Abstract
Study design
Multi-center, repeated measures
Objectives
Evaluate psychometric properties of the SCIM-III in children.
Setting
Seven facilities in North America
Methods
One-hundred and twenty-seven youths, mean age of 10.8 years and chronic spinal cord injury/dysfunction completed two administrations of the Spinal Cord Independence Measure-III (SCIM-III). Mean, standard deviation, range values were calculated for SCIM-III total and subscales for the entire sample, four age groups and injury characteristics. Test-retest reliability, concurrent validity, and floor and ceiling effects were examined.
Results
Total SCIM-III and self-care (SC) subscale scores for the youngest age group were lower than those for the three older age groups. There were statistically significant differences in SC subscale scores between neurological level (NL) C5-T1 and T2 -T12; C5-T1 and L1-S4/5; and T2-T12 and L1-S4/5 and in in-room, and indoor/outdoor mobility subscale scores between C1-C4 and T2-T12; C1-C4 and L1-S4/5; C5-T1 and T2-T12; C5-T1 and L1-S4/5; and T2-T12 and L1-S4/5. All scores between motor complete and motor incomplete differed. Test-retest reliability was good (ICC values = > 0.84) and there was moderate to strong correlation between SCIM-III and the FIM® Instrument (r = 0.77–0.92). Ceiling effects were present in the SC subscale for the oldest age group (24%) and for NL L1-S4/5 (35.5%) and in in-room mobility subscale for 6–12 (45.7%), 13–15 (30.43%) and 16–17 (60%) ages, paraplegia (42.4%), tetraplegia (37.1%), incomplete injuries (50%), and T2-T12 (38%) and L1-S4/5 (100%) NL.
Conclusion
Despite limitations in content range, the SCIM-III is reproducible, and a valid indicator of physical functioning in youth with SCI/D 6 years of age and older.
Sponsorship
The study was funded by the Craig H. Neilsen Foundation, Spinal Cord Injury Research on the Translation Spectrum, Senior Research Award Grant #282592 (Mulcahey, PI)
Similar content being viewed by others
Introduction
The Spinal Cord Independence Measure (SCIM-III) is a disability rating scale of overall physical function that assesses ability in 19 activities across three domains (self-care, respiration and sphincter, and mobility) [1,2,3,4,5,6,7]. Total SCIM-III scores range between 0–100, with higher scores reflecting greater independence and level of function. Sub-scores can be calculated for self-care (six items, score range = 0–20), respiration and sphincter (four items, score range = 0–40), and mobility (nine items, score range = 0–40). Mobility function can be further analyzed into two subscales, one for in-room mobility and toilet (three items, score range = 0–10), and another for indoor and outdoor mobility (six items, score range = 0–30). The ideal method for scoring SCIM items is through observation of performance, but items not readily observable (sphincter management) are scored by chart review [6, 7]. Scoring by interview can also occur with small decreases in precision [8]. Strong psychometric properties of the SCIM-III have been well established in clinical samples of adults with spinal cord injury SCI [2,3,4], and is likely the reason why it is the only instrument of overall physical function that is highly recommended for use in SCI clinical trials [9], and endorsed by the international community [10,11,12,13,14].
The SCIM-III items are highly relevant to youth with SCI and dysfunction (SCI/D), and to outcomes of pediatric rehabilitation and research [15]. Given this relevance, the strong psychometric properties of the SCIM-III in adults, and recent trends in enrolling adolescents with SCI into clinical trials it is important to evaluate the SCIM-III in youth. The purpose of this study was to evaluate the lower age in which the SCIM-III has utility, and to establish the psychometric properties of the SCIM-III in youth with SCI/D.
Methods
Design
This study was part of a larger multi-center repeated measures study aimed to examine the psychometric properties of instruments used for adult SCI clinical trials in children and youths, and to determine the lower age in which the instruments have utility.
Participants
Between April 2014 and September 2016, a sample of convenience was recruited at the point-of-care at seven facilities across the United States specializing in pediatric SCI rehabilitation. Eligible participants had a traumatic or non-traumatic acquired SCI/D of at least 3 months duration, were between 2 and 17 years of age, and spoke and/or read English. Youths were excluded if they had progressive spinal cord disease (i.e., spinal muscle atrophy, muscular dystrophy), spina bifida, traumatic brain injury that interfered with comprehension and following directions, suspected conversion syndrome or suicidal ideation as defined by being on one-to-one status. Children younger than 24 months of age were excluded because they would not be expected to participate in activities included in the SCIM-III assessment from a developmental perspective. The study was approved by each of the seven participating facility’s ethics/IRB committee. Prior to participation, written parental consent was obtained for all participants from parents/legal guardians, and youth, aged 7–17 years also provided written assent.
Data collection tools and instruments
Demographic data
We developed a study specific case report form (CRF) using the National Institutes Neurological Diseases and Stroke (NINDS) common data elements (CDE) [9, 16] to record month and year of birth, gender, ethnicity, race, primary language, hand dominance, date of injury, cause of injury, type of schooling, and the child’s highest educational level.
Neurological data
The International Standards for Neurological Classification of SCI (ISNCSCI) [17] was used to determine severity, neurological level (NL) and American Spinal Injury Association Impairment Scale (AIS). This was completed at the time of study participation or obtained from the medical record as long as it was within 1 year of study participation.
Spinal Cord Independence Measure
The SCIM-III [1] is a 19-item disease specific scale that measures daily activities of high relevance to persons with SCI. The SCIM-III generates a total score between 0–100, where higher scores reflect greater level of physical function [18], and scores for three subscales including self-care (score range between 0–20), respiration and sphincter (score range between 0–40), and mobility (in-room mobility, score range between 0–10; indoor-outdoor mobility, score range between 0–30). Three large-scale psychometric studies [2,3,4] with adults demonstrated moderate to high reliability of scores across raters, broader content range when compared to the FIM® Instrument, and responsiveness to functional change between admission to and discharge from initial rehabilitation. Additional work has established clinically important differences in SCIM-III scores [19, 20] and expected values for neurologically complete injuries [5]. We have previously established the content validity of the SCIM-III for children [15].
The SCIM-III was developed as a performance measure for which raters observe performance of each SCIM-III item, and record the observed level of functioning, using the SCIM-III scoring criteria [1], but has also been validated for administration by way of interview [8] and self-report [21, 22].
FIM® Instrument
The FIM® Instrument [23] and WeeFIM® Instrument and for children [24] are used widely to assess physical and cognitive dimensions of persons with SCI. The FIM® Instrument is comprised of 18-items grouped into two subscales, FIM® motor and FIM® cognitive. The FIM® motor contains 13 items that evaluate eating, grooming, bathing, dressing, bladder and bowel management, body transfers, and mobility including walking, wheeled and stairs. Each FIM® motor item is scored using a 7-point ordinal scale where “1” represents total physical assistance, and “7” represents complete independence, with no physical assistance, supervision, or devices. The score of each FIM® motor item is summed to obtain a total FIM® motor score, that ranges between 13 and 91. The FIM® motor was used as the gold-standard instrument, to evaluate validity of the SCIM-III.
Investigator and rater training
A two-day face-to-face meeting was convened during which time investigators and research assistants were trained in the study’s data collection, management, and transmission protocols. SCIM-III items and response scales, and recommendations for SCIM-III administration proposed by Anderson et al. [4] were reviewed. Clarity on administration and scoring of two SCIM-III items (steps and bowel) was provided by the SCIM-III author prior to implementation (email communication with Dr. Catz, March 2014). The FIM® items and response scales were also reviewed, and following the investigators’ meeting, research assistants, who were all either licensed occupational or physical therapists, completed the online FIM® Instrument training and credentialing program provided by the Uniform Data System for Medical Rehabilitation, prior to them collecting data. Each investigator and research assistant were provided with a study manual that contained standardized case report forms (CRFs) for collection and recording of demographic and neurological data, and procedural guidelines, including those for de-identifying data and transmitting them to the lead site.
Data collection and management procedures
Demographic data were obtained from the medical record and by way of interview with the participant and parent. ISNCSCI examinations were obtained from the medical records, if performed within 1 year of study enrollment. If unavailable or if the ISNCSCI in the medical record dated back more than 1 year, the ISNCSCI examinations were done by trained physicians, physician assistants, or therapists at each site. If an ISNCSCI examination was not completed due to age or refusal, a series of questions were asked about volitional movement in the lower extremities, sensibility during bowel programs, and spasticity.
The SCIM-III and FIM® Instrument were administered on two separate occasions by the same rater, using a combination of observation and interview. For children younger than 5 years of age, the parent was the primary respondent and for children younger than 13 years of age, the parent supplemented information provided by the participants. Youths 13 years of age and older were the primary respondents. The same method was used for each administration for an individual participant. The sequence of SCIM-III and FIM® Instrument administration was randomly determined by each site. The time between repeated measures ranged between 1–12 h for 91 (73.%) participants, and between 12–24 h for 32 (26%) participants. One participant completed the second test session 1 week following the initial administration. Data were recorded on the standardized SCIM-III and FIM® Instrument scoring sheets.
Each of the seven facilities was assigned a facility identification number that was used in combination with a unique identification number to de-identify data prior to transmitting them to the lead site. Once transmitted, the study coordinator reviewed the data for completeness, and for quality. In the event of incomplete data, or appearance of poor quality, inconsistency or inaccuracy, data were returned to the site with specific questions and instructions for review. Following quality review, data were entered into a secure study specific database. For the duration of the study, biweekly team meetings were conducted via teleconference to monitor enrollment, discuss study procedures, and to provide clarity on data collection, management, and transmittal procedures.
Data analysis
Data were exported to SAS v 9.4 (SAS Institute, Cary, NC) for analysis. Mean (M), standard deviation (SD) and range (R) values were calculated for SCIM-III total and subscales for the entire sample, four age groups (2–5; 6–12; 13–15; 16–17), NL, AIS category and type (paraplegia/tetraplegia) of injury. Results were examined with reference to published adult values. Analysis of variance (ANOVA) was used to examine differences in SCIM-III total and subscale scores across age groups, NL, AIS category, and between paraplegia and tetraplegia.
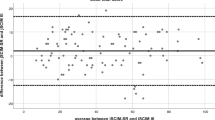
Reliability of repeated SCIM-III scores was examined using intraclass correlation coefficient (ICC) (model 2,1), with 95% confidence intervals. ICC values above 0.75 were considered indicative of good reliability, and values that exceeded 0.90, excellent reliability [25]. Concurrent validity between SCIM-III and FIM® Instrument total and subscales was examined using Pearson product-moment coefficient of correlation (r); r coefficients ranging from 0.25–0.50 were interpreted as having a fair degree of relationship, values ranging between 0.50–0.75 were interpreted as having moderate to good relationship, and values that exceeded 0.75 were considered as having a good to excellent relationship [25]. Floor and ceiling effects were examined for the SCIM –III total and subscales for the entire sample, four age groups, NL, AIS category, and paraplegia and tetraplegia. Ceiling effects were considered negligable at ≤5%, acceptable at ≤20%, and poor at >20% [26].
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this study.
Results
Of the 163 participants who were screened for participation, 36 failed screening due to: declined invitation to participate (n = 13); did not speak and/or read English (n = 9); were too young or unable to follow instructions (n = 7); had C1-C2 level injuries with concomitant brain injuries (n = 4); legal guardians were unavailable for consent (n = 2); and were on post-surgical restrictions that disallowed performance of activities (n = 1). As summarized in Table 1, 127 youths with a mean age of 10.8 years (range = 2–17 years), and a mean time since injury of 4.8 years (range = 3 months–17 years) were enrolled. The majority of participants were Caucasian (84%), non-Hispanic (81%), and had injuries that resulted in paraplegia (72%), with slightly more boys (54%) than girls. Non-traumatic acquired etiologies were the primary cause of injury (51%) followed by transport, which include vehicular crashes and pedestrian-vehicular accidents (37%). Of the 127 participants who completed the first SCIM-III administration, 124 completed the second administration of the SCIM-III. There were no significant differences between those who completed both SCIM-III administrations and those who completed only the first administration (Table 1).
Mean, standard deviation, and range values for SCIM-III subscales and total scale are shown for the entire sample, with reference to published adult reports (Table 2), for each of the four pediatric age groups (Table 3), and for NL, AIS, and type of injury (Table 4). Values for C2-C3, and C4-5 were higher than reported for adults, but comparable to adults for NL groups C6-T1, T2-T6, T7-T12, and L1-L2 [5].
As expected, total SCIM and self-care subscale scores for the youngest age group were statistically lower than the total and self-care subscale scores for the three older age groups (shown in Table 5). Significant differences between the 2–5 and 16–17 year age groups were also seen in respiratory/sphincter and indoor mobility subscale scores. No other differences were found across age groups.
There were no differences in total score or in each subscale score between C1-4 and C5-T1 NL groups (Table 5). Except for L1-S4/5 NL group having significantly higher (better) total SCIM and respiratory/sphincter subscale scores, there were no other statistically significant differences in total SCIM or respiratory/sphincter subscale scores across NL groups (Table 5). As shown in Table 5, there were statistically significant differences in self-care subscale scores between NL groups C5-T1 and T2 -T12; C5-T1 and L1-S4/5; and T2-T12 and L1-S4/5. Likewise, there were statistically significant differences in in-room and indoor/outdoor mobility subscale scores between C1-C4 and T2-T12; C1-C4 and L1-S4/5; C5-T1 and T2-T12; C5-T1 and L1-S4/5; and T2-T12 and L1-S4/5 (Table 5).
There were statistically significant differences in total and all subscale scores between AIS A/B (motor complete) and AIS C/D (motor incomplete) (Table 5). When AIS A and AIS B/C/D scores were compared, significant differences were only seen in total and indoor/outdoor mobility subscale scores, but not in self-care, respiratory/sphincter or in-room mobility subscale scores (Table 5). Self-care and in-room mobility subscale scores differed, with statistical significance being present when comparing individuals with paraplegia and tetraplegia.
Test-retest reliability was good across all age, NL, severity (complete/incomplete) and type of injury (paraplegia/tetraplegia) comparisons as evidence by ICC values = > 0.84, with the majority of them > 0.90. Lack of variability in in-room mobility across participants designated as AIS D prevented ICC calculations. There was strong correlation between total SCIM and FIM® Instrument total scores (r = 0.92, p < 0.0001), SCIM and FIM® self-care subscales (r = 0.92, p < 0.0001), SCIM respiratory/sphincter and FIM® bladder/bowel subscales (r = 0.89, p < 0.0001), and good correlation between SCIM in-room mobility and FIM® transfer subscales (r = 0.81, p < 0.0001) and SCIM indoor/outdoor mobility and FIM® walk/stairs subscales (r = 0.77, p < 0.0001).
There were no floor effects for the total SCIM-III or any subscale for any sample analysis. When examined for the total sample, each of the four age groups, type (paraplegia/tetraplegia), severity (complete/incomplete) and NL, SCIM-III total scale showed negligible ceiling effects (<2%). The SCIM SC subscale showed acceptable ceiling effects (<20%) for 0–5, 6–12, and 13–16 age groups, paraplegia and tetraplegia, complete and incomplete injuries, and NL C1-C4, C5-T1, and T2-T12. However, unacceptably high ceiling effects were present in the SC subscale for the oldest age group (24%) and for NL group L1-S4/5 (36%). Except for unacceptably high ceiling effects for L1-S4/5 (38%) and incomplete injuries (24%), ceiling and floor effects for the respiration/sphincter subscale were small (<15%). The in-room mobility subscale had unacceptably high ceiling effects for 6–12 (46%), 13–15 (30%) and 16–17 (60%) age groups, paraplegia (42%), tetraplegia (37%), incomplete injuries (50%), and for T2-T12 (38%) and L1-S4/5 (100%) NL groups. Ceiling effects for indoor and outdoor mobility were acceptable for all sample analyses.
Discussion
This study established several important psychometric properties of the SCIM-III, when used with children and youth with SCI/D. First, the scores for the total scale and sub-scales followed a relatively predictable pattern, with lower scores (less function) seen for youth with higher degrees of impairment, and higher scores (better function) for youth with less impairment. This trend was present when examined as a function of ISNCSCI neurologic level, AIS classification, and type of SCI (tetraplegia/paraplegia). It is important to note that despite this trend, SCIM-III total and subscale scores were not significantly different across all comparisons. In fact, the only comparison that resulted in statistically significant differences in scores for the total SCIM-III and each subscale was with motor complete versus motor incomplete injuries, where the motor incomplete group had significantly higher scores in the total SCIM-III score, and in each subscale, indicating a higher level of functioning in all areas assessed by SCIM-III. The only other comparison that had similar findings was with NL group L1-S4/5, where total SCIM-III and each subscale score was significantly higher than scores from the three other NL groups, except for the SC score comparison with the T2-T12 NL group. The fact that the SCIM-III total and subscale scores did not consistently show significant differences across all comparisons is not necessarily a limitation of the instrument, but rather may illustrate how the three domains of function (as measured by the different subscales) are disproportionately affected by the NL of injury. It is possible that some comparison groups were in fact quite similar as reflected in these results or that the measure may not be sensitive to small differences. However, this points to the need for further deliberation about how best to group participants by known differences.
A second important finding of this study concerned the comparison of SCIM-III scores between the youngest age group and the three older age groups. As one would anticipate, when compared to the scores from each of the three older age groups, SCIM-III total and self-care scores for the youngest age group (2–5) were considerably lower. Lower SCIM-III self-care scores in the 2–5 year age group may be due to injury-related factors, but are more likely attributed to typical developmental expectations for independence in eating, dressing, and grooming. As an example, children as young as 24 months may use a spoon, but do not achieve full independence in utensil use until 6 years of age or older [27]. Likewise, while children as young as 24 months remove socks, children do not become independent with all aspects of dressing until 5 years of age, and may require help with some aspects (belts, tying, etc.) at 6 and 7 years of age [27]. Published normative data on developmental self-care skills can aid in the interpretation of SCIM-III SC scores for the youngest age group, but normative data on SCIM-III items are needed for full utility of the scale in youth, particularly within the youngest age group. For these reasons, the SCIM-III is not recommended for use in children under 6 years of age.
Another important property of the SCIM-III relates to the SC subscale. The SC subscale demonstrated the ability to discriminate between and among more comparisons than the total scale and each of the other subscales. In fact, the SC subscale discriminated not only between the youngest and older age groups and motor complete and incomplete injuries, but also between paraplegia and tetraplegia, and among NL groups C1-C4 and T2-T12; C1-C4 and L1-S4/5;C5-T1 and T2-T12; and C5-T1 and L1-S4/5. The ability of a scale to discriminate between or among groups with known differences is an important psychometric property, and one that SCIM-III SC subscale demonstrates in pediatrics.
The results of the study also demonstrated strong reliability of SCIM-III total and subscale scores on repeated administration. Strong reliability of scores on repeated administration under conditions where change is not expected is a fundamental measurement property, and essential for instruments that are used to evaluate treatment outcomes. Finally, this study demonstrated strong correlation between the SCIM-III and the FIM® Instrument, providing further validation of the SCIM-III in children.
This study also revealed limitations of several SCIM-III subscales in content range. The unacceptably high ceiling effects of the SC subscale for the 16–17 year age group and L1-S4/5 NL group, and of the in-room mobility subscale for the three older age groups, paraplegia and tetraplegia, incomplete injuries, and NL groups T2-T12 and L1-S4/5 are major limitations of the scale, and must be considered in the decision to use the SCIM-III with children with those characteristics. Previous reports have cited ceiling and floor effects as potential limitations of the SCIM-III [28].
When compared to adult scores, SCIM-III total and subscale scores from the pediatric sample were slightly higher, indicating better overall function than the samples studied by Itzkovich et al. [2] and Fekete et al. [21]. The higher scores in the pediatric sample may be due to the chronicity of the injury (4.8 years) and having more years of experience with performing activities similar to the SCIM-III items, whereas the adult samples had more recent injuries and less exposure to activity performance. It is also plausible that youth with SCI/D have better overall function when compared to adults [29], due to relatively smaller and lighter bodies, greater flexibility, and other factors such as access to therapy services over a greater period of time. This finding highlights the importance of establishing pediatric-SCI references for SCIM-III, as a way to establish objective criterion for SCIM-III items as a function of injury characteristics and age.
There are limitations to this study. First, we administered the SCIM-III using a combination of observation and interview. With interview, it is possible that children and caregivers over or underestimated their performance. While observation of performance is the assessment mode of choice during in-patient rehabilitation, administration of the SCIM-III in an outpatient or ambulatory care center is typically done by way of interview or self report, due to restrictions of time and resources. For this reason, a SCIM-III self-report for youth (SCIM-III SR-Y) has recently been developed [15] and is currently undergoing psychometric testing. For children and youth, we advocate that the SCIM-III be administered as intended (observation of performance) and the SCIM-III SR-Y be used for interview. Work on developing normative and criterion references for the SCIM-III for pediatric SCI/D is needed, and when undertaken should administer the SCIM-III by observation of actual performance.
The time between repeated measures of the SCIM-III was short, and recall (interview) or fatigue (performance) may have influenced the second administration. We did not provide any therapy to ensure participants were functioning at their greatest potential, nor did we record information about whether participants were actively involved in therapy. The sample in the study does not fully represent the population of pediatric SCI/D, and there a relatively large portion of the sample (27.5%) that did not have formal ISNCSCI examinations.
Conclusion
The SCIM-III is reliable, and a valid indicator of physical functioning in youth with SCI/D who are 6 years of age and older. The utility of the instrument for youth would be greatly enhanced with normative references, especially for SC. Likewise, utility of the instrument for children of all ages would be enhanced with criterion reference that consider both age and injury characteristics. The unacceptably high ceiling effects are concerning, particularly if the SCIM-III is used to evaluate treatment effectiveness. In general, SCIM-III items and response scale are not developmentally relevant to children under 24 months of age, and given the wide developmental difference in pre-school children and lack of normative references for the SCIM-III, it is not recommended for children younger than 6 years old.
References
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM—spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6.
Itzkovich M, Gelernter I, Biering-Sorenson F, Weeks C, Laramee MT, Craven BC, et al. The spinal cord independence measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33.
Bluvshtein V, Front L, Itzkovich M, Aidinoff E, Gelernter I, Hart J, et al. SCIM III is reliable and valid in a separate analysis for traumatic spinal cord lesions. Spinal Cord. 2011;49:292–6.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K, et al. United states (US) multi-center study to assess the validity and reliability of the spinal cord independence measure (SCIM III). Spinal Cord. 2011;49:880–5.
Aidinoff E, Front L, Itzkovich M, Gelernter I, Hart J, Biering-Sørensen F, et al. Expected spinal cord independence measure, third version, scores for various neurological levels after complete spinal cord lesions. Spinal Cord. 2011;49:893–6.
Catz A, Itzkovich M. Spinal cord independence measure: comprehensive ability rating scale for the spinal cord lesion patient. J Rehabil Res. 2007;44:65–8.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J, et al. Disability assessment by a single rater or a team: a comparative study with the Catz-Itzkovich Spinal Cord Independence Measure. J Rehabil Med. 2002;34:226–30.
Itzkovich M, Tamir A, Philo O, Steinberg F, Ronen J, Spasser R, et al. Reliability of the Catz-Itzkovich Spinal Cord Independence Measure assessment by interview and comparison with observation. Am J Phys Med Rehabil. 2003;82:267–72.
Biering-Sorenson F, Alai S, Anderson K, Charlifue S, Chen Y, DeVivo M, et al. Common data elements for spinal cord injury clinical research: A National Institute for Neurological Disorders and Stroke project. Spinal Cord. 2015;53:265–77.
Bonavita J, Torre M, China S, Bressi F, Bonatti E, Capirossi R, et al. Validation of the Italian version of the Spinal Cord Independence Measure (SCIM III) Self-Report. Spinal Cord. 2016;54:553–60.
Wannapakhe J, Saensook W, Keawjoho C, Amatachaya S. Reliability and discriminative ability of the spinal cord independence measure III (Thai version). Spinal Cord. 2016;54:213–20.
Michailidou C, Marston L, De Souza LH. Translation into Greek and initial validity and reliability testing of a modified version of the SCIM III, in both English and Greek, for self-use. Disabil Rehabil. 2016;38:180–8.
Unalan H, Misirlioglu TO, Erhan B, Akyuz M, Gunduz B, Irgi E, et al. Validity and reliability study of the Turkish version of Spinal Cord Independence Measure-III. Spinal Cord. 2015;53:455–60.
Aguilar-Rodríguez M, Peña-Pachés L, Grao-Castellote C, Torralba-Collados F, Hervás-Marín D, Giner-Pascual M. Adaptation and validation of the Spanish self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord. 2015;53:451–4.
Mulcahey MJ, Calhoun CL, Sinko R, Kelly EH, Vogel LC. The spinal cord independence measure (SCIM)-III self report for youth. Spinal Cord. 2016;54:204–12.
Mulcahey MJ, Vogel LC, Sheikh M, Arango-Lasprilla JC, Augutis M, Garner E, et al. Recommendations for the National Institute for Neurologic Disorders and Stroke Spinal Cord Injury Common Data Elements for Children and Youth with SCI. Spinal Cord. 2017;55:331–40.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med. 2011;34:547–54. https://doi.org/10.1179/107902611X13186000420242.
Catz A, Itzkovich M. Spinal cord independence measure: comprehensive ability rating scale for the spinal cord lesion patient. J Rehabil Res. 2007;44:65–8.
Scivolette G, Tamburella F, Laurenza L, Molinari M. The spinal cord independence measure: how much change is clinically significant for spinal cord injury subjects. Disabil Rehabil. 2013;35:1808–13.
Corallo V, Torre M, Ferrara G, Guerra F, Nicosia G, Romanelli E, et al. What do spinal cord injury patients think of their improvement? A distribution and anchor based study of the minimal clinically important difference of the Spinal Cord Independence Measure III (SCIM III). Eur J Phys Rehabil Med. 2017;53:508–15. https://doi.org/10.23736/S1973-9087.17.04240-X.
Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Luthi H, et al. Development and validation of a self-report version of the spinal independence measure (SCIM III). Spinal Cord. 2013;51:40–7. https://doi.org/10.1038/sc.2012.87.
Michailidou C, Marston L, De Souza LH. Using the Spinal Cord Independence Measure (SCIM III) by self-use. Disabil Rehabil. 2016;38:1325–6. https://doi.org/10.3109/09638288.2015.1080765.
Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18.
Msall ME, DiGaudio K, Rogers BT, LaForest S, Catanzaro NL, Campbell J, et al. The functional independence measure for children (WeeFIM). Conceptual basis and pilot use in children with disabilities. Clin Pediatr (Phila). 1994;33:421–30.
Portney LG, Watkins MP. Foundations of clinical research. Applications to practice. 3rd ed. Philadelphia: FA Davis Company; 2015.
Andresen EM. Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil. 2000;81(Suppl 2):S15–20.
Haley SM, Coster WJ, Ludlow L, Haltiwanger JT, Andrellos PJ. The Pediatric Evaluation of Disability Inventory. 1992. http://www.pearsonclinical.com/childhood/products/100000505/pediatric-evaluation-of-disability-inventory-pedi.html.
Ackerman P, Morrison SA, McDowell S, Vazquez L. Using the Spinal Cord Independence Measure III to measure functional recovery in a post-acute spinal cord injury program. Spinal Cord. 2010;48:380–7.
JA MA, Post MWM, Gorter JW, Martin Ginis KA, TheSHAPE-SCI Research Group. Differences in health, participation and life satisfaction outcomes in adults following paediatric- versus adult-sustained spinal cord injury. Spinal Cord. 2016;54:1197–120.
Acknowledgements
The study was funded by the Craig H. Neilsen Foundation, Spinal Cord Injury Research on the Translation Spectrum, Senior Research Award Grant #282592 (Mulcahey, PI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Mulcahey receives research support from the Shriners Hospitals for Children, National Institute Neurological Disease and Stroke, The Craig H. Neilsen Foundation and The Rick Hansen Institute. She receives compensation for her role as Associate Editor for Topics in Spinal Cord Rehabilitation, royalties for the textbook “The Child and Young Adult with Spinal Cord Injury” and has received compensation as review panel chair/member for the Dept. of Defense and the Craig H. Neilsen Foundation. Dr. Vogel receives compensation for his role as Editor for Topics in Spinal Cord Injury Rehabilitation, royalties for the textbook “The Child and Young Adult with Spinal Cord Injury” and has received compensation as review panel chair/member for the Dept. of Defense. The remaining authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mulcahey, M., Thielen, C.C., Sadowsky, C. et al. Despite limitations in content range, the SCIM-III is reproducible and a valid indicator of physical function in youths with spinal cord injury and dysfunction. Spinal Cord 56, 332–340 (2018). https://doi.org/10.1038/s41393-017-0036-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-017-0036-0