Abstract
Depressive symptomology has been linked to low-grade peripheral inflammatory markers (PIMs), specifically C-reactive protein (CRP) and white blood cell count (WBC). However, such associations may be affected by multiple moderators (including race/ethnicity), though few well-powered and racially diverse studies have examined this. We examined 31 moderators of PIM-depression relationships in a large racially diverse cohort (n = 21,570). We also examined if associations between PIM and depression severity were dependent on clinical cutpoints for moderate depressive symptoms and elevated CRP. We found several positive moderators of PIM-depression relationships for both WBC and CRP: ongoing medication use (antidepressant, statin, or any prescription drug), presence of sleep concerns, and poor health status (β’s = 0.06–0.21, p’s < 0.05). For both WBC and CRP, individuals of non-Hispanic White race/ethnicity were found to have stronger PIM-depression associations overall relative to minoritized groups (B’s = 0.14 to 1.01, p’s < 0.05). For CRP, stronger PIM-depression relationships existed for individuals with moderate (or greater) depression severity or elevated CRP (B’s = 0.27 to 0.49, p’s < 0.05). Thus, a wide range of moderators appears to affect PIM-depression associations. These results could help identify participants with strong coupling of PIM-depression severity, to guide future research and personalized treatments for depression and to indicate gaps in the applicability of widely referenced theoretical models among racial/ethnic minoritized groups.
Similar content being viewed by others
Introduction
In recent years, the relationship between low-grade peripheral inflammatory marker (PIM) elevation and depressive symptomology has been highlighted [1]. Numerous studies identify cross-sectional associations between PIMs (e.g., C-reactive protein (CRP), interleukin-6 (IL-6), white blood cell count (WBC)) and depression severity and suggest bidirectional casual associations between PIMs and depression [2,3,4,5,6]. Specifically, PIMs may be causally related to depressive symptoms through effects on neurotransmitters, neural circuitry, or other biological pathways (e.g., hypothalamic-pituitary axis, gut-brain axis, or kynurenine pathway activation) that are associated with depressive symptoms [3]. Furthermore, growing evidence suggests that low-grade PIM elevation may contribute to or be associated with depressive symptomology more strongly in certain subgroups of depressed patients (e.g., males) [7, 8]. While prior studies have examined such subgroups of patients based on depressive symptoms [9, 10] or immunological profiles [11], fewer studies have examined subgroups based on other readily available patient-level characteristics (e.g., age) that might contribute to variation in strength of PIM-depression associations [12]. Yet, identification of such subgroups is critical to help guide individualized treatments for depression (e.g., immunomodulatory agents or specific antidepressants) that would allow unique targeting of inflammatory dysregulation. From a statistical standpoint, lack of attention to subgroup effects on PIM-depression associations may result in Simpson’s paradox (whereby statistical relationships present in a population are reversed or absent when breaking down the population into subgroups) or result in failure to detect PIM-depression associations that are more relevant for select subgroups [13].
To better recognize such subgroups, studies have started to examine a few moderators (e.g., gender, body mass index) of the PIM-depression relationship [12]. Assessment of the effects of potential moderators would allow elucidation of the precise patient-level factors, which when present or at greater severity, might be linked to stronger PIM-depression associations. Prior studies have examined variations in the relationship between PIM levels and depression severity in a few different subgroups [12], with some suggesting that PIM-depression severity associations are greater in males, White individuals, and individuals with obesity. However, a comprehensive review of the literature reveals mixed results in terms of both the existence and the direction of differences in the strength of PIM-depression severity relationships across these and other subgroups (see Supplementary Material S1). These mixed results may be explained by differences in the nature of the cohorts (e.g., depressed participants, community cohorts, or cohorts with certain physical health conditions) which could limit ability to detect significant effects, particularly given that strength of such associations between depression severity and PIMs may vary based on the subgroup. In addition, many relationships have only been examined in small cohorts and with factors more distally related to depression—e.g., in one small study (n = 87), sleep disturbance was associated with greater associations between stress and inflammatory gene-expression [14], but it was unclear if such associations might extend to relationships between depressive symptoms and PIMs. Given these disparate findings, examination of a wide range of potential moderators (e.g., antidepressant use, physical activity, substance use, or psychosocial factors) in a singular well-powered cohort (which has not been done in prior studies) could fine-tune research involved in the study of PIM-depression associations.
Furthermore, while some studies have examined moderators of inflammatory-depression relationships for CRP, few have examined such relationships for another important PIM–WBC. Higher WBC levels have been associated with greater depression severity [5, 6] and increased risk of outcomes related to depression (e.g., suicide) [15] and might be tied to depression differently from CRP given that it indexes physiologically different aspects of the immune system [16, 17]. Importantly, prior research also has suggested that interaction effects related to PIM or depression subgroups may exist, for instance, that PIM-depression associations are stronger in individuals with greater CRP levels or with clinical depression [3, 18, 19].
Recent research has emphasized the importance of studying one potential moderator in particular– race/ethnicity [20]. Though examination of race/ethnicity as a variable in analysis is important to provide information on generalizability of a study and to identify potential disparities/inequities in the relevance and influence of pathophysiological mechanisms related to depression, race and ethnicity are dynamic social constructs that stand in for other factors, including but not limited to social determinants of health, racial/ethnic disparities, ancestral heritage, and effects of racism [21]. Thus, close examination of moderation effects of race/ethnicity is needed given the dearth of large cohort studies examining PIM-depression associations in racial and ethnic minorities and mixed results in prior analyses [22].
To answer these questions, we sought to examine a wide range of potential moderators of the relationship between PIMs (WBC, CRP) and depression in a large, well-powered, racially diverse community cohort (n = 21,570). To identify whether certain moderators affect the strength and/or direction of PIM-depression relationships, we utilize data from the racially diverse National Health and Nutrition Examination Survey (NHANES) cohort to examine 31 potential moderators for which prior empirical evidence supports a role in PIM-depression relationships (see Supplementary Material S1), including a close examination of moderation effects of race/ethnicity. We hypothesized that the potential role of these moderators would be clarified through our use of a large sample and comprehensive analytic approach. Given evidence from prior studies [3, 18, 19], we also examined interaction effects related to PIM or depression severity subgroups, e.g., if PIM-depression severity associations were stronger in participants with elevated CRP or with Patient Health Questionnaire (PHQ)-defined moderate/severe depression. On an exploratory basis, to enhance clinical relevance, we also examined moderator effects specifically in a subgroup of participants with PHQ-defined moderate/severe depression (n = 1692). Our results can be used to identify cohorts of individuals with close linkage of depressive symptoms with PIM levels, based on a broad range of patient-level characteristics. Identification of such cohorts would allow recognition of patient populations that might specifically benefit from interventions targeting depression related to inflammatory dysregulation and inform studies attempting to parse pathophysiological links between depression and low-grade PIM elevation.
Methods
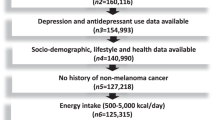
Participants
Participants included 21,570 adults participating in any of five cycles of NHANES (cycles included 2005–2006, 2007–2008, 2009–2010, 2015–2016, 2017–2018) with at least one PIM level (CRP or WBC count) and with complete PHQ-9 scores [23]. NHANES is a survey that has been conducted in the United States to provide vital and health statistics on the US population. The survey includes an interview (covering participant-reported sociodemographic information, medical information, depression survey (PHQ-9)) and also a mobile laboratory consisting of medical professionals who conduct further assessment of health status and obtain laboratory tests. One of NHANES’ goals is to provide greater health information related to racial/ethnic minorities, which are thus overrepresented in NHANES [23].
Primary measures
The well-validated PHQ-9 was used as our measure of depression severity, with scores ranging from 0 to 27 (greater scores indicating worse depression severity). PHQ scores can be used to categorically reflect severity of depression, i.e., indicating moderate depression (scores 10–14), moderately severe depression (scores 15–19), or severe depression (scores 20+) [24]. Our use of the term “moderate/severe depression” indicates moderate, moderately severe, or severe depression. Serum CRP levels were obtained through analysis via latex-enhanced nephelometry on a Behring Nephelometer or Beckman Coulter Synchron analyzers, with LLODs < 0.15 mg/L. Values below the LLOD were replaced by the LLOD divided by the square root of two. WBC counts were obtained through Beckman Coulter analyzers. Consistent with prior studies, we excluded participants with CRP > 10 mg/L or WBC > 11 × 109 cells/L which represent likely active infection/inflammation. Normal clinical values for CRP range between 0 and 10 mg/L and for WBC range between 4.5 and 11 × 109 cells/L [25, 26]. Of note, PIM levels were appreciably similar across different cycles of NHANES and the methods used to assess both CRP and WBC in NHANES have consistently demonstrated high reliability (see Supplementary Material S2) [27, 28].
Moderators
We examined 31 potential moderators, with more extensive details in Supplementary Material S3. Demographic measures included age, gender (male/female), marital status (married/cohabitating or not), education level (above or equivalent to/below high school), poverty index (lower scores indicating greater poverty levels). We included self-reported race/ethnicity as both a dichotomous measure (non-Hispanic White vs. non-White or Hispanic) to be consistent with prior studies and a categorical measure with four categories: non-Hispanic White, Black, Mexican–American, and Other Hispanic (Hispanic but not Mexican–American). For gender and race, no other categories (e.g., other genders or races/ethnicities) were available in NHANES datasets. Objective measures obtained included body mass index (BMI), obesity (defined as BMI > 30), serum cotinine levels (reflecting recent nicotine exposure), hemoglobin A1C (used both continuously and dichotomized at 6.5%). Self-report measures based on questionnaires included smoking (presence/absence in past month), general health status (scaled 1–5 with higher scores indicating worse overall health), vigorous physical activity (both days/week and presence/absence), sedentary time (minutes/week), alcohol use (drinks/day over the past year), illicit drug use (use ever), specific current prescription medication use (i.e., antidepressant, opiate, NSAID, statin), any aspirin use, any current prescription medication use (presence/absence), sleep concerns (presence/absence), and sleep disorder diagnosis (presence/absence).
Analysis details
The statistical software R version 3.5.2 (see https://cran.r-project.org/) was used for statistical analyses (with use of the packages interactions and lsr). For primary moderation analyses, linear regression models incorporated the interaction terms and main effects of the PIM and moderator as independent variables (IVs) in predicting the dependent variable (DV) of depression severity (operationalized by PHQ-9 scores). To examine interaction effects related to PIM or depression severity subgroups, we used linear regression models examining the interaction of PHQ-defined moderate/severe depression status × PIM in predicting depression severity and independently, interaction of elevated CRP status (CRP > 3 mg/L) × PIM in predicting depression severity, given prior studies suggesting this form of statistical interaction [19, 29]. A significant interaction term in either of these analyses indicates an interactive relationship between PIMs and the moderator. Both WBC and CRP were natural log-transformed in all analyses given skewed distributions, with raw values only presented for descriptive purposes. All categorical variables (including elevated CRP status and PHQ-defined moderate/severe depression status) were dummy coded. Standardized beta coefficients (utilizing z-score standardization) are presented for comparison of continuous variables, while unstandardized beta coefficients are presented for comparison of categorical variables (as these were dummy coded). In the Supplementary Material, we also provide examples of regression equations (see Supplementary Material S4) and tables/graphs examining simple slopes to more easily interpret moderation effects (see Supplementary Material S5). FDR multiple comparisons adjustment was used for all tests done for all primary analyses for PIM (i.e., correcting for 64 comparisons), with reporting of both unadjusted and adjusted p values.
In exploratory analyses, we also examined PIM*moderator interactions in predicting depression severity solely in participants with PHQ-9-defined moderate/severe depression, in identical fashion to our primary analysis (with a similar analysis done for nondepressed participants for descriptive purposes in Supplementary Material S6).
In sensitivity analyses examining impact of covariates, we individually included potential covariates (age, gender, race, smoking, prescription drug use, chronic illness burden, BMI, recent acute illness, and poverty) that might confound relationships by including covariates in linear regression models with exactly 4 IVs (PIM*moderator interaction terms and covariate of interest) and one DV (PHQ-9 scores) (see Supplementary Material S7/S8/S9). This methodology was used given prior studies noting variance in results dependent on which covariates were included in analysis and potential causal effects of depression on covariates, which would reduce ability to detect true effect sizes. Our sensitivity analysis examining impact of covariates generally had appreciably similar results to those in the primary analysis, with exceptions noted in the results. For interested readers, we also performed a post hoc replication analysis examining two random subsamples of the full datasets, finding that significant moderation models were similarly predictive in two random subsamples of data (see Supplementary Material S10).
Results
Demographic and clinical characteristics
Our cohort was comprised of 21,570 individuals (mean age = 48.1, 50.8% male, 43% non-Hispanic White). Average CRP levels were 2.39 mg/L and average WBC levels were 6.9 × 109 cells/L. Average PHQ-9 scores were 3.04, with ~7.8% of the cohort with scores above the PHQ-9 cutpoint associated with clinical depression (PHQ-9 score > 9) [24]. Depression severity was significantly associated with both logCRP levels (Std. β = 0.28, p = 1.2 × 10−24, n = 21,315) and logWBC levels (Std. β = 0.26, p = 1.5 × 10−20, n = 21,506). For descriptive purposes, summary statistics for all moderators are listed in Supplementary Material S11.
Interactions of PIM and moderators to predict depression severity
In our moderation analyses, for both logCRP and logWBC, participants with ongoing prescription medication use (antidepressant, statin, or any prescription drug), sleep concerns, and worse general health status had stronger associations between PIMs (both logWBC and logCRP) and depression severity as compared to patients without or with lesser levels of those factors (padjusted’s < 0.05; see Table 1). For logWBC specifically, participants with SSRI use had stronger logWBC-depression associations (padjusted < 0.001). For logCRP specifically, participants with NSAID use, greater BMI/obesity, greater HbA1c, greater age, with a sleep disorder, and with greater levels of poverty had stronger logCRP-depression associations (padjusted’s < 0.05). No appreciable differences were noted on sensitivity analysis adjusting for potential confounders for these listed significant findings, except that moderation effects related to HbA1c and age for logCRP were lower and not statistically significant (see Supplementary Material S7). Figures 1, 2 descriptively illustrate PIM-depression severity based on the moderator level. For interested readers, we also provide a summary table of variables that were potential moderators, potential confounders, or both in Supplementary Material S12.
This figure displays effect sizes for CRP-depression associations (beta weights in linear regression models with CRP as IV and PHQ-9 as the DV) in the subgroup with either higher levels of the moderator (e.g., participants with moderator present or (for display purposes) with values of moderator > median of the moderator—in blue) and the subgroup with lower levels of the moderator (e.g., participants with moderator absent or (for display purposes) with values of moderator < median of the moderator—in orange). For instance, for antidepressant use, beta weights for logCRP were 0.39 in antidepressant users and approximately 0.17 in non-users of antidepressants when examining linear regression models with logCRP as the IV and PHQ-9 scores as the DV in these two subgroups. Asterisks are provided by the moderator’s name in the bar graph for those with significant interaction effects (adjusted p < 0.05) as described in Table 1. The bracketed numbers indicate the magnitude of difference between PIM-depression associations in the group with higher levels of the moderator and the group with lower levels of the moderator, with highlighting of the moderator in orange done for those with a magnitude difference of 2 or greater.
This figure displays effect sizes for WBC-depression associations (beta weights in linear regression models with WBC as IV and PHQ-9 as the DV) in the subgroup with either higher levels of the moderator (e.g., participants with moderator present or (for display purposes) with values of moderator > median of the moderator—in blue) and the subgroup with lower levels of the moderator (e.g., participants with moderator absent or (for display purposes) with values of moderator < median of the moderator—in orange). For instance, for antidepressant use, beta weights for logWBC were approximately 2.7 in antidepressant users and approximately 0.76 in non-users of antidepressants when examining linear regression models with logWBC as the IV and PHQ-9 scores as the DV in these two subgroups. Asterisks are provided by the moderator’s name in the bar graph for those with significant interaction effects (adjusted p < 0.05) as described in Table 1. The bracketed numbers indicate the magnitude of difference between PIM-depression associations in the group with higher levels of the moderator and the group with lower levels of the moderator, with highlighting of the moderator in orange done for those with a magnitude difference of 2 or greater.
Differences in PIM-depression severity relationships based on Racial/Ethnic Group
In our moderation analyses examining race/ethnicity, for both logCRP and logWBC, participants of non-Hispanic White race/ethnicity (compared to minoritized races/ethnicities and Black race/ethnicity specifically) had stronger associations between PIMs and depression severity (padjusted’s < 0.05; see Table 2). For logWBC specifically, participants of non-Hispanic White race (compared to Mexican–American race/ethnicity and Other Hispanic race/ethnicity) had stronger logWBC-depression associations (padjusted’s < 0.01). On examination of specific racial/ethnic groups where significant moderator effect differences were found, significant associations between logCRP and depression severity were observed in non-Hispanic White participants (B = 0.339, p < 0.001) but not Black participants (B = 0.0927, p = 0.09). For logWBC, associations between logWBC and depression severity were observed in participants of White (B = 1.64, p < 0.001) and Black race/ethnicities (B = 0.84, p < 0.001), but not participants of Mexican–American and Other Hispanic ethnicities (p’s > 0.7). No appreciable differences were noted on sensitivity analysis adjusting for potential confounders (see Supplementary Material S8). Supplementary Material S13 descriptively illustrates PIM-depression severity based on the race/ethnicity.
Interaction effects related to PIM or depression severity subgroups
For logCRP, there was evidence of an overall interaction relationship related to depression severity subgroups between PHQ scores and logCRP, whereby participants with PHQ-defined moderate/severe depression (n = 1692), as compared to those without (n = 19,878), had significantly stronger associations between logCRP and depression severity (Std. B = 0.08, B = 0.27, punadjusted < 0.001, padjusted < 0.001). Similarly, for logCRP, participants with CRP > 3 mg/L (n = 6102), as compared to those with CRP < 3 mg/L (n = 15,213), had stronger associations between logCRP and depression severity (Std. B = 0.245, B = 0.49, punadjusted = 0.002, padjusted = 0.007). For logWBC, interaction effects related to PIM or depression severity subgroups were not identified (punadjusted’s > 0.11). No appreciable differences were noted on sensitivity analysis adjusting for potential confounders (see Supplementary Material S9).
Moderation effects within PHQ-defined moderate/severe depression cohort
To examine clinical relevance to MDD, we also examined if similar moderator effects existed within participants with PHQ-defined moderate/severe depression (n = 1692, see Table 3). For logCRP, worse health status, greater sedentary time, and non-married/non-cohabitating status were associated with greater logCRP-depression associations (p’s < 0.05). For logWBC, use of SSRIs, use of any prescription medication, presence of sleep disorder, and less alcohol use were associated with greater logWBC-depression associations (p’s < 0.05). Qualitatively, some similarities with our primary findings existed in terms of moderation effects (e.g., for health status and sedentary time), but also notable differences in presence or direction of moderation effects for other findings (e.g., NSAID use for WBC/CRP, BMI for CRP, and alcohol use for WBC). In examining the unique moderator of race/ethnic group, significant moderating effects of race/ethnicity on PIM-depression severity were not found for either logCRP or logWBC, with the supplement detailing PIM-depression associations within racial/ethnic subgroups (see Supplementary Material S14).
Discussion
Our analysis of the large, racially diverse, community based NHANES cohort supports previously reported associations between depression severity and PIMs (both WBC and CRP). This study adds to the existing literature by providing strong evidence for a significant effect of several moderators that alter the strength, presence/absence, or direction of these associations. Specifically, we found that participants using certain medications (antidepressants or statins), using any prescription medication, with poor health status or sleep concerns, or of non-Hispanic White race/ethnicity (as compared to both minoritized races/ethnicities and specifically Black race/ethnicity) had stronger PIM-depression associations for both WBC and CRP, while additional PIM-specific moderation effects were also noted. These findings from a large and diverse community sample suggest that models linking PIMs and depression, which are based largely on homogeneous or selective cohorts (e.g., predominantly Caucasian with limited racial diversity) may be far more relevant for certain subsets of patients than for others, with corresponding potential specific treatment needs (e.g., specific immunomodulatory treatments targeting depressive symptoms). Interaction effects related to PIM or depression severity subgroups were also found such that participants with both elevated CRP and with PHQ-9-defined moderate/severe depression had significantly stronger associations between depression severity and CRP (but not WBC). Our findings greatly advance the evidence base identifying moderators of PIM-depression associations, given that prior studies implying such associations have often examined few moderators in a given sample (e.g., <5), used selective cohorts (e.g., including individuals with specific physical illness but not healthy individuals, precluding true moderation tests), examined only select PIMs (e.g., CRP but not WBC), and/or examined moderating effects on the association between PIMs and constructs peripherally related to depression severity (e.g., stress), but not to depression symptoms per se (see Supplementary Material S1). In sum, these findings allow greater precision in identifying multilevel patient characteristics that may be associated with either stronger or weaker associations between PIMs-depression severity for both WBC and CRP, allowing more nuanced approaches to identifying patients who might respond to treatments targeting inflammatory dysregulation in depression.
For our primary findings for moderators common to both CRP and WBC, we identified that use of any prescription medication or certain prescribed medications (antidepressants or statins) were associated with greater PIM-depression severity relationships, which is surprising given that certain antidepressants (e.g., certain SSRIs) and certain statins have been associated with reductions in PIMs (e.g., interleukin-6 or CRP) [30]. However, this might reflect that in such patients, residual low-grade inflammation, due to either a wider range of disease processes (e.g., physical diseases requiring additional medication treatment) or sequalae of such diseases, makes a particularly strong contribution to depression (or vice versa). In the case of antidepressants, it could also be the case that these medications are better equipped to reduce depressive symptoms with discrete etiologies unrelated to WBC/CRP, while leaving depression driven by PIMs relatively unresolved, thus enhancing associations between PIMs and depression. We also identified that patients with sleep concerns and poor health status had stronger associations between depression severity and inflammatory processes, consistent with extant studies noting effects of these factors which might potentially contribute to immune system sensitization [31, 32].
We also found several PIM-specific moderators of PIM-depression associations, emphasizing that moderators of these relationships are complex and not uniform across types of PIMs. For CRP specifically, NSAID use, less physical activity (both amount and presence), greater obesity/BMI, higher HbA1c, older age, greater poverty levels, and sleep disorders were linked to stronger PIM-depression associations. Metabolic factors (greater obesity/BMI and higher HbA1c) and less physical activity have been hypothesized in theoretical models to synergistically contribute (along with inflammatory dysregulation) to depressive symptoms via neuronal neurotransmitter effects [33]. Similarly, poverty, greater age, and sleep disorders may be associated with other factors that might either sensitize the immune system or depressive symptomology (e.g., health status, stress, adiposity-related metabolites), while moderating effects of NSAID use may be related to physical illnesses requiring NSAID use that have stronger associations between PIMs and depression severity [34, 35]. For WBC specifically, SSRI use was linked to stronger PIM-depression relationships, which may be for reasons as described above for antidepressant use.
Of note, we found that CRP and WBC had different moderators of the PIM-depression severity association, particularly with CRP having several cardiometabolic and stress-related moderators (greater obesity/BMI, higher HbA1c, and sleep disorders). These differences may be because CRP itself is thought to play a strong role in worsening of stress/metabolic conditions (compared to WBC which may not be as closely linked [36]), and thus CRP elevations in the context of these stress/cardiometabolic conditions may play a particularly large contribution to such conditions. Notably, CRP and WBC reflect a different set of biological processes, as CRP is an acute phase protein released by the liver in response to factors (prominently interleukin-6) released by immune cells and adipocytes while WBC is an index of circulating cells in blood released from the bone marrow or blood vessel walls in response to a broad array of immune factors such as colony-stimulating factors or chemoattractants [16, 37]. Consistent with prior studies [16, 17], our results emphasize that while PIMs have similarities in moderation effects, notable differences in moderation effects between PIMs exist, warranting caution in extrapolating results from one PIM to another or utilizing “composite” PIM indices.
The racially diverse nature of our cohort allowed for well-powered analysis of race/ethnicity moderator effects. It is important to recognize that race/ethnic categories are not genetically defined but rather are social constructs which are largely cumulative proxies for societal factors that result in wide-reaching disparities (e.g., impacts of systemic racism; socioeconomic disparities, etc.) [21]. For CRP (similar to reports in smaller analyses of NHANES [22]), participants of non-Hispanic White race (as compared to all non-White/Hispanic race/ethnicities, and to Black participants in particular) had significantly stronger PIM-depression associations, with similar findings for WBC, though participants with Mexican–American and Other Hispanic race/ethnicity also had significantly weaker PIM-depression associations compared to participants of White race for WBC. However, when examining individuals with PHQ-defined moderate/severe depression, such moderation effects of race/ethnicity appeared to be nonexistent or much weaker, suggesting depressed patient cohorts might have more uniform PIM-depression links across racial groups.
Our findings related to race/ethnicity emphasize the importance of moderator and subgroup analyses, given that in individuals with PHQ-defined moderate/severe depression, depressive symptoms may simply contribute more significantly to PIM variability (extinguishing any effects related to race/ethnicity) given medium to large reported effect associations between moderate/severe depression and PIMs in meta-analyses [38], while in individuals without these high level of depressive symptoms, other factors differing amongst racial/ethnic groups (e.g., level of discrimination or socioeconomic status) may contribute to PIM variability [39, 40]. Thus, research in minoritized depressed populations might focus on health characteristics that are linked to stronger PIM-depression associations. For instance, if researchers observe positive effects of targeted behavioral treatments towards obesity in minoritized populations, they might then be able to utilize such behavioral treatments in conjunction with anti-inflammatory treatments (e.g., infliximab) to maximize effectiveness of such treatments to treat depressive symptoms. However, further studies are required to fully understand factors affecting PIMs levels and depressive symptoms in minoritized groups. Importantly, given that such studies often use self-report measures of depression, these studies would benefit from thoroughly validating existing self-report depression measures in minoritized groups, though preliminary studies suggest that certain self-report measures such as the PHQ-9 are valid and reliable amongst different racial/ethnic minority groups [41,42,43].
In regards to interaction effects related to PIM or depression severity subgroups, we found that CRP-depression severity relationships were stronger in participants with PHQ-defined moderate/severe depression and also in participants with elevated CRP levels (which did not occur for WBC-depression severity relationships). Stronger CRP-depression severity association in depressed patients or patients with elevated CRP is consistent with existing theories of bidirectional interactions between PIMs and depressive symptoms that may be present in patients with moderate/severe depression [3].
On exploratory analysis solely examining participants with PHQ-defined moderate/severe depression (n = 1692), we found that some moderator effects were similar to the primary results (e.g., SSRI use for WBC). However, certain moderator effects disappeared (e.g., BMI for CRP) while other moderator effects emerged (e.g., alcohol use for WBC). Thus, a unique pattern of moderation effects may be relevant to clinically depressed patients as compared to nondepressed individuals. Future methodologically rigorous studies are needed to examine the pattern of such moderator effects specifically in patients with clinician-assessed major depressive disorder to extend the clinical relevance of our findings.
Our findings advance the field by identifying individual-level factors that are linked to stronger PIM-depression associations, which allows more targeted assessment of potential mechanisms related to PIM-depression associations and hones the focus on inflammatory-related treatments that might target depressive symptoms. Importantly, individual moderator relationships strongly affected PIM-depression associations, given patients with certain characteristics (e.g., taking SSRIs), as compared to patients without those characteristics, had up to 4 times stronger PIM-depression severity associations. If such moderator effects compounded, this could lead to PIM-depression associations that could potentially be much higher (e.g., up to 10+ times) for individuals with multiple positive moderators (e.g., for CRP, individuals who had both elevated BMI and were NSAID users). From a statistical standpoint, these findings speak to the need to stratify analyses (or include moderator or interaction effects related to PIM or depression severity subgroups) in studies examining PIM-depression associations, given that solely covarying for variables might lead to biased estimates in the presence of moderating effects. Similarly, exclusion of participants based on moderators, grouping together of subgroups (leading to reversal/disappearance of subgroup effects), and smaller sample sizes may affect potential PIM-depression associations (see Supplementary Material S15 for further discussion).
Yet, our analysis should be considered in the context of certain limitations. Primarily, our measures of depression and certain moderators (e.g., health status, substance use, medications) were based on self-report and thus susceptible to biases that could either overinflate or underestimate effect sizes. However, at least some self-report measures (e.g., health status) have shown moderate clinical concordance, and PHQ-9 scores are well-validated with respect to clinician-assessed depression diagnosis [24]. Given the multiple comparisons correction, our findings may have been vulnerable to Type II error. Lastly, we were unable to account for potential associations that may be secondary to other variables (e.g., genetic factors, unmeasured pathophysiological factors, childhood trauma) or account for causal relationships between variables, which might be better explored in future longitudinal studies (e.g., randomized controlled trials).
In summary, in our analysis of 21,570 participants in a racially diverse community sample, we found several common positive moderators (antidepressant use, statin use, sleep concerns, prescription medication use, poor health status, non-Hispanic White race/ethnicity) of PIM-depression severity associations for both WBC and CRP, as well as several PIM-specific moderators. Our findings emphasize that individuals with such participant characteristics (or factors associated with these characteristics) have stronger coupling of PIMs and depression severity, making them populations where clinical assessment of low-grade PIMs and corresponding prescription of treatments targeting inflammatory-related depression, when present, may be particularly useful and warranted. Moreover, identification of these patient-specific moderators can help refine studies examining pathophysiological underpinnings of depression related to inflammatory dysregulation by shedding light on the subgroups of individuals where the theoretical model of inflammatory-related depression may be more vs. less applicable. Guided by our cross-sectional findings, future studies probing causal relationships could be designed to further identify the causal chains linking moderators, PIMs, and depression symptoms.
References
Köhler CA, Freitas TH, Stubbs B, Maes M, Solmi M, Veronese N, et al. Peripheral alterations in cytokine and chemokine levels after antidepressant drug treatment for major depressive disorder: systematic review and meta-analysis. Mol Neurobiol. 2018;55:4195–206.
Valkanova V, Ebmeier KP, Allan CL. CRP, IL-6 and depression: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2013;150:736–44.
Rengasamy M, Marsland A, Spada M, Hsiung K, Kovats T, Price RB. A chicken and egg scenario in psychoneuroimmunology: bidirectional mechanisms linking cytokines and depression. J Affect Disord Rep. 2021;6:100177.
Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107:234–56.
Shafiee M, Tayefi M, Hassanian SM, Ghaneifar Z, Parizadeh MR, Avan A, et al. Depression and anxiety symptoms are associated with white blood cell count and red cell distribution width: a sex-stratified analysis in a population-based study. Psychoneuroendocrinology. 2017;84:101–08.
Sealock JM, Lee YH, Moscati A, Venkatesh S, Voloudakis G, Straub P, et al. Use of the PsycheMERGE network to investigate the association between depression polygenic scores and white blood cell count. JAMA Psychiatry. 2021;78:1365–74.
Felger JC, Miller AH. Identifying immunophenotypes of inflammation in depression: dismantling the monolith. Biol Psychiatry. 2020;88:136–8.
Milaneschi Y, Lamers F, Berk M, Penninx BW. Depression heterogeneity and its biological underpinnings: toward immunometabolic depression. Biol Psychiatry. 2020;88:369–80.
Lamers F, Milaneschi Y, Vinkers CH, Schoevers RA, Giltay EJ, Penninx BW. Depression profilers and immuno-metabolic dysregulation: longitudinal results from the NESDA study. Brain Behav Immun. 2020;88:174–83.
Moriarity DP, van Borkulo C, Alloy LB. Inflammatory phenotype of depression symptom structure: a network perspective. Brain Behav Immun. 2021;93:35–42.
Lynall M-E, Turner L, Bhatti J, Cavanagh J, de Boer P, Mondelli V, et al. Peripheral blood cell–stratified subgroups of inflamed depression. Biol Psychiatry. 2020;88:185–96.
Cho SH, Lim J-E, Lee J, Lee JS, Jeong H-G, Lee M-S, et al. Association between high-sensitivity C-reactive protein levels and depression: moderation by age, sex, obesity, and aerobic physical activity. J Affect Disord. 2021;291:375–83.
Kievit R, Frankenhuis WE, Waldorp L, Borsboom D. Simpson’s paradox in psychological science: a practical guide. Front Psychol. 2013;4:513.
Chiang JJ, Cole SW, Bower JE, Irwin MR, Taylor SE, Arevalo J, et al. Daily interpersonal stress, sleep duration, and gene regulation during late adolescence. Psychoneuroendocrinology. 2019;103:147–55.
Batty GD, Jung KJ, Lee S, Back JH, Jee SH. Systemic inflammation and suicide risk: cohort study of 419 527 Korean men and women. J Epidemiol Community Health. 2018;72:572–4.
Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Front Immunol. 2018;9:754.
McIntyre WJ, Tami JA. Introduction to immunology. Pharmacotherapy. 1992;12:2S–10S.
Liukkonen T, Silvennoinen-Kassinen S, Jokelainen J, Räsänen P, Leinonen M, Meyer-Rochow VB, et al. The association between C-reactive protein levels and depression: results from the northern Finland 1966 birth cohort study. Biol Psychiatry. 2006;60:825–30.
Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med. 2009;71:171–86.
Horn SR, Long MM, Nelson BW, Allen NB, Fisher PA, Byrne ML. Replication and reproducibility issues in the relationship between C-reactive protein and depression: a systematic review and focused meta-analysis. Brain Behav Immun. 2018;73:85–114.
Flanagin A, Frey T, Christiansen SL. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA. 2021;326:621–7.
Case SM, Stewart JC. Race/ethnicity moderates the relationship between depressive symptom severity and C-reactive protein: 2005–2010 NHANES data. Brain Behav Immun. 2014;41:101–08.
NHANES. Centers for Disease Control and Prevention website. 2021. https://doi.org/10.1038/s41386-022-01341-1. accessed June 20 2021.
Moriarty AS, Gilbody S, McMillan D, Manea L. Screening and case finding for major depressive disorder using the Patient Health Questionnaire (PHQ-9): a meta-analysis. Gen Hosp Psychiatry. 2015;37:567–76.
Osei-Bimpong A, Meek J, Lewis S. ESR or CRP? A comparison of their clinical utility. Hematology. 2007;12:353–7.
Riley LK, Rupert J. Evaluation of patients with leukocytosis. Am Fam Physician. 2015;92:1004–11.
Fink P, Romer M, Haeckel R, Fateh-Moghadam A, Delanghe J, Gressner A, et al. Measurement of proteins with the Behring Nephelometer. A multicentre evaluation. J Clin Chem Clin Biochem. 1989;27:261–76.
Imeri F, Herklotz R, Risch L, Arbetsleitner C, Zerlauth M, Risch GM, et al. Stability of hematological analytes depends on the hematology analyser used: a stability study with Bayer Advia 120, Beckman Coulter LH 750 and Sysmex XE 2100. Clin Chim Acta. 2008;397:68–71.
Felger JC, Haroon E, Patel TA, Goldsmith DR, Wommack EC, Woolwine BJ, et al. What does plasma CRP tell us about peripheral and central inflammation in depression? Mol Psychiatry. 2020;25:1301–11.
O’Connor M-F, Bower JE, Cho HJ, Creswell JD, Dimitrov S, Hamby ME, et al. To assess, to control, to exclude: effects of biobehavioral factors on circulating inflammatory markers. Brain Behav Immun. 2009;23:887–97.
Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–15.
Austin V, Crack PJ, Bozinovski S, Miller AA, Vlahos R. COPD and stroke: are systemic inflammation and oxidative stress the missing links? Clin Sci. 2016;130:1039–50.
Chan KL, Cathomas F, Russo SJ. Central and peripheral inflammation link metabolic syndrome and major depressive disorder. Physiology. 2019;34:123–33.
Sparkman NL, Johnson RW. Neuroinflammation associated with aging sensitizes the brain to the effects of infection or stress. Neuroimmunomodulation. 2008;15:323–30.
Steptoe A, Owen N, Kunz-Ebrecht S, Mohamed-Ali V. Inflammatory cytokines, socioeconomic status, and acute stress responsivity. Brain Behav Immun. 2002;16:774–84.
Haffner SM. The metabolic syndrome: inflammation, diabetes mellitus, and cardiovascular disease. Am J Cardiol. 2006;97:3–11.
Abramson N, Melton B. Leukocytosis: basics of clinical assessment. Am Fam Physician. 2000;62:2053–60.
Osimo EF, Pillinger T, Rodriguez IM, Khandaker GM, Pariante CM, Howes OD. Inflammatory markers in depression: a meta-analysis of mean differences and variability in 5166 patients and 5083 controls. Brain Behavior Immunity. 2020;87:901–9.
Lewis TT, Aiello AE, Leurgans S, Kelly J, Barnes LL. Self-reported experiences of everyday discrimination are associated with elevated C-reactive protein levels in older African-American adults. Brain Behav Immun. 2010;24:438–43.
Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann NY Acad Sci. 2010;1186:69–101.
Patel JS, Oh Y, Rand KL, Wu W, Cyders MA, Kroenke K, et al. Measurement invariance of the patient health questionnaire‐9 (PHQ‐9) depression screener in US adults across sex, race/ethnicity, and education level: Nhanes 2005–2016. Depress Anxiety. 2019;36:813–23.
Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210:653–61.
Sung SC, Low CCH, Fung DSS, Chan YH. Screening for major and minor depression in a multiethnic sample of A sian primary care patients: A comparison of the nine‐item Patient Health Questionnaire (PHQ‐9) and the 16‐item Quick Inventory of Depressive Symptomatology–Self‐Report (QIDS‐SR16). Asia‐Pac Psychiatry. 2013;5:249–58.
Funding
This research was supported by funding from the Ruth L. Kirschstein National Research Service Award Institutional Research Training Grants sponsored by the National Institutes of Health (Grant No. NIH T32 MH018951: Brent).
Author information
Authors and Affiliations
Contributions
MR and RP contributed to the study conception. MR primarily analyzed data. MR, SA, MS, and RP interpreted the data. MR and MS wrote the paper with input from the other authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rengasamy, M., Da Costa E Silva, S.A., Spada, M. et al. Does the moderator matter? Identification of multiple moderators of the association between peripheral inflammatory markers and depression severity in a large racially diverse community cohort. Neuropsychopharmacol. 47, 1693–1701 (2022). https://doi.org/10.1038/s41386-022-01341-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-022-01341-1
This article is cited by
-
Exploring the multiverse: the impact of researchers’ analytic decisions on relationships between depression and inflammatory markers
Neuropsychopharmacology (2023)
-
Does the moderator matter? Identification of multiple moderators of the association between peripheral inflammatory markers and depression severity in a large racially diverse community cohort
Neuropsychopharmacology (2022)