Abstract
Research regarding the mental health of the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual, 2 Spirit (LGBTQIA2S+) community has been historically biased by individual and structural homophobia, biphobia, and transphobia, resulting in research that does not represent the best quality science. Furthermore, much of this research does not serve the best interests or priorities of LGBTQIA2S + communities, despite significant mental health disparities and great need for quality mental health research and treatments in these populations. Here, we will highlight how bias has resulted in missed opportunities for advancing understanding of mental health within LGBTQIA2S + communities. We cite up-to-date research on mental health disparities facing the LGBTQIA2S + community and targeted treatment strategies, as well as guidance from health care professionals. Importantly, research is discussed from both preclinical and clinical perspectives, providing common language and research priorities from a translational perspective. Given the rising tide of anti-transgender sentiment among certain political factions, we further emphasize and discuss the impact of historical and present day ciscentrism and structural transphobia in transgender mental health research, from both clinical and translational perspectives, with suggestions for future directions to improve the quality of this field. Finally, we address current best practices for treatment of mental health issues in this community. This approach provides an opportunity to dispel myths regarding the LGBTQIA2S + community as well as inform the scientific community of best practices to work with this community in an equitable manner. Thus, our approach ties preclinical and clinical research within the LGBTQIA2S + community.
Similar content being viewed by others
Introduction
Science and medicine have a history of pathologizing the Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, Asexual, 2 Spirit (LGBTQIA2S+) community (definitions in Box 1). It was not until 1974 that same-sex attraction was removed from the Diagnostic and Statistical Manual of Mental Disorders (DSM), yet distress over same-sex attraction remained until 2013 [1, 2]. Research on the health of the LGBTQIA2S + community has been biased by individual and structural homophobia, biphobia, and transphobia, resulting in research that fails to represent the best science. Here, we amplify the call from the community to de-pathologize these identities within science, particularly neuroscience and psychiatry. Furthermore, we describe the need for precise reporting of demographic data in health-related research, provide treatment directions, and convey such information to the public for both knowledge and policy decision-making.
Numerous examples exist of recently published studies pathologizing the LGBTQIA2S + community; even calling for eugenic practices to reduce our number - modifying the neural circuits of transgender, non-binary, and/or gender diverse (TNG) people to eliminate their transness. We will not cite these papers. One retracted example is a review article from 2021 that compared altered neurotransmitter levels in LGBTQIA2S + people vs. heterosexuals, to alterations in people with psychiatric conditions, arguing that LGBTQIA2S + identity is innately pathological. The impact of minority stress on the LGBTQIA2S + people was only briefly mentioned, despite well-established links between stress and psychiatric illness. The authors discussed the role of neurotransmitters in rodent partner preference, comparing to human sexual orientation. They manipulated graphs from another study, mislabeling axes to make it appear that drug treatment can ‘change’ an animal’s ‘sexual preference’ (male mounting behavior). Such manipulations and misrepresentations are highly problematic. Additionally, the trans community has been used as a ‘model’, or ‘natural experiment’ for hormone activity in the context of behavior and physiology, e.g., ‘inducing gender dysphoria’ in TNG people in the scanner to determine neural correlates. While it is important to be aware of the mistakes of the past, our commentary will focus on looking ahead to best experimental practices for basic and clinical science that can address the needs of the LGBTQIA2S + community, starting with guidance on best clinical practices for this diverse community with specific mental health needs.
Clinical approaches
Practical steps exist that can improve the mental health and quality of life for LGBTQIA2S + people. The relationship between psychiatry and the community is fraught e.g., many TNG people require a diagnosis to access medical transition services with ICD-10 still using the term “gender identity disorder” for insurance billing. The APA replaced “gender identity disorder” with “gender dysphoria” for DSM-V (2013), paralleling changes made to homosexuality diagnoses (1970s/80 s). The terminology of disease and disorder highlights how LGBTQIA2S + people have been harmed by the healthcare system, influencing access to gender-affirming hormone therapy (GAHT) and other TNG healthcare needs. Many studies documented discriminatory, even violent, treatment of LGBTQIA2S + people seeking health care [3]. Even well-meaning providers often lack knowledge of appropriate care. These diagnostic issues are compounded by the now well-documented prevalence of discriminatory treatment of racial minority groups by the mental health field [4], with LGBTQIA2S + people of color experiencing more deterrents to quality mental health care.
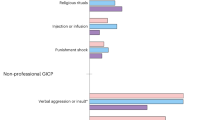
Members of the community are at increased risk for mental health struggles, including depression, anxiety, PTSD, substance use, and suicide [5]. Increased risk arise from factors including discrimination, marginalization, bullying, and loneliness. Unlike others, sexual and gender minorities are often stigmatized by their own families of origin, with long-term negative effects including underinsurance and housing instability [5]. Delineating the impact of these stressors remain vital in working with this community and coordinating preclinical research (see below). These factors, plus negative prior healthcare experiences, impact clinic attendance, compounding difficulties faced by LGBTQIAS2 + people.
Providers hoping to support LGBTQIA2S + people also face challenges, e.g., sufficient training [6], and avoiding/ignoring topics not understood. Some clinicians fear committing microaggressions, offending patients, or being out-of-date. Providers may refer patients to specialists, leading to a bimodal distribution in which providers see either few or exclusively LGBTQIA2S + patients. Providers may have implicit or even explicit prejudice against sexual and gender minorities, compounding challenges faced by those seeking help. Finally, there is a growing movement from the political right using violent threats to intimidate and terrorize healthcare providers serving this community, particularly trans-youth providers.
Challenges are common, but steps can be taken to help LGBTQIAS2 + people lead healthy, joyful lives [7]. Clinicians should mirror patients’ language about their identities, relationships, pronouns, and bodies. Any misstep, briefly apologize and move on. Rather than assuming what a word or phrase might mean, take a curious stance, asking open-ended, clarifying questions (see Box 2). Validate the unique strengths of LGBTQIAS2 + people and affirm healthy or rewarding expressions of sexuality/gender. Identifying and restructuring any cognitions that may arise from minority stress, e.g., belief of personal failure, inferiority, or expectation of rejection (the latter is a constant experience within the community and not a distortion as it accurately predicts future experiences). Finally, as with all patients, it is vital to facilitate emotional awareness, regulation, and acceptance.
Clinics and research facilities are also important. Front-desk staff should avoid using gendered words/pronouns with new patients/participants. Gender-neutral bathrooms should be available. Protocols should exist to share names/pronouns, address mail, and leave phone messages for future contact. Easily accessible lists should be made of local and online LGBTQIAS2 + resources. Charts should lead with names and pronouns the patients themselves use. Finally, notes and auto-populated text should be gender-affirming. Such steps can destigmatize, minimize stress, and increase access to quality mental health care for all.
Gender-affirming care for youth
We have seen an onslaught of transphobic attacks on research and gender-affirming medical care presently available to TNG youth. Verbal threats against staff of pediatric gender clinics (2022), warranted increased police security for such university-based programs (https://www.wcvb.com/article/boston-children-s-hospital-transgender-care-harassment/40924239). A four-site NIH-funded research on GAHT was investigated for ‘suppressing data not supportive of GAHT’ – patently not true – while calls for more evidence-based studies of pediatric gender care were made and referred to as ‘vital’! How can such research be conducted while under attack and meet the needs of trans youth, while being accused of child abuse?
The new paradigm of gender development articulates that gender variations are not psychiatric disorders and do not warrant treatment to “fix”/discourage gender expansive expressions/identities. Rather, children demonstrate multiple pathways to healthy gender consolidation, interweaving biology, socialization, and cultural context as they traverse from infancy to adulthood. There are increased number of adolescents seeking gender care worldwide, e.g., Tavistock and Portman group from the UK’s National Health Service reported >2500 referrals (2021), up from 137 (2011). Researchers and social commentators, asserted that this increase [they describe as “rapid onset gender dysphoria” (ROGD)], is a form of contagion due to social influencers and activist-providers promoting a ‘transgender agenda’. This work was conducted from a biased sample i.e., recruited from online forums for parents unsupportive of their child’s identity. This ‘sudden’ disclosure of transgender identity is more likely because youths knew they were transgender and did not disclose because they (rightly), suspected poor support. A simpler explanation comes from the experience of left-handed people. Actuarial data reveal a jump in left-handed people from 2–10% (1900–1950), remaining consistent at ~10% to this day [8, 9]. Sudden onset of left-handedness was not a contagion, but likely arose from removing the taboo against left-handedness, who prohibited from expressing left-handedness, were forced to use their right. Lifting left-handed prejudice enabled more left-handed people to live an authentic left-handed life. Likewise, lifting biases against gender diversity enables youth to explore and articulate their authentic gender selves, increasing numbers seeking GAHT. The fact that many cisgender people express concern about numbers of TNG people is telling. The notion that, as a society, we should limit the number of people allowed access to medical transition belies claims that handwringing regarding TNG youth is not rooted in bigotry.
No major professional association has validated ROGD. Such pseudo-scientific claims contribute to transphobic rhetoric and action, e.g., protests at facilities providing TNG care. Researchers continue to study and publish peer-reviewed reports on GAHT that help children, practitioners will continue to provide such care. GAHT reduces odds of depression and suicidality, representing a vital health care intervention [10]. High rates of satisfaction among receiving such care [11], support its continued practice to help the small Ts in this community.
Preclinical research-sex differences
How can researchers conduct preclinical work that benefits LGBTQIA2S + communities? Rodent models enable the study of LGBTQIA2S + health, if used with due consideration of translational applicability and to societal issues faced (not reproducible in rodents). While such limitations need to be considered generally, interpretation of rodent behavioral data presents a particular challenge for questions related to gender identity/sexual orientation given political standpoints [12], writing laws for political expediency hurting LGBTQIA2S + youth. Too often researchers still confuse socially constructed concepts of ‘gender’ with ‘sex’, only the latter is observable in rodents based on anogenital distance differences, gonads, or XX or XY chromosomes. These concepts are often rooted in bioessentialism and phrases like “biological sex” can be anti-trans dog-whistles.
While research study design include both sexes, rodent experimental outcomes usually do not show a binary profile when comparing females and males. Sex differences in biological and behavioral measures can be observed, but there are distribution variances overlap. Female rodents are not necessarily more variable than males [13], a premise precluding use of females in research for decades. Overlapping variance may suggest that rodent behavior may not be sexually dimorphic and consideration of female and male data as a continuum in rodent studies.
We urge caution when attempting to study the neurobiological mechanisms underlying gender identity/sexual orientation. One crucial consideration for this research lies in the challenge of finding relevant behavioral correlates of human sexual preference in rodents. Studies have assessed effects of hormones or neurotransmitters on mounting behavior to evaluate sexual preference, but this behavior is also a sign of aggression/dominance in rodents - not applicable to human sexual orientation. Furthermore, it is unclear how knowing the biological basis of sexual orientation/gender identity research would improve LGBTQIA2S + health. Research should be guided by the need to address health challenges disproportionately affecting this community. Thus, rodent research aimed at better treating/preventing stress effects and on long-lasting behavioral outcomes will benefit LGBTQIA2S + communities. Other species exist for which same-sex preferences may be clearer (e.g., non-human primates), but such laboratory-based research opportunities remain limited. Either way, the choice of any model to improve LGBTQIA2S + health should be guided by the specific needs of the community. Improving treatments or preventions to mitigate the impact of minority stress on mental health should certainly take precedence over understanding the biological basis underlying LGBTQIA2S + identity.
Preclinical research-GAHT
Translational research historically failed to acknowledge TNG or intersex people. The first animal model of GAHT use was recent [14]—one year after the U.S. National Institute of Health mandated use of females (in addition to males), in research. No regulations yet require gender expansive individuals be included. Randomized controlled trials on GAHT cannot be ethically conducted because GAHT is already established as the standard-of-care improving mental health outcomes [10, 15]. This lack of research enables the pathologization of TNG people, promoting discriminatory policies (Miyagi et al 2021), including restricting GAHT access [16].
Animal models of GAHT enable genetic manipulation and precise neuronal/molecular recordings impossible in humans. Thus, researchers can address deficits in our knowledge of GAHT effects specifically: (1) gene expression in the brain; (2) neural processes involved in affective-relevant behaviors; (3) neural networks controlling social behavior; (4) cognitive processes; and (5) neurological control of metabolism and physiology [17]. Each process requires careful longitudinal monitoring coupled with community-based knowledge to ensure that translational research addresses the needs of the TNG community. Additionally, such research should be mindful of the language used to describe patterns of GAHT effects, avoiding pathologizing language (e.g., “impair”/“deficit”), instead utilizing “reduce”/“increase”, when describing outcomes.
It is important to state that in expanding our understanding of the effects of hormonal and developmental state on TNG identity, researchers do not contribute to biologically essentialist notions of gender and sex. Setting arbitrary biological parameters for TNG identities would serve as an additional barrier to accessing healthcare. Such stressors coupled with increased rejection sensitivity would lead to healthcare avoidance, devastating mental health [18,19,20,21]. Translational research should also answer the questions raised above at important developmental stages [17], to inform the long-term impact on TNG-relevant physiological outcomes.
Most biomedical and sociocultural discussions of GAHT outcomes focus on physical characteristics, not neurological impacts. Avenues for future research include, investigating the impact of gonadal hormonal milieu on psychiatric medication efficacy, response to rejection and ostracization, cognition during chronic stress, and metabolism throughout life. Utilizing translational research approaches-to help the TNG community vs. using that community-are urgently needed for their mental health.
Discussion
The long-history of stigmatizing the LGBTQIA2S + community (from those providing care, the public, families, to leading neuroscientists and psychiatrists), has increased their susceptibility to psychiatric illness. The actions of the political right and other groups, attacking LGBTQIA2S + people, organizations, researchers, and clinicians, should be of increasing concern. We warn neuroscience and psychiatry against the use of their work and express a call-to-action in support of our LGBTQIA2S + community. Such stigmatization and negative (including traumatic), experiences drive stress responses, negatively impacting mental health [5]. Previously, this stress feedback was not well-handled in the clinic, given stigmatization, lack-of-knowledge, and poor training. Thus, while we acknowledge stress contributions to the development of psychiatric conditions, psychiatry and neuroscience have long-contributed to the higher odds-ratio of occurrence within the LGBTQIA2 + community. Going beyond recrimination, however, we show here that researchers and clinicians can provide an off-ramp to better mental health for all (Box 3).
We know that GAHT lowers odds of depression and suicidality [10], with high rates of satisfaction [11], thus is a vital health care intervention. Research understanding the impact of GAHT are still required. GAHT impact on brain gene expression, neural networks involved in affective, social-, and cognitive-relevant behaviors, plus metabolism and physiology (at all developmental stages), can be determined preclinically–studies unfathomable in humans. Such research recognizes that caution should be taken when attempting to study the neurobiological mechanisms underlying gender identity/sexual orientation, as relevant behavioral correlates of human sexual preference remain unclear. Overlapping biological and behavioral variance seen between male and female rodents suggest viewing these data as a continuum. Importantly, all research should be guided by the need to address health challenges disproportionately affecting this community, including minimizing stress impacts in future studies.
Ultimately, with increased TNG youth requiring GAHT, scientists should be able to help using approved techniques that reduce depression and suicidal ideation rates without violent or political threats. While generating data on such care, the scientific field should be wary of it being used to create scientific-sounding issues as providing cover for anti-trans dog whistles [e.g., ROGD [22]]. TNG is not an illness – there is no ‘contagion’. Increased visibility and awareness give people the language for self-expression. Recognizing people as they are is an important step toward improving mental health in the community.
References
Association AP (1994). Diagnostic and statistical manual of mental disorders. 4th Edition.
Association AP (2013). Diagnostic and statistical manual of mental disorders. 5th Edition.
Rodriguez A, Agardh A, Asamoah BO. Self-reported discrimination in health-care settings based on recognizability as transgender: a cross-sectional study among transgender U.S. citizens. Arch Sex Behav. 2018;47:973–85.
Shim RS. Dismantling structural racism in psychiatry: a path to mental health equity. Am J Psychiatry. 2021;178:592–8.
Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in white and Latino lesbian, gay, and bisexual young adults. Pediatrics. 2009;123:346–52.
Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306:971–7.
Stubbe DE. Interest in identity: improving LGBTQ psychiatric care. Focus (Am Psychiatr Publ). 2020;18:300–3.
Papadatou-Pastou M, Ntolka E, Schmitz J, Martin M, Munafo MR, Ocklenburg S, et al. Human handedness: A meta-analysis. Psychol Bull. 2020;146:481–524.
Gilbert AN, Wysocki CJ. Hand preference and age in the United States. Neuropsychologia. 1992;30:601–8.
Green AE, DeChants JP, Price MN, Davis CK. Association of gender-affirming hormone therapy with depression, thoughts of suicide, and attempted suicide among transgender and nonbinary youth. J Adolesc Health. 2022;70:643–9.
Sequeira GM, Kidd KM, Rankine J, Miller E, Ray KN, Fortenberry JD, et al. Gender-diverse youth’s experiences and satisfaction with telemedicine for gender-affirming care during the COVID-19 pandemic. Transgend Health. 2022;7:127–34.
Park BC, Das RK, Drolet BC. Political issues surrounding gender-affirming care for transgender youth-reply. JAMA Pediatr. 2022;176:323.
Becker JB, Prendergast BJ, Liang JW. Female rats are not more variable than male rats: a meta-analysis of neuroscience studies. Biol Sex Differ. 2016;7:34.
Goetz TG, Mamillapalli R, Devlin MJ, Robbins AE, Majidi-Zolbin M, Taylor HS. Cross-sex testosterone therapy in ovariectomized mice: addition of low-dose estrogen preserves bone architecture. Am J Physiol Endocrinol Metab. 2017;313:E540–51.
Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, Deutsch MB, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgend Health. 2022;23:S1–S259.
Redcay A, Bergquist K, Luquet W. On the basis of gender: a medical-legal review of barriers to healthcare for transgender and gender-expansive patients. Soc Work Public Health. 2021;36:615–27.
Aghi K, Goetz TG, Pfau DR, Sun SED, Roepke TA, Guthman EM. Centering the needs of transgender, nonbinary, and gender-diverse populations in neuroendocrine models of gender-affirming hormone therapy. Biol Psychiatry Cogn Neurosci Neuroimaging. 2022;7:1268–79.
Hughto JMW, Pachankis JE, Reisner SL. Healthcare mistreatment and avoidance in trans masculine adults: the mediating role of rejection sensitivity. Psychol Sex Orientat Gend Divers. 2018;5:471–81.
Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: a meta-analytic review. Psychol Bull. 2014;140:921–48.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129:674–97.
Puckett JA, Matsuno E, Dyar C, Mustanski B, Newcomb ME. Mental health and resilience in transgender individuals: What type of support makes a difference? J Fam Psychol. 2019;33:954–64.
Bauer GR, Lawson ML, Metzger DL, Trans Youth CANRT. Do clinical data from transgender adolescents support the phenomenon of “rapid onset gender dysphoria”? J Pediatr. 2022;243:224–227.e222.
Acknowledgements
We would like to thank Drs. E. Kale Edmiston, E. Mae Guthman and William Carlezon for their support and encouragement, as well as the American College of Neuropsychopharmacology for the opportunity to bring together these researchers, providing a platform to discuss such important topics. We also would like to thank funding sources R25MH119043 and R13MH126604.
Author information
Authors and Affiliations
Contributions
TG: Substantial Contributions to the work design, drafting the work, and final approval. KA: Substantial Contributions to the work design, drafting the work, and final approval. CA: Substantial Contributions to the work design, drafting the work, and final approval. DE: Substantial Contributions to the work design, drafting the work, and final approval. NE: Substantial Contributions to the work design, drafting the work, and final approval. JM: Instigating the work, contributing to its design, drafting, and final approval. JY: Instigating the work, contributing to its design, drafting, and final approval. TR: Instigating the work, contributing to its design, drafting, and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goetz, T.G., Aghi, K., Anacker, C. et al. Perspective on equitable translational studies and clinical support for an unbiased inclusion of the LGBTQIA2S+community. Neuropsychopharmacol. 48, 852–856 (2023). https://doi.org/10.1038/s41386-023-01558-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-023-01558-8
This article is cited by
-
Integrating sex and gender in mental health research: enhanced funding for better treatments
Nature Mental Health (2023)