Abstract
Apnoea, a pause in respiration, is ubiquitous in preterm infants and are often associated with physiological instability, which may lead to longer-term adverse neurodevelopmental consequences. Despite current therapies aimed at reducing the apnoea burden, preterm infants continue to exhibit apnoeic events throughout their hospital admission. Bedside staff are frequently required to manually intervene with different forms of stimuli, with the aim of re-establishing respiratory cadence and minimizing the physiological impact of each apnoeic event. Such a reactive approach makes apnoea and its associated adverse consequences inevitable and places a heavy reliance on human intervention. Different approaches to improving apnoea management in preterm infants have been investigated, including the use of various sensory stimuli. Despite studies reporting sensory stimuli of various forms to have potential in reducing apnoea frequency, non-invasive intermittent positive pressure ventilation is the only automated stimulus currently used in the clinical setting for infants with persistent apnoeic events. We find that the development of automated closed-looped sensory stimulation systems for apnoea mitigation in preterm infants receiving non-invasive respiratory support is warranted, including the possibility of stimulation being applied preventatively, and in a multi-modal form.
Impact
-
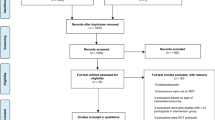
This review examines the effects of various forms of sensory stimulation on apnoea mitigation in preterm infants, namely localized tactile, generalized kinesthetic, airway pressure, auditory, and olfactory stimulations.
-
Amongst the 31 studies reviewed, each form of sensory stimulation showed some positive effects, although the findings were not definitive and comparative studies were lacking.
-
We find that the development of automated closed-loop sensory stimulation systems for apnoea mitigation is warranted, including the possibility of stimulation being applied preventatively, and in a multi-modal form.
Similar content being viewed by others
Introduction
Apnoea reflects the immaturity of respiratory control in preterm infants and is observed in essentially all preterm infants born at <30 weeks gestation.1 Apnoeic events occur most prominently at 2–4 weeks of life, a time when infants are usually requiring non-invasive respiratory support.1 Apnoeic events often lead to physiological instability including hypoxia and/or bradycardia, which has been associated with adverse neurodevelopmental outcomes.2
Current approaches to reduce apnoea burden in preterm infants include caffeine administration and the use of non-invasive respiratory support.3,4 Despite such preventative clinical management, apnoeic events continue to be observed during a preterm infant’s admission in the neonatal intensive care unit (NICU). Bedside staff caring for preterm infants are often required to intervene urgently in response to detected apnoeic events by providing additional interventions such as tactile stimulation, airway optimization and positive pressure ventilation, with the goal of re-establishing the infant’s respiratory efforts. Such a reactive management system creates a response delay and is laborious for bedside staff, makes apnoea-associated physiological instability inevitable, and heightens the risk of longer-term consequences.
Beyond current measures used in clinical practice, previous studies have investigated several forms of sensory stimulation for apnoea prevention and mitigation in preterm infants. Sensory stimuli explored include localized tactile, generalized kinesthetic, olfactory and auditory, as well as non-invasive intermittent positive pressure ventilation (NIPPV). These forms of stimulation have been delivered either in an automated closed-looped system or manually by nurses, and either preventatively or reactively (upon detection of an apnoeic event). Furthering our understanding of sensory stimulation for apnoea mitigation can contribute to improving the respiratory care of preterm infants. This paper explores the potential for sensory stimuli to mitigate apnoeic events in preterm infants, reviewing previous studies and their inherent limitations, identifying gaps in knowledge and important considerations that may help to optimize this mode of therapy. For the purpose of this review, we have excluded treatments considered part of standard management for preterm infants with respiratory insufficiency (caffeine therapy and nasal continuous positive airway pressure (nCPAP)). We have also excluded methods such as carbon dioxide insufflation and pharyngeal catheters that would be unlikely to have widespread practical applications.
Sensory stimuli for apnoea of prematurity
Localized tactile stimulation
Nurses commonly apply localized cutaneous (by touching the infant’s skin) and/or proprioceptive (by moving a major joint) stimulation to preterm infants in a site-targeted fashion, after being alerted to an apnoeic event.5 These localized tactile stimuli may produce their effect via cortical arousal and the reflexive coupling of cutaneous and/or proprioceptive stimulation to ventilation, whereby somatosensory stimulation has been demonstrated to influence respiratory rate and pattern in patients.6,7,8,9,10
Preventative application of tactile stimulation
Various forms of tactile stimulus have been previously applied in a continuous fashion in preterm infants, investigating their effect on apnoea frequency. Four studies reported a decrease in apnoea frequency when tactile stimulation was applied, despite these studies having applied the tactile stimulation for a different duration, regularity and intensity to different sites (Table 1).11,12,13,14 Jirapaet further found preventative tactile stimulation to be more effective in reducing central and mixed apnoeic events than obstructive apnoeic events.12
Reactive application of tactile stimulation
A tactile stimulus can alternatively be applied in a reactive manner, whereby the stimulus is delivered only upon the detection of an apnoeic event, analogous to current NICU nursing management (Table 1).15,16,17,18 While systems used by Pichardo et al.16 and Lovell et al.18 required bedside staff to identify the need for the stimulus to be delivered, others have used an automated closed-looped delivery system whereby tactile stimuli was delivered upon apnoea detection without requiring staff input.15,17 Even though methods of detecting apnoeic events differed, with Frank et al. and Pichardo et al. using thoracic impedance monitoring and Camargo et al. having used a custom-built system for apnoea detection, the tactile stimuli applied to preterm infants in these studies were of similar duration and intensity.15,16,17,18 Reactive tactile stimulation of this form has been found—with varying success rates—to lead to re-establishment of respiratory efforts to a varying degree and performed comparably to manual nursing intervention (Table 1).15,16,17,18
While these results of preventative and reactive localized tactile stimulation show some promise, it is important to consider the effects of confounders associated with using tactile stimulus, for example, the coexistence of an auditory stimulus. Sound, often a soft hum, is generated if a vibrating mechanism is used and can be perceived by the infant via air or bone conduction. In the absence of sound monitoring during the interventional periods, the reported effectiveness in reducing or terminating apnoeic events may not be solely attributable to the tactile stimulus.
Tactile stimulation has been applied to different anatomical sites in previous studies, in large part without a clear rationale for the choice of one site over another (Table 1). Further understanding of the most effective site for the application of a tactile stimulus to maintain and/or re-establish respiratory effort in preterm infants will be important in guiding device design for clinical implementation.
Generalized kinesthetic stimulation
Generalized kinesthetic stimulation delivered using different forms of vibratory mattresses aims to mimic the constant movements experienced by a foetus in utero. Such generalized stimuli are thought to produce subcortical arousal via somatosensory afferents, leading to augmentation of breathing and diminution of inhibitory reflexes.19,20,21,22 In addition, preterm infants on oscillating mattresses have been found to experience shorter periods of rapid eye movement (REM) sleep phase during which apnoeic events are usually more prevalent.23,24
Previous studies of kinesthetic stimulation applied preventatively in preterm infants have for the most part reported modest reductions in apnoeic event frequency (Table 2).19,22,24,25,26,27,28,29,30,31 Notwithstanding the small sample sizes and application of stimuli of varying intensity, displacement and duration, previous studies do appear to demonstrate the potential for kinesthetic stimulation to reduce apnoea frequency in preterm infants (Table 2).19,22,24,25,26,27,28,29,30,31 Meaningful comparisons between studies are limited by the different definitions for apnoeic events used in each study (Table 2).19,22,24,25,26,27,28,29,30
It will be important to more fully explore the possible side effects of prolonged and/or repeated kinesthetic stimulation, such as restlessness and increased blood pressure.24,25,29 The optimal characteristics of the kinesthetic stimulus also require investigation in future comparative studies.
Airway stimulation via application of intermittent positive pressure ventilation
nCPAP delivered via nasal mask or prongs is a common form of non-invasive respiratory support used for preterm infants admitted to the NICU with respiratory insufficiency. Amongst other effects, the applied positive airway pressure stents the upper airway reducing upper airway resistance, as well as providing a stimulus.3
An alternative form of non-invasive support, NIPPV, is used to a variable extent in NICUs worldwide. During NIPPV, brief positive pressure inflations are superimposed on the background of nCPAP, at a pre-determined rate and/or when triggered by the infant’s inspiratory efforts.32 This results in phasic distension of the nasopharynx, which has been proposed to restore respiratory cadence by activating the pharyngeal dilator muscles, as well as by stimulation of the Head’s paradoxical reflex where rapid lung inflation triggers a deep inspiration.33,34,35
Previous studies comparing the effects of NIPPV with nCPAP alone in preterm infants have found periods of NIPPV to be associated with a lower frequency of apnoeic events (Table 3).32,36,37,38 Gizzi et al. further reported that synchronized NIPPV, whereby the superimposed positive pressure inflations were delivered in synchrony with inspiratory efforts, significantly reduced the frequency of apnoeic events when compared to unsynchronized NIPPV.36
While previous evidence supports the use of NIPPV to reduce apnoea burden in preterm infants, it is important to note the relatively short duration of the study epochs in these reports, ranging from 4 to 6 h (Table 3).32,36,37,38 The effectiveness of prolonged NIPPV in apnoea mitigation remains to be determined. In addition, there is a limited description in the studies regarding the differentiation of actual infant-initiated respiratory activity from recorded respiratory excursions induced by positive pressure ventilation, with the latter potentially masking central apnoea. Further investigations with a larger sample size and longer study duration are needed to examine if the effects of NIPPV in reducing apnoea frequency can be maintained over time.
Extending the concept of NIPPV as a nasopharyngeal stimulus, further considerations should be given to the reactive application of positive pressure inflations, where additional positive pressure inflation is only delivered when impending apnoea is predicted,39 or in the early stages of a detected pause in respiration. Such an approach may help to maintain or restore respiratory cadence via reflex mechanisms, mitigating adverse apnoea-associated physiological consequences while minimizing the risks associated with the unremitting application of NIPPV in preterm infants.40
Auditory stimulation
Preterm infants demonstrate neurological responses to auditory stimuli, with an inherent tendency to entrain their physiological rhythms to the tempo of the stimulus.41,42 The effects of auditory stimulation on immature autonomic functions, including apnoea frequency, in preterm infants have been studied using various targeted sounds, such as lullabies, the mother’s voice and live music (Table 4).43,44,45,46,47
Infants were found to have a lower rate of apnoeic events when exposed to targeted auditory stimuli, although the differences between intervention and control epochs were non-significant in three of the studies.43,44,45,46,47 Duration and volume of the auditory stimuli used varied considerably between studies (Table 4).43,44,45,46,47 The low frequency of apnoeic events is likely a contributory factor to the findings, related to the inclusion of infants still weaning from mechanical ventilation43, or conversely relatively mature infants no longer requiring any respiratory support.45,46
Given the previously mixed methodology and sample populations, further studies are required to more fully explore and understand the potential for targeted auditory stimuli to reduce apnoea burden in preterm infants requiring non-invasive respiratory support. Future studies will need to explore the effectiveness of different types, volume and duration of sounds used, as well as the timing of stimulus delivery (i.e. preventative vs. reactive application).
Olfactory stimulation
Exposure to odorants has been demonstrated to modulate respiratory rate in both term and preterm infants, particularly during REM sleep.23,48,49 Odours perceived to be pleasant by adults, such as vanillin (a pure olfactory stimulus) and lavender (a trigeminal stimulus), have led to an increase in respiratory efforts.49,50 On the other hand, odours perceived as unpleasant to adults, including ammonium sulfide (a pure olfactory stimulus) and vetiver (a trigeminal stimulus), have led to a diminution of respiratory activity.49,50 Regardless of the substance used, exposure to odorants has been associated with an initial transient decrease in tidal volume.49,50 Term infants exposed to vanillin have also demonstrated an increase in orbito-frontal blood flow and oxyhaemoglobin levels, although the mechanism of action of vanillin in producing these responses is still unclear.51,52
The use of olfactory stimulation to quell apnoeic events in preterm infants was initially reported by Marlier et al. in 2005, who demonstrated a reduction in apnoea frequency when infants were exposed to vanillin.53 Subsequent studies exposing preterm infants to different concentrations of vanillin and/or other odours have replicated these findings in infants with persistent apnoeic events (Table 5). Furthermore, Kanbur and Balci reported a sustained decrease in apnoea frequency for the initial 24 h after infants were no longer exposed to vanillin.54
With the promising findings that an olfactory stimulus may be a feasible means of reducing apnoea frequency, it is important to acknowledge that these studies were in large part conducted in infants of more advanced postnatal age who were breathing spontaneously.53,54,55,56,57 The frequency and severity of apnoeic events in such infants may well differ from more immature infants receiving non-invasive respiratory support.1 Additional studies in this latter group are needed and will entail the development of a method for olfactory stimulus delivery to preterm infants receiving non-invasive respiratory support in a reactive manner.
Further considerations
As outlined above, various sensory stimuli have been found to have some effect in decreasing apnoea frequency in preterm infants, but the current evidence is far from compelling. Beyond the small sample sizes and a lack of intervention blinding (with exception to studies of olfactory stimuli), several previous studies also relied on apnoea reporting by bedside staff, a limitation that can be addressed with the availability of real-time physiological data collection. In the following section, we consider factors that may limit the effectiveness of stimulation (e.g. habituation, reactive stimulus delivery), and propose some potential improvements to this form of therapy.
Habituation
Habituation is the observed diminution or extinction of a response following repeated exposure of an individual to a selected stimulus over several short periods, or a single long period.58,59 Preterm infants are continuously exposed to an array of stimuli throughout their stay in the NICU, and would, over time, be expected to habituate to repetitive inconsequential stimuli.58,59 While habituation may be beneficial to avoid sleep deprivation, this process can also diminish the response to stimulation applied with protective intent.59 Preterm infants have also been shown to habituate more readily to sound than to visual or tactile stimuli.58
As has been described above, the various forms of stimuli investigated for their effect on apnoea in preterm infants, for the most part, have been applied in a continuous fashion, regardless of the infant’s respiratory state. Furthermore, most of these studies with preventative application of a stimulus have been of relatively short duration, and none of the studies have investigated whether preterm infants habituated to the applied stimulus evidenced by a diminution in its effectiveness in reducing apnoea frequency over time.58 While Bloch-Salisbury et al. found apnoea frequency to be halved when generalized kinesthetic stimulation only lasted for 10 min at a time, Smith et al., using the same method of stimulus, found little differences in apnoea frequency between intervention and control periods when stimulation lasted longer.22,31 The extrapolation of previous study findings to the situation of continuous prolonged use of a monotonic and unimodal stimulus is thus fraught, and consideration of alternating types and duration of sensory stimuli to avoid habituation will be essential. Future studies should use longer investigative epochs and apply analytical methods that allow any effects of habituation to be identified.
Reactive delivery of stimuli for apnoea mitigation
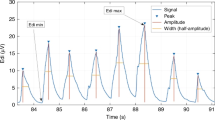
Currently, the only reactive stimuli delivered to mitigate apnoeic events are provided by nursing staff. With technological advances, the development of automated closed-looped stimulus delivery systems to react to apnoeic events in preterm infants is within reach. Given that longer-lasting apnoeic events are more challenging to terminate, such systems could be programmed to intervene early, soon after the onset of a respiratory pause. Development of these devices will require the coupling of stimulus delivery to the reliable respiratory monitoring device(s).
Reactive delivery of a stimulus (i.e. delivering stimulus only upon detection of apnoea) to apnoeic events has thus far been limited to the application of tactile stimulation, and the relevant studies have been for short durations.15,16,17,18 The lack of a device capable of reactive stimulus delivery is in large part related to technological limitations preventing other forms of stimulus to be coupled with a respiratory monitor, particularly in the setting of non-invasive respiratory support where flow sensing of respiratory activity is unreliable. Further studies and technological developments aimed at enabling different types of stimuli to be delivered in an automated reactive fashion for preterm infants will allow more generalizable findings and be more acceptable for translation of research to clinical implementation.
Stimulus delivery coupled with prediction of impending apnoeic events
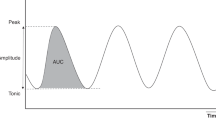
Whilst delivery of a stimulus soon after the onset of a respiratory pause may curtail the downstream hypoxic or bradycardic consequences, ideally, stimulation could begin when an impending apnoeic event is predicted, with the aim of maintaining, rather than restoring, respiratory cadence. Systems to predict apnoea in preterm infants are starting to be developed39,60 and have the potential to be linked in feedback loops to devices applying stimulation of various forms.
An automated closed-looped multi-stimuli delivery system coupled with a reliable respiratory monitor and a predictive system of apnoeic events in preterm infants would be ideal to allow for the stimuli delivery to commence just prior to, or close to the onset of, a respiratory pause and be maintained for only the required duration to maintain respiratory cadence. In this way, continuous stimulation and its associated risks may be avoided, whilst at the same time intervening at an ideal time before respiration has actually ceased.
Stimulus selection based on apnoea sub-types
Apnoeic events are classified into three main sub-types: central apnoea where there is a lack of central respiratory drive; obstructive apnoea where airflow is impeded by mechanical upper airway obstruction, often with glottic closure; and mixed apnoea, which involves a combination of both central and obstructive components in a single event. With physiological differences between the apnoea sub-types, it is natural to consider the possibility that some forms of stimulation may be more effective than others in mitigating a particular sub-type of apnoea. This difference had been previously reported by Jirapaet, where when compared to standard care, vibrotactile stimulation was able to reduce central and mixed apnoeic events more significantly in preterm infants than obstructive apnoeic events.12
Future studies investigating the effects of potential stimuli on different apnoea sub-types will guide a more effective selection of stimulus, or combination of stimuli, to decrease apnoea burden in preterm infants.
Multi-modal stimulation
The effectiveness of each type of stimulus in apnoea mitigation has until now almost exclusively been examined in isolation, comparing a single form of stimulation with standard care. Given the observed capacity for habituation in preterm infants, consideration and further investigation of multi-modal stimulation are warranted.58 Such stimuli could be used in combination (i.e. multiple stimuli used simultaneously), or in rotation, where only one stimulus is provided at a time in a pseudo-randomised order.
Garcia and White-Traut have preliminarily examined the effect of multi-modal stimulation, comparing a combination of tactile, gustatory and olfactory stimulation with an isolated tactile stimulus in otherwise well preterm infants who were not requiring any respiratory support.61 The multi-modal stimulus was a lemon-glycerine swab stick applied to the infant’s lip and tongue, while the unimodal tactile stimulus was a brief shaking of the infant’s leg by a researcher.61 The study found that infants re-established respiratory cadence sooner when exposed to multi-modal stimulation rather than an isolated tactile stimulus (multi-modal stimulation: 5.99 ± 0.49 s; isolated tactile stimulation: 6.59 ± 0.47 s, p value = 0.01). However, the observed mean difference was only in the order of 0.6 s.61
An important limitation of the study by Garcia and White-Traut is that the effect of the various components of the multi-modal stimulus was not examined in isolation.61 Nonetheless, the results do support the concept of multi-modal stimulation and encourage further studies of this approach for re-establishing respiratory efforts in preterm infants with apnoea, especially those receiving non-invasive respiratory support.
Conclusion
Various sensory stimuli have been previously found to be variably effective in mitigating apnoea in preterm infants, although further compelling evidence is still needed. Current limitations include our rudimentary understanding of habituation, and a lack of devices to deliver sensory stimuli in an automated closed-looped system and in a multi-modal form for preterm infants receiving non-invasive respiratory support. However, these limitations are undoubtedly surmountable with ongoing research.
Expanding our current repertoire of management tools for apnoeic events in preterm infants through the application of alternative sensory stimulation may help avoid apnoea-associated physiological instability, whilst at the same time reducing nursing workload.
References
Fairchild, K. et al. Clinical associations of immature breathing in preterm infants: part 1-central apnea. Pediatr. Res. 80, 21–27 (2016).
Di Fiore, J. et al. Cardiorespiratory events in preterm infants: interventions and consequences. J. Perinatol. 36, 251 (2016).
Miller, M. J., Carlo, W. A. & Martin, R. J. Continuous positive airway pressure selectively reduces obstructive apnea in preterm infants. J. Pediatr. 106, 91–94 (1985).
Schmidt, B. et al. Caffeine therapy for apnea of prematurity. N. Engl. J. Med. 354, 2112–2121 (2006).
Hagan, R., Bryan, A., Bryan, M. & Gulston, G. Neonatal chest wall afferents and regulation of respiration. J. Appl. Physiol. 42, 362–367 (1977).
Iscoe, S. & Polosa, C. Synchronization of respiratory frequency by somatic afferent stimulation. J. Appl. Physiol. 40, 138–148 (1976).
Ishida, K., Yasuda, Y. & Miyamura, M. Cardiorespiratory response at the onset of passive leg movements during sleep in humans. Eur. J. Appl. Physiol. Occup. Physiol. 66, 507–513 (1993).
Iwamoto, E. et al. The neural influence on the occurrence of locomotor–respiratory coordination. Respir. Physiol. Neurobiol. 173, 23–28 (2010).
Potts, J. T., Rybak, I. A. & Paton, J. F. Respiratory rhythm entrainment by somatic afferent stimulation. J. Neurosci. 25, 1965–1978 (2005).
Lijowska, A. S., Reed, N. W., Chiodini, B. A. M. & Thach, B. T. Sequential arousal and airway-defensive behavior of infants in asphyxial sleep environments. J. Appl. Physiol. 83, 219–228 (1997).
Dong, L.-B., Li, Y.-F., Zhang, Y. & Qiao, S. A pilot study of limb stimulation for the treatment of neonatal apnea. Medicine 97, e12827 (2018).
Jirapaet, K. The effect of vertical pulsating stimulation on apnea of prematurity. J. Med. Assoc. 76, 319–326 (1993).
Kattwinkel, J. et al. Apnea of prematurity. Comparative therapeutic effects of cutaneous stimulation and nasal continuous positive airway pressure. J. Pediatr. 86, 588–592 (1975).
Kesavan, K. et al. Neuromodulation of limb proprioceptive afferents decreases apnea of prematurity and accompanying intermittent hypoxia and bradycardia. PLoS ONE 11, e0157349 (2016).
Camargo, V. C., Honorato da Silva, S., Freitas de Amorim, M. & Nohama, P. Instrumentation for the detection and interruption of apnea episodes for premature newborn. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2014, 2127–2130 (2014).
Pichardo, R. et al. Vibrotactile stimulation system to treat apnea of prematurity. Biomed. Instrum. Technol. 37, 34–40 (2003).
Frank, U. A. et al. Treatment of apnea in neonates with an automated monitor-actuated apnea arrestor. Pediatrics 51, 878–883 (1973).
Lovell, J. et al. Vibrotactile stimulation for treatment of neonatal apnea: a preliminary study. Conn. Med. 63, 323–325 (1999).
Osborn, D. A. & Henderson-Smart, D. J. Kinesthetic stimulation for treating apnea in preterm infants. Cochrane Database Syst. Rev. 1999, CD000499 (2000).
Osborn, D. A. & Henderson‐Smart, D. J. Kinesthetic stimulation for preventing apnea in preterm infants. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD000373, CD000373 (2002).
Mortola, J. P. Respiratory Physiology of Newborn Mammals: A Comparative Perspective (JHU Press, 2001).
Bloch-Salisbury, E., Indic, P., Bednarek, F. & Paydarfar, D. Stabilizing immature breathing patterns of preterm infants using stochastic mechanosensory stimulation. J. Appl. Physiol. 107, 1017–1027 (2009).
Lehtonen, L. & Martin, R. J. Ontogeny of sleep and awake states in relation to breathing in preterm infants. Semin. Neonatol. 9, 229–238 (2004).
Svenningsen, N., Wittström, C. & Hellström-Westas, L. OSCILLO-oscillating air mattress in neonatal care of very preterm babies. Technol. Health Care 3, 43–46 (1995).
Jones, R. A. A controlled trial of a regularly cycled oscillating waterbed and a non-oscillating waterbed in the prevention of apnoea in the preterm infant. Arch. Dis. Child 56, 889–891 (1981).
Korner, A. F., Guilleminault, C., Van den Hoed, J. & Baldwin, R. B. Reduction of sleep apnea and bradycardia in preterm infants on oscillating water beds: a controlled polygraphic study. Pediatrics 61, 528–533 (1978).
Korner, A. F., Kraemer, H. C., Haffner, M. E. & Cosper, L. M. Effects of waterbed flotation on premature infants: a pilot study. Pediatrics 56, 361–367 (1975).
Korner, A. F., Ruppel, E. M. & Rho, J. M. Effects of water beds on the sleep and motility of theophylline-treated preterm infants. Pediatrics 70, 864–869 (1982).
Saigal, S., Watts, J. & Campbell, D. Randomized clinical trial of an oscillating air mattress in preterm infants: effect on apnea, growth, and development. J. Pediatr. 109, 857–864 (1986).
Tuck, S. et al. Effect of a rocking bed on apnoea of prematurity. Arch. Dis. Child 57, 475–477 (1982).
Smith, V. C. et al. Stochastic resonance effects on apnea, bradycardia, and oxygenation: a randomized controlled trial. Pediatrics 136, e1561–e1568 (2015).
Ryan, C. A., Finer, N. N. & Peters, K. L. Nasal intermittent positive-pressure ventilation offers no advantages over nasal continuous positive airway pressure in apnea of prematurity. Am. J. Dis. Child. 143, 1196–1198 (1989).
Moretti, C. et al. Synchronized nasal intermittent positive pressure ventilation of the newborn: technical issues and clinical results. Neonatology 109, 359–365 (2016).
Abu-Osba, Y. K., Brouillette, R. T., Wilson, S. L. & Thach, B. T. Breathing pattern and transcutaneous oxygen tension during motor activity in preterm infants. Am. Rev. Respir. Dis. 125, 382–387 (1982).
Widdicombe, J. Henry Head and his paradoxical reflex. J. Physiol. 559(Part 1), 1 (2004).
Gizzi, C. et al. Is synchronised NIPPV more effective than NIPPV and NCPAP in treating apnoea of prematurity (AOP)? A randomised cross-over trial. Arch. Dis. Child Fetal Neonatal Ed. 100, F17–F23 (2015).
Lin, C. H., Wang, S. T., Lin, Y. J. & Yeh, T. F. Efficacy of nasal intermittent positive pressure ventilation in treating apnea of prematurity. Pediatr. Pulmonol. 26, 349–353 (1998).
Pantalitschka, T. et al. Randomised crossover trial of four nasal respiratory support systems for apnoea of prematurity in very low birthweight infants. Arch. Dis. Child Fetal Neonatal Ed. 94, F245–F248 (2009).
Lim, K. et al. Predicting apnoeic events in preterm infants. Front. Pediatr. 8, 570 (2020).
Dargaville, P. A. et al. An authentic animal model of the very preterm infant on nasal continuous positive airway pressure. Intens. Care Med. Exp. 3, 51 (2015).
Uchida, M. O. et al. Effect of mother’s voice on neonatal respiratory activity and EEG delta amplitude. Dev. Psychobiol. 60, 140–149 (2018).
Ingersoll, E. W. & Thoman, E. B. The breathing bear: effects on respiration in premature infants. Physiol. Behav. 56, 855–859 (1994).
Cassidy, J. W. & Standley, J. M. The effect of music listening on physiological responses of premature infants in the NICU. J. Music Ther. 32, 208–227 (1995).
Schwilling, D. et al. Live music reduces stress levels in very low‐birthweight infants. Acta Paediatr. 104, 360–367 (2015).
Shellhaas, R. A. et al. Maternal voice and infant sleep in the neonatal intensive care unit. Pediatrics 144, e20190288 (2019).
Parga, J. J. et al. A prospective observational cohort study of exposure to womb-like sounds to stabilize breathing and cardiovascular patterns in preterm neonates. J. Matern. Fetal Neonatal Med. 31, 2245–2251 (2018).
Doheny, L. et al. Exposure to biological maternal sounds improves cardiorespiratory regulation in extremely preterm infants. J. Matern. Fetal Neonatal Med. 25, 1591–1594 (2012).
Marlier, L. et al. Premature newborns differentiate the affective value of odours during sleep. J. Matern. Fetal Neonatal Med. 11(Suppl. 1), 64 (2002).
Marlier, L., Schaal, B., Gaugler, C. & Messer, J. Olfaction in premature human newborns: detection and discrimination abilities two months before gestational term. Chem. Signals Vertebrates 9, 205–209 (2001).
Arzi, A. et al. The influence of odorants on respiratory patterns in sleep. Chem. Senses 35, 31–40 (2010).
Bartocci, M. et al. Activation of olfactory cortex in newborn infants after odor stimulation: a functional near-infrared spectroscopy study. Pediatr. Res. 48, 18–23 (2000).
Aoyama, S. et al. Maternal breast milk odour induces frontal lobe activation in neonates: a NIRS study. Early Hum. Dev. 86, 541–545 (2010).
Marlier, L., Gaugler, C. & Messer, J. Olfactory stimulation prevents apnea in premature newborns. Pediatrics 115, 83–88 (2005).
Kanbur, B. N. & Balci, S. Impact of the odors of vanilla extract and breast milk on the frequency of apnea in preterm neonates. Jpn. J. Nurs. Sci. 17, e12271 (2020).
Edraki, M. et al. Olfactory stimulation by vanillin prevents apnea in premature newborn infants. Iran. J. Pediatr. 23, 261 (2013).
Aghagoli, S. et al. Aromatherapy with rosa damascenes in apnea, bradycardia and Spo2 of preterm infants; a randomized clinical trial. Int. J. Pediatr. 4, 1911–1918 (2016).
Yaghoubi, S., Salmani, N., Dehghani, K. & DavoodiZadehJolgeh, H. Investigating effect of olfactory stimulation by vanilla on the rate of apnea attacks in neonates with apnea of prematurity: a randomized clinical trial. Int. J. Pediatr. 5, 6221–6229 (2017).
Castillo, M. U., de Moraes Barros, M. C. & Guinsburg, R. Habituation responses to external stimuli: is the habituation of preterm infants at a postconceptual age of 40 weeks equal to that of term infants? Arch. Dis. Child 99, F402–F407 (2014).
McNamara, F., Wulbrand, H. & Thach, B. T. Habituation of the infant arousal response. Sleep 22, 320–326 (1999).
Williamson, J. R., Bliss, D. W. & Paydarfar, D. Forecasting respiratory collapse: theory and practice for averting life-threatening infant apneas. Respir. Physiol. Neurobiol. 189, 223–231 (2013).
Garcia, A. P. & White-Traut, R. Preterm infants’ responses to taste/smell and tactile stimulation during an apneic episode. J. Pediatr. Nurs. 8, 245–252 (1993).
Funding
This work was supported by an Australian NHMRC Post-Graduate Scholarship to Dr. Kathleen Lim (#1190694), and an NHMRC Ideas Grant (#118251).
Author information
Authors and Affiliations
Contributions
K.L. conceived and conducted the review (with P.A.D), wrote the first draft of the manuscript and approved the final draft. S.J.E.C., A.B.t.P. and T.J.G provided intellectual input to the review, edited the manuscript and approved the final draft. P.A.D conceived and conducted the review (with K.L.), edited the manuscript and approved the final draft.
Corresponding author
Ethics declarations
Competing interests
All authors declare that this review was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lim, K., Cramer, S.J.E., te Pas, A.B. et al. Sensory stimulation for apnoea mitigation in preterm infants. Pediatr Res 92, 637–646 (2022). https://doi.org/10.1038/s41390-021-01828-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01828-5