Abstract
Background
Social determinants of health (SDH) can substantially impact health outcomes. A systematic review, however, has never been conducted on associations of SDH with congenital heart disease (CHD) outcomes. The aim, therefore, was to conduct such a systematic review.
Methods
Seven databases were searched through May 2020 to identify articles on SDH associations with CHD. SDH examined included poverty, uninsurance, housing instability, parental educational attainment, immigration status, food insecurity, and transportation barriers. Studies were independently selected and coded by two researchers based on the PICO statement.
Results
The search generated 3992 citations; 88 were included in the final database. SDH were significantly associated with a lower likelihood of fetal CHD diagnosis, higher CHD incidence and prevalence, increased infant mortality, adverse post-surgical outcomes (including hospital readmission and death), decreased healthcare access (including missed appointments, no shows, and loss to follow-up), impaired neurodevelopmental outcomes (including IQ and school performance) and quality of life, and adverse outcomes for adults with CHD (including endocarditis, hospitalization, and death).
Conclusions
SDH are associated with a wide range of adverse outcomes for fetuses, children, and adults with CHD. SDH screening and referral to appropriate services has the potential to improve outcomes for CHD patients across the lifespan.
Impact
-
Social determinants of health (SDH) are associated with a wide range of adverse outcomes for fetuses, children, and adults with congenital heart disease (CHD).
-
This is the first systematic review (to our knowledge) on associations of SDH with congenital heart disease CHD outcomes.
-
SDH screening and referral to appropriate services has the potential to improve outcomes for CHD patients across the lifespan.
Similar content being viewed by others
Background
Innovation and technical advancement have revolutionized the field of pediatric and adult congenital heart disease (CHD) over the past century. As clinical outcomes have improved dramatically over time, however, healthcare disparities have persisted for the most vulnerable populations. Structural cardiac defects are the most common birth defect, affecting approximately 0.8–1% of the population.1,2,3 These birth defects range in complexity and occur across all the socioeconomic groups. With CHD mortality in infancy and childhood decreasing substantially with the evolution of advanced surgical and catheter-based interventions, >90% of children with CHD now survive into adulthood, and this large population of adults with CHD continues to grow with time.4 As a result, there are now more adults than children living with CHD in the US. Although survival has improved, CHD patients continue to face major socioeconomic and demographic disparities in outcomes at all ages.3
Social determinants of health (SDH) are conditions in which people live and grow up within the wider context of systems and influences shaping daily life.5 SDH include poverty, lack of insurance, housing instability, parental educational attainment, immigration status, food insecurity, and transportation barriers. These factors contribute to poor clinical outcomes, healthcare inequities, and escalating healthcare costs. The central importance of the association of SDH with health outcomes specifically in the context of cardiovascular diseases was underscored by the American Heart Association and American College of Cardiology in their 2019 guidelines for clinical risk assessment.6 There are no published systematic reviews, however, of the associations of SDH with major CHD outcomes across the lifespan, including fetal diagnosis; incidence and prevalence; infant mortality; post-surgical outcomes; access to care, loss to follow-up, and hospital readmissions; neurodevelopmental outcomes and quality of life (QOL); and adult CHD. The study aim, therefore, was to conduct a systematic review of the association of SDH with CHD outcomes.
Methods
SDH: definitions
The following SDH were included in this analysis: poverty, uninsurance, housing instability, parental educational attainment, immigration status, food insecurity, and transportation barriers. These were chosen because they are the domains addressed in a recently published SDH screening instrument used for interventions effective in reducing social risks and improving child and caregiver health.7 For articles in which there was no assessment of socioeconomic status (SES), Medicaid coverage was used as a proxy for low income.
Outcomes
The following CHD outcome categories across the lifespan were evaluated: fetal diagnosis; incidence and prevalence; infant mortality; post-surgical outcomes; access to care, loss to follow-up, and hospital readmissions; neurodevelopmental outcomes and QOL; and adult CHD.
Inclusion and exclusion criteria
Inclusion criteria consisted of published, original research on the associations of SDH with CHD. Exclusion criteria included: (1) letters to the editor, commentaries, editorials, viewpoints, perspectives, opinion pieces, case reports, book chapters, author or keyword indexes, and review articles; (2) publications that did not address clinical outcomes in patients with CHD; (3) articles focusing on acquired pediatric cardiac diseases, variants of normal, patent foramen ovale, primary arrhythmias, cardiovascular complications of connective tissue disorders, and pulmonary hypertension in the absence of structural CHD; (4) studies that classified SDH as race/ethnicity, maternal stress, environmental exposures, or vitamin or drug/alcohol exposures; (5) animal-only studies; (6) analyses of the association of CHD (as an independent variable) with SDH (as the dependent variable); and (7) articles on populations outside of the US or Canada (because the focus was on SDH in developed countries in North America with comparable healthcare systems).
Literature search
Using sentinel articles to harvest and test search terms, the following search strategy was developed for PubMed/MEDLINE to retrieve all records using natural language and controlled vocabulary (when available) relating to the association of SDH with CHD (Table 1). This strategy then was translated and adapted for the other databases. The following databases were searched from date of inception through May 18, 2020: PubMed MEDLINE (including Pre-MEDLINE and non-MEDLINE; 1945 to May 2020), Scopus (Elsevier; 1966 to May 2020), Cochrane Central Register of Controlled Trials (Wiley; through May 2020), CINAHL (Ebsco; 1981 to May 2020), PsycInfo (Ebsco; 1872 to May 2020), Social Interventions Research & Evaluation Network (SIREN) Evidence & Resource Library (University of California, San Francisco; through May 2020), and SocIndex (Ebsco; 1895 to May 2020). No filters were used for language or publication date. ProQuest RefWorks (Legacy version) was used to de-duplicate and manage all citations.
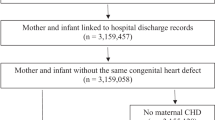
Once articles were identified and compiled by the search criteria described above and duplicates removed, vetting was performed by title and abstract by two authors using strict inclusion and exclusion criteria (Fig. 1). For studies for which there was lack of clarity regarding whether or not inclusion criteria were met, final decisions were made by reaching consensus among at least three authors. Once title and abstract vetting was completed, a full-text review was performed using the inclusion and exclusion criteria to determine final inclusion in the systematic review. Consensus opinion with regards to inclusion of studies was again reached when questions arose.
PROSPERO registration
This systematic review was registered in PROSPERO (CRD42020169253).
Results
The initial search generated 3992 citations. A total of 88 studies met inclusion criteria (Fig. 1 and Table 2). Study designs were variable and included retrospective chart reviews, retrospective and prospective cohort studies, cross-sectional studies, and prospective case–control studies. No studies were identified that examine housing instability.
The sections that follow report the findings on SDH associations with seven major CHD outcomes across the lifespan: fetal diagnosis; incidence and prevalence; infant mortality; post-surgical outcomes; access to care, loss to follow-up, and hospital readmissions; neurodevelopmental outcomes and QOL; and adult CHD.
Fetal diagnosis of CHD
Four articles were identified that examined SDH associations with the fetal diagnosis of CHD (Table 2).8,9,10,11 Three studies documented that poverty or low SES is associated with a significantly lower likelihood of a prenatal CHD diagnosis; one study also found that low maternal educational attainment and public insurance were SDH risk factors for no prenatal CHD diagnosis. An analysis of 444 patients presenting to Boston Children’s Hospital with critical CHD (defined as surgical or catheter intervention required in infants ≤30 days old) revealed that only 35% of those in the lowest SES composite-score quartile received a prenatal CHD diagnosis, vs. 62% of those in the highest SES quartile. A retrospective study of >2.5 million infants born in California revealed that the lowest income tertile, public insurance, and low maternal educational attainment were associated with a significantly higher likelihood of CHD. In a study of 535 patients presenting to Children’s Hospital of Wisconsin with CHD, residing in a higher poverty zip code was associated with a significantly lower odds of a prenatal CHD diagnosis. One study of 100 Cincinnati infants with CHD found no association of family income, parental educational attainment, or insurance coverage with prenatal CHD diagnosis, although the sample size (100) was limited and multivariable analyses were not performed.
CHD incidence and prevalence
Fifteen articles examined the association of SDH with CHD incidence and prevalence (Table 2).12,13,14,15,16,17,18,19,20,21,22,23,24,25,26 Poverty generally was found to be significantly associated with CHD incidence and prevalence, but such associations were either equivocal or lacking for other SDH examined, including food insecurity, immigration, and parental educational attainment.
Eleven articles analyzed an association between low SES and an increased CHD incidence or prevalence, and most found that SES was significantly associated with CHD incidence or prevalence. SES definitions, however, varied among the studies, with low SES defined as individual poverty, low family income, neighborhood poverty, maternal educational attainment, parental employment, operator/laborer occupation, crowding, rental occupancy, or some combination thereof.12,13,14,15,17,18,19,20,21,25,26 A study of 1.9 million children born in Ontario, Canada, revealed that birth in low SES areas was associated with significantly higher CHD rates (rate ratio = 1.20; 95% confidence interval [CI] = 1.15–1.24).12 A population-based study of 2.4 million live-born infants in California documented that those residing in neighborhoods with the lowest SES composite score had a significantly higher CHD incidence vs. those from the highest SES neighborhoods (adjusted odds ratio (OR) = 1.31; 95% CI, 1.21–1.41).25 Low SES also was found to be associated with a significantly higher CHD incidence risk in studies using cardiology clinic registries13 and national databases.17
Two articles used the Nationwide Inpatient Sample (NIS) to examine secular trends in CHD prevalence, but reached different conclusions. One study demonstrated that those in the upper income quartile experienced a significantly greater temporal decrease in the prevalence of severe CHD vs. those in the lowest income quartile,19 whereas another found that mild CHD prevalence significantly increased only in the high SES group.20 Another population-based study using the NIS reported that the overall CHD incidence was actually significantly lower in the lowest SES group, although the authors speculated that this may have been due to lower access to hospitals with better diagnostic tools.21
A study on food insecurity as a risk factor for conotruncal heart defects reported that food insecurity was associated with higher adjusted odds of d-transposition of the great arteries, but only among normal-weight and underweight mothers (and not those who were overweight or obese); no association of food insecurity, however, was found with tetralogy of Fallot.16 An analysis of the National Birth Defects Prevention Study revealed that having immigrant parents was associated with significant lower odds of certain CHDs, with the greatest number of significantly protective adjusted ORs noted for foreign-born parents residing ≤5 years vs. >5 years in the US.22 Another study, however, found no association of maternal birthplace with left ventricular outflow-tract malformations.24 Two studies found no association of maternal educational attainment with CHD prevalence.23,24
Infant mortality
Nine articles analyzed associations between SDH and infant mortality in CHD patients (Table 2). Poverty, low parental educational attainment, uninsurance, transportation barriers, and immigration status were significantly associated with infant mortality.1,2,3,27,28,29,30,31,32
A study of 229 children with hypoplastic left heart syndrome (HLHS) identified via the Metropolitan Atlanta Congenital Defects Program documented survival rates that were almost three times worse for those residing in high-poverty (9%) vs. low-poverty (25%; P < 0.001) neighborhoods.32 An analysis of data from birth-defect surveillance programs from four states (Arizona, New York, New Jersey, and Texas) on almost 10,000 infants with CHD revealed that poverty was associated with about double the adjusted odds of infant mortality.3
Low maternal educational attainment was associated with a significantly higher risk of CHD infant mortality in three studies.1,3,30 For example, one study of coarctation of the aorta revealed a mortality rates of 27% for infants of mothers who had not completed high school vs. 5% for those who at least completed high school (P = 0.004).30 Research on 4390 infants with CHD also documented that lower paternal educational was associated with a 62% increased risk of infant mortality.31
An analysis of the Texas Birth Defects Registry revealed that uninsured infants with critical and noncritical CHDs had approximately triple and double the risk of neonatal mortality, respectively, compared with infants with private insurance.29 Another Texas study found that residing in a county bordering Mexico was associated with higher adjusted odds of CHD infant mortality.28
Post-surgical outcomes
A total of 25 articles evaluated the association of SDH with post-surgical outcomes in CHD patients (Table 2). Poverty and low SES were consistently associated with adverse post-operative outcomes, including worse HLHS survival,33 increased in-hospital mortality and resource utilization after orthotopic heart transplant for single-ventricle vs. cardiomyopathy patient cohorts,34 higher inter-stage mortality in the Single Ventricle Reconstruction Trial,35 higher mortality following congenital heart surgery,36 worse 1-year transplant-free survival after the Norwood procedure (stage I palliation for single-ventricle CHD),37 unplanned readmission in the first 90 days after congenital heart surgery,38 longer length of stay and higher resource utilization in patients who underwent congenital heart surgery,39,40 and lower school functioning and QOL.41
One study found that lower maternal educational attainment was associated with a lower Mental Developmental Index score in children who underwent the Norwood procedure,42 but another study found that maternal educational attainment was not associated with neurodevelopmental outcomes in multivariable analyses.43 Two studies found that distance to the hospital was actually associated with a lower risk of readmission post-operatively.38,44 One study also found no association of uninsurance with post-surgical outcomes.44
Access to care, loss to follow-up, and hospital readmissions
Nine articles examined the association of SDH with access to care, loss to follow-up, and hospital admissions (Table 2). Poverty/low SES, transportation barriers, parental educational attainment, and immigrant status were significantly associated with these outcomes. Eight studies documented significant associations of poverty/low SES with these outcomes, including increased risk of missed appointments, loss to follow-up, and hospital readmissions, as well as increases over time of the proportion of admissions to and bed days in pediatric cardiology specialty-care centers. For example, a study of 1034 patients in a large urban pediatric hospital in the Midwest revealed that Medicaid coverage was associated with a significant higher adjusted odds of missing at least one scheduled annual cardiology clinic follow-up visit.45 A study of nearly 800 patients showed that Medicaid coverage and lower median household income were associated with double the unadjusted odds of missed appointments for cardiac magnetic resonance imaging.46 A matched case–control study on risk factors for loss to cardiology clinic follow-up among children and young adults with CHD documented a 1.2 times greater odds of loss to follow-up for every $10,000 reduction in family income.47
Two studies examined transportation barriers and found having to travel ≥200 miles was associated with missed appointments (significantly in bivariate analysis, but with a non-significant trend in multivariable analysis),48 and residence in rural poor communities was associated with the longest mean drive time (69 min) to cardiology clinics.49 One study of a pediatric cardiology outreach clinic for immigrant and refugees found a no-show rate that was higher than the national benchmark.50
Neurodevelopmental outcomes and QOL
Eight articles examined the association of SDH with neurodevelopmental outcomes and QOL in children with CHD and their parents (Table 2). Poverty, parental educational attainment, and transportation barriers were significantly associated with worse neurodevelopmental outcomes and QOL in most studies. Five articles found that poverty/low income was significantly associated with adverse neurodevelopmental or QOL outcomes, including decreased intelligence quotient (IQ), socialization, adaptive behavior, cognition, parental perceived cognitive problems, genetic knowledge, grade-level literacy and math proficiency, memory, and family QOL. For example, an analysis of Arkansas data on children who had CHD surgery at <1 year old found that poverty was associated with double the adjusted odds of not achieving grade-level proficiency in literacy and triple the adjusted odds of not achieving grade-level proficiency in math.51
Lower maternal educational attainment was significantly associated with lower child performance IQ, socialization, adaptive behavior, and cognition in one study52 and with lower grade-level proficiency in literacy in another study.51 Two studies, however, found no association of maternal educational attainment with grade-level proficiency in math or with screening positive on a measure of autism spectrum disorder.51,53
A recent study of 140 parents of young children found that, even when accounting for the severity of the child’s CHD defect (ranging from an innocent murmur to CHD treatment necessitating cardiopulmonary bypass), low income was associated with a significantly lower family QOL.54 Another study found that SES was not associated with parental stress.55
One study showed that a greater travel distance to the hospital was associated with double the adjusted odds of not achieving grade-level proficiency in literacy, but no such association was found for math proficiency.51
Adult congenital heart disease (ACHD)
Nineteen articles examined associations of SDH with ACHD outcomes. Poverty/low income (13 studies), uninsurance (5 studies), educational attainment (3 studies), and transportation barriers (3 studies) were significantly associated with adverse ACHD outcomes (Table 2). Poverty/low income was significantly associated with a variety of adverse ACHD outcomes, including hospital admissions,56 hospital readmission57 and death after ACHD surgery,58 higher inpatient resource utilization,59 physical QOL,60 worse neurocognitive test performance,61 endocarditis-related hospitalizations,62 surgical complications,63 and missed clinic appointments.64 For example, analyses of national databases documented double the odds of inpatient death for low-income (Medicaid) patients after ACHD surgery58 and that patients in the lowest income quartile had significantly higher adjusted odds of hospitalization for infective endocarditis vs. the next income quartile.62
All five studies on uninsurance found significant associations with adverse ACHD outcomes, including significantly greater odds of hospitalization,56,65 outpatient loss to follow-up,66,67 unsuccessful transfer of care from pediatric to adult congenital cardiology care,66 and hospitalization for infective endocarditis.62 For example, one study found that uninsured ACHD patients were significantly less likely to have their pediatric care transferred to ACHD cardiologists, at only 8%, and most likely to have no follow-up, at 74%.66
Three studies found that ACHD patient educational attainment was significantly associated with adverse ACHD outcomes, including lower purpose-of-life scores,68 decreased exercise frequency,69 and residing farther from an ACHD center.70 Three studies also examined the association of transportation barriers with adverse ACHD outcomes. One found that transportation barriers were significantly associated with performance of ACHD surgery outside of an ACHD specialty center.71 Another study revealed that uninsurance, poverty, and lower educational attainment were significantly associated with ACHD patients with >6-h drive to the nearest ACHD center.70 The third study, however, found no association of driving distance with attendance at ACHD outpatient clinic appointments.72
Discussion
This systematic review documented that a wide variety of SDH are significantly associated with adverse outcomes across the lifespan of CHD patients, from prenatal diagnosis to ACHD. Indeed, the study findings dramatically underscore that SDH are significantly associated with many of the most important and serious CHD outcomes, including a lower likelihood of prenatal diagnosis, increased CHD incidence, higher infant mortality, worse post-surgical outcomes, greater inpatient resource utilization, more missed clinic appointments, increased loss to follow-up, lower performance IQ, worse cognition, decreased grade-level proficiency in literacy and math, reduced family QOL, a higher risk for ACHD endocarditis, more ACHD hospitalizations and hospital readmissions, unsuccessful transfer of care from pediatric to adult congenital cardiology care, and increased odds of complications and death after ACHD surgery.
These study findings indicate that an urgent priority and one of the most important interventions for CHD patients would be routinely screening for SDH, with referrals to appropriate services for those who screen positive. The study results suggest that this SDH screening and referral should occur in all CHD care settings, including prenatal visits, neonatal intensive care units and pediatric intensive care units, primary-care and specialty practices, and ACHD clinics. Major national organizations, including the American Academy of Pediatrics, American College of Cardiology, American Academy of Family Physicians, and National Academy of Sciences, Engineering, and Medicine, have all endorsed SDH screening and referral to appropriate services.6,73,74,75,76 Research shows that patients and caregivers are comfortable with SDH screening.73,77,78,79,80 A recent study showed that SDH screening and referral can reduce the number of SDH and improve child health.7
Parent mentors are an evidence-based intervention that has the potential to prove effective in both reducing SDH and improving outcomes for children with CHD and their families. Parent mentors are a special category of community health workers who already have a child with a particular condition (such as CHD) who then receive training to help other parents with children with that condition, including obtaining appropriate healthcare and addressing SDH. A randomized, controlled trial (RCT) of the effects of parent mentors on children with asthma and their families revealed that parent mentors were associated with significant reductions in wheezing, asthma exacerbations, emergency-department visits, and missed parental work days, while improving parental self-efficacy, and saving money.81 Another RCT of a parent-mentor intervention to enroll uninsured children documented that parent mentors are significantly more effective than traditional Medicaid/CHIP outreach and enrollment methods in insuring uninsured minority children; obtaining insurance faster; renewing coverage; improving access to primary, dental, and specialty care; reducing unmet needs and out-of-pocket costs; achieving parental satisfaction and care quality; and sustaining long-term coverage; they also saved $6045 per insured child per year, an 850% return on investment.82 This RCT resulted in federal legislation in the 2018 CHIP Reauthorization bill83 and $120 million in Centers for Medicare and Medicaid Services funding for parent mentors.84,85,86 Thus, parent mentors could analogously prove to be highly effective in addressing SDH in children with CHD and their families.
Study findings on the associations of SDH with ACHD have important implications for practice, research, and policy. CHD has morphed from a critical disease among children to a chronic condition in which the number of ACHD patients (~1.3 million) now exceeds the number children with CHD.9,58,66 Given that at least 85% of children with CHD survive to adulthood, there is an urgent need to provide high-quality specialty care to the growing ACHD population.68 Over time, the number of ACHD hospitalizations has doubled, from ~36,000 in 1998 to >72,000 in 2005.58 Furthermore, the increasing complexity of ACHD has warranted creation of an ACHD subspecialty for centers treating ACHD. SDH screening and appropriate referral to services is thus increasingly critical for ACHD patients. The study results also underscore the importance of consistently considering SES as well as SDH in general when examining health and healthcare outcomes for fetuses, children, and adults with CHD. Furthermore, the study findings suggest that additional research is warranted on the association between SDH and CHD in other developed countries and in developing nations, as well as country comparative studies, particularly regarding the impact of variations in welfare state configurations. Until such research is conducted, caution should be exercised regarding generalizing our study results beyond populations in the US and Canada.
This systematic review revealed several unanswered questions. No published studies were identified on the association of housing instability with CHD outcomes, and a paucity of research was noted on several SDH, including food insecurity, transportation barriers, and lack of health insurance, so more research is need on these topics. The fewest number of studies was noted for fetal diagnosis of CHD, so more investigations are needed of which specific SDH are associated with CHD fetal diagnosis and that provide a deeper exploration for the reasons behind these associations. Although several studies found associations of low maternal educational attainment with infant mortality and other CHD outcomes, only a single study examined paternal educational attainment, so an ongoing unanswered question is whether and how low paternal educational attainment is associated with CHD outcomes.
Based on the findings of this systematic review, a research agenda is proposed. More studies are needed on the unanswered questions noted above. Research is needed on whether multiple SDH are associated with even worse CHD outcomes and how the various SDH might interact. For example, would an uninsured child with household poverty, food insufficiency, and low parental educational attainment be at especially high risk for adverse CHD outcomes? Studies are needed on whether SDH screening and referral to appropriate services results in reduction of SDH and improved outcomes. RCTs are urgently needed of innovative interventions, such as parent mentors, that might eliminate SDH and achieve better outcomes for children and adults with CHDs and their families. More research also is warranted on interventions tailored to reducing SDH for ACHD patients.
Conclusion
SDH are significantly associated with adverse outcomes across the lifespan of CHD patients, from prenatal diagnosis to ACHD. The study findings dramatically underscore that SDH are significantly associated with many of the most important and serious CHD outcomes, including a lower likelihood of prenatal diagnosis, increased CHD incidence, higher infant mortality, worse post-surgical outcomes, greater inpatient resource utilization, more missed clinic appointments, increased loss to follow-up, lower performance IQ, worse cognition, decreased grade-level proficiency in literacy and math, reduced family QOL, a higher risk for ACHD endocarditis, more ACHD hospitalizations and hospital readmissions, unsuccessful transfer of care from pediatric to adult congenital cardiology care, and increased odds of complications and death after ACHD surgery. SDH screening and referral to appropriate services has the potential to improve outcomes for CHD patients across the lifespan. RCTs are urgently needed of innovative interventions, such as parent mentors, that might eliminate SDH and achieve better outcomes for children and adults with CHDs and their families.
References
Peyvandi, S. et al. Socioeconomic mediators of racial and ethnic disparities in congenital heart disease outcomes: a population-based study in California. J. Am. Heart Assoc. 7, e010342 (2018).
Pace, N. D. et al. Sociodemographic factors and survival of infants with congenital heart defects. Pediatrics 142, e20180302 (2018).
Kucik, J. E. et al. Community socioeconomic disadvantage and the survival of infants with congenital heart defects. Am. J. Public Health 104, e150–e157 (2014).
Gilboa, S. M. et al. Congenital heart defects in the United States: estimating the magnitude of the affected population in 2010. Circulation 134, 101–109 (2016).
U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy people 2020: an opportunity to address societal determinants of health in the U.S. https://www.healthypeople.gov/sites/default/files/SocietalDeterminantsHealth.pdf (2020).
Hammond, G. & Joynt Maddox, K. E. A theoretical framework for clinical implementation of social determinants of health. JAMA Cardiol. 4, 1189–1190 (2019).
Gottlieb, L. M. et al. Effects of in-person assistance vs personalized written resources about social services on household social risks and child and caregiver health: a randomized clinical trial. JAMA Netw. Open 3, e200701 (2020).
Hill, G. D., Block, J. R., Tanem, J. B. & Frommelt, M. A. Disparities in the prenatal detection of critical congenital heart disease. Prenat. Diagn. 35, 859–863 (2015).
Peiris, V. et al. Association of socioeconomic position and medical insurance with fetal diagnosis of critical congenital heart disease. Circ. Cardiovasc. Qual. Outcomes 2, 354–360 (2009).
Purkey, N. J. et al. Birth location of infants with critical congenital heart disease in California. Pediatr. Cardiol. 40, 310–318 (2019).
Sekar, P. et al. Diagnosis of congenital heart disease in an era of universal prenatal ultrasound screening in southwest Ohio. Cardiol. Young 25, 35–41 (2015).
Agha, M. M. et al. Socioeconomic status and prevalence of congenital heart defects: does universal access to health care system eliminate the gap? Birth Defects Res. A Clin. Mol. Teratol. 91, 1011–1018 (2011).
Baron, A. M. et al. Congential heart disease in the medicaid population of southern Arizona. Am. J. Cardiol. 88, 462–465 (2001).
Carmichael, S. L., Ma, C. & Shaw, G. M. Socioeconomic measures, orofacial clefts, and conotruncal heart defects in California. Birth Defects Res. A Clin. Mol. Teratol. 85, 850–857 (2009).
Carmichael, S. L., Nelson, V., Wasserman, C. R. & Croen, L. A. Socio-economic status and risk of conotruncal heart defects and orofacial clefts. Paediatr. Perinat. Epidemiol. 17, 264–271 (2003).
Carmichael, S. L. et al. Maternal food insecurity is associated with increased risk of certain birth defects. J. Nutr. 137, 2087–2092 (2007).
Chou, F. S., Chakradhar, R. & Ghimire, L. V. Socioeconomic and racial disparities in the prevalence of congenital heart disease in infants of diabetic mothers. J. Matern. Fetal Neonatal Med. https://doi.org/10.1080/14767058.2019.1702955 (2019).
Correa-Villasenor, A. et al. White-black differences in cardiovascular malformation in infancy and socioeconomic factors. Am. J. Epidemiol. 134, 393–402 (1991).
Egbe, A. et al. Changing prevalence of severe congenital heart disease: a population-based study. Pediatr. Cardiol. 35, 1232–1238 (2014).
Egbe, A. et al. Temporal variation of birth prevalence of congenital heart disease in the United States. Congenit. Heart Dis. 2015, 43–50 (2015).
Egbe, A. et al. Incidences and sociodemographics of specific congenital heart diseases in the United States of America: an evaluation of hospital discharge diagnoses. Pediatr. Cardiol. 35, 975–982 (2014).
Hoyt, A. T. et al. Selected acculturation factors and birth defects in the National Birth Defects Prevention Study, 1997-2011. Birth Defects Res. 111, 598–612 (2019).
Long, J., Ramadhani, T. & Mitchell, L. E. Epidemiology of nonsyndromic conotruncal heart defects in Texas, 1999-2004. Birth Defects Res. A Clin. Mol. Teratol. 88, 971–979 (2010).
McBride, K. L. et al. Epidemiology of noncomplex left ventricular outflow tract obstruction malformations (Aortic valve stenosis, coarctation of the aorta, hypoplastic left heart syndrome) In Texas, 1999 –2001. Birth Defects Res. A Clin. Mol. Teratol. 73, 555–561 (2005).
Peyvandi, S. et al. Environmental and socioeconomic factors influence the live-born incidence of congenital heart disease: a population-based study in California. J. Am. Heart Assoc. 9, e015255 (2020).
Yang, J. et al. Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am. J. Epidemiol. 167, 145–154 (2008).
Almli, L. M., et al. Association between infant mortality attributable to birth defects and payment source for delivery — United States, 2011–2013. MMWR Morbidity Mortality Wkly Rep. 66, 84–87 (2017).
Fixler, D. E. et al. Effect of acculturation and distance from cardiac center on congenital heart disease mortality. Pediatrics 129, 1118–1124 (2012).
Kucik, J. E. et al. Role of health insurance on the survival of infants with congenital heart defects. Am. J. Public Health 104, e62–e70 (2014).
Kuehl, K. S., Baffa, J. M. & Chase, G. A. Insurance and education determine survival in infantile coarctation of the aorta. J. Health Care Poor Underserved 11, 400–411 (2000).
Kuehl, K. S., Loffredo, C. A. & Ferencz, C. Failure to diagnose congenital heart disease in infancy. Pediatrics 103, 743–747 (1999).
Siffel, C., Riehle-Colarusso, T., Oster, M. E. & Correa, A. Survival of children with hypoplastic left heart syndrome. Pediatrics 136, e864–e870 (2015).
Hirsch, J. C. et al. Population-based analysis of survival for hypoplastic left heart syndrome. J. Pediatr. 159, 57–63 (2011).
Bradford, T. T. et al. Comparison of inhospital outcomes of pediatric heart transplantation between single ventricle congenital heart disease and cardiomyopathy. Pediatr. Transplant. 23, e13495 (2019).
Ghanayem, N. S. et al. Interstage mortality after the Norwood procedure: results of the multicenter Single Ventricle Reconstruction trial. J. Thorac. Cardiovasc. Surg. 144, 896–906 (2012).
DeMone, J. A. et al. Risk of death for medicaid recipients undergoing congenital heart surgery. Pediatr. Cardiol. 24, 97–102 (2003).
Tashiro, J. et al. Patent ductus arteriosus ligation in premature infants in the United States. J. Surg. Res. 190, 613–622 (2014).
Lushaj, E. B. et al. Beyond 30 days: analysis of unplanned readmissions during the first year following congenital heart surgery. World J. Pediatr. Congenit. Heart Surg. 11, 177–182 (2020).
Connor, J. A., Gauvreau, K. & Jenkins, K. J. Factors associated with increased resource utilization for congenital heart disease. Pediatrics 116, 689–695 (2005).
Peterson, J. K., Chen, Y., Nguyen, D. V. & Setty, S. P. Current trends in racial, ethnic, and healthcare disparities associated with pediatric cardiac surgery outcomes. Congenit. Heart Dis. 12, 520–532 (2017).
Garcia Guerra, G. et al. Quality of life 4 years after complex heart surgery in infancy. J. Thorac. Cardiovasc. Surg. 145, 482–488 e482 (2013).
Newburger, J. W. et al. Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the Single Ventricle Reconstruction trial. Circulation 125, 2081–2091 (2012).
Alton, G. Y. et al. Early childhood health, growth, and neurodevelopmental outcomes after complete repair of total anomalous pulmonary venous connection at 6 weeks or younger. J. Thorac. Cardiovasc. Surg. 133, 905–911 (2007).
Mackie, A. S. et al. Risk factors for readmission after neonatal cardiac surgery. Ann. Thorac. Surg. 78, 1972–1978 (2004). Discussion 1978.
Jackson, J. L. et al. Racial disparities in clinic follow-up early in life among survivors of congenital heart disease. Congenit. Heart Dis. 14, 305–310 (2019).
Lu, J. C. et al. Predictors of missed appointments in patients referred for congenital or pediatric cardiac magnetic resonance. Pediatr. Radiol. 47, 911–916 (2017).
Mackie, A. S. et al. Risk factors for loss to follow-up among children and young adults with congenital heart disease. Cardiol. Young 22, 307–315 (2012).
Loccoh, E. C. et al. Prevalence and risk factors associated with non-attendance in neurodevelopmental follow-up clinic among infants with CHD. Cardiol. Young 28, 554–560 (2018).
Sommerhalter, K. M. et al. Proximity to pediatric cardiac surgical care among adolescents with congenital heart defects in 11 New York counties. Birth Defects Res. 109, 1494–1503 (2017).
Agrawal, H. et al. Bridging the cardiac needs of a large, underserved immigrant and resettled refugee population. J. Pediatr. 219, 83–88 (2020).
Mulkey, S. B. et al. School-age test proficiency and special education after congenital heart disease surgery in infancy. J. Pediatr. 178, 47.e1–54.e1 (2016).
Majnemer, A. et al. Developmental and functional outcomes at school entry in children with congenital heart defects. J. Pediatr. 153, 55–60 (2008).
Bean Jaworski, J. L. et al. Rates of autism and potential risk factors in children with congenital heart defects. Congenit. Heart Dis. 12, 421–429 (2017).
Lee, J. S. et al. Parents of very young children with congenital heart defects report good quality of life for their children and families regardless of defect severity. Pediatr. Cardiol. 41, 46–53 (2020).
Uzark, K. & Jones, K. Parenting stress and children with heart disease. J. Pediatr. Health Care 17, 163–168 (2003).
Gurvitz, M. Z. et al. Changes in hospitalization patterns among patients with congenital heart disease during the transition from adolescence to adulthood. J. Am. Coll. Cardiol. 49, 875–882 (2007).
Kim, Y. Y., He, W., MacGillivray, T. E. & Benavidez, O. J. Readmissions after adult congenital heart surgery: frequency and risk factors. Congenit. Heart Dis. 12, 159–165 (2017).
Kim, Y. Y. et al. Risk factors for death after adult congenital heart surgery in pediatric hospitals. Circ. Cardiovasc. Qual. Outcomes 4, 433–439 (2011).
Kim, Y. Y. et al. Resource use among adult congenital heart surgery admissions in pediatric hospitals: risk factors for high resource utilization and association with inpatient death. Circ. Cardiovasc. Qual. Outcomes 4, 634–639 (2011).
Jackson, J. L. et al. Medical factors that predict quality of life for young adults with congenital heart disease: what matters most? Int. J. Cardiol. 202, 804–809 (2016).
Kasmi, L. et al. Neurocognitive and psychological outcomes in adults with dextro-transposition of the great arteries corrected by the arterial switch operation. Ann. Thorac. Surg. 105, 830–836 (2018).
Egbe, A. C., Vallabhajosyula, S., Akintoye, E. & Connolly, H. M. Trends and outcomes of infective endocarditis in adults with tetralogy of fallot: a review of the national inpatient sample database. Can. J. Cardiol. 35, 721–726 (2019).
Setton, M., He, W. & Benavidez, O. J. Morbidity during adult congenital heart surgery admissions. Pediatr. Cardiol. 40, 987–993 (2019).
Bhatt, A. B., Rajabali, A., He, W. & Benavidez, O. J. High resource use among adult congenital heart surgery admissions in adult hospitals: risk factors and association with death and comorbidities. Congenit. Heart Dis. 10, 13–20 (2015).
Lu, Y., Agrawal, G., Lin, C. W. & Williams, R. G. Inpatient admissions and costs of congenital heart disease from adolescence to young adulthood. Am. Heart J. 168, 948–955 (2014).
Bohun, C. M. et al. Challenges of intra-institutional transfer of care from paediatric to adult congenital cardiology: the need for retention as well as transition. Cardiol. Young 26, 327–333 (2016).
Goossens, E., Fernandes, S. M., Landzberg, M. J. & Moons, P. Implementation of the American College of Cardiology/American Heart Association 2008 Guidelines for the management of adults with congenital heart disease. Am. J. Cardiol. 116, 452–457 (2015).
Balon, Y. E., Then, K. L., Rankin, J. A. & Fung, T. Looking beyond the biophysical realm to optimize health: results of a survey of psychological well-being in adults with congenital cardiac disease. Cardiol. Young 18, 494–501 (2008).
Connor, B. et al. Factors associated with increased exercise in adults with congenital heart disease. Am. J. Cardiol. 124, 947–951 (2019).
Salciccioli, K. B. et al. A model for geographic and sociodemographic access to care disparities for adults with congenital heart disease. Congenit. Heart Dis. 14, 752–759 (2019).
Fernandes, S. M. et al. Trends in utilization of specialty care centers in California for adults with congenital heart disease. Am. J. Cardiol. 115, 1298–1304 (2015).
Awh, K. et al. Clinic nonattendance is associated with increased emergency department visits in adults with congenital heart disease. Congenit. Heart Dis. 14, 726–734 (2019).
De Marchis, E. H., Alderwick, H. & Gottlieb, L. M. Do patients want help addressing social risks? J. Am. Board Fam. Med. 33, 170–175 (2020).
National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health (National Academies Press, Washington, DC, 2019).
Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics 137, 1–14 (2016).
American Academy of Physicians. The EveryONE project: screening tools and resources to advance health equity. https://www.aafp.org/patient-care/social-determinants-of-health/everyone-project/eop-tools.html (2020).
Byhoff, E. et al. Part II. A qualitative study of social risk screening acceptability in patients and caregivers. Am. J. Prev. Med. 57, S38–S46 (2019).
De Marchis, E. H. et al. Part I: A quantitative study of social risk screening acceptability in patients and caregivers. Am. J. Prev. Med. 57, S25–S37 (2019).
Hassan, A. et al. Youths’ health-related social problems: concerns often overlooked during the medical visit. J. Adolesce. Health 53, 265–271 (2013).
Wylie, S. A. et al. Assessing and referring adolescents’ health-related social problems: qualitative evaluation of a novel web-based approach. J. Telemed. Telecare 18, 392–398 (2012).
Flores, G. et al. Improving asthma outcomes in minority children: a randomized, controlled trial of parent mentors. Pediatrics 124, 1522–1532 (2009).
Flores, G. et al. Parent mentors and insuring uninsured children: a randomized controlled trial. Pediatrics 137, e20153519 (2016).
US Congress. Rules Committee Print 115-55. Text of Extension of Continuing Appropriations Act, 2018 [Showing the text of H.J. Res. 125, as introduced]. http://docs.house.gov/billsthisweek/20180115/BILLS-115SAHR195-RCP115-55.pdf (2018).
Centers for Medicare & Medicaid Services Insurekidsnow.gov. Engaging parent mentors to increase participation of eligible children in Medicaid and CHIP. https://www.insurekidsnow.gov/webinars-videos/webinars/20181108/index.html (2018).
Centers for Medicare & Medicaid Services Insurekidsnow.gov. 2019 HEALTHY KIDS outreach and enrollment cooperative agreements. CMS awards $48 million to help enroll eligible children in health coverage. https://www.insurekidsnow.gov/campaign/funding/2019-healthykids/index.html (2019).
Centers for Medicare & Medicaid Services Insurekidsnow.gov. Connecting Kids to Coverage Outreach and Enrollment Grants. CMS Awards Nearly $6 Million in Funding for Nine New Connecting Kids to Coverage HEALTHY KIDS American Indian and Alaska Native (AI/AN) 2020 Outreach and Enrollment Cooperative Agreements. https://www.insurekidsnow.gov/campaign-information/outreach-enrollment-grants/index.html (2020).
Chang, R.-K. R., Chen, A. Y. & Klitzner, T. S. Clinical management of infants with hypoplastic left heart syndrome in the United States, 1988–1997. Pediatrics 110, 292–298 (2002).
Erickson, L. C. et al. The impact of managed care insurance on use of lower-mortality hospitals by children undergoing cardiac surgery in California. Pediatrics 105, 1271–1278 (2000).
McCrindle, B. W. et al. Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation 113, 1123–1129 (2006).
Benavidez, O. J., Gauvreau, K. & Jenkins, K. J. Racial and ethnic disparities in mortality following congenital heart surgery. Pediatr. Cardiol. 27, 321–328 (2006).
Chang, R. K., Rodriguez, S., Lee, M. & Klitzner, T. S. Risk factors for deaths occurring within 30 days and 1 year after hospital discharge for cardiac surgery among pediatric patients. Am. Heart J. 152, 386–393 (2006).
Chang, R.-K. R., Chen, A. Y. & Klitzner, T. S. Factors associated with age at operation for children with congenital heart disease. Pediatrics 105, 1073–1081 (2000).
Williams, I. A. et al. Functional state following the Fontan procedure. Cardiol. Young 19, 320–330 (2009).
Chan, T., Pinto, N. M. & Bratton, S. L. Racial and insurance disparities in hospital mortality for children undergoing congenital heart surgery. Pediatr. Cardiol. 33, 1026–1039 (2012).
Tweddell, J. S. et al. Intermediate-term mortality and cardiac transplantation in infants with single-ventricle lesions: risk factors and their interaction with shunt type. J. Thorac. Cardiovasc. Surg. 144, 152–159 (2012).
Bucholz, E. M., Sleeper, L. A. & Newburger, J. W. Neighborhood socioeconomic status and outcomes following the Norwood procedure: an analysis of the Pediatric Heart Network Single Ventricle Reconstruction trial public data set. J. Am. Heart Assoc. 7, e007065 (2018).
Benavidez, O. J., He, W. & Lahoud-Rahme, M. Readmissions following congenital heart surgery in infants and children. Pediatr. Cardiol. 40, 994–1000 (2019).
Goldberg, C. S. et al. Behavior and quality of life at 6 years for children with hypoplastic left heart syndrome. Pediatrics 144, e20191010 (2019).
Chamberlain, L. J. et al. Variation in use of pediatric cardiology subspecialty care: a total population study in California, 1983 to 2011. J. Am. Coll. Cardiol. 66, 37–44 (2015).
Demianczyk, A. C. et al. Social risk factors impact hospital readmission and outpatient appointment adherence for children with congenital heart disease. J. Pediatr. 205, 35.e1–40.e1 (2019).
Woo, J. L. et al. Minimum travel distance among publicly insured infants with severe congenital heart disease: potential impact of in-state restrictions. Pediatr. Cardiol. 40, 1599–1608 (2019).
Limbers, C. A., Emery, K. & Uzark, K. Factors associated with perceived cognitive problems in children and adolescents with congenital heart disease. J. Clin. Psychol. Med. Settings 20, 192–198 (2013).
Fitzgerald-Butt, S. M. et al. Genetic knowledge and attitudes of parents of children with congenital heart defects. Am. J. Med. Genet. A 164A, 3069–3075 (2014).
Cassidy, A. R., Newburger, J. W. & Bellinger, D. C. Learning and memory in adolescents with critical biventricular congenital heart disease. J. Int. Neuropsychol. Soc. 23, 627–639 (2017).
Agarwal, S. et al. Trends in the burden of adult congenital heart disease in US emergency departments. Clin. Cardiol. 39, 391–398 (2016).
Vaikunth, S. S. et al. Short-term outcomes following implementation of a dedicated young adult congenital heart disease transition program. Congenit. Heart Dis. 13, 85–91 (2018).
Acknowledgements
We thank Brenda Labbe for her administrative support. No extramural financial assistance was received in support of this study.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the study conception and design, acquisition of data, analysis, interpretation of data, drafting the article, and revising the article critically for important intellectual content. Conceptualization: B.D. and G.F.; methodology: B.D., M.G., and G.F.; data curation: B.D., J.H.L., and M.G.; writing: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
As this was a systematic review, patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Davey, B., Sinha, R., Lee, J.H. et al. Social determinants of health and outcomes for children and adults with congenital heart disease: a systematic review. Pediatr Res 89, 275–294 (2021). https://doi.org/10.1038/s41390-020-01196-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-020-01196-6
This article is cited by
-
Impact of Social Determinants of Health on Outcomes for Patients with Adult Congenital Heart Disease
Current Cardiology Reports (2024)
-
Lower Socioeconomic Status is Associated with an Increased Incidence and Spectrum of Major Congenital Heart Disease and Associated Extracardiac Pathology
Pediatric Cardiology (2024)
-
Association between maternal marginalization and infants born with congenital heart disease in Ontario Canada
BMC Public Health (2023)
-
The ‘Ironclad friendship’ of China-Cambodia, lays the first step in the foundation of early diagnosis and treatment of asymptomatic congenital heart Defects- A multi-national screening and intervention project, 2017–2020
BMC Cardiovascular Disorders (2023)
-
Social inequities hurt babies’ hearts: a commentary on Forero-Manzano, MJ, et al.
Pediatric Research (2023)