Abstract
The normal prostate epithelial structure is maintained by homeostatic interactions with smooth muscle cells. However, structural alterations of the stroma are commonly observed in prostatic proliferative diseases, leading to the abnormalities of prostate epithelial structure. A decrease in the androgen level experimentally induces stromal remodeling, i.e., replacement of smooth muscle cells with fibroblasts or myofibroblasts. In this study, we investigated the effects of castration-induced stromal remodeling and subsequent aberrant activation of epithelial–stromal interactions on the reconstituted human prostate-like epithelial structure. We performed in vivo experiments using the human prostate epithelial cell line BPH-1 and fetal rat urogenital sinus mesenchyme to generate heterotypic tissue recombinants that form human prostate-like epithelial structure (i.e., solid- and canalized-epithelial cords). Host mice were castrated at 12 weeks post transplantation (castration) and implanted with a dihydrotestosterone pellet at 14 days post castration (androgen replacement treatment; ART). In the castration group, the percentages of fibrotic area and disrupted prostate epithelial structure without the basement membrane (BM) increased proportionally in a time-dependent manner, but were suppressed by ART. In the castration group, tenascin-C (TNC)-positive fibroblasts were abundant in the stroma surrounding disrupted prostate epithelial structure without the BM. TGF-β1 secretion from BPH-1 cells was increased by co-culturing with human primary cultured prostate fibroblasts. TNC mRNA expression was increased in fibroblasts co-culturing with BPH-1 cells and was suppressed by treatment with a TGF-β RI kinase inhibitor. Moreover, in the castration group, the percentage of p-Smad2-positive cells was significantly higher in the stroma surrounding disrupted prostate epithelial structure without the BM. Our results demonstrate that castration-induced stromal remodeling disrupted the reconstituted human prostate-like epithelial structure and induced the appearance of TNC-positive fibroblasts accompanied by activation of TGF-β signaling. The alteration of prostate stromal structure may be responsible for loss of the BM and epithelial cell polarity.
Similar content being viewed by others
Introduction
The incidences of proliferative diseases such as benign prostatic hyperplasia (BPH) and prostate cancer (PCa) increase with advancing age, despite decreasing androgen levels [1]. The histopathological features of BPH are nodular hyperplasia and/or chronic inflammation, whereas those of PCa are atypical glands called Gleason patterns. There are structural differences in the epithelium between BPH and PCa; however, the stromal structures of BPH and PCa are quite similar (e.g., abundant fibroblasts and myofibroblasts, and few smooth muscle cells) [2, 3]. Structural alterations of the stroma in both BPH and PCa are referred to as stromal remodeling (i.e., replacement of smooth muscle cells with fibroblasts or myofibroblasts). Fibroblasts and myofibroblasts secrete cytokines and growth factors such as interleukin-6 (IL-6), epidermal growth factor family members, fibroblast growth factors (FGFs), insulin-like growth factors, and transforming growth factor-β (TGF-β), which are involved in the development and progression of proliferative diseases such as BPH and PCa [4, 5]. Moreover, fibroblasts and myofibroblasts secrete high levels of extracellular matrix (ECM) proteins, such as fibronectin (FN), tenascin-C (TNC), and types I and II collagen [3, 6]. The ECM is considered to play a role in the migration, invasion, and growth of PCa cells [7]. Thus, active stimuli from fibroblasts and myofibroblasts can be associated with the abnormalities in prostate epithelial structure.
The androgen status affects the structures of the prostate stroma and epithelium. In the absence of androgen, prostate structural regression is attributed mainly to a functional decrease in the secretory activity of luminal epithelial cells and to a reduced in the number of luminal epithelial cells by apoptosis [8, 9]. Moreover, castration induces stromal remodeling in the dog and mouse prostate stroma [10, 11]. Castration-induced stromal remodeling is accompanied by functional transformation of the prostate stromal environment [12]. In the absence of androgen, basal cells of the dog prostate lose their capacity to differentiate into luminal cells [10]. In the mouse prostate, the number of basal cells was increased by activation of FGF2/FGFR signaling in the absence of androgen and then returned to baseline levels following androgen replacement treatment (ART) [11]. Therefore, we hypothesize that castration-induced stromal remodeling and subsequent aberrant activation of epithelial–stromal interactions may induce the abnormalities in prostate epithelial structure.
In prostate, androgen acts on smooth muscle cells to maintain a fully differentiated prostate epithelial structure, which is composed of an outer layer of basal cells with basement membrane (BM) and an inner layer of luminal cells [13, 14]. Loss of the BM is commonly observed in hyperplastic glands, prostatic intraepithelial neoplasia, and adenocarcinoma, leading to loss of epithelial cell polarity [14, 15]. In adult tissues including prostate, the BM regulates the organization of epithelial cells such as growth/quiescence, functional differentiation, and polarity of epithelial cells [16]. Thus, we hypothesize that loss of the BM may be the first step for initiating prostate proliferative diseases such as BPH and PCa.
There are few mouse models available that can be used to evaluate the effects of stromal remodeling and subsequent aberrant activation of epithelial–stromal interactions on prostate epithelial structure. BPH occurs naturally in human and dog prostates, but not in the mouse prostate [17, 18]. Moreover, in genetically engineered mouse models of PCa, the induced PCa differs both in phenotype and behavior from those of human PCa [19]. The reason why simulation of prostatic proliferative diseases is difficult in mice may be that the stromal structures of human and mouse prostates are clearly different (e.g., thick vs. thin smooth muscle layer in human vs. mouse prostates, respectively).
To recapitulate the thick smooth muscle layer in the human prostate, we used a tissue recombination model composed of a human prostate epithelial cell line (BPH-1) and rat urogenital sinus mesenchyme (rUGM). BPH-1 cells were isolated from BPH specimens and immortalized using the SV40 large T antigen (SV40 Tag) [20]. A feature of BPH-1 cells is the loss of androgen receptor (AR) expression, whereas BPH-1 cells + rUGM tissue recombinants form solid- and canalized-epithelial cords with a well-defined BM induced by BPH-1 cells and thick sheets of well-differentiated smooth muscle derived from rUGM [13]. These structures resemble the human prostate structure in in vivo animal models. In this study, we investigated the effects of castration-induced stromal remodeling and subsequent aberrant activation of epithelial–stromal interactions on the reconstituted human prostate-like epithelial structure (i.e., solid- and canalized-epithelial cords) in BPH-1 cells + rUGM tissue recombinants.
Materials and methods
Reagents
Dihydrotestosterone (DHT) was purchased from Tokyo Chemical Industry Co., Ltd (Tokyo, Japan). TGF-β type I receptor (RI) kinase inhibitor (SB-431542) was purchased from Sigma-Aldrich, Inc. (St. Louis, MO, USA). Mouse monoclonal anti-SV40 Tag antibody was purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Rabbit polyclonal anti-human TNC antibody was purchased from Immuno-Biological Laboratories Co., Ltd (Gunma, Japan). Mouse monoclonal anti-α-smooth muscle actin (αSMA) and mouse monoclonal anti-vimentin antibodies were purchased from Sigma-Aldrich, Inc. Mouse monoclonal antihuman collagen IV antibody was purchased from Dako Cytomation (Copenhagen, Denmark). Rabbit polyclonal p-Smad2 (phospho S467) antibody was purchased from Abcam Inc. (Cambridge, MA, USA).
Isolation of fibroblasts from the prostate tissue of PCa patients
This study involving human subjects was approved by the institutional review board of our institution. Consent was obtained from each patient after full disclosure of the purpose and nature of all procedures. Primary cultured prostate fibroblasts (pcPrFs) were isolated from PCa biopsy specimens collected from patients with advanced PCa, as described previously [21].
Cell culture
The nontumorigenic human prostate epithelial cell line BPH-1 was obtained from Dr Simon W. Hayward (Northshore University HealthSystem, Chicago, IL, USA). The commercially available human prostate stromal cell line PrSC was purchased from Lonza Group Ltd (Basel, Switzerland). BPH-1 cells were cultured in RPMI-1640 with phenol red (RPMI (+)) supplemented with 10% fetal bovine serum (FBS) and 1% antibiotic/antimycotic solution. PrSC and pcPrFs were cultured in medium prepared using the SCBM Bullet Kit (Lonza Group Ltd).
DHT treatment
PrSC and pcPrFs (pcPrF-M7, pcPrF-M11, and pcPrF-M24) were seeded into six-well plates (6.0 × 104 cells/well) in SCBM and cultured for 2 days. The culture medium was replaced with RPMI-1640 without phenol red (RPMI (−)) supplemented with 1% charcoal-stripped (CS)-FBS containing various concentrations of DHT for 2 days.
Co-culture of fibroblasts with BPH-1 cells and TGF-β RI kinase inhibitor treatment
PrSC and pcPrFs (pcPrF-M7, pcPrF-M11, and pcPrF-M24) were co-cultured with BPH-1 cells in six-well plates using cell culture inserts (BD Falcon, Franklin Lakes, NJ, USA). PrSC and pcPrFs were seeded into six-well plates (6.0 × 104 cells/well) in SCBM, whereas BPH-1 cells were seeded into cell culture inserts (2.0 × 104 cells/well) in RPMI (+) supplemented with 10% FBS for 2 days. The culture medium for fibroblasts and BPH-1 cells was replaced with RPMI (−) supplemented with 1% CS-FBS containing DHT (0.1 nM) and various concentrations of the TGF-β RI kinase inhibitor. The inserts with BPH-1 cells were then placed into six-well plates for 2 days. DHT concentrations in the incubation medium were selected based on previous studies of DHT levels in prostate tissue after castration [22, 23].
RNA extraction, cDNA preparation, and real-time PCR analysis
Total RNA was extracted using the RNeasy Mini Kit (Qiagen Inc., Valencia, CA, USA) in accordance with the manufacturer’s instructions. The RNA concentration was determined spectrophotometrically. cDNA was reverse transcribed from 100 ng of total RNA using the High Capacity RNA-to-cDNA Kit (Life Technologies, Foster City, CA, USA) in a total volume of 20 μl. TaqMan quantitative PCR was performed using the Applied Biosystems StepOne real-time PCR system (Life Technologies). TaqMan Gene Expression Assays for TNC (Hs01115665_m1) were performed using EagleTaq Master Mix containing ROX (Roche Diagnostics, Mannheim, Germany). All data were analyzed using StepOne Software version 2.1 (Applied Biosystems, Foster City, CA, USA), and mRNA levels were normalized to those of GAPDH (Hs99999905_m1).
Enzyme-linked immunosorbent assay (ELISA)
For quantitative determination of TGF-β1, vascular endothelial growth factor (VEGF), and IL-6 protein levels, aliquots of conditioned medium were collected and subjected to ELISA using Quantikine human TGF-β1, VEGF, and IL-6 immunoassay kits (R & D Systems, Inc. Minneapolis, MN, USA).
Animal studies
Eight-week-old male severe combined immunodeficiency (SCID) mice (C.B-17/lcr-scid/scidJcl) were purchased from CLEA Japan, Inc. (Tokyo, Japan). Pregnant Sprague-Dawley rats were purchased from SLC Japan, Inc. (Shizuoka, Japan). All animals were maintained in a pathogen-free environment, under experimental protocol guidelines approved by the Mie University Committee on Animal Investigations.
Preparation and processing of grafts
rUGM was prepared from 18-day-old embryonic fetuses (plug date denoted as day 0). Urogenital sinuses were dissected from fetuses and separated into epithelial and mesenchymal components by tryptic digestion, as described previously [24]. Cell recombinants were prepared by mixing 1.0 × 105 BPH-1 cells with 3.0 × 105 rUGM in suspension. Pelleted cells were resuspended in 50 μl neutralized collagen type І (from rat tail) solution for gels. Recombinants were grafted beneath the renal capsule of 24 male SCID mice (8 groups × 3 mice).
Androgen manipulation in mice
Male SCID mice underwent sham operation (sham group) and surgical castration (castration group) at 12 weeks post transplantation via a scrotal incision under isoflurane anesthesia. The mice were then sacrificed at 7, 14, and 28 days post castration. The kidneys were excised, and the grafts were dissected free of the host kidney. For the ART experiment, mice were castrated as above, and a 20 mg DHT pellet was implanted subcutaneously at 14 days post castration (ART group). DHT pellets were generated in our laboratory using a pellet press (Parr Instrument Company, Moline, IL, USA). At 14 days after implantation of the DHT pellet, the mice were sacrificed and grafts were collected. The 48 grafts (8 groups × 3 mice × 2 grafts) were fixed in 10% neutral-buffered formalin (Nacalai Tesque, Kyoto, Japan) at room temperature overnight for histopathological analysis and immunohistochemical staining, and then processed and embedded in paraffin in accordance with standard procedures.
Histopathology and immunohistochemistry
For histopathology, standard hematoxylin and eosin (H&E) and Masson’s trichrome staining were performed as described previously [2]. Next, immunohistochemical staining was performed using the ImmPRESS Reagent Kit (Vector Laboratories, Inc., Burlingame, CA, USA). For antigen retrieval of SV40 Tag, TNC, collagen IV, and p-Smad2, Antigen Unmasking Solution (Vector Laboratories, Inc.), 1.3 mg/ml pepsin solution (Sigma-Aldrich, Inc.), Proteinase K (Dako Cytomation), and Tris-EDTA buffer solution pH 9.0 (Nacalai Tesque) were used, respectively. Antigen retrieval was not performed for αSMA and vimentin. TNC, αSMA, collagen IV, vimentin, and p-Smad2 antibodies were used at dilutions of 1:1000, 1:10,000, 1:50, 1:300, and 1:300, respectively.
Image analysis
To calculate the percentage of fibrotic area, sections were photographed after Masson’s trichrome staining using a microscope digital camera (DP 74, Olympus Corporation, Tokyo, Japan) combined with the CellSens Standard 1.17 imaging system (Olympus Corporation). The images were scanned into a computer at a magnification of ×200. Each section was randomly photographed at a maximum of five visual fields of view. Using the Win ROOF 2015 image analysis program (ver. 3, Mitani, Fukui, Japan), the percentage of fibrotic area was calculated as described previously [2]. To calculate the percentage of disrupted solid- and canalized-epithelial cords, sections were photographed after collagen IV and SV40 Tag staining as described above. In this study, we defined normal vs. disrupted solid- and canalized-epithelial cords as the presence vs. absence of collagen IV-positive BM, respectively. SV40 Tag staining images were scanned into a computer at a magnification of ×40. Whole sections were photographed, and using the Win ROOF 2015 image analysis program, normal solid- and canalized-epithelial cords were removed from each image. The areas of disrupted solid- and canalized-epithelial cords were measured.
To calculate the percentage of p-Smad2-positive stromal cells, sections were photographed after p-Smad2 staining as described above. The images were scanned into a computer at a magnification of ×400. Sections were randomly photographed at a maximum of five visual fields of view. Using the Win ROOF 2015 image analysis program, the numbers of p-Smad2-positive and negative stromal cells were counted individually.
Statistical analysis
Results were expressed as the means ± standard deviation (SD). Statistically significant differences between two groups were determined using Student’s t test or Welch’s test. For comparisons among more than two groups, Tukey’s or Dunnett’s multiple comparison test was used. Differences with P values less than 0.05 were considered statistically significant. All statistical analyses were performed using SPSS Statistics version 23 (IBM Corp., Tokyo, Japan).
Results
Effect of the androgen level on the reconstituted human prostate-like stromal structure in BPH-1 cells + rUGM tissue recombinants in vivo
BPH-1 cells + rUGM tissue recombinants were grown for 16 weeks after grafting beneath the renal capsule in male SCID mice in the sham (Fig. 1a, panel a), castration (Fig. 1a, panel b), and ART (Fig. 1a, panel c) groups. To investigate the effect of castration and subsequent ART on the reconstituted human prostate-like stromal structure, Masson’s trichrome staining was performed in tissue sections from mice of the sham (Fig. 1a, panel d), castration (Fig. 1a, panel e), and ART (Fig. 1a, panel f) groups. Masson’s trichrome staining distinguished collagen fibers from smooth muscle in the reconstituted human prostate-like stromal structure.
a, a–c Representative gross appearances of BPH-1 cells + rUGM tissue recombinants, which were grafted beneath the renal capsule of male SCID mice in the (a) sham group at 28 days post sham-operation, (b) castration group at 28 days post castration, and (c) ART group at 14 days post ART (bar = 2 mm). Representative image of Masson’s trichrome staining in the (d) sham group, (e) castration group, and (f) ART group. Bar = 100 μm, magnification = ×200. b Percentage of fibrotic area. ○ sham group, ● castration group, and □ ART group. Values represent the means ± SD. ***P < 0.001, castration group vs. sham group at each time point. †††P < 0.001, castration group vs. ART group at each time point. ART androgen replacement treatment, NS not significant.
In the sham group, the percentage of fibrotic area increased slightly in a time-dependent manner (Fig. 1b). However, the percentage of fibrotic area in castration group was significantly higher than that in the sham group at 7, 14, and 28 days post castration (Fig. 1b). ART suppressed the progression of fibrosis. The percentage of fibrotic area at 14 days post ART was approximately the same between the ART and sham groups (Fig. 1b).
Effect of the androgen level on the reconstituted human prostate-like epithelial structure in BPH-1 cells + rUGM tissue recombinants in vivo
To investigate the effect of castration and subsequent ART on the reconstituted human prostate-like epithelial structure (i.e., solid- and canalized-epithelial cords), immunohistochemical staining of collagen IV and SV40 was performed in tissue sections from each group. Normal solid- and canalized-epithelial cords are separated from the stroma by the BM. The BM is composed of type IV collagen, which forms a continuous lining that surrounds and attaches to the basal cell layer. Collagen IV staining indicated collagen IV-positive BM formation in normal solid- and canalized-epithelial cords (Fig. 2a, panel a), but not in disrupted solid- and canalized-epithelial cords (Fig. 2a, panel b). Because BPH-1 cells were immortalized with SV40 Tag, this antigen was expressed only in solid- and canalized-epithelial cords reconstituted with BPH-1 cells. SV40 Tag staining was performed in tissue sections from mice in the sham (Fig. 2b, panel a), castration (Fig. 2b, panel b), and ART (Fig. 2b, panel c) groups.
a (a) Representative image of collagen IV staining in normal solid- and canalized-epithelial cords. a (b) Representative image of collagen IV staining in disrupted solid- and canalized-epithelial cords. Arrowheads indicate collagen IV-positive BM. Bar = 50 μm, magnification = ×400. b Representative image of SV40 Tag staining in the (a) sham group at 28 days post sham-operation, (b) castration group at 28 days post castration, and (c) ART group at 14 days post ART. Bar = 100 μm, magnification = ×200. c Percentage of disrupted solid- and canalized-epithelial cords. ○ sham group, ● castration group, and □ ART group. Values represent the means ± SD. ***P < 0.001, castration group vs. sham group at each time point. †††P < 0.001, castration group vs. ART group at each time point. ‡‡‡P < 0.001, ART group vs. sham group at each time point. Tag large T antigen, ART androgen replacement treatment.
In the sham group, the percentage of disrupted solid- and canalized-epithelial cords was slightly increased in a time-dependent manner (Fig. 2c). However, percentage of disrupted solid- and canalized-epithelial cords in castration group was significantly higher than that in the sham group at 7, 14, and 28 days post castration (Fig. 2c). ART suppressed the increase in the percentage of disrupted solid- and canalized-epithelial cords induced by castration. Even so, the percentage of disrupted solid- and canalized-epithelial cords at 14 days post ART was still higher in the ART group than sham group (Fig. 2c).
Effect of the androgen level on the stromal histopathological characteristics of BPH-1 cells + rUGM tissue recombinants in vivo
H&E staining revealed both normal (Fig. 3a, c, e) and disrupted (Fig. 3b, d, f) solid- and canalized-epithelial cords in all groups. Only H&E staining could not distinguish stromal components. In the sham group, αSMA, TNC, and vimentin staining indicated no differences in the reconstituted human prostate-like stromal structure surrounding normal vs. disrupted solid- and canalized-epithelial cords (Fig. 3g, h, m, n, s, t). Similarly, in the castration and ART groups, αSMA and vimentin staining indicated no difference in the reconstituted human prostate-like stromal structure surrounding normal vs. disrupted solid- and canalized-epithelial cords (Fig. 3i–l, u–x). However, in the castration and ART groups, TNC-positive fibroblasts were abundant in the reconstituted human prostate-like stromal structure surrounding disrupted, compared with normal, solid- and canalized-epithelial cords (Fig. 3o–r).
a–f Representative image of H&E staining in each group. g–l Representative image of αSMA staining of the reconstituted human prostate-like stromal structure in each group. m–r Representative image of TNC staining in the reconstituted human prostate-like stromal structure in each group. s–x Representative image of vimentin staining in the reconstituted human prostate-like stromal structure in each group. Bar = 100 μm, magnification = ×200.
Effect of co-culture with fibroblasts on cytokine secretion from BPH-1 cells in vitro
TGF-β1 and VEGF secretion from BPH-1 cells were significantly increased by co-culturing with pcPrF-M24 (Fig. 4a, b). In contrast, VEGF secretion from BPH-1 cells was decreased by co-culturing with pcPrF-M7 (Fig. 4b). IL-6 secretion from BPH-1 cells was significantly increased by co-culturing with all fibroblast lines (Fig. 4c).
a Effect of co-culture with fibroblasts on TGF-β1 secretion from BPH-1 cells. b Effect of co-culture with fibroblasts on VEGF secretion from BPH-1 cells. c Effect of co-culture with fibroblasts on IL-6 secretion from BPH-1 cells. For quantitative determination of TGF-β1, VEGF, and IL-6, aliquots of conditioned medium were subjected to ELISA. Values represent the means ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001 vs. BPH-1 cells alone.
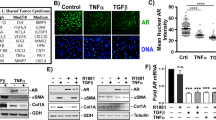
Effect of DHT on TNC mRNA expression in fibroblasts in vitro
Upon changing the culture medium from SCBM to 1% CS-FBS RPMI (−), TNC mRNA expression was decreased in pcPrF-M11 but was not affected in PrSC, pcPrF-M7, or pcPrF-M24 (Fig. 5). After culturing the cells in 1% CS-FBS RPMI (−) supplemented with 0.1 nM DHT for 2 days, TNC mRNA expression was decreased in PrSC (Fig. 5a), whereas it was not affected by the DHT level in pcPrF-M7, pcPrF-M11, or pcPrF-M24 (Fig. 5b–d).
a PrSC, b pcPrF-M7, c pcPrF-M11, and d pcPrF-M24 were cultured in SCBM or 1% CS-FBS RPMI (−) containing various concentrations of DHT (0–0.1 nM). Total RNA was isolated from fibroblasts and subjected to TaqMan quantitative RT-PCR analysis. The relative mRNA expression of TNC was determined in fibroblasts. Values represent the means ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001 vs. fibroblasts in 1% CS-FBS RPMI (−) without DHT. CS-FBS charcoal-stripped-fetal bovine serum, DHT dihydrotestosterone.
Effect of co-culturing with BPH-1 cells and treatment with a TGF-β RI kinase inhibitor on TNC mRNA expression in fibroblasts in vitro
TNC mRNA expression was significantly increased in fibroblasts (PrSC, pcPrF-M7, pcPrF-M11, and pcPrF-M24) by co-culturing with BPH-1 cells for 2 days (Fig. 6). To examine whether the increase in the TNC mRNA expression was induced by reciprocal interactions between fibroblasts and BPH-1 cells via TGF-β1 signaling, we performed co-culture experiments using a TGF-β RI kinase inhibitor (SB-431542). SB-431542 significantly suppressed the increase in the TNC mRNA level in all fibroblast lines co-culturing with BPH-1 cells, in a dose-dependent manner (Fig. 6).
a PrSC, b pcPrF-M7, c pcPrF-M11, and d pcPrF-M24 were co-cultured with BPH-1 cells in SCBM or 1% CS-FBS RPMI (−) containing DHT (0.1 nM) and various concentrations of TGF-β RI kinase inhibitor (0–10 μM). Total RNA was isolated from fibroblasts and subjected to TaqMan quantitative RT-PCR analysis. The relative mRNA expression of TNC was determined in fibroblasts. Values represent the means ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001 vs. fibroblasts alone in 1% CS-FBS RPMI (−) containing DHT (0.1 nM).
Effect of the androgen level on stromal TGF-β1 signaling in BPH-1 cells + rUGM tissue recombinants in vivo
To investigate activation of TGF-β1 signaling in the reconstituted human prostate-like stromal structure, p-Smad2 staining was performed in tissue sections from mice in the sham, castration, and ART groups (Fig. 7a). In the castration group, the percentage of p-Smad2-positive stromal cells in the reconstituted human prostate-like stromal structure surrounding disrupted solid- and canalized-epithelial cords was significantly higher than that of surrounding normal solid- and canalized-epithelial cords (Fig. 7b). In addition, the percentage of p-Smad2-positive stromal cells in the reconstituted human prostate-like stromal structure surrounding disrupted solid- and canalized-epithelial cords was significantly higher in the castration group than in the sham and ART groups (Fig. 7b). In the ART group, the percentage of p-Smad2-positive stromal cells in the reconstituted human prostate-like stromal structure surrounding disrupted solid- and canalized-epithelial cords was similar to that surrounding normal solid- and canalized-epithelial cords (Fig. 7b).
a Representative image of p-Smad2 staining in each group. Inserts shows magnification of the images at ×1000, and arrowheads indicate p-Smad2-positive stromal cells. Bar = 50 μm, magnification = ×400. b The number of p-Smad2-positive stromal cells per 100 stromal cells was counted. Values represent the means ± SD. ***P < 0.001, percentage of p-Smad2-positive stromal cells surrounding disrupted vs. normal solid- and canalized-epithelial cords in the castration group. †††P < 0.001, percentage of p-Smad2-positive stromal cells surrounding disrupted solid- and canalized-epithelial cords in the castration group vs. sham group. ‡P < 0.05, percentage of p-Smad2-positive stromal cells surrounding disrupted solid- and canalized-epithelial cords in the castration group vs. ART group. ART androgen replacement treatment, NS not significant.
Discussion
In this study, the increased percentage of disrupted solid- and canalized-epithelial cords was proportional to the progression of castration-induced stromal remodeling in the reconstituted human prostate-like structure. This suggests that castration-induced stromal remodeling may disrupt the reconstituted human prostate-like epithelial structure. Thick sheets of well-differentiated smooth muscle maintain normal solid- and canalized-epithelial cords with a well-defined BM in BPH-1 cells + rUGM tissue recombinants [13]. In general, the attachment of epithelial cells to the BM is important for maintenance of tissue integrity [16]. The BM contains a variety of adhesive ECM glycoproteins, including collagen IV, laminin, FN, and proteoglycan [25]. The BM covers the basal surfaces of epithelia by attaching epithelial cells directly to the BM. The BM contains information that influences the organization of epithelial cells [16]. In particular, the BM plays critical roles in the development of epithelial cell polarity and thus is an essential structure for the maintenance of prostate epithelial structure. In this study, our results indicated that normal solid- and canalized-epithelial cords had the ability to form BM, whereas disrupted solid- and canalized-epithelial cords lost that ability.
In the castration group, TNC-positive fibroblasts were abundant in the reconstituted human prostate-like stromal structure surrounding disrupted solid- and canalized-epithelial cords. TNC is a hexametric glycoprotein of the ECM produced by the mesenchyme, fibroblasts, and cancer cells [26]. In normal adult tissue, TNC expression is less abundant, whereas it is induced during tissue remodeling, such as wound healing, involution, and tumorigenesis [27]. TNC induces loss of focal adhesions and promotes cell spreading via modulating the expression of actin in the cytoskeleton [26, 27]. Even in the sham group, the percentage of disrupted solid- and canalized-epithelial cords was increased, and TNC-positive fibroblasts were scarce, suggesting that the antiadhesive and cell spreading effects of TNC may not be necessary to induce disruption of the reconstituted human prostate-like epithelial structure. However, the increased abundance of TNC-positive fibroblasts in the castration group may lead to further disruption of the reconstituted human prostate-like epithelial structure.
We hypothesize two mechanisms for the increased abundance of TNC-positive fibroblasts in the reconstituted human prostate-like stromal structure of the castration group: (1) castration may induce upregulation of TNC expression in fibroblasts; and (2) aberrant activation of epithelial–stromal interactions may induce upregulation of TNC expression in fibroblasts. Very little is known about the signaling pathways involved in the regulation of TNC in this context. Our results indicated that TNC mRNA expression in fibroblasts such as pcPrF-M7, pcPrF-M11, and pcPrF-M24 was not directly affected by the DHT level. In contrast, previous studies have reported that several cytokines upregulate TNC expression. For example, TGF-β, IL-4, platelet-derived growth factor, and bFGF upregulate TNC synthesis in human dermal fibroblasts [28]. In the prostate, TNC mRNA expression in PrSC was upregulated by TGF-β treatment [29]. TGF-β-induced TNC expression has been reported to be mediated by the Smad family of transcriptional regulators [28, 30]. In the castration group, our results indicated that the number of p-Smad2-positive cells was significantly increased in TNC-positive fibroblasts surrounding disrupted solid- and canalized-epithelial cords. In co-cultures of cancer cells and fibroblasts, fibroblasts directly increased the expression of TGF-β in breast and lung cancer cells [31]. According to our co-culture experiments of BPH-1 cells with fibroblasts, we showed that TGF-β1 secretion from BPH-1 cells and TNC mRNA expression in fibroblasts were increased. The characteristics of fibroblasts such as PrSC and pcPrFs were diversity, e.g., clinicopathological characteristics of patients and the level of cytokine secretions [21]. This feature of fibroblasts may cause the differing results in co-cultures of BPH-1 cells with PrSC and pcPrFs, i.e., the alteration of cytokine secretions from BPH-1 cells were different by co-culturing with each fibroblast. Moreover, treatment with the TGF-β RI kinase inhibitor suppressed the increase in TNC mRNA expression in fibroblasts co-culturing with BPH-1 cells. Finally, these findings and our results suggest that TNC-positive fibroblasts may be induced by aberrant activation of epithelial–stromal interactions via TGF-β signaling.
Figure 8 illustrates our proposed role for TNC-positive fibroblasts in proliferative diseases such as BPH and PCa. A decrease in androgen levels with advancing age often is seen in patients with BPH [1, 32]. Of note, androgen levels are low in patients with PCa after androgen deprivation therapy (ADT) [22, 23]. Stromal remodeling can be induced experimentally by decreasing the androgen level (e.g., castration induces stromal remodeling in dog and mouse prostate stroma) [10, 11]. Under low-androgen conditions, we infer from our results that the number of TNC-positive fibroblasts may increase in prostate stroma. Several studies have reported that TNC-positive fibroblasts are associated with progression of BPH and PCa. For example, TNC expression is elevated in the BPH stroma, and TNC emerges as a likely candidate regulator of the hyperplastic phenotype observed in BPH [33]. In our laboratory, Sasaki et al. reported that pcPrFs derived from different human PCa specimens displayed high TNC mRNA expression [21]. In addition, TNC expression is significantly increased in the human PCa stroma surrounding neoplastic glands [34]. TNC expression in PCa stroma was associated with proliferation, invasion, and metastasis of PCa [35]. In the clinic, overexpression of TNC as a potential biomarker of cancer associated fibroblasts was significantly correlated with a poor prognosis of patients with PCa [36]. These findings and our results suggest that a decrease in the androgen level may induce TNC-positive fibroblasts via aberrant activation of epithelial–stromal interactions, which may cause progression of BPH and PCa.
Castration induces stromal remodeling and disruption of prostate epithelial structure via loss of BM formation and epithelial cell polarity. Subsequently, TGF-β1 secretion from prostate epithelial cells is increased by aberrant activation of epithelial–stromal interactions. Finally, TNC-positive fibroblasts are induced by aberrant activation of TGF-β1 signaling. On the other hand, ART suppresses the progression of stromal remodeling and the increase in the percentage of disrupted prostate epithelial structure. TNC tenascin-C, ART androgen replacement treatment.
We infer from our results that ADT may induce stromal remodeling and aberrant activation of TGF-β signaling in patients with advanced PCa. Aberrant activation of TGF-β signaling occurred in the PCa stroma led to AR activation and contributed to the emergence of CRPC [37, 38]. Therefore, TGF-β signaling could be the therapeutic targeting for the treatment of patients with advanced PCa. It is possible that treatment with a TGF-β RI kinase inhibitor in combination with ADT may suppress the progression of PCa. For example, galunisertib is a clinically tested low-molecular-weight inhibitor of TGF-β RI kinase [39]. Galunisertib has antitumor activity in tumor-bearing animal models such as breast cancer, colon cancer, lung cancer, and hepatocellular carcinoma [39]. Moreover, the combination of galunisertib with concurrent temozolomide (TMZ) for treatment of glioma models was more effective than TMZ monotherapy [40]. Using human PCa cell lines such as LNCaP, VCaP, and C4-2B cells, Song et al. demonstrated synergistic effects of galunisertib combined with enzalutamide, a nonsteroidal second-generation antiandrogen agent, in inhibiting CRPC progression [41]. In a mouse model of PCa, the combination of galunisertib with enzalutamide suppressed prostate tumor progression via inhibition of epithelial–mesenchymal transition, compared with galunisertib or enzalutamide monotherapy [42]. We suggest that early treatment with a TGF-β RI kinase inhibitor in combination with ADT may suppress PCa progression via inhibition of aberrant activation of TGF-β signaling. Finally, further studies are needed to elucidate the role of stromal remodeling in prostate epithelial structure, which may provide insights into the role of prostate stromal structure in prostate proliferative diseases such as BPH and PCa, and new treatments for PCa.
References
Shibata Y, Ito K, Suzuki K, Nakano K, Fukabori Y, Suzuki R, et al. Changes in the endocrine environment of the human prostate transition zone with aging: simultaneous quantitative analysis of prostatic sex steroids and comparison with human prostatic histological composition. Prostate. 2000;42:45–55.
Imamura T, Ishii K, Kanda H, Arase S, Yoshio Y, Hori Y, et al. Structural changes in alpha1-adrenoceptor antagonist-treated human prostatic stroma. Clin Exp Med. 2010;10:99–106.
Tuxhorn JA, Ayala GE, Smith MJ, Smith VC, Dang TD, Rowley DR. Reactive stroma in human prostate cancer: induction of myofibroblast phenotype and extracellular matrix remodeling. Clin Cancer Res. 2002;8:2912–23.
Chung LW, Baseman A, Assikis V, Zhau HE. Molecular insights into prostate cancer progression: the missing link of tumor microenvironment. J Urol. 2005;173:10–20.
Russell PJ, Bennett S, Stricker P. Growth factor involvement in progression of prostate cancer. Clin Chem. 1998;44:705–23.
Erdogan B, Ao M, White LM, Means AL, Brewer BM, Yang L, et al. Cancer-associated fibroblasts promote directional cancer cell migration by aligning fibronectin. J Cell Biol. 2017;216:3799–816.
Leach DA, Need EF, Toivanen R, Trotta AP, Palethorpe HM, Tamblyn DJ, et al. Stromal androgen receptor regulates the composition of the microenvironment to influence prostate cancer outcome. Oncotarget. 2015;6:16135–50.
English HF, Santen RJ, Isaacs JT. Response of glandular versus basal rat ventral prostatic epithelial cells to androgen withdrawal and replacement. Prostate. 1987;11:229–42.
Antonioli E, Cardoso AB, Carvalho HF. Effects of long-term castration on the smooth muscle cell phenotype of the rat ventral prostate. J Androl. 2007;28:777–83.
Shidaifat F, Daradka M, Al-Omari R. Effect of androgen ablation on prostatic cell differentiation in dogs. Endocr Res. 2004;30:327–34.
Kato M, Ishii K, Iwamoto Y, Sasaki T, Kanda H, Yamada Y, et al. Activation of FGF2-FGFR signaling in the castrated mouse prostate stimulates the proliferation of basal epithelial cells. Biol Reprod. 2013;89:81.
Vilamaior PS, Taboga SR, Carvalho HF. Modulation of smooth muscle cell function: morphological evidence for a contractile to synthetic transition in the rat ventral prostate after castration. Cell Biol Int. 2005;29:809–16.
Wang Y, Sudilovsky D, Zhang B, Haughney PC, Rosen MA, Wu DS, et al. A human prostatic epithelial model of hormonal carcinogenesis. Cancer Res. 2001;61:6064–72.
Liu A, Wei L, Gardner WA, Deng CX, Man YG. Correlated alterations in prostate basal cell layer and basement membrane. Int J Biol Sci. 2009;5:276–85.
Bonkhoff H, Wernert N, Dhom G, Remberger K. Basement membranes in fetal, adult normal, hyperplastic and neoplastic human prostate. Virchows Arch A Pathol Anat Histopathol. 1991;418:375–81.
Gumbiner BM. Cell adhesion: the molecular basis of tissue architecture and morphogenesis. Cell. 1996;84:345–57.
Coffey DS, Walsh PC. Clinical and experimental studies of benign prostatic hyperplasia. Urol Clin North Am. 1990;17:461–75.
Sugimura Y, Sakurai M, Hayashi N, Yamashita A, Kawamura J. Age-related changes of the prostate gland in the senescence-accelerated mouse. Prostate. 1994;24:24–32.
Grabowska MM, DeGraff DJ, Yu X, Jin RJ, Chen Z, Borowsky AD, et al. Mouse models of prostate cancer: picking the best model for the question. Cancer Metastasis Rev. 2014;33:377–97.
Hayward SW, Dahiya R, Cunha GR, Bartek J, Deshpande N, Narayan P. Establishment and characterization of an immortalized but non-transformed human prostate epithelial cell line: BPH-1. In Vitro Cell Dev Biol Anim. 1995;31:14–24.
Sasaki T, Ishii K, Iwamoto Y, Kato M, Miki M, Kanda H, et al. Fibroblasts prolong serum prostate-specific antigen decline after androgen deprivation therapy in prostate cancer. Lab Investig. 2016;96:338–49.
Mohler JL, Gregory CW, Ford OH 3rd, Kim D, Weaver CM, Petrusz P, et al. The androgen axis in recurrent prostate cancer. Clin Cancer Res. 2004;10:440–8.
Titus MA, Schell MJ, Lih FB, Tomer KB, Mohler JL. Testosterone and dihydrotestosterone tissue levels in recurrent prostate cancer. Clin Cancer Res. 2005;11:4653–7.
Ishii K, Imamura T, Iguchi K, Arase S, Yoshio Y, Arima K, et al. Evidence that androgen-independent stromal growth factor signals promote androgen-insensitive prostate cancer cell growth in vivo. Endocr Relat Cancer. 2009;16:415–28.
Mosher DF, Sottile J, Wu C, McDonald JA. Assembly of extracellular matrix. Curr Opin Cell Biol. 1992;4:810–8.
Orend G, Chiquet-Ehrismann R. Tenascin-C induced signaling in cancer. Cancer Lett. 2006;244:143–63.
Jones PL, Jones FS. Tenascin-C in development and disease: gene regulation and cell function. Matrix Biol. 2000;19:581–96.
Jinnin M, Ihn H, Asano Y, Yamane K, Trojanowska M, Tamaki K. Tenascin-C upregulation by transforming growth factor-beta in human dermal fibroblasts involves Smad3, Sp1, and Ets1. Oncogene. 2004;23:1656–67.
Ishii K, Mizokami A, Tsunoda T, Iguchi K, Kato M, Hori Y, et al. Heterogenous induction of carcinoma-associated fibroblast-like differentiation in normal human prostatic fibroblasts by co-culturing with prostate cancer cells. J Cell Biochem. 2011;112:3604–11.
Maschler S, Grunert S, Danielopol A, Wirl BeugH. Enhanced tenascin-C expression and matrix deposition during Ras/TGF-beta-induced progression of mammary tumor cells. Oncogene. 2004;23:3622–33.
Limoge M, Safina A, Beattie A, Kapus L, Truskinovsky AM, Bakin AV. Tumor-fibroblast interactions stimulate tumor vascularization by enhancing cytokine-driven production of MMP9 by tumor cells. Oncotarget. 2017;8:35592–608.
Martov AG, Ergakov DV. Age-related androgen deficiency and benign prostatic hyperplasia: how to improve the rehabilitation of patients after transurethral surgery?. Urologiia. 2016:110–7.
Schauer IG, Rowley DR. The functional role of reactive stroma in benign prostatic hyperplasia. Differentiation. 2011;82:200–10.
Kruslin B, Ulamec M, Tomas D. Prostate cancer stroma: an important factor in cancer growth and progression. Bosn J Basic Med Sci. 2015;15:1–8.
Barron DA, Rowley DR. The reactive stroma microenvironment and prostate cancer progression. Endocr Relat Cancer. 2012;19:R187–204.
Ni WD, Yang ZT, Cui CA, Cui Y, Fang LY, Xuan YH. Tenascin-C is a potential cancer-associated fibroblasts marker and predicts poor prognosis in prostate cancer. Biochem Biophys Res Commun. 2017;486:607–12.
Eastham JA, Truong LD, Rogers E, Kattan M, Flanders KC, Scardino PT, et al. Transforming growth factor-beta 1: comparative immunohistochemical localization in human primary and metastatic prostate cancer. Lab Investig. 1995;73:628–35.
Pu H, Begemann DE, Kyprianou N. Aberrant TGF-beta signaling drives castration-resistant prostate cancer in a male mouse model of prostate tumorigenesis. Endocrinology. 2017;158:1612–22.
Herbertz S, Sawyer JS, Stauber AJ, Gueorguieva I, Driscoll KE, Estrem ST, et al. Clinical development of galunisertib (LY2157299 monohydrate), a small molecule inhibitor of transforming growth factor-beta signaling pathway. Drug Des Devel Ther. 2015;9:4479–99.
Zhang M, Herion TW, Timke C, Han N, Hauser K, Weber KJ, et al. Trimodal glioblastoma treatment consisting of concurrent radiotherapy, temozolomide, and the novel TGF-beta receptor I kinase inhibitor LY2109761. Neoplasia. 2011;13:537–49.
Song B, Park SH, Zhao JC, Fong KW, Li S, Lee Y, et al. Targeting FOXA1- mediated repression of TGF-beta signaling suppresses castration-resistant prostate cancer progression. J Clin Investig. 2018;129:569–82.
Paller C, Pu H, Begemann DE, Wade CA, Hensley PJ, Kyprianou N. TGF-beta receptor I inhibitor enhances response to enzalutamide in a pre-clinical model of advanced prostate cancer. Prostate. 2019;79:31–43.
Acknowledgements
We would like to thank Mrs Izumi Matsuoka and Ms Yumi Yoshikawa for their technical support. This work was supported by Grants-in-Aid from the Ministry of Education for Science and Culture of Japan (grant number 15K10583).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kajiwara, S., Ishii, K., Sasaki, T. et al. Castration-induced stromal remodeling disrupts the reconstituted prostate epithelial structure. Lab Invest 100, 670–681 (2020). https://doi.org/10.1038/s41374-019-0352-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41374-019-0352-4