Abstract
Study design
Secondary psychometric analysis of cross-sectional previously collected data.
Objectives
Explore the floor and ceiling effects, convergent, and divergent validity of the International Spinal Cord Injury Basic Quality of Life Data Set (SCI QoL-BDS) in a sample of people with spinal cord damage (SCD) from different countries, with different causes (both traumatic and non-traumatic), and different settings.
Setting
Community dwellers with SCD in Australia, Brazil, India, The Netherlands, and USA, and inpatient rehabilitation: India.
Methods
Adults (>18 years) with chronic SCD with either traumatic or non-traumatic aetiologies living in the community (n = 624), in inpatient rehabilitation following the onset of SCI (India; n = 115) and able-bodied controls (Australia; n = 220) had the following data collected by survey or face-face interview: SCI QoL-BDS, demographic and clinical characteristics (e.g., age, gender, years post SCI/SCD, education, employment) and reference measures of quality of life, disability and depression.
Results
For the whole sample, there were no notable floor or ceiling effects, internal consistency was good (Cronbach’s alpha = 0.84) and the corrected item-total correlations generally were acceptable (all > 0.3 except for in Brazilian cohort). Convergent and divergent validity were largely confirmed though there were some aspects of validity that were suboptimal.
Conclusions
Only minor psychometric issues were identified. This preliminary analysis suggests that there are no reason for concern about the use of the SCI QoL-BDS for clinical or research purposes, notwithstanding the need for further studies.
Similar content being viewed by others
Introduction
Spinal cord damage (SCD) from any cause, whether traumatic spinal cord injury (SCI) or non-traumatic spinal cord dysfunction (SCDys), can result in body impairment, activity limitation, and participation restriction. It is typically associated with a potential decrease in quality of life (QoL) [1]. Numerous researchers have studied QoL following SCI, but results are difficult to compare because of variation in definitions of QoL, study designs, inclusion criteria, and measures used [2]. Furthermore, there is no universally accepted definition of QoL, despite efforts at defining this concept [3, 4].
To increase comparability between QoL studies, an International SCI QoL Basic Data Set (SCI QoL-BDS) [5] was developed by the International Spinal Cord Society (ISCoS) and the American Spinal Injury Association (ASIA) as part of the International SCI Data Sets Project [6]. The purpose of this SCI QoL BDS, like all International SCI Basic Data Sets, is to standardise the collection and reporting of a minimal amount of information necessary to provide clinicians and researchers with vital information and to facilitate comparing the results of different studies of QoL in individuals with SCD. It was designed to include a minimal number of data elements, which together can be included in any study and can be collected in routine clinical practice [6].
The SCI QoL-BDS was developed by an international expert committee and is based on the definition of subjective QoL as reflecting an individual’s overall perception of, and satisfaction with, how things are in his/her life [7]. Its three items rate the individual’s satisfaction with the domains of life as a whole, physical health and mental health on a scale of 0 (completely dissatisfied) to 10 (completely satisfied); higher scores reflect a better QoL [3,4,5, 7]. A total score of the QOL-BDS can be computed as the average of the three item scores (range–10).
The SCI QoL-BDS is recommended by ISCoS and ASIA for use in studies requiring measures of QoL after SCD and can be collected in routine clinical practice. A recent study from The Netherlands has reported acceptable validity of the SCI QoL-BDS in a sample of people with mostly SCI who were wheelchair users and at least 10 years post onset of SCD [8]. Further, similarity of SCI QoL-BDS scores from the United States and Brazil suggested cross-cultural validity [9]. However, in order to justify the use of the SCI QoL-BDS internationally and across the continuum of care, it needs to be validated in a range of other countries and settings.
The objective of this paper was to perform a secondary analysis of existing data previously collected independently at different sites in order to explore the psychometric properties of the SCI QoL-BDS, including the floor and ceiling effects and obtain preliminary data on reliability and validity, in a sample of people with SCD from different causes across different countries and settings. In doing so the authors focused the analyses on item functioning or performance (i.e., ceiling and floor effects), reliability (measured as internal consistency) and validity, including convergent and divergent validation. As part of testing the divergent validity, it was hypothesised that there would be significant differences in the SCI QoL-BDS scores of the following groups: (1) chronic SCD (lower scores) and controls, (2) chronic SCD and the inpatients with recent onset SCD (lower scores), and (3) inpatients with recent onset SCD (lower scores) and the controls. A secondary objective was to explore the relationship between demographic and clinical characteristics and the SCI QoL-BDS.
Methods
Study design and setting
This collaboration was an exploratory study that sought to assess the psychometric properties of the SCI QoL-BDS by way of secondary analysis of data from several cross-sectional studies. Each investigator had independently completed data collection of the SCI QoL-BDS in the country where they are based (Australia, Brazil, India, The Netherlands, and USA). SCI QoL-BDS data, study design, setting, and sample characteristics from Australia [10], The Netherlands [8], Brazil and USA [9] have been described in previous publications. Further details about the studies’ designs and settings are presented in Supplementary file 1.
Participants
All participants were adults (18 years and older) and included rehabilitation inpatients and others living in the community. Participants with either SCI or SCDys were included. Furthermore, in Australia, data was also collected from a sample of non-disabled community residing adults, to allow comparison between those with SCD and those without. All sites excluded people with severe psychiatric or cognitive impairments. Additional details regarding the inclusion criteria are shown in Supplementary file 1.
Variables
The SCI QoL-BDS was assessed in English from participants in Australia, India, and USA. In the Netherlands [8], and Brazil [9], it was translated into Dutch and Portuguese, respectively, following the recommended international guidelines [11].
Demographic variables included gender, language, marital status (married/living together vs single, divorced etc.), age at time of completion of questionnaire, number of years post onset of SCD, setting of participant at time of completion of questionnaire (inpatient rehabilitation vs. residing in community), level of education (college and higher education vs lower/intermediate education); employment status (no paid work vs some paid work).
Clinical characteristics included aetiology of SCD (SCI vs SCDys), level of SCD (paraplegia vs tetraplegia) and completeness of SCD (motor complete vs motor incomplete). The completeness of SCD was determined in Brazil, India, The Netherlands and USA according to the International Standards for Neurological Classification in SCI (ISNCSCI) [12]. Complete SCI was defined as having AIS grade A. In Australia, the grade was estimated from a brief measure of functional abilities, the Spinal Functional Abilities Scale (S-FAS) [13], because the ISNCSCI was not available for the community participants.
Self-report measures relevant to the construct validity of the SCI QoL-BDS that were collected in one or more countries, were: for QoL, the WHOQOL-BREF [14] a 5-item selection of the WHOQOL-BREF;[15] Hospital Anxiety and Depression Scale (HADS);[16] Mental Health Inventory-5 [17] and the SCI-Secondary Conditions Scale [18]. A summary of the measures collected by the participating centres is shown in Supplementary file 1.
WHOQOL-BREF
WHOQOL-BREF was developed by the WHO, it comprises 26 items that measure 4 broad domains: physical health, psychological health, social relationships, and environment [14].
WHOQOL-BREF 5-item selection
In a previous study, five items from the WHOQOL showed cross-cultural validity as a brief measure of QOL. These five items cover overall quality of life, satisfaction with health, daily activities, relationships, and living conditions [15].
Hospital Anxiety and Depression Scale
The HADS is a widely used measure of anxiety and depression. It is an ordinal scale with fourteen items, scored from 0 to 3; range of 0–21 for anxiety or depression [16]. HADS has acceptable psychometric properties in people with SCI [19]. Only the Depression score was used in this study.
Mental Health Inventory-5
Mental Health Inventory-5, is identical to the Mental Health subscale of the Medical Outcome Studies Short-Form-36 (SF-36) [17], and has been used in SCI research. It consists of five questions on mood over the last 4 weeks and has demonstrated acceptable construct validity and convergent validity in individuals with SCI [17].
SCI-Secondary Conditions Scale
SCI-Secondary Conditions Scale is a reliable and valid scale, with 16 items cover problems common in people with SCD [18]. The items are physiological in nature; they can be self-reported by patients; and can be prevented or managed. A 4-point ordinal scoring system (ranges from 0 = not experienced/insignificant problem never limiting activity to 3 = significant/chronic problem) gives a total score ranging from 0 to 48, derived by adding the problem ratings; higher scores indicate greater overall problem with secondary conditions.
Statistical methods
Descriptive analysis was performed. The mean and standard deviations as well as the median and Interquartile rage were reported for numerical summary data. Skewness was considered to be present if the corresponding statistics was below −1.0 or above 1.0.
Floor and ceiling effects
A ceiling effect is when a high proportion of subjects have the maximum scores, and floor effect is when they have the lowest scores. A notable floor or ceiling effect in an outcome measure means that there is more variance in the construct than the question is able to measure; it reduces the responsiveness of the outcome. The proportion of patients who had a floor (SCI QoL-BDS item score = 0) or ceiling (SCI QoL-BDS item score = 10) was assessed to determine the presence of a notable floor or ceiling effects. We used a threshold of 15% to assess notable floor or ceiling effects [20].
Internal consistency
The internal consistency of the SCI QoL-BDS was assessed using Cronbach’s α. Internal consistency was considered acceptable if Cronbach’s α coefficient was at least .70 and all corrected item–total correlations were larger than .30 [21].
Validity
Convergent and discriminant validity of the SCI QoL-BDS were explored [22]. Convergent validity is demonstrated by a high correlation with measures of a related construct and discriminant validity by a significant difference in scores between groups that are expected to differ.
Convergent validity was assessed using Spearman correlation because the SCI QoL-BDS involves ordinal scores. Correlations of .60 or higher between the SCI QoL-BDS items and other measures were hypothesised, because these items/instruments assess similar constructs: [2, 23]
-
SCI QoL-BDS general QoL item with the WHOQOL-BREF satisfaction with overall quality of life item (item 1);
-
SCI QoL-BDS physical health item with the overall rating of health item (item 2) and the physical health scale of the WHOQOL-BREF, and the SCI-SCS;
-
SCI QoL-BDS psychological health item with the WHOQOL-BREF negative feelings item (item 26), the WHOQOL-BREF psychological scale, and the MHI-5 or HADS-Depression;
-
SCI Qol-BDS total score with the WHOQOL-BREF total score, or the WHOQOL-5 total score
Discriminant validity was assessed by performing ANOVAs comparing the SCI QoL-BDS scores for sub-groups of participants whom we expected to differ significantly [24]. For this analysis we planned three comparisons: (1) those with chronic SCD and the controls, (2) those with chronic SCD and the inpatients with recent onset SCI, and (3) inpatients with recent onset SCI and the controls.
Finally, associations were calculated between the mean SCI QoL-BDS scores and key demographic and clinical variables to determine whether these had a relationship. Nonparametric Spearman correlations were used in all analyses because of partly skewed score distributions. We expected low correlations with demographic characteristics and low to moderate correlations with proxy measures for functioning (having work; level of SCD).
Statistical analyses were performed using SPSS version 24.0 for Windows (IBM Corporation, Armonk, NY, USA). For this study, p values of less than 0.05 were deemed statistically significant.
Results
Data were available on a total of 959 participants; 624 participants from 5 countries had chronic SCD (SCI or SCDys) and were living in the community, 115 participants from India had recent onset SCI and were undergoing initial inpatient rehabilitation, and 220 people were a convenient sample of able-bodied controls (without SCD) from Australia. The demographic and clinical characteristics of participants are shown in Table 1.
Floor and ceiling effect
The score distributions of the SCI QoL-BDS items are displayed in Table 2, and supplementary files 2 (frequency distributions) and 3 (table of floor, ceiling and skewness). There were few notable floor or ceiling effects, 19% of the Indian inpatients gave their physical health the lowest score, and 30% of the Brazilian sample gave their mental health the best positive score. Score distributions were positively skewed, indicating a clustering of scores at the high (positive) end of the scale, but within limits except for the general life satisfaction item in the Netherlands, Brazil and the Australian control sample, and the mental health item in Brazil.
Internal consistency
The internal consistency of the SCI QoL-BDS was good, with a Cronbach alpha of 0.84 in the whole sample. Good inter-item correlations were observed for all subgroups, except for the mental health item in the Brazil sample. See Table 3.
Validity
The associations between the SCI QoL-BDS components and other measures indicated generally good convergent validity, except for a low correlation between the SCI-QoL-BDS physical health item and the SCI-SCS. See Table 4 and Supplementary file 4.
In spite of group differences in terms of their neurological characteristics, few differences were found in relation to their demographic and clinical characteristics. Females and married individuals were more satisfied with their life as a whole compared to males and those who were single. Having paid work was associated with a higher rating on all three QoL scores (Supplementary file 4). Age was not significantly associated with QoL-BDS scores. Time since onset of the injury was weakly associated with satisfaction with life as a whole (r = 0.14; p < 0.001) and satisfaction with mental health (r = 0.13; p = 0.002), but not with satisfaction with physical health (r = 0.03; p = 0.410). Level of SCD was not associated with QoL-BDS scores. Completeness of SCI was only associated with satisfaction with physical health. There was no difference in QoL scores between the two aetiology groups (Supplementary file 4).
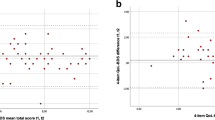
The divergent validity, determined by assessing the difference between SCI QoL-BDS scores in individuals with chronic SCD, recent SCI in inpatient rehabilitation and non-disabled individuals without SCD is shown in Table 2. These differences were highly significant for satisfaction with life as a whole (F = 109.4; p < 0.001), satisfaction with physical health (F = 184.4; p < 0.001), satisfaction with mental health (F = 38.4; p < 0.001) and the total SCI QoL-BDS (F = 136.9; p < 0.001). Post-hoc comparisons with Bonferroni correction showed all between-subgroup comparisons to be highly significant (p < 0.001), with the only exception being the difference in satisfaction with mental health between individuals with chronic SCI and controls without SCI (p = 0.60).
Discussion
Overall, our findings provide preliminary evidence that the psychometric properties of the SCI QoL-BDS are within an acceptable range. For the whole sample, there was no notable floor or ceiling effect. The findings are also generally suggestive of convergent, divergent and known groups validity. The internal consistency was good and the corrected item-correlations generally were acceptable. There were, however, some aspects of reliability and validity that were suboptimal. The item on satisfaction with mental health showed a few problems, particularly in the sample from Brazil, that warrants further investigation. The only demographic variable that was significantly associated with SCI QoL-BDS scores was employment and no clinical variables were associated.
Our results are consistent with reports from others regarding people with SCD having a lower QoL compared to healthy controls [1, 25], providing support for the discriminant validity of the SCI QoL-BDS. The outcomes of this project were in keeping with those reported for the cohort from The Netherlands [8]. The findings also concur with those of others regarding the absence of influence of the level or completeness of SCD on QoL [8, 15, 25].
To our knowledge, this is the first report comparing QoL in people with post-acute SCI still in inpatient rehabilitation to people with chronic SCD living in the community. In addition, this study compares people with SCDys to those with SCI, with no significant differences found between these groups.
Although based on retrospective data analyses, our findings provide preliminary indications of validity and reliability for the SCIQOL-BDS and it is based on data from five international sites. As such it is the first attempt to begin looking at SCI QOL-BDS data across sites and its potential use for research and clinical applications.
A number of limitations of this study need to be acknowledged. As this was a secondary analysis, these results need to be interpreted with caution, and it is not possible to generalise our findings. Because of the retrospective nature of this project, it was not possible to pre-specify the inclusion or exclusion criteria, as well as study variables and their definitions. Some variables were only collected at one or two centres. It is not possible to determine the extent to which the observed differences in SCI QoL-BDS scores between able-bodied and SCD groups were attributable to their SCD status (aetiology, level, grade, acute/chronic) and not demographic or other factors. To address these limitations, further validation studies of the SCI QoL-BDS are needed. These should be international, multi-centre, and prospective. It is suggested that cognitive interviews [26] be conducted with people with SCD in different countries to determine the cross-cultural validity, that is, if the understanding of the concept of QoL after SCD is uniform and consistent. Reliability testing is also required. Funding has been obtained for a prospective study that will be addressing these limitations. Longitudinal studies of QoL are also required, that start from inpatient rehabilitation, as well as determination of test-retest reliability.
In conclusion, based on the data analysed here the SCI QoL-BDS shows acceptable psychometric properties, with some previously identified issues discussed. We found no reason for concern about the use of the SCI QoL-BDS, notwithstanding the need for further studies.
References
Post MW, van Leeuwen CM. Psychosocial issues in spinal cord injury: a review. Spinal Cord. 2012;50:382–9.
Hill MR, Noonan VK, Sakakibara BM, Miller WC. Quality of life instruments and definitions in individuals with spinal cord injury: a systematic review. Spinal Cord. 2010;48:438–50.
Dijkers MP. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42(Suppl 1):87–110.
Post M. Quality of life after spinal cord injury. J Neurol Phys Ther. 2005;29:139–46.
Charlifue S, Post MW, Biering-Sørensen F, Catz A, Dijkers M, Geyh S, et al. International spinal cord injury quality of life Basic Data Set. Spinal Cord. 2012;50:672–5.
Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T, et al. International spinal cord injury data sets. Spinal Cord. 2006;44:530–4.
Wood-Dauphinee S, Exner G, Bostanci B, Glass C, Jochheim KA, Kluger P, et al. Quality of life in patients with spinal cord injury—basic issues, assessment, and recommendations. Restor Neurol Neurosci. 2002;20:135–49.
Post MWM, Adriaansen JJE, Charlifue S, Biering-Sørensen F, van Asbeck FWA. Good validity of the international spinal cord injury quality of life basic data set. Spinal Cord. 2016;54:314–8.
Tate D, Forchheimer M. Review of cross-cultural issues related to quality of life after spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20:181–90.
New PW, Currie KE. Development of a comprehensive survey of sexuality issues including a self-report version of the International Spinal Cord Injury sexual function basic datasets. Spinal Cord. 2016;54:584–91.
Biering-Sørensen F, Alexander MS, Burns S, Charlifue S, DeVivo M, Dietz V, et al. Recommendations for translation and reliability testing of International Spinal Cord Injury Data Sets. Spinal Cord. 2011;49:357–60.
Kirshblum SC, Burns SB, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
New PW. Secondary conditions in a community sample of people with spinal cord damage. J Spinal Cord Med. 2016;39:665–70.
WHOQoL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–8.
Geyh S, Fellinghauer BA, Kirchberger I, Post MW. Cross-cultural validity of four quality of life scales in persons with spinal cord injury. Health Qual Life Outcomes. 2010;3:94.
Snaith RP. The hospital anxiety and depression scale. Health Qual life Outcomes. 2003;1:29.
Van Leeuwen CM, van der Woude LH, Post MW. Validity of the mental health subscale of the SF-36 in persons with spinal cord injury. Spinal Cord. 2012;50:707–10.
Kalpakjian C, Scelza W, Forchheimer M, Toussaint L. Preliminary reliability and validity of a Spinal Cord Injury Secondary Conditions Scale. J Spinal Cord Med. 2007;30:131–9.
Woolrich R, Kennedy P, Tasiemski T. A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychol Health Med. 2006;11:80–90.
McHorney C, Tarlov A. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4:293–307.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42.
Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 4th ed. New York: Oxford University Press; 2008.
Visser-Meily JM, Post MW, Riphagen II, Lindeman E. Measures used to assess burden among caregivers of stroke patients: a review. Clin Rehabil. 2004;18:601–23.
van Leeuwen CM, Post MW, Hoekstra T, van der Woude L, de Groot S, Snoek GJ, et al. Trajectories in the course of life satisfaction after spinal cord injury: identification and predictors. Arch Phys Med Rehabil. 2011;92:207–13.
Boakye M, Leigh BC, Skelly AC. Quality of life in persons with spinal cord injury: comparisons with other populations. J Neurosurg Spine. 2012;17(Suppl):29–37.
Acquadro C, Conway K, Hareendran A, Aaronson N. European Regulatory Issues and Quality of Life Assessment (ERIQA) Group. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health. 2008;11:509–21.
Acknowledgements
Some of the results were presented at the 2016 International Spinal Cord Society annual meeting, Vienna, Austria.
Author information
Authors and Affiliations
Contributions
PWN, MWMP and DGT conceived the project. All authors contributed to the data collection and analysis plan. MWMP analysed the data. PWN prepared the first draft of the manuscript. All authors contributed to the manuscript revisions and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Anonymous data were sent to one of the authors (MWMP) who performed all statistical analyses. Institution-specific agreements to this data-sharing were made and signed, if required, in the respective country.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
New, P.W., Tate, D.G., Forchheimer, M.B. et al. Preliminary psychometric analyses of the International Spinal Cord Injury Quality of Life Basic Data Set. Spinal Cord 57, 789–795 (2019). https://doi.org/10.1038/s41393-019-0273-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0273-5
This article is cited by
-
The social dimension of quality of life following spinal cord injury or disease: an international ICF-linking study
Spinal Cord (2024)
-
Reciprocal association between pain and quality of life after newly acquired spinal cord injury
Quality of Life Research (2024)
-
Predictors of resilience for people with spinal cord injury over two periods of COVID-19 social distancing restrictions: a 12-month longitudinal study using structural equation modelling
BMC Public Health (2023)
-
Internal consistency and convergent validity of the International Spinal Cord Injury Quality of Life Basic Data Set at discharge from first rehabilitation
Spinal Cord (2022)
-
Longitudinal measurement invariance of the international spinal cord injury quality of life basic data set (SCI-QoL-BDS) during spinal cord injury/disorder inpatient rehabilitation
Quality of Life Research (2022)