit for both pain and locomotor function across a range of pre-clinical models of acute spinal cord injury. Due to low adherence of reporting items on the SYRCLE checklist, the risk of bias and validity of the reported outcomes remains unclear. Meta-analysis could not be conducted due to small sample sizes and large variation in study design. This highlights the need for additional high-quality preclinical studies with consistent methodology to evaluate the efficacy of cannabinoids in treating SCI. Furthermore, before cannabinoids can be considered in the long-term management of SCI, extensive longitudinal studies are required to monitor the incidence of long-term side effects such as addiction and cognitive decline.
Data availability
Data availability is not applicable to this article as no datasets were generated or analysed during the current study.
References
Bennett J, Das JM, Emmady PD. Spinal cord injuries. 2020. https://www.ncbi.nlm.nih.gov/books/NBK560721/.
Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: What learns a worldwide literature survey? Spinal Cord. 2006;44:523–9. https://pubmed.ncbi.nlm.nih.gov/16389270/.
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31.
Davies BM, Mowforth OD, Smith EK, Kotter MRN. Degenerative cervical myelopathy. BMJ. 2018;360. www.myelopathy.org.
Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, et al. Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS ONE. 2017;12. https://pubmed.ncbi.nlm.nih.gov/28081205/.
Widerström-Noga EG, Felipe-Cuervo E, Broton JG, Duncan RC, Yezierski RP. Perceived difficulty in dealing with consequences of spinal cord injury. Arch Phys Med Rehabil. 1999;80:580–6.
Profyris C, Cheema SS, Zang DW, Azari MF, Boyle K, Petratos S. Degenerative and regenerative mechanisms governing spinal cord injury. Neurobiol Dis. 2004;15:415–36. https://pubmed.ncbi.nlm.nih.gov/15056450/.
Sekhon LHS, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine. 2001;26. https://pubmed.ncbi.nlm.nih.gov/11805601/.
Cardenas DD, Jensen MP. Treatments for chronic pain in persons with spinal cord injury: a survey study. J Spinal Cord Med. 2006;29:109–17. https://www.tandfonline.com/doi/abs/10.1080/10790268.2006.11753864.
Arevalo-Martin A, Garcia-Ovejero D, Molina-Holgado E. The endocannabinoid 2-arachidonoylglycerol reduces lesion expansion and white matter damage after spinal cord injury. Neurobiol Dis. 2010;38:304–12. (Arevalo-Martin, Garcia-Ovejero, Molina-Holgado) Laboratorio de Neuroinflamacion, Unidad de Neurologia Experimental, Hospital Nacional de Paraplejicos (SESCAM), 45071 Toledo, Spain A. Arevalo-Martin, Laboratorio de Neuroinflamacion, Unidad de Neurologia. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=50822802, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:20156559&id=doi:10.1016%2Fj.nbd.2010.02.002&issn=09.
Garcia-Ovejero D, Arevalo-Martin A, Petrosino S, Docagne F, Hagen C, Bisogno T. et al. The endocannabinoid system is modulated in response to spinal cord injury in rats. Neurobiol Dis. 2009;33:57–71. https://pubmed.ncbi.nlm.nih.gov/18930143/.
Amantea D, Spagnuolo P, Bari M, Fezza F, Mazzei C, Tassorelli C, et al. Modulation of the endocannabinoid system by focal brain ischemia in the rat is involved in neuroprotection afforded by 17beta-estradiol. FEBS J. 2007;274:4464–75. (Amantea, Spagnuolo, Mazzei, Morrone, Bagetta) Department of Pharmacobiology, University Center for the Study of Adaptive Disorder and Headache (UCADH), University of Calabria, Rende (CS), Italy (Spagnuolo, Bari, Fezza) Department of Experimental Medicine. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed10&AN=47301708, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:17666109&id=doi:10.1111%2Fj.1742-4658.2007.05975.x&.
Panikashvili D, Simeonidou C, Ben-Shabat S, Hanus L, Breuer A, Mechoulam R, et al. An endogenous cannabinoid (2-AG) is neuroprotective after brain injury. Nature. 2001;413:527–31. (Panikashvili, Simeonidou, Shohami) Department of Pharmacology, Medical Faculty, Hebrew University, Jerusalem 91120, Israel (Panikashvili, Ben-Shabat, Hanus, Breuer, Mechoulam) Department of Medicinal Chemistry and Natural Products, Medical Faculty, Hebre. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed7&AN=32938751, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:11586361&id=doi:10.1038%2F35097089&issn=0028-0836&is.
Van Der Flier FE, Kwee CMB, Cath DC, Batelaan NM, Groenink L, Duits P. et al. Cannabidiol enhancement of exposure therapy in treatment refractory patients with phobias: study protocol of a randomized controlled trial. BMC Psychiatry. 2019;19:69 https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-019-2022-x.
ISRCTN - ISRCTN87895237: multi-centre trial of cannabidiol (CBD) for the treatment of Parkinson’s disease psychosis. http://www.isrctn.com/ISRCTN87895237.
Efficacy and safety of cannabidiol oral solution (GWP42003-P, CBD-OS) in patients with rett syndrome. 2020. https://clinicaltrials.gov/ct2/show/NCT03848832.
A randomized controlled trial of cannabidiol (GWP42003-P, CBD) for seizures in tuberous sclerosis complex (GWPCARE6). 2020. https://clinicaltrials.gov/ct2/show/NCT02544763.
Booz GW. Cannabidiol as an emergent therapeutic strategy for lessening the impact of inflammation on oxidative stress. Free Radical Biol Med. 2011;51:1054–61. (Booz) Department of Pharmacology and Toxicology, School of Medicine, University of Mississippi Medical Center, Jackson, MS 39216, United States G.W. Booz, Department of Pharmacology and Toxicology, School of Medicine, University of Mississippi Medical C. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed12&AN=51269220, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:21238581&id=doi:10.1016%2Fj.freeradbiomed.2011.01.0.
Kozela E, Juknat A, Gao F, Kaushansky N, Coppola G, Vogel Z. Pathways and gene networks mediating the regulatory effects of cannabidiol, a nonpsychoactive cannabinoid, in autoimmune T cells. J Neuroinflammation. 2016;13:136. Kozela, Ewa. The Dr Miriam and Sheldon G. Adelson Center for the Biology of Addictive Diseases, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, 6997801, Israel. kozelae@post.tau.ac.il. Kozela, Ewa. Department of Neurobiology, Weizmann Institu. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med12&AN=27256343, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:medline&id=pmid:27256343&id=doi:10.1186%2Fs12974-016-0603-x&issn=17.
Arevalo-Martin A, Garcia-Ovejero D, Gomez O, Rubio-Araiz A, Navarro-Galve B, Guaza C, et al. CB2 cannabinoid receptors as an emerging target for demyelinating diseases: from neuroimmune interactions to cell replacement strategies. Brit J Pharmacol. 2008;153:216–25. (Arevalo-Martin, Garcia-Ovejero, Gomez, Rubio-Araiz, Navarro-Galve, Molina-Holgado) Laboratory of Neuroinflammation, Unidad de Neurologia Experimental, Hospital Nacional de Paraplejicos (SESCAM), 45071 Toledo, Spain (Arevalo-Martin, Garcia-Ovejero, Gomez. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med6&AN=17891163, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:medline&id=pmid:17891163&id=doi:10.1038%2Fsj.bjp.0707466&issn=0007-1.
Fernandez-Lopez D, Pradillo JM, Garcia-Yebenes I, Martinez-Orgado JA, Moro MA, Lizasoain I. The cannabinoid WIN55212-2 promotes neural repair after neonatal hypoxia-ischemia. Stroke. 2010;41:2956–64. (Fernandez-Lopez, Pradillo, Garcia-Yebenes, Moro, Lizasoain) Unidad de Investigacion Neurovascular, Departamento de Farmacologia, Universidad Complutense de Madrid, Madrid, Spain (Martinez-Orgado) Departamento de Neonatologia y Pediatria, Hospital Univers. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=51121494, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:21115947&id=doi:10.1161%2FSTROKEAHA.110.599357&issn.
Desroches J, Charron S, Bouchard JF, Beaulieu P. Endocannabinoids decrease neuropathic pain-related behavior in mice through the activation of one or both peripheral CB1 and CB2 receptors. Neuropharmacology. 2014;77:441–52. Desroches, Julie. Department of Pharmacology, Universite de Montreal, Montreal, Quebec, Canada. Charron, Sophie. Faculty of Medicine, School of Optometry, Universite de Montreal, Montreal, Quebec, Canada. Bouchard, Jean-Francois. Faculty of Medicine, Sc. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med10&AN=24148808, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:medline&id=pmid:24148808&id=doi:10.1016%2Fj.neuropharm.2013.10.006&.
Nabata KJ, Tse EK, Nightingale TE, Lee AHX, Eng JJ, Querée M. et al. The therapeutic potential and usage patterns of cannabinoids in people with spinal cord injuries: a systematic review. Curr Neuropharmacol. 2021;19:402–32. https://www.eurekaselect.com/181078/article.
Fisher E, Moore RA, Fogarty AE, Finn DP, Finnerup NB, Gilron I. Medicine for pain management: a systematic review of randomised controlled trials. Pain. 2021; 162(Suppl 1):S45–S66.
Soliman N, Haroutounian S, Hohmann AG, Krane E, Liao J, Macleod M, et al. Systematic review and meta-analysis of cannabinoids, cannabis-based medicines, and endocannabinoid system modulators tested for antinociceptive effects in animal models of injury-related or pathological persistent pain. Pain. 2021;162:S26–S44.
Davies BM, Khan DZ, Mowforth OD, McNair AGK, Gronlund T, Kolias AG, et al. RE-CODE DCM (REsearch objectives and common data elements for degenerative cervical myelopathy): a consensus process to improve research efficiency in DCM, through establishment of a standardized dataset for clinical research and the definition of the research priorities. Glob Spine J. 2019;9:65S–76S.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097 https://dx.plos.org/10.1371/journal.pmed.1000097.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368. https://doi.org/10.1136/bmj.l6890.
Hooijmans CR, Rovers MM, De Vries RBM, Leenaars M, Ritskes-Hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14:43 https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-14-43.
Ahmed MM, Rajpal S, Sweeney C, Gerovac TA, Allcock B, McChesney S, et al. Cannabinoid subtype-2 receptors modulate the antihyperalgesic effect of WIN 55,212-2 in rats with neuropathic spinal cord injury pain. Spine J. 2010;10:1049–54. (Ahmed, Rajpal, Sweeney, Gerovac, Allcock, McChesney, Patel, Tilghman, Miranpuri, Resnick) Department of Neurological Surgery, University of Wisconsin, School of Medicine and Public Health, 600 Highland Ave., Madison, WI 53792, United States D. K. Resnic. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=51095068, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:20920894&id=doi:10.1016%2Fj.spinee.2010.08.015&issn.
Arevalo-Martin A, Garcia-Ovejero D, Sierra-Palomares Y, Paniagua-Torija B, Gonzalez-Gil I, Ortega-Gutierrez S, et al. Early endogenous activation of CB1 and CB2 receptors after spinal cord injury is a protective response involved in spontaneous recovery. PLoS One. 2012;7. (Arevalo-Martin, Garcia-Ovejero, Sierra-Palomares, Paniagua-Torija, Molina-Holgado) Laboratorio de Neuroinflamacion, Hospital Nacional de Paraplejicos, SESCAM, Toledo, Spain (Gonzalez-Gil, Ortega-Gutierrez) Departamento de Quimica Organica I, Facultad de. http://www.plosone.org/article/fetchObjectAttachment.action?uri=info%3Adoi%2F10.1371%2Fjournal.pone.0049057&representation=PDF, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed13&AN=366043267https://cambridge-primo.hoste.
Latini L, Bisicchia E, Sasso V, Chiurchiu V, Cavallucci V, Molinari M, et al. Cannabinoid CB2 receptor (CB2R) stimulation delays rubrospinal mitochondrial-dependent degeneration and improves functional recovery after spinal cord hemisection by ERK1/2 inactivation. Vol. 5, Cell Death Dis. 2014;5. (Latini, Bisicchia, Sasso, Chiurchiu, Cavallucci, Molinari, Maccarrone, Viscomi) Santa Lucia Foundation, IRCCS 65, Via Ardeatina 354, Rome 00179, Italy (Chiurchiu) Faculty of Veterinary Medicine, University of Teramo, Teramo, Italy (Maccarrone). http://www.nature.com/cddis/marketing/index.html, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed15&AN=603835153https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid.
Su BX, Chen X, Huo J, Guo SY, Ma R, Liu YW The synthetic cannabinoid WIN55212-2 ameliorates traumatic spinal cord injury via inhibition of GAPDH/Siah1 in a CB2-receptor dependent manner. Brain Res. 2017;1671:85–92. (Su, Huo, Ma) Department of Anesthesiology, Xijing Hospital, Fourth Military Medical University, Xi’an 710032, China (Chen) Department of Anesthesiology, Shaanxi Provincial People’s Hospital, Xi’an 710068, China (Guo) Department of Pharmaceutics, Tangdu H. http://www.elsevier.com/locate/bri, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed18&AN=617384164, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:28716633&id=do.
Su B, Dong H, Ma R, Zhang X, Ding Q, Xiong L. Cannabinoid 1 receptor mediation of spinal cord ischemic tolerance induced by limb remote ischemia preconditioning in rats. J Thoracic Cardiovasc Surg. 2009;138:1409–16. (Su, Dong, Ma, Zhang, Ding, Xiong) Department of Anesthesiology, Xijing Hospital, Fourth Military Medical University, Xi’an, Shaanxi, China L. Xiong, Department of Anesthesiology, Xijing Hospital, Fourth Military Medical University, Xi’an, Shaanxi, China. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=50620853, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:19709680&id=doi:10.1016%2Fj.jtcvs.2009.07.014&issn=.
Hama A, Sagen J. Antinociceptive effect of cannabinoid agonist WIN 55,212-2 in rats with a spinal cord injury. Exp Neurol. 2007;204:454–7. (Hama, Sagen) University of Miami Miller School of Medicine, The Miami Project to Cure Paralysis, 1095 NW 14th Terrace, (R-48), Miami, FL 33136, United States A. Hama, University of Miami Miller School of Medicine, The Miami Project to Cure Paralysis, 10. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed10&AN=46330252, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:17045264&id=doi:10.1016%2Fj.expneurol.2006.09.002&i.
Hama A, Sagen J. Sustained antinociceptive effect of cannabinoid receptor agonist WIN 55,212-2 over time in rat model of neuropathic spinal cord injury pain. J Rehabil Res Dev. 2009;46:135–44. (Hama, Sagen) Miami Project to Cure Paralysis, University of Miami Leonard M. Miller School of Medicine, Miami, FL, United States (Hama) Miami Project to Cure Paralysis, University of Miami Leonard M. Miller School of Medicine, 1095 NW 14th Terrace (R-48). http://www.rehab.research.va.gov/jour/09/46/1/pdf/hama.pdf, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=354618147, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embas.
Hama AT, Sagen J. Cannabinoid receptor-mediated antinociception with acetaminophen drug combinations in rats with neuropathic spinal cord injury pain. Neuropharmacology. 2010;58:758–66. (Hama, Sagen) The Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, 1095 NW 14th Terrace (R-48), Miami, FL 33136, United States A.T. Hama, The Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, 1. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed11&AN=50755289, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:20035773&id=doi:10.1016%2Fj.neuropharm.2009.12.010&.
Hama A, Sagen J. Activation of spinal and supraspinal cannabinoid-1 receptors leads to antinociception in a rat model of neuropathic spinal cord injury pain. Brain Res. 2011;1412:44–54. (Hama, Sagen) Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, 1095 NW 14th Terrace (R-48), Miami, FL 33136, United States A. Hama, Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, 1095 NW 14t. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed12&AN=51552397, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:21813113&id=doi:10.1016%2Fj.brainres.2011.07.031&is.
Hama AT, Pearson JP, Sagen J. Effects of repeated dosing with mechanistically distinct antinociceptive ligands in a rat model of neuropathic spinal cord injury pain. Pharmacol Res Perspect. 2014;2. (Hama, Sagen) The Miami Project to Cure Paralysis, University of Miami Miller School of Medicine, Miami, FL 33136, United States (Pearson) Ironwood Pharmaceuticals, Inc, Cambridge, MA 02142, United States A.T. Hama, The Miami Project to Cure Paralysis, U. http://onlinelibrary.wiley.com/journal/10.1002/(ISSN)2052-1707, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed15&AN=619047340, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:e.
Huo J, Ma R, Chai X, Liang HJ, Jiang P, Zhu XLING, et al. Inhibiting a spinal cord signaling pathway protects against ischemia injury in rats. J Thorac Cardiovasc Surg. 2019;157:494–503.e1. https://doi.org/10.1016/j.jtcvs.2018.07.045.
Jing N, Fang B, Wang ZL, Ma H. Remote ischemia preconditioning attenuates blood-spinal cord barrier breakdown in rats undergoing spinal cord ischemia reperfusion injury: associated with activation and upregulation of CB1 and CB2 receptors. Cell Physiol Biochem. 2017;43:2516–24. (Jing, Fang, Wang, Ma) Department of Anesthesiology, Affiliated Hospital, China Medical University, North Nanjing Street, No. 155, Shenyang, China. http://www.karger.ch/journals/cpb/cpb_jh.htm, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed18&AN=619183156, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:2913.
Kwiatkoski M, Guimaraes FS, Del-Bel E. Cannabidiol-treated rats exhibited higher motor score after cryogenic spinal cord injury Neurotox Res. 2012;21:271–80. (Kwiatkoski, Del-Bel) Department of Physiology, Faculty of Medicine of Ribeirao Preto (FMRP), Universidade de Sao Paulo, Ribeirao Preto, SP 14049-904, Brazil (Kwiatkoski, Del-Bel) Department MEF-Physiology, School of Odontology, Universidade de Sao Paulo. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed13&AN=51619303, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:21915768&id=doi:10.1007%2Fs12640-011-9273-8&issn=10.
Genovese T, Esposito E, Mazzon E, Di Paola R, Meli R, Bramanti P, et al. Effects of palmitoylethanolamide on signaling pathways implicated in the development of spinal cord injury. J Pharmacol Exp Therap. 2008;326:12–23. (Genovese, Esposito, Mazzon, Di Paola, Bramanti, Cuzzocrea) IRCCS Centro Neurolesi Bonino-Pulejo, Messina, Italy (Esposito, Meli, Calignano) Department of Experimental Pharmacology, University of Naples Federico II, Naples, Italy (Piomelli). http://jpet.aspetjournals.org/cgi/reprint/326/1/12https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed10&AN=351872139, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmi.
Hong J, Nandiwada V, Jones V, Lu M, Warner DS, Mukhopadhyay S, et al. CB1 cannabinoid receptor agonist inhibits matrix metalloproteinase activity in spinal cord injury: a possible mechanism of improved recovery. Neurosci Lett. 2015;597:19–24. (Hong, Lu, Warner, Sheng) The Multidisciplinary Neuroprotection Laboratories, Department of Anesthesiology, Duke University Medical Center, Durham, NC, United States (Hong) Department of Neurosurgery, Tangshan Gongren Hospital, Hebei, China (Lu) Departmen. http://www.elsevier.com/locate/neulet, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed16&AN=603886976, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:25881484&id.
Impellizzeri D, Cordaro M, Bruschetta G, Siracusa R, Crupi R, Esposito E, et al. N-palmitoylethanolamine-oxazoline as a new therapeutic strategy to control neuroinflammation: neuroprotective effects in experimental models of spinal cord and brain injury. J Neurotrauma. 2017;34:2609–23. (Impellizzeri, Cordaro, Bruschetta, Siracusa, Crupi, Esposito, Cuzzocrea) Department of Chemical, Biological, Pharmaceutical, and Environmental Sciences, University of Messina, Viale Ferdinando Stagno D’Alcontres, Messina 31-98166, Italy (Cuzzocrea) Manch. http://www.liebertonline.com/neu, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed18&AN=618268100, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid:28095731&id=doi.
Li H, Kong W, Chambers CR, Yu D, Ganea D, Tuma RF, et al. The non-psychoactive phytocannabinoid cannabidiol (CBD) attenuates pro-inflammatory mediators, T cell infiltration, and thermal sensitivity following spinal cord injury in mice. Cell Immunol. 2018;329:1–9. (Li, Chambers) Center for Substance Abuse Research, Lewis Katz School of Medicine, Temple University, Philadelphia, PA 19140, United States (Kong, Ganea) Microbiology and Immunology Department, Lewis Katz School of Medicine, Temple University, Philadelphi. http://www.elsevier.com/inca/publications/store/6/2/2/8/0/4/index.htt, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emexb&AN=2000770546https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid.
Paterniti I, Impellizzeri D, Crupi R, Morabito R, Campolo M, Esposito E, et al. Molecular evidence for the involvement of PPAR-delta and PPAR-gamma in anti-inflammatory and neuroprotective activities of palmitoylethanolamide after spinal cord trauma. J Neuroinflammation. 2013;10. (Paterniti, Impellizzeri, Crupi, Morabito, Campolo, Esposito, Cuzzocrea) Department of Biological and Environmental Sciences, University of Messina, Viale Ferdinando Stagno D’Alcontres, Messina 31-98166, Italy (Cuzzocrea) Manchester Biomedical Research Ce. http://www.jneuroinflammation.com/content/10/1/20, https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed14&AN=52424618, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:embase&id=pmid.
Paterniti I, Impellizzeri D, Di Paola R, Navarra M, Cuzzocrea S, Esposito E. A new co-ultramicronized composite including palmitoylethanolamide and luteolin to prevent neuroinflammation in spinal cord injury. J Neuroinflammation. 2013;10:1–11.
Noble LJ, Donovan F, Igarashi T, Goussev S, Werb Z. Matrix metalloproteinases limit functional recovery after spinal cord injury by modulation of early vascular events. J Neurosci. 2002;22:7526–35. https://pubmed.ncbi.nlm.nih.gov/12196576/.
Kundi S, Bicknell R, Ahmed Z. Spinal cord injury: current mammalian models. Am J Neurosci. 2013;4:1–12. 1.
Sharif-Alhoseini M, Khormali M, Rezaei M, Safdarian M, Hajighadery A, Khalatbari MM, et al. Animal models of spinal cord injury: a systematic review. Vol. 55, Spinal Cord. 2017;55:714–21. www.nature.com/sc.
YS G, BC H, KM J, CE H. Effect of age at time of spinal cord injury on behavioral outcomes in rat. J Neurotrauma. 2004;21:983–93. https://pubmed.ncbi.nlm.nih.gov/15318998/.
du Sert NP, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M, et al. The arrive guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol. 2020;18:e3000410 https://doi.org/10.1371/journal.pbio.3000410.
Vermersch P. Sativex() (tetrahydrocannabinol + cannabidiol), an endocannabinoid system modulator: basic features and main clinical data. Expert Rev Neurother. 2011:11;15–9. Vermersch, Patrick. Centre Hospitalier Regional Universitaire de Lille, Lille, France. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med7&AN=21449855, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:medline&id=pmid:21449855&id=doi:10.1586%2Fern.11.27&issn=1473-7175&i.
Sekar K, Pack A. Epidiolex as adjunct therapy for treatment of refractory epilepsy: a comprehensive review with a focus on adverse effects. F1000Res. 2019;8:F1000 Res. https://pubmed.ncbi.nlm.nih.gov/30854190/.
Devinsky O, Cross JH, Laux L, Marsh E, Miller I, Nabbout R, et al. Trial of cannabidiol for drug-resistant seizures in the dravet syndrome. N Engl J Med. 2017;376:2011–20. (Devinsky) New York University, Langone Comprehensive Epilepsy Center, New York, United States (Cross) University College London, Great Ormond Street Institute of Child Health, London, United Kingdom (Wright) GW Pharmaceuticals, London, United Kingdom. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medc&AN=28538134, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:medline&id=pmid:28538134&id=doi:10.1056%2FNEJMoa1611618&issn=0028-47.
Devinsky O, Patel AD, Thiele EA, Wong MH, Appleton R, Harden CL, et al. Randomized, dose-ranging safety trial of cannabidiol in Dravet syndrome. Neurology. 2018;90:e1204–11. (Devinsky) From the NYU Comprehensive Epilepsy Center (O.D.), New York, NY;Nationwide Children’s Hospital and the Ohio State University College of Medicine (A.D.P.), Columbus; Massachusetts General Hospital (E.A.T.), Boston; Wake Forest School of Medicine. https://ovidsp.ovid.com/athens/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medl&AN=29540584, https://cambridge-primo.hosted.exlibrisgroup.com/openurl/44CAM/44CAM_services_page?sid=OVID:medline&id=pmid:29540584&id=doi:10.1212%2FWNL.0000000000005254&issn=.
Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R, Leone S. Paracetamol: new vistas of an old drug. CNS Drug Rev; 2006;12:250–75. https://pubmed.ncbi.nlm.nih.gov/17227290/.
Högestätt ED, Jönsson BAG, Ermund A, Andersson DA, Björk H, Alexander JP. et al. Conversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous system. J Biol Chem. 2005;280:31405–12. https://pubmed.ncbi.nlm.nih.gov/15987694/.
Panlilio LV, Goldberg SR, Justinova Z. Cannabinoid abuse and addiction: clinical and preclinical findings. Clin Pharmacol Ther. 2015;97:616–27.
Cheriyan T, Ryan DJ, Weinreb JH, Cheriyan J, Paul JC, Lafage V, et al. Spinal cord injury models: A review. Spinal Cord. 2014;52:588–95.
Zhang N, Fang MR, Chen HH, Gou FM, Ding MX. Evaluation of spinal cord injury animal models. Neural Regen Res. 2014;9:2008–2012.
Mazensky D, Flesarova S, Sulla I. Arterial Blood Supply to the Spinal Cord in Animal Models of Spinal Cord Injury. A Review. Anat Rec. 2017;300:2091–2106.
Collins GH, West NR, Parmely JD, Samson FM, Ward DA. The histopathology of freezing injury to the rat spinal cord. A light microscope study. I. Early degenerative changes. J Neuropathol Exp Neurol. 1986;45:721–41.
Acknowledgements
We gratefully acknowledge support from the Cambridge NIHR Brain Injury MedTech Cooperative. MRNK is funded by an NIHR Clinician Scientist Award CS-2015-15-023. BMD is supported by a Royal College of Surgeons Research Fellowship and a NIHR Clinical Doctoral Research Fellowship.
Author information
Authors and Affiliations
Contributions
FIB contributed to designing review protocol and was responsible for screening potentially eligible studies, extracting and analysing data, interpreting results, creating ‘Summary of findings’ tables and writing the report. ODM and BMD were responsible for designing review protocol and provided feedback on the report. IK contributed conducting the search and screening potentially eligible studies. MBB, AIB, SA, MA, RD, BG, TO, LO, JQT, SR, GS, UW, BW contributed to screening potentially eligible studies. LS contributed to question formulation and article drafting. RDB provided feedback on the report, particularly with a focus on in vivo models, and inputted to assist with completion of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bhatti, F.I., Mowforth, O.D., Butler, M.B. et al. Systematic review of the impact of cannabinoids on neurobehavioral outcomes in preclinical models of traumatic and nontraumatic spinal cord injury. Spinal Cord 59, 1221–1239 (2021). https://doi.org/10.1038/s41393-021-00680-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00680-y
This article is cited by
-
Cannabinoids for Acute Pain Management: Approaches and Rationale
Current Pain and Headache Reports (2024)
-
Drug Repurposing for Spinal Cord Injury: Progress Towards Therapeutic Intervention for Primary Factors and Secondary Complications
Pharmaceutical Medicine (2023)