Abstract
Although sex differences in psychiatric disorders abound, few neuropsychopharmacology (NPP) studies consider sex as a biological variable (SABV). We conducted a scoping review of this literature in humans by systematically searching PubMed to identify peer-reviewed journal articles published before March 2020 that (1) studied FDA-approved medications used to treat psychiatric disorders (or related symptoms) and (2) adequately evaluated sex differences using in vivo neuroimaging methodologies. Of the 251 NPP studies that included both sexes and considered SABV in analyses, 80% used methodologies that eliminated the effect of sex (e.g., by including sex as a covariate to control for its effect). Only 20% (50 studies) adequately evaluated sex differences either by testing for an interaction involving sex or by stratifying analyses by sex. Of these 50 studies, 72% found statistically significant sex differences in at least one outcome. Sex differences in neural and behavioral outcomes were studied more often in drugs indicated for conditions with known sex differences. Likewise, the majority of studies conducted in those drug classes noted sex differences: antidepressants (13 of 16), antipsychotics (10 of 12), sedative-hypnotics (6 of 10), and stimulants (6 of 10). In contrast, only two studies of mood stabilizers evaluated SABV, with one noting a sex difference. By mapping this literature, we bring into sharp relief how few studies adequately evaluate sex differences in NPP studies. Currently, all NIH-funded studies are required to consider SABV. We urge scientific journals, peer reviewers, and regulatory agencies to require researchers to consider SABV in their research. Continuing to ignore SABV in NPP research has ramifications both in terms of rigor and reproducibility of research, potentially leading to costly consequences and unrealized benefits.
Similar content being viewed by others
Introduction
Although potential sex differences are rarely evaluated within the brain [1,2,3], in published findings, they are remarkably prevalent [2, 4,5,6,7], with reliable sex differences found in brain size, contributing to differences in white/gray matter ratio, intra- versus interhemispheric connectivity, and regional cortical and subcortical volumes [8]. Normative sex differences in the brain may give rise to sex-biased vulnerabilities to certain psychiatric disorders—such as anxiety, depression, schizophrenia, and attention deficit hyperactivity disorder (ADHD) [4, 9]. In general, women are more likely than men to be prescribed psychiatric medications—even for psychiatric disorders that are more common among men [10,11,12,13,14,15]. Many of these drugs show differences in efficacy as well as side effects between males and females, e.g., [15,16,17], which may be related, in part, to sex differences in how these drugs act on the brain. Yet, except for zolpidem (Ambien®) [18], these medications are prescribed without consideration of sex.
In order to examine the extent to which sex differences have been appropriately evaluated in human neuropsychopharmacology (NPP) studies, we conducted a scoping review, a technique that allows researchers to map the relevant literature in a field of interest [19]. Compared to systematic reviews, scoping reviews tend to have greater breadth than depth and include all studies on a given topic regardless of study design (i.e., not only randomized controlled trials) [19]. As a result, scoping reviews do not seek to synthesize the evidence and do not assess whether the findings are robust or generalizable [19]. However, like systematic reviews, scoping reviews employ a systematic search of the literature. Because our review topic was broad with emerging evidence across a wide variety of study designs, a scoping review was the appropriate approach to investigate whether studies utilizing human neuroimaging in psychopharmacology research consider sex as a biological variable (SABV) in analyses. In our scoping review, we use the term ‘neuropsychopharmacology’ to refer to human studies using neural measures (in our case neuroimaging) to either predict treatment response or understand neural effects of psychiatric drugs.
We expected to find that few NPP studies evaluated sex differences—in either the neural effects of pharmacotherapy or neural predictors of treatment response. This assumption was based on three lines of evidence. First, neuroimaging technologies are expensive, which leads to smaller sample sizes in neuroimaging studies and limits power to detect sex differences. Second, clinical neuroscience studies typically do not test for sex differences [2, 3]. For example, one systematic review of human neuroscience studies found that only 12% of studies included both sexes and considered sex as an experimental variable [1]. Third, until recently, no mandate required consideration of sex differences in federally funded research. Even after the NIH implemented its 2015 policy requiring consideration of sex as a biological variable (SABV) [20], a study conducted at a research-intensive university found that few studies submitted to the institutional review board in 2016 were designed to evaluate SABV, even though many of the studies were already funded [21].
Methods
Our scoping review aimed to identify peer-reviewed journal articles published before March 2020 and written in English that studied FDA-approved psychiatric medications in humans, used in vivo neuroimaging methodologies, and appropriately evaluated sex differences (defined as testing for an interaction involving sex or stratifying analyses by sex).
We conducted a PubMed search in March 2020 (for a list of the specific search terms, see Table S1 in supplemental materials). Our search targeted five classes of psychiatric medications: antidepressants, antipsychotics, mood stabilizers, sedative-hypnotics, and stimulants. Although we chose to focus on sex differences (biological factors) rather than gender differences (social factors), when conducting our literature search, we included both terms in our search because many researchers use them interchangeably. In line with the current recommendation for search strategy [8], we included ‘sex’ and ‘gender’ in addition to terms related to ‘sex differences’ and ‘gender differences’ to capture studies that investigated sex regardless of whether they found statistically significant differences. Our PubMed search yielded 1615 journal articles, which were imported into Covidence [22], an online tool that streamlines the process of screening journal articles.
We applied three tiers of criteria to determine whether studies should be included in the scoping review (see Figs. 1, 2). During title and abstract screening, studies were determined to be relevant if they met all Tier 1 criteria. We only included studies that used a study design that allowed researchers to test for associations between neural measures and drug effects (e.g., predicting drug responders and non-responders from neural measures at baseline, between-subjects designs comparing treatment and control groups on neural outcome measures, within-subjects designs identifying neural changes from baseline to after receiving treatment). Relevant studies were then assessed for eligibility during full-text review. We first considered whether publications met all Tier 2 criteria before assessing studies for Tier 3 criteria, which evaluated whether sex differences were appropriately evaluated.
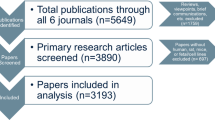
Studies identified through our search strategy (N = 1615) were subjected to title and abstract screening first. Studies that met all Tier 1 criteria (N = 350) underwent full text review. To meet Tier 2 criteria, studies had to include both sexes, use inferential statistics, and use an appropriate study design. For studies that met Tier 2 criteria (N = 251), we considered whether they appropriately tested for sex differences using Tier 3 criteria. Only 20% of studies that included both sexes and otherwise met criteria appropriately tested for sex differences (N = 50).
Using our search strategy, 1615 studies were identified and subjected to title and abstract screening. Of these studies, 350 were considered relevant and assessed for eligibility during full text review. Only 50 studies adequately tested for sex differences, met all other criteria, and therefore were included in our scoping review. Excluded studies either did not include both sexes, did not use a study design of interest, did not adequately test for sex differences, or tested for them but did not report their findings.
Results
Across 50 NPP studies that adequately tested for sex differences and reported their findings, 36 (72%) reported statistically significant sex differences on at least one outcome. In the following subsections organized by the five drug classes investigated herein—antidepressants, antipsychotics, mood stabilizers, sedative-hypnotics, and stimulants—we review the evidence for and against sex differences across multiple types of NPP studies: (1) studies that use baseline neural measures to predict treatment response (which we refer to as ‘biomarker studies’) (2) treatment studies that test the neural effects of the pharmacologic intervention in patients, (3) challenge studies that demonstrate the neural effects of the drug in healthy participants, and (4) adverse effect studies that identify neural underpinnings of treatment risk. Table 1 provides details on each study, such as the study design, the overall sample size, and the number of participants broken down by sex to contextualize the results.
Antidepressants (n = 16)
Females are twice as likely to suffer from depression as males [23]. The effectiveness of certain types of antidepressants may differ by sex. For example, females may respond better than males to selective serotonin reuptake inhibitors [SSRIs] whereas males may respond better to tricyclic antidepressants [TCAs] [16, 24]. Sex differences in the efficacy of different types of antidepressants may stem from sex differences in the underlying neural circuitry that is targeted by them [23, 25]. Overall, we found that 13 of 16 antidepressant studies meeting our review criteria reported statistically significant sex differences in at least one outcome.
Biomarker studies: neural predictors of antidepressant response (n = 7)
Frontal alpha asymmetry (n = 3)
Frontal alpha asymmetry refers to the difference in alpha activity over the left and right frontal brain regions [26]. Alpha waves are useful to measure because they are inversely related to cortical activation. Lower alpha activity (greater cortical activation) over the left versus right frontal region is thought to reflect a more positive emotional propensity and a more approach-oriented motivational tendency [26]. Three electroencephalography (EEG) studies showed that frontal alpha asymmetry at baseline predicted SSRI treatment response in a sex-dependent manner [27,28,29]. The first study measured alpha waves while participants rested with their eyes either open or closed [27]. At baseline, females who responded to SSRI treatment (compared to females who did not) showed greater activation (less alpha) over the left hemisphere during the eyes open condition. In males, alpha asymmetry did not predict treatment response. Two EEG studies measuring frontal alpha asymmetry replicated this finding [28, 29]. Both studies used the same large sample of patients with MDD and found that higher activity (less alpha) over the left frontal cortex at baseline [28] as well as after eight weeks of antidepressant treatment [29] predicted response to SSRIs (escitalopram and sertraline) in females but not in males. If baseline frontal brain asymmetry had been used to guide treatment selection in females, treatment response rates could have been improved by 7% for venlafaxine-XR and 14% for escitalopram and sertraline [28]. Importantly, when males and females were analyzed together, frontal alpha asymmetry did not predict response to treatment, obscuring a potentially critical biomarker for females.
Event-related potentials (n = 1)
Previous studies have shown that event-related potentials (ERPs)—changes in electrical activity in the brain resulting from a specific sensory event (such as a sound)—can predict response to antidepressant treatment (for a review, Olbrich & Arns [30]). Typically, such studies have not considered SABV. However, a recent study found that ERPs predicted treatment response for males but not females [31]. Compared to male non-responders, male responders to SNRI treatment (venlafaxine-XR) had larger N1 amplitudes (an ERP that is larger when a stimulus is unpredictable).
Serotonergic system (n = 1)
Given that the serotonin (5-HT1A) receptor has been implicated in depression [32], one PET-CT study used the 5-HT1A receptor antagonist radiotracer [18F]Mefway to test whether the density of 5-HT1A receptors could be used as a biomarker to predict treatment response to an SSRI (escitalopram) [33]. This study found that baseline density of serotonin receptors did not predict treatment outcomes regardless of sex.
Regional brain volumes (n = 2)
Recent meta-analyses consistently indicate an association between depression and reduced hippocampal volume [34,35,36]. Only two studies have considered whether SABV impacts the predictive value of baseline hippocampal volume on antidepressant response [37, 38]. In the first study, larger right hippocampal volume at baseline predicted responder status only in females [37]. The second study tested whether various regional brain volumes pre-treatment were predictive of response to antidepressant treatment (across a wide range of antidepressant types) in patients hospitalized for a depressive episode [38]. Multiple regional brain volumes interacted with sex (left hippocampal cluster × right hippocampal cluster × subcallosal/orbitofrontal cortex cluster × sex) to predict reductions in depression severity after five weeks of treatment [38].
Treatment studies: neural effects of antidepressants in patients (n = 6)
Regional brain volumes (n = 2)
In children and adults, antidepressant treatment can induce changes in regional brain volumes over time. Two studies that considered the impact of sex found mixed results [39, 40]. In a study of children with obsessive-compulsive disorder (OCD), thalamic volume decreased significantly after 12 weeks of paroxetine treatment such that post-treatment thalamic volume in children with OCD was similar to that of the healthy comparison group [39]. Reduction in thalamic volume was correlated with reduction in OCD symptoms although no sex differences were observed. By contrast, in a prospective study on a large cohort of older adults with depression, antidepressant use was associated with slower hippocampal volume loss in males but not females [40].
Neural activation and connectivity (n = 3)
Three EEG studies demonstrate that antidepressants affect neural activation and connectivity in a sex-dependent manner [41,42,43]. Two studies showed effects in males only [42, 43]. In a large study, male responders had decreased alpha connectivity between two brain regions (the subgenual anterior cingulate cortex and the dorsolateral/dorsomedial prefrontal cortex [dlPFC and dmPFC]) from baseline to eight weeks after starting antidepressant treatment, but female responders did not show this effect [42]. In another study, males that responded to either a serotonin reuptake enhancer (tianeptine) or an SSRI (paroxetine) demonstrated a sharp decline in the higher sigma frequency range during non-REM sleep from days 7 to 42 of treatment whereas non-responders did not show any change in this frequency range [43]. Finally, one study found that medications (antidepressants, antipsychotics, or both) affected various EEG measures in patients with depression, and these effects were modified by sex and age in complex ways [41].
Dopaminergic system (n = 1)
Bupropion, a primarily dopaminergic antidepressant, was studied using single-photon emission computed tomography (SPECT) to examine dopamine transporter availability in the striatum in depressed patients before and after treatment [44]. At baseline, depressed patients showed greater dopamine transporter availability in the bilateral striatum compared to healthy controls. After successful treatment with bupropion, dopamine transporter binding decreased in all subregions of the striatum in females, but only in the right caudate for males.
Challenge studies: neural effects of antidepressants in healthy participants (n = 2)
In healthy volunteers, positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) studies tested whether sex modified the effect of acute citalopram administration on brain glucose metabolism and neural activation, respectively [45, 46]. In the PET study, citalopram led to widespread increases in cortical glucose metabolism in females and a decrease in regional glucose metabolism in males compared to placebo [45]. The fMRI study, however, found no sex differences although citalopram affected activation in several regions involved in serotonergic neurotransmission in a dose-dependent manner [46].
Adverse effect studies: neural underpinnings of antidepressant risk (n = 1)
The risks of taking antidepressants differ for males and females. Bupropion hydrochloride increases the risk of seizures, particularly in females, who are at 1.5 times higher risk of seizures while taking bupropion than males [47]. In a large EEG study of patients taking bupropion, females were more than twice as likely as males to present with specific waveforms associated with seizure risk even after controlling for confounders such as dosage [48, 49].
Antipsychotics (n = 12)
Estrogen appears to influence the efficacy and side effects of antipsychotics [50, 51]. Although female patients with schizophrenia are more likely to experience symptom improvement with antipsychotic treatment across all symptom categories (positive, negative, depressive, and cognitive symptoms) [52], they are less likely to respond to antipsychotics in the hypogonadal state of post menopause [53]. Overall, 10 of 12 antipsychotic studies meeting our review criteria reported statistically significant sex differences in at least one outcome.
Biomarker studies: neural predictors of antipsychotic response (n = 4)
Regional brain volumes (n = 3)
Two studies identified brain region volumes that predicted antipsychotic treatment outcomes in a sex-dependent manner [54, 55]. In the first study, larger striato-thalamic volumes at baseline predicted remission after one year of treatment in female but not male patients with schizophrenia [54]. In the second study, cerebral third ventricle size was evaluated as a potential biomarker of antipsychotic response (lithium or haloperidol) [55] given that increased ventricle size at baseline has been associated with poorer treatment response in previous studies [48, 56]. Of all of the effects tested, one sex difference emerged: those who had a delayed response to haloperidol tended to have a larger cerebral third ventricle, and this effect was driven by males who had a substantially larger third ventricle area and width than females.
Not all studies that evaluated regional brain volumes as a biomarker of treatment response found sex to be a relevant moderator [57]. One study found that larger pituitary volume at baseline (which has been associated with HPA-axis hyperactivation) predicted less improvement of symptoms in first-episode psychosis patients after 12 weeks of treatment with quetiapine fumarate [57]. Although the effect was large, it was not dependent on sex.
EEG abnormalities (n = 1)
Minor EEG abnormalities at baseline predicted a favorable response to clozapine in a sex-dependent manner [58]. Female patients with abnormal EEGs had significantly greater improvement compared to female patients with normal EEGs [58]. EEG measures were not predictive of treatment response in male patients.
Treatment studies: neural effects of antipsychotics in patients
Regional brain volumes (n = 2)
Two magnetic resonance imaging (MRI) studies demonstrated sex-specific changes in basal ganglia volumes in patients with schizophrenia after treatment with either typical [59] or atypical antipsychotics [59, 60]. The first study found that basal ganglia volumes (specifically, the caudate nucleus, nucleus accumbens, and putamen volumes) increased after treatment [59]. One specific sex difference emerged: in the 11 patients receiving risperidone treatment, the nucleus accumbens volume increased in all but one of the eight male patients, but decreased in all three female patients [59]. The second study showed sex-dependent changes in caudate volume with exposure to atypical antipsychotics: higher exposure to atypical antipsychotics predicted greater enlargement of the caudate in males but the correlation was in the opposite direction for females [60].
Dopamine receptor binding (n = 1)
Previous studies have reported left lateralization of striatal D2 receptor (D2R) binding in males with schizophrenia [61, 62]. To test whether antipsychotics diminish this asymmetry, drug naïve hospitalized patients with schizophrenia were injected with [123I]iodobenzamide radio tracer 2 h before a baseline SPECT scan and then injected with the highly potent antipsychotic benperidol 20 min before a second SPECT scan in order to measure change in D2R binding [63]. At baseline, male patients were more likely to show a left-lateralized asymmetry of striatal D2R binding compared to female patients (6 of 11 males versus 3 of 12 females). After benperidol challenge, this left lateralization diminished in male patients (2 of 11 males) and remained the same in female patients (3 of 12 females) [63].
Myelin integrity (n = 1)
Diffusion tensor imaging (DTI) is a way of understanding the integrity of white-matter tracts—the neural connections critical for coordination between brain regions. High diffusivity, or free-diffusion of water in all directions, is a sign of poor white matter integrity and has been observed in DTI studies of patients with schizophrenia [64, 65]. One DTI study examined whether sex impacted change in diffusivity in patients treated with antipsychotics for 28 days [66]. Although treatment was associated with a significant reduction in diffusivity measured in multiple brain regions among those who responded to antipsychotic treatment, in this small sample, no sex differences emerged.
Neural activation (n = 2)
Typical and atypical antipsychotics affect neural activation in a sex-dependent way that could have clinical significance [67]. Using [18F]-2-fluoro-2-deoxy-D-glucose (FDG) PET, regional glucose metabolism was measured in male and female patients with schizophrenia before and after treatment with either a typical antipsychotic (fluphenazine) or an atypical antipsychotic (clozapine) [67]. Patients were compared to same-sex healthy controls. A sex by diagnosis interaction effect emerged with respect to cingulate metabolism, such that female patients receiving antipsychotic treatment had a significantly lower cingulate cortex metabolism (−9.1% and −11.4% on clozapine and fluphenazine, respectively) compared to female controls whereas male patients did not differ from male controls. In the basal ganglia, clozapine increased metabolic rates in the female patients (15%) to a greater extent than in the male patients (4%) relative to their same sex controls whereas fluphenazine increased metabolic rates to a similar extent in female (22%) and male (24%) patients. Both antipsychotics increased hippocampal metabolism in patients compared to healthy controls, with no sex differences observed.
In order to determine whether sex affects the neural mechanisms underlying treatment, a resting EEG study measured brain waves in patients with schizophrenia being treated with an atypical antipsychotic (either olanzapine or risperidone) [68]. Relative to male patients, female patients had decreased current density in delta frequency slow waves at the middle frontal gyrus [68].
Challenge studies: neural effects of antipsychotics in healthy participants (n = 2)
A recent review indicates that females with schizophrenia show better treatment outcomes for many antipsychotics [69]. Two EEG studies provide neural evidence in healthy adults suggesting that antipsychotic effects on sleep may contribute to greater symptom improvement among women compared to men [70, 71]. Whereas morning [70] and evening [71] doses of olanzapine increase slow-wave sleep in females, males showed either no effect or a decrease in slow-wave sleep [70, 71].
Mood stabilizers (n = 2)
Although overall prevalence rates of bipolar disorder do not differ between males and females [72], females may be at a higher risk of bipolar II disorder [73]. Furthermore, a meta-analysis provided evidence that the brains of males and females with bipolar disorder may differ in terms of structure and function at baseline [74]. Studies, however, have not reported substantial sex differences in response to pharmacologic treatment [73]. Overall, 1 of the 2 mood stabilizer studies meeting our review criteria reported statistically significant sex differences in at least one neuroimaging outcome.
Treatment studies: neural effects of mood stabilizers in patients (n = 1)
MRI studies have found that bipolar disorder is associated with abnormalities in amygdala volume, but these studies have not always adequately accounted for mood stabilizer exposure or current use (e.g., [75]). One study tested whether bipolar disorder was associated with differences in amygdala volume depending on whether patients took mood stabilizers (either lithium or divalproex) [76]. The medicated patients had larger right amygdala volumes than unmedicated patients, but no significant sex differences emerged in either group.
Challenge studies: neural effects of mood stabilizers in healthy participants (n = 1)
Mood stabilizers can affect the brain waves of healthy volunteers in a sex-dependent manner. Healthy volunteers underwent EEG before and after ten days of lithium carbonate administration [77]. Lithium led to power increases in the entire frequency range, and important sex differences emerged: lithium increased theta and beta power to a greater extent in females compared to males, and the topographic distribution varied by sex as well.
Sedative-hypnotics (n = 10)
Females are prescribed benzodiazepines about twice as frequently as males, and some evidence even suggests that benzodiazepines exert a more potent effect on females compared to males at the same dose [15]. Zolpidem, a non-benzodiazepine hypnotic, was the first drug for which the FDA recommended sex-based dosing, halving its recommended dosing to 5 mg for females after adverse reports consistently indicated higher next-morning sedation in females taking 10 mg [18]. Overall, 6 of 10 sedative-hypnotic studies meeting our review criteria reported statistically significant sex differences in at least one outcome.
Treatment studies: neural effects of sedative-hypnotics in patients (n = 2)
Two studies investigated whether long-term benzodiazepine use changes brain structure and whether sex modifies these effects [78, 79]. In the first study, the ventricle area to brain area ratio (VBR) was measured using computed tomography (CT) scans in a group of long-term benzodiazepine users [78]. In the benzodiazepine group, the VBR was larger in males compared to females. A second study did not completely replicate these findings [79]. A negative but non-significant correlation was found between VBR and sex among benzodiazepine users, but it was unclear whether this finding was in the same direction as the first study or not.
Challenge studies: neural effects of sedative-hypnotics in healthy participants (n = 8)
In healthy volunteers, two challenge studies provided evidence that diazepam decreases brain activation to a greater extent in females compared to males [80, 81]. In an EEG study, females had a sharper decline in cortical activation than males 11 h after taking a 10 mg dose of diazepam [80]. In an fMRI study, female participants administered 10 mg of diazepam demonstrated worse behavioral performance on a cognitive task and lower activation in the PFC compared to their male counterparts [81]. These two studies suggest that the same dose of diazepam impairs females more than males. A third study using waking EEG revealed expected changes in the coupling of high frequencies between hemispheres with acute diazepam administration in healthy participants. Although this effect occurred regardless of sex, relative power was more impacted in women while coherent activity between hemispheres was more affected in males [82].
While diazepam studies revealed sex differences, one study using another type of benzodiazepine, lorazepam, did not. In this PET imaging [18F]FDG study, lorazepam consistently decreased whole-brain metabolism and impaired cognitive and motor performance relative to placebo, but no sex differences were revealed [83].
Among healthy volunteers administered sedative-hypnotics, sex differences in neuroimaging outcomes are mixed [84,85,86,87,88]. In a randomized, double-blinded, placebo-controlled trial, the effects of hypnotics (10 mg of zolpidem and 5, 10, and 15 mg of gaboxadol) on EEG power spectra during sleep differed by sex [85]. At 10 mg of zolpidem, females had greater increases in sleep spindle activity in non-rapid eye movement (non-REM) sleep than males. At 10 and 15 mg of gaboxadol, females experienced greater increases in delta and theta activity during both non-REM and REM sleep. In another EEG study, gaboxadol (10 and 15 mg) induced a dose-related increase in low frequencies during sleep, and these effects were greater in females than males [86].
Two EEG studies, however, did not show sex differences [87, 88]. In these studies, beta amplitudes (an index of drowsiness) were measured by averaging over the left and right frontotemporal leads at baseline and 8 h after taking either zolpidem [87] or triazolam [87, 88]. Both medications produced increases in beta amplitude, which is in line with research showing that beta is enhanced during drowsiness and that sedating drugs increase beta amplitude [89]. No sex differences in beta amplitude were observed for either medication. In addition, the second study focused on interaction effects of age and sex and reported that age was not associated with differences in beta amplitude between the triazolam and placebo conditions in either males or females [88].
Stimulants (n = 10)
In epidemiologic studies, ADHD in childhood is twice as prevalent in males than in females, although sex differences in clinical symptom presentation lead to less frequent and later detection among females [90]. ADHD presents differently at a neural level in males and females in children [91] as well as in adults [92]. This may have important implications for the way that stimulants act in the CNS. Overall, 6 of 10 stimulant studies meeting our review criteria reported statistically significant sex differences in at least one outcome.
Treatment studies: neural effects of stimulants in patients (n = 1)
In a large longitudinal study, regional brain volume changes were tracked over time in children with ADHD [93]. Children with ADHD who were medicated were compared to those who were not. Although no significant sex differences emerged, medicated children with ADHD as well as healthy controls had larger total white matter volumes than unmedicated children with ADHD.
Challenge studies: neural effects of stimulants in healthy participants (n = 9)
Changes in neural activation (n = 1)
Methylphenidate inhibits the uptake of dopamine and norepinephrine, increasing levels of both neurotransmitters in the PFC. In a [18F]FDG PET study, an acute dose of methylphenidate was given to cannabis abusers and healthy controls, and sex interacted with group (cannabis abusers vs. healthy controls) to predict change in regional brain glucose metabolism in exploratory analyses [94]. Although male cannabis abusers and male controls did not differ, female cannabis abusers exhibited blunted methylphenidate-induced response across multiple brain regions compared to female controls.
Dopaminergic system (n = 8)
Two PET studies using [11C]raclopride to measure striatal dopamine binding potential and dopamine release reported sex differences in amphetamine-induced dopamine release in striatal and extra-striatal regions [95, 96]. Whereas males tended to show higher dopamine release in striatal regions such as the ventral striatum [95], females exhibited higher dopamine release in the right globus pallidus and the right inferior frontal gyrus [96]. A follow-up study [97] using the same data [96] revealed that in males, but not females, amphetamine-induced dopamine release correlated with cognitive and affective measures. In a [18F]fallypride PET study, amphetamine challenge led to significantly higher dopamine release relative to placebo [98]. A significant three-way interaction emerged for drug (amphetamine vs. placebo), age group (aged 2–30 vs. aged 50–65), and sex, such that young adult males had greater amphetamine-induced dopamine release in the bilateral ventral striatum and right putamen compared to young adult females. No sex differences were found for these brain regions in middle-aged participants.
Smoking is associated with impaired dopamine response to an amphetamine challenge in a sex-dependent manner [99]. A [11C]FLB457 PET study measured dopamine D2R availability at baseline and 3 h after amphetamine administration in smokers and non-smokers. Female smokers showed significantly lower amphetamine-induced dopamine release in the dlPFC than male smokers and female non-smokers. In addition, male smokers had lower dlPFC D2R availability than male nonsmokers, but female smokers and non-smokers did not differ.
Early life adversity can impact dopaminergic functioning [100, 101]. A PET study using [18F]FDG found that a history of childhood adversity is positively associated with ventral striatal dopamine response to an amphetamine challenge [102]. However, sex was not a relevant moderator. In a subsequent PET study using the same methods, higher amphetamine-induced dopamine release in the ventral striatum was associated with less advantageous decision-making in healthy adults [103]. This effect did not differ by sex either.
Amphetamine challenge induces an abnormally large stimulation of D2R transmission in patients with schizophrenia [104, 105]. In order to test for the effect of sex and antipsychotic use on amphetamine-induced dopamine transmission, [123I]IBZM SPECT scans were conducted before and after an amphetamine challenge in patients with schizophrenia and healthy controls [106]. Patients with schizophrenia exhibited excessive stimulation of dopamine transmission compared to control participants, and this was associated with a worsening of positive symptoms. However, no sex by diagnosis interaction was observed.
Discussion
Our scoping review had three main goals: to evaluate how many studies adequately tested for sex differences, to determine the frequency with which significant sex differences were found, and to map the literature on sex differences in NPP studies of psychiatric drugs.
In our scoping review, 251 of the 350 studies evaluated during full-text review met our initial criteria: they were pharmacologic studies that included both sexes and, to some extent, considered that sex could impact the results. Unfortunately, 80% of these 251 studies used methodologies that effectively eliminated the effect of sex (e.g., by including sex as a covariate), obscuring potential sex differences. Only 20% of these studies used appropriate statistical methods to test for sex differences (see Fig. 3).
The larger pie chart is based on 251 studies that included both sexes and considered that sex could impact the results. However, 80% of studies used methodologies that essentially eliminated the effect of sex (e.g., by controlling for sex as covariate), whereas 20% of studies appropriately evaluated sex differences (by either testing for an interaction involving sex or stratifying the analysis by sex). The smaller pie chart is based on the 50 studies that appropriately evaluated sex differences. Of these, 36 found at least one sex difference whereas 14 did not.
We examined whether sex affects findings from NPP studies, specifically those examining the relationship between neural measures and drugs used to treat psychiatric disorders. Across five classes of psychiatric drugs and a wide variety of study designs, 72% of studies that evaluated sex differences reported significant findings, demonstrating that sex can impact (1) the way that psychiatric drugs affect the brain and (2) the extent to which neural biomarkers predict drug treatment response. The majority of NPP studies focusing on antidepressants, antipsychotics, sedative-hypnotics, and stimulants found sex differences. Only two mood stabilizer studies evaluated SABV, with more studies considering sex in the other drug classes, likely due to known sex differences in the disorders they treat. In contrast, substantial sex differences in mood stabilizer response have not been observed in bipolar patients [73].
Sex differences may be particularly important to consider when predicting antidepressant response from frontal asymmetry and hippocampal volume. In female patients with depression, greater cortical activation over the left hemisphere predicted successful treatment response to SSRIs, a finding that replicated in two separate datasets across three published studies [27,28,29]. Because this biomarker was not a significant predictor of treatment response in males, when findings were aggregated across sex, this obscured an important biomarker for females. EEG is inexpensive relative to most neuroscience techniques but could be used clinically to inform choice of drug administration in females.
A recent meta-analysis revealed that smaller baseline hippocampal volume predicted lower antidepressant response rates in depressed patients [107]. The study in our scoping review found this effect only in female responders [37]. Even though this study was included in the meta-analysis, the meta-analysis used weak methodologies to conclude that sex did not impact the effect. In fact, the meta-analysis only tested whether the percentage of females in the study was associated with the response or remission rate of antidepressant treatment and did not actually test whether sex moderated the effect of hippocampal volume on antidepressant response. Future research on this topic should test for sex differences.
Antipsychotics have differential sex effects in both patients with schizophrenia and healthy participants. In patients, two studies suggested that antipsychotics may be more likely to increase basal ganglia volumes in males [59, 60]. In healthy participants, olanzapine increased slow-wave sleep in females but not males across two studies [70, 71]. Although these sex differences remain to be tested in patients with schizophrenia, greater slow-wave sleep is associated with better cognitive performance in patients with schizophrenia [108] so these findings may help explain why females taking olanzapine show a better response to treatment [109].
Only two studies considered the impact of SABV on mood stabilizer neural effects [76, 77], and one of the studies revealed sex differences in healthy participants administered lithium for ten days, suggesting that lithium may act differentially on the brains of males and females. Therefore, even though males and females do not differ in bipolar prevalence or mood stabilizer response [73], mood stabilizers may still affect male and female brains differently.
Two studies in healthy participants showed that diazepam decreased brain activation and increased cognitive impairment to a greater extent in females compared to males [80, 81]. Like zolpidem, the same dose of diazepam impairs females more than males. While GABAA receptor binding sites differ between benzodiazepines and non-benzodiazepine sedatives, this finding is in concert with the observation that women have greater sedation with zolpidem, further emphasizing that sex must be taken into consideration when developing GABAA receptor agonist medications.
The vast majority of stimulant studies (8 of 10) were PET studies using amphetamine challenge to measure dopamine release. Studies on patient samples revealed intriguing sex differences that may explain sex differences to certain addictions. In response to an amphetamine challenge, female cannabis abusers and smokers showed lower glucose metabolism across multiple brain regions and blunted dopamine release in the dlPFC, respectively [94, 99]. Blunted dopamine transmission increases addiction risk and relapse [110], suggesting that female smokers and cannabis abusers may be at greater risk of relapse during periods of abstinence.
Limitations
Our scoping review has three limitations that are important to highlight. The first limitation is that we only included studies in our scoping review that clearly stated in the abstract that the purpose of the study was to test for associations between neural measures and psychiatric drug effects. Therefore, we would have inadvertently excluded studies that did test for these associations if this was not mentioned in the abstract.
The second limitation is that the evidence included in our scoping review may unintentionally overrepresent studies in which researchers found significant sex differences given that significant findings are more likely to be reported and published than null results. Such biases have been found in neuroimaging research. For example, one meta-analysis of human fMRI studies indicated that reporting and publishing biases led to an excess of significant findings being published, such that 88% of studies evaluating sex differences reported significant effects in the abstract [111]. In this meta-analysis, one key piece of evidence pointed to a selective reporting bias rather than a high prevalence of real sex differences. Studies with larger sample sizes should be more likely to detect sex differences (when real sex differences are present). However, such a relationship was absent, suggesting that the high prevalence of significant sex differences may reflect a selective reporting bias instead.
A third limitation is that we did not assess whether studies were adequately powered to evaluate sex differences. Importantly, interaction effects require a larger sample size to ensure adequate power than stratified analyses. This difference in power affects whether sex differences are detected. For example, a systematic review of substance abuse-related MRI studies found that 81% of studies that stratified analyses by sex identified a significant sex difference compared to only 31% of studies that tested for interaction effects involving sex [2]. Many findings reported in this review had small sample sizes (see Table 1). This can lead to two problematic situations, simultaneously increasing the likelihood of false negatives and false positives [112]. Alarmingly, one review estimated the median statistical power in neuroscience studies to be between 8–31% [112]. Therefore, null results may reflect a study being underpowered rather than the absence of a sex difference, but significant findings may be in excess due to a combination of low power as well as biases in reporting and publishing [8, 113]. This makes it difficult to draw firm conclusions from this scoping review. Only when we have sufficiently powered studies to detect true sex differences (when they exist) and researchers are encouraged to publish whether they found sex differences (regardless of outcome) will we be confident in the scientific literature regarding whether sex differences are highly prevalent, relatively rare, or somewhere in between.
Conclusions
Although some debate remains on whether sex differences in the brain are indeed prevalent and important [8, 113], our findings emphasize that in the context of psychiatric drugs, the potential impact of sex on outcomes of interest should be evaluated to enhance the rigor and reproducibility of NPP research. Across multiple imaging modalities and classes of psychiatric drugs, sex-based differences in the association between neural measures and drug effects were common in studies that used appropriate statistical methods to test for them. For the vast majority of significant sex differences reported in this review, no apparent replication attempts have been made. In our entire scoping review, we identified only four replication attempts: three findings replicated, and one did not (see Table 2). While this scoping review does not provide clear answers, it is a call to action. Nearly the entire field of sex differences in NPP is wide open for discovery. Even though pharmacologic interventions are often used to treat psychiatric disorders with broadly recognized sex differences [9] and the field of psychiatry is aiming for individualized medicine [114], 80% of NPP studies in this systematic review did not analyze and/or report on the impact of sex. While the benefits of evaluating the role of sex are considerable (e.g., improving the predictive value of biomarkers, guiding the development of more targeted pharmacologic treatments, enhancing the reproducibility of results), the consequences of ignoring the role of sex may be even more substantial and could cause significant harm either through adverse effects or lack of access to a potentially effective treatment [115, 116]. Thus, we urge scientific journals, peer reviewers, granting agencies, and regulatory agencies (such as institutional review boards) to follow the NIH’s example and require consideration of SABV [18, 20, 117]. Doing so will be critical in driving medicine towards greater equity and biomedical research towards greater rigor and reproducibility.
References
Mamlouk GM, Dorris DM, Barrett LR, Meitzen J. Sex bias and omission in neuroscience research is influenced by research model and journal, but not reported NIH funding. Front Neuroendocrinol. 2020;57:100835.
Lind KE, Gutierrez EJ, Yamamoto DJ, Regner MF, McKee SA, Tanabe J. Sex disparities in substance abuse research: Evaluating 23 years of structural neuroimaging studies. Drug Alcohol Depend. 2017;173:92–6.
Moningka H, Lichenstein S, Worhunsky PD, DeVito EE, Scheinost D, Yip SW. Can neuroimaging help combat the opioid epidemic? A systematic review of clinical and pharmacological challenge fMRI studies with recommendations for future research. Neuropsychopharmacology. 2019;44:259–73.
Cahill L. Why sex matters for neuroscience. Nat Rev Neurosci. 2006;7:477–84.
Ritchie SJ, Cox SR, Shen X, Lombardo MV, Reus LM, Alloza C, et al. Sex differences in the adult human brain: Evidence from 5216 UK biobank participants. Cereb Cortex. 2018;28:2959–75.
Luders E, Gaser C, Narr KL, Toga AW. Why sex matters: brain size independent differences in gray matter distributions between men and women. J Neurosci. 2009;29:14265–70.
Cahill L. His brain, her brain. Sci Am. 2005;292:40–7.
Eliot L, Ahmed A, Khan H, Patel J. Dump the “dimorphism”: Comprehensive synthesis of human brain studies reveals few male-female differences beyond size. Neurosci Biobehav Rev. 2021;125:667–97.
Kaczkurkin AN, Raznahan A, Satterthwaite TD. Sex differences in the developing brain: Insights from multimodal neuroimaging. Neuropsychopharmacol. 2019;44:71–85.
Zhong W, Maradit-Kremers H, St Sauver JL, Yawn BP, Ebbert JO, Roger VL, et al. Age and sex patterns of drug prescribing in a defined American population. Mayo Clin Proc. 2013;88:697–707.
Safer DJ. Recent trends in stimulant usage. J Atten Disord. 2016;20:471–7.
Sundbom LT, Bingefors K, Hedborg K, Isacson D. Are men under-treated and women over-treated with antidepressants? Findings from a cross-sectional survey in Sweden. BJPsych Bull. 2017;41:145–50.
Smith MC. Small comfort: history of minor tranquilizers. 1st ed. New York: Praeger; 1985.
Moore TJ, Mattison DR. Adult utilization of psychiatric drugs and differences by sex, age, and race. JAMA Intern Med. 2017;177:274–5.
Donoghue J, Lader M. Usage of benzodiazepines: a review. Int J Psychiatry Clin Pract. 2010;14:78–87.
Sramek J, Murphy M, Cutler N. Sex differences in the psychopharmacological treatment of depression. Dialogues Clin Neurosci. 2016;18:447–57.
Lange B, Mueller JK, Leweke FM, Bumb JM. How gender affects the pharmacotherapeutic approach to treating psychosis—a systematic review. Expert Opin Pharmacother. 2017;18:351–62.
Mazure CM, Jones DP. Twenty years and still counting: including women as participants and studying sex and gender in biomedical research. BMC Women’s Health. 2015;15:1–16.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
National Institutes of Health. Consideration of sex as a biological variable in NIH-funded research. 2015. Available from: https://orwh.od.nih.gov/sites/orwh/files/docs/NOT-OD-15-102_Guidance.pdf.
Freeman A, Stanko P, Berkowitz LN, Parnell N, Zuppe A, Bale TL, et al. Inclusion of sex and gender in biomedical research: Survey of clinical research proposed at the University of Pennsylvania. Biol Sex Differ. 2017;8:1–8.
Health Innovations. Covidence Systematic Review Software. Melbourne, Australia. Available from: www.covidence.org.
LeGates TA, Kvarta MD, Thompson SM. Sex differences in antidepressant efficacy. Neuropsychopharmacology 2019;44:140–54.
Khan A, Brodhead AE, Schwartz KA, Kolts RL, Brown WA. Sex differences in antidepressant response in recent antidepressant clinical trials. J Clin Psychopharmacol. 2005;25:318–24.
Williams AV, Trainor BC. The impact of sex as a biological variable in the search for novel antidepressants. Front Endocrinol (Lausanne). 2018;50:107–17.
Smith EE, Reznik SJ, Stewart JL, Allen JJB. Assessing and conceptualizing frontal EEG asymmetry: An updated primer on recording, processing, analyzing, and interpreting frontal alpha asymmetry. Int J Psychophysiol. 2017;111:98–114.
Bruder GE, Stewart JW, Tenke CE, McGrath PJ, Leite P, Bhattacharya N, et al. Electroencephalographic and perceptual asymmetry differences between responders and nonresponders to an SSRI antidepressant. Biol Psychiatry. 2001;49:416–25.
Arns M, Bruder G, Hegerl U, Spooner C, Palmer DM, Etkin A, et al. EEG alpha asymmetry as a gender-specific predictor of outcome to acute treatment with different antidepressant medications in the randomized iSPOT-D study. Clin Neurophysiol. 2016;127:509–19.
van der Vinne N, Vollebregt MA, van Putten MJAM, Arns M. Stability of frontal alpha asymmetry in depressed patients during antidepressant treatment. NeuroImage Clin. 2019;24:102056.
Olbrich S, Arns M. EEG biomarkers in major depressive disorder: discriminative power and prediction of treatment response. Int Rev Psychiatry. 2013;25:604–18.
van Dinteren R, Arns M, Kenemans L, Jongsma MLA, Kessels RPC, Fitzgerald P, et al. Utility of event-related potentials in predicting antidepressant treatment response: An iSPOT-D report. Eur Neuropsychopharmacol. 2015;25:1981–90.
Kaufman J, DeLorenzo C, Choudhury S, Parsey RV. The 5-HT1A receptor in major depressive disorder. Eur Neuropsychopharmacol. 2016;26:397–410.
Barth M, Dunzinger A, Wimmer I, Winkler J, Rittmannsberger H, Nader M, et al. Serotonin 1A receptor density measured by F18-Mefway PET/CT in mesiotemporal cortex and raphe does not discriminate therapeutic response in patients with major depressive episode. Q J Nucl Med Mol Imaging. 2018;64:203–10.
Wise T, Radua J, Via E, Cardoner N, Abe O, Adams TM, et al. Common and distinct patterns of grey-matter volume alteration in major depression and bipolar disorder: evidence from voxel-based meta-analysis. Mol Psychiatry. 2017;22:1455–63.
Schmaal L, Veltman DJ, Van Erp TGM, Smann PG, Frodl T, Jahanshad N, et al. Subcortical brain alterations in major depressive disorder: findings from the ENIGMA Major Depressive Disorder working group. Mol Psychiatry. 2016;21:806–12.
Santos MAO, Bezerra LS, Carvalho ARMR, Brainer-Lima AM. Global hippocampal atrophy in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Trends Psychiatry Psychother. 2018;40:369–78.
Vakili K, Pillay SS, Lafer B, Fava M, Renshaw PF, Bonello-Cintron CM, et al. Hippocampal volume in primary unipolar major depression: a magnetic resonance imaging study. Biol Psychiatry 2000;47:1087–90.
Sämann PG, Höhn D, Chechko N, Kloiber S, Lucae S, Ising M, et al. Prediction of antidepressant treatment response from gray matter volume across diagnostic categories. Eur Neuropsychopharmacol. 2013;23:1503–15.
Gilbert AR, Moore GJ, Keshavan MS, Paulson LAD, Narula V, Mac Master FP, et al. Decrease in thalamic volumes of pediatric patients with obsessive-compulsive disorder who are taking paroxetine. Arch Gen Psychiatry. 2000;57:449–56.
Elbejjani M, Fuhrer R, Abrahamowicz M, Mazoyer B, Crivello F, Tzourio C, et al. Depression, depressive symptoms, and rate of hippocampal atrophy in a longitudinal cohort of older men and women. Psychol Med. 2015;45:1931–44.
Shagass C, Roemer RA, Josiassen RC. Some quantitative EEG findings in unmedicated and medicated major depressives. Neuropsychobiology 1988;19:169–75.
Iseger TA, Korgaonkar MS, Kenemans JL, Grieve SM, Baeken C, Fitzgerald PB, et al. EEG connectivity between the subgenual anterior cingulate and prefrontal cortices in response to antidepressant medication. Eur Neuropsychopharmacol. 2017;27:301–12.
Murck H, Nickel T, Künzel H, Antonijevic IA, Schill J, Zobel A, et al. State markers of depression in sleep EEG: Dependency on drug and gender in patients treated with tianeptine orparoxetine. Neuropsychopharmacology 2003;28:348–58.
Hsiao M-C, Lin K-J, Liu C-Y, Beck Schatz D. The interaction between dopamine transporter function, gender differences, and possible laterality in depression. Psychiatry Res—Neuroimaging. 2013;211:72–7.
Munro CA, Workman CI, Kramer E, Hermann C, Ma Y, Dhawan V, et al. Serotonin modulation of cerebral glucose metabolism: sex and age effects. Synapse. 2012;66:955–64.
Edes AE, McKie S, Szabo E, Kokonyei G, Pap D, Zsombok T, et al. Spatiotemporal brain activation pattern following acute citalopram challenge is dose dependent and associated with neuroticism: a human phMRI study. Neuropharmacology 2019;170:107807.
Davidson J. Seizures and bupropion: a review. J Clin Psychiatry. 1989;50:256–61.
Smith RC, Baumgartner R, Ravichandran GK, Mauldin M, Burd A, Vroulis G, et al. Lateral ventricular enlargement and clinical response in schizophrenia. Psychiatry Res. 1985;14:241–53.
Macaluso M, Zackula R, D'Empaire I, Baker B, Liow K, & Preskorn SH. Twenty percent of a representative sample of patients taking bupropion have abnormal, asymptomatic electroencephalographic findings. J Clin Psychopharmacol. 2010;30:312–7.
Gogos A, Ney LJ, Seymour N, Van Rheenen TE, Felmingham KL. Sex differences in schizophrenia, bipolar disorder, and post-traumatic stress disorder: are gonadal hormones the link? Br J Pharmacol. 2019;176:4119–35.
Lindamer LA, Buse DC, Lohr JB, Jeste DV. Hormone replacement therapy in postmenopausal women with schizophrenia: Positive effect on negative symptoms? Biol Psychiatry. 2001;49:47–51.
Usall J, Suarez D, Haro JM. the SOHO Study Group. Gender differences in response to antipsychotic treatment in outpatients with schizophrenia. Psychiatry Res. 2007;153:225–31.
González-Rodríguez A, Catalán R, Penadés R, Ruiz Cortés V, Torra M, Seeman MV, et al. Antipsychotic response worsens with postmenopausal duration in women with schizophrenia. J Clin Psychopharmacol. 2016;36:580–7.
Fung G, Cheung C, Chen E, Lam C, Chiu C, Law C, et al. MRI predicts remission at 1 year in first-episode schizophrenia in females with larger striato-thalamic volumes. Neuropsychobiology. 2014;69:243–8.
Kaplan MJ, Lazoff M, Kelly K, Lukin R, Garver DL. Enlargement of cerebral third ventricle in psychotic patients with delayed response to neuroleptics. Biol Psychiatry. 1990;27:205–14.
Weinberger DR, Bigelow LB, Kleinman JE, Klein ST, Rosenblatt JE, Wyatt RJ. Cerebral ventricular enlargement in chronic schizophrenia: An association with poor response to treatment. Arch Gen Psychiatry. 1980;37:11–3.
Garner B, Berger GE, Nicolo JP, Mackinnon A, Wood SJ, Pariante CM, et al. Pituitary volume and early treatment response in drug-naïve first-episode psychosis patients. Schizophr Res. 2009;113:65–71.
Pillay SS, Stoll AL, Weiss MK, Tohen M, Zarate CA, Banov MD, et al. EEG abnormalities before clozapine therapy predict a good clinical response to clozapine. Ann Clin Psychiatry. 1996;8:1–5.
Glenthoj A, Glenthoj BY, Mackeprang T, Pagsberg AK, Hemmingsen RP, Jernigan TL, et al. Basal ganglia volumes in drug-naive first-episode schizophrenia patients before and after short-term treatment with either a typical or an atypical antipsychotic drug. Psychiatry Res—Neuroimaging. 2007;154:199–208.
Heitmiller DR, Nopoulos PC, Andreasen NC. Changes in caudate volume after exposure to atypical neuroleptics in patients with schizophrenia may be sex-dependent. Schizophr Res. 2004;66:137–42.
Pilowsky LS, Costa DC, Ell PJ. Verhoeff NPLG, Murray RM, Kerwin RW. D2 dopamine receptor binding in the basal ganglia of antipsychotic-free schizophrenic patients: An 123I-IBZM single photon emission computerised tomography study. Br J Psychiatry. 1994;164:16–26.
Acton PD, Pilowsky LS, Costa DC, Ell PJ. Multivariate cluster analysis of dynamic iodine-123 iodobenzamide SPET dopamine D2 receptor images in schizophrenia. Eur J Nucl Med. 1997;24:111–8.
Schröder J, Bubeck B, Silvestri S, Demisch S, Sauer H. Gender differences in D2 dopamine receptor binding in drug-naive patients with schizophrenia: an [123I]iodobenzamide single photon emission computed tomography study. Psychiatry Res - Neuroimaging. 1997;75:115–23.
Burns J, Job D, Bastin ME, Whalley H, Macgillivray T, Johnstone EC, et al. Structural disconnectivity in schizophrenia: A diffusion tensor magnetic resonance imaging study. Br J Psychiatry. 2003;182:439–43.
Lim KO, Hedehus M, Moseley M, de Crespigny A, Sullivan EV, Pfefferbaum A. Compromised white matter tract integrity in schizophrenia inferred from diffusion tensor imaging. Arch Gen Psychiatry. 1999;56:367–74.
Garver DL, Holcomb JA, Christensen JD. Compromised myelin integrity during psychosis with repair during remission in drug-responding schizophrenia. Int J Neuropsychopharmacol. 2008;11:49–61.
Cohen RM, Nordahl TE, Semple WE, Pickar D. The brain metabolic patterns of clozapine- and fluphenazine-treated female patients with schizophrenia: Evidence of a sex effect. Neuropsychopharmacology 1999;21:632–40.
Eugene A, Masiak J, Kapica J, Masiak M. Electrophysiological neuroimaging using sLORETA comparing 22 age matched male and female schizophrenia patients. Hosp Chron. 2015;10:91–8.
Fernando P, Sommer IEC, Hasan A. Do we need sex-oriented clinical practice guidelines for the treatment of schizophrenia? Curr Opin Psychiatry. 2020;33:192–9.
Gimenez S, Sergio R, Gich I, Clos S, Grasa E, Rosa-Maria A, et al. Sex differences in sleep after a single oral morning dose of olanzapine in healthy volunteers. Hum Psychopharmacol. 2011;26:498–507.
Lindberg N, Virkkunen M, Tani P, Appelberg B, Virkkala J, Rimón R, et al. Effect of a single-dose of olanzapine on sleep in healthy females and males. Int Clin Psychopharmacol. 2002;17:177–84.
Flores-Ramos M, Leff P, Fernández-Guasti A, Becerra Palars C. Is it important to consider the sex of the patient when using lithium or valproate to treat the bipolar disorder? Pharm Biochem Behav. 2017;152:105–11.
Diflorio A, Jones I. Is sex important? Gender differences in bipolar disorder. Int Rev Psychiatry. 2010;22:437–52.
Jogia J, Dima D, Frangou S. Sex differences in bipolar disorder: a review of neuroimaging findings and new evidence. Bipolar Disord. 2012;14:461–71.
Velakoulis D, Wood SJ, Wong MTH, McGorry PD, Yung A, Phillips L, et al. Hippocampal and amygdala volumes according to psychosis stage and diagnosis. Arch Gen Psychiatry. 2006;63:139–49.
Savitz J, Nugent AC, Bogers W, Liu A, Sills R, Luckenbaugh DA, et al. Amygdala volume in depressed patients with bipolar disorder assessed using high resolution 3T MRI: the impact of medication. Neuroimage.2010;49:2966–76.
Thau K, Rappelsberger P, Lovrek A, Petsche H, Simhandl C, Topitz A. Effect of lithium on the EEG of healthy males and females: a probability mapping study. Neuropsychobiology. 1988;20:158–63.
Lader M, Ron M, Petursson H. Computerized axial brain tomography in long-term benzodiazepine users. Psychol Med. 1984;14:203–6.
Perera K, Powell T, Jenner F. Computerized axial tomographic studies following long-term use of benzodiazepines. Psychol Med. 1987;17:775–7.
Sierra JC, Luna-Villegas G, Buela-Casal G, Fernández-Guardiola A. The assessment of residual effects of a single dose of diazepam on visually-defined EEG patterns. J Psychopharmacol. 1997;11:367–72.
Muñoz-Torres Z, Armony JL, Trejo-Martínez D, Conde R, Corsi-Cabrera M. Prefrontal activity decline in women under a single dose of diazepam during rule-guided responses: An fMRI study. Exp Brain Res. 2016;234:3483–95.
Romano-Torres M, Borja-Lascurain E, Chao-Rebolledo C, Del-Río-Portilla Y, Corsi-Cabrera M. Effect of diazepam on EEG power and coherent activity: sex differences. Psychoneuroendocrinology. 2002;27:821–33.
Wang G-J, Volkow ND, Fowler JS, Hitzemann RJ, Pappas NR, Netusil N. Evaluation of gender difference in regional brain metabolic responses to lorazepam. Psychiatry Res—Neuroimaging. 1998;82:37–46.
Lankford DA, Corser BC, Zheng Y-P, Li Z, Snavely DB, Lines CR, et al. Effect of gaboxadol on sleep in adult and elderly patients with primary insomnia: Results from two randomized, placebo-controlled, 30-night polysomnography studies. Sleep. 2008;31:1359–70.
Dijk DJ, James LM, Peters S, Walsh JK, Deacon S. Sex differences and the effect of gaboxadol and zolpidem on EEG power spectra in NREM and REM sleep. J Psychopharmacol. 2010;24:1613–8.
Ma J, Dijk D-J, Svetnik V, Tymofyeyev Y, Ray S, Walsh JK, et al. EEG power spectra response to a 4-h phase advance and gaboxadol treatment in 822 men and women. J Clin Sleep Med. 2011;7:493–501.
Greenblatt DJ, Harmatz JS, Von Moltke LL, Wright CE, Durol ALB, Harrel-Joseph LM, et al. Comparative kinetics and response to the benzodiazepine agonists triazolam and zolpidem: evaluation of sex-dependent differences. J Pharm Exp Ther. 2000;293:435–43.
Greenblatt DJ, Harmatz JS, Von Moltke LL, Wright CE, Shader RI. Age and gender effects on the pharmacokinetics and pharmacodynamics of triazolam, a cytochrome P450 3A substrate. Clin Pharm Ther. 2004;76:467–79.
St. Louis E, Frey L, editors. Electroencephalography (EEG): an introductory text and atlas of normal and abnormal findings in adults, children, and infants. Chicago, IL: American Epilepsy Society; 2016.
Hermens DF, Cooper NJ, Kohn M, Clarke S, Gordon E. Predicting stimulant medication response in ADHD: Evidence from an integrated profile of neuropsychological, psychophysiological, and clinical factors. J Integr Neurosci. 2005;4:107–21.
Poissant H, Rapin L, Chenail S, Mendrek A. Forethought in youth with attention deficit/hyperactivity disorder: an fMRI study of sex-specific differences. Psychiatry J. 2016;2016:1–8.
Endres D, Van Elst LT, Maier SJ, Feige B, Goll P, Meyer SA, et al. Neurochemical sex differences in adult ADHD patients: an MRS study. Biol Sex Differ. 2019;10:1–11.
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, et al. Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. J Am Med Assoc. 2002;288:1740–8.
Wiers CE, Shokri-Kojori E, Wong CT, Abi-Dargham A, Demiral ŞB, Tomasi D, et al. Cannabis abusers show hypofrontality and blunted brain responses to a stimulant challenge in females but not in males. Neuropsychopharmacology. 2016;41:2596–605.
Munro CA, McCaul ME, Wong DF, Oswald LM, Zhou Y, Brasic J, et al. Sex differences in striatal dopamine release in healthy adults. Biol Psychiatry. 2006;59:966–74.
Riccardi P, Zald D, Li R, Park S, Ansari MS, Dawant B, et al. Sex differences in amphetamine-induced displacement of [18F]fallypride in striatal and extrastriatal regions: a PET study. Am J Psychiatry. 2006;163:1639–41.
Riccardi P, Park S, Anderson S, Doop M, Ansari MS, Schmidt D, et al. Sex differences in the relationship of regional dopamine release to affect and cognitive function in striatal and extrastriatal regions using positron emission tomography and [18F]fallypride. Synapse. 2011;65:99–102.
Smith CT, Dang LC, Burgess LL, Perkins SF, San Juan MD, Smith DK, et al. Lack of consistent sex differences in d-amphetamine-induced dopamine release measured with [18F]fallypride PET. Psychopharmacology (Berl). 2019;236:581–90.
Zakiniaeiz Y, Hillmer AT, Matuskey D, Nabulsi N, Ropchan J, Mazure CM, et al. Sex differences in amphetamine-induced dopamine release in the dorsolateral prefrontal cortex of tobacco smokers. Neuropsychopharmacology 2019;44:2205–11.
Rodrigues A-J, Leão P, Carvalho M, Almeida OFX, Sousa N. Potential programming of dopaminergic circuits by early life stress. Psychopharmacology (Berl). 2011;214:107–20.
Novick AM, Levandowski ML, Laumann LE, Philip NS, Price LH, Tyrka AR. The effects of early life stress on reward processing. J Psychiatr Res. 2018;101:80–103.
Oswald LM, Wand GS, Kuwabara H, Wong DF, Zhu S, Brasic JR. History of childhood adversity is positively associated with ventral striatal dopamine responses to amphetamine. Psychopharmacology (Berl). 2014;231:2417–33.
Oswald LM, Wand GS, Wong DF, Brown CH, Kuwabara H, Brašić JR. Risky decision-making and ventral striatal dopamine responses to amphetamine: a positron emission tomography [11C]raclopride study in healthy adults. Neuroimage. 2015;113:26–36.
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D’Souza CD, Erdos J, et al. Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci USA. 1996;93:9235–40.
Abi-Dargham A, Gil R, Krystal J, Baldwin RM, Seibyl JP, Bowers M, et al. Increased striatal dopamine transmission in schizophrenia: Confirmation in a second cohort. Am J Psychiatry. 1998;155:761–7.
Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R. Increased dopamine transmission in schizophrenia: Relationship to illness phases. Biol Psychiatry. 1999;46:56–72.
Colle R, Dupong I, Colliot O, Deflesselle E, Hardy P, Falissard B, et al. Smaller hippocampal volumes predict lower antidepressant response/remission rates in depressed patients: a meta-analysis. World J Biol Psychiatry. 2018;19:360–7.
Göder R, Aldenhoff JB, Boigs M, Braun S, Koch J, Fritzer G. Delta power in sleep in relation to neuropsychological performance in healthy subjects and schizophrenia patients. J Neuropsychiatry Clin Neurosci. 2006;18:529–35.
Goldstein JM, Cohen LS, Horton NJ, Lee H, Andersen S, Tohen M, et al. Sex differences in clinical response to olanzapine compared with haloperidol. Psychiatry Res. 2002;110:27–37.
Trifilieff P, Ducrocq F, van der Veldt S, Martinez D. Blunted dopamine transmission in addiction: potential mechanisms and implications for behavior. Semin Nucl Med. 2017;47:64–74.
David SP, Naudet F, Laude J, Radua J, Fusar-Poli P, Chu I, et al. Potential reporting bias in neuroimaging studies of sex differences. Sci Rep. 2018;8:1–8.
Button KS, Ioannidis JPA, Mokrysz C, Nosek BA, Flint J, Robinson ESJ, et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci. 2013;14:365–76.
Eliot L. The trouble with sex differences. Neuron. 2011;72:895–8.
Ozomaro U, Wahlestedt C, Nemeroff CB. Personalized medicine in psychiatry: problems and promises. BMC Med. 2013;11:1–35.
Carey JL, Nader N, Chai PR, Carreiro S, Griswold MK, Boyle KL. Drugs and medical devices: adverse events and the impact on women’s health. Clin Ther. 2017;39:10–22.
Tharpe N. Adverse drug reactions in women’s health care. J Midwifery Women’s Heal. 2011;56:205–13.
Duffy KA, Ziolek TA, Epperson CN. Filling the regulatory gap: potential role of institutional review boards in promoting consideration of sex as a biological variable. J Women’s Heal. 2020;29:868–75.
Acknowledgements
The authors thank Andy Novick, Brianna Soreth, and Mary Sammel for their helpful feedback on the manuscript. Special thanks to Rachel Johnson for help interpreting statistical findings from some of the papers. Dr. Epperson’s work is supported by NIH grant R01CA216687. She consults for Sage Therapeutics and Asarina Pharma and is an investigator for a multisite clinical trial conducted by Sage Therapeutics. Dr. Epperson serves as a scientific advisor for BabyScripts and on the Board of Directors for the Parthenon Management Group. Dr. Duffy declares no conflicts of interest.
Author information
Authors and Affiliations
Contributions
Under the supervision of C.N.E., K.A.D. conducted the systematic literature search, assessed whether studies met inclusion criteria, and wrote the first draft of the manuscript. C.N.E. provided adjudication on appropriateness for article inclusion and critical revisions.
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Duffy, K.A., Epperson, C.N. Evaluating the evidence for sex differences: a scoping review of human neuroimaging in psychopharmacology research. Neuropsychopharmacol. 47, 430–443 (2022). https://doi.org/10.1038/s41386-021-01162-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-021-01162-8
This article is cited by
-
Consideration of sex as a biological variable in diabetes research across twenty years
Biology of Sex Differences (2024)
-
Cortical alterations associated with lower response to methylphenidate in adults with ADHD
Nature Mental Health (2024)
-
Disentangling sex differences in PTSD risk factors
Nature Mental Health (2024)
-
Are we moving the dial? Canadian health research funding trends for women’s health, 2S/LGBTQ + health, sex, or gender considerations
Biology of Sex Differences (2023)