Abstract
Objective
Quantify blood fatty acids and growth outcomes in preterm infants fed the exclusive human milk diet.
Methods
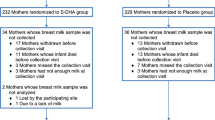
A prospective cohort study of 30 infants 24–34 weeks gestation and ≤1250 g fed the exclusive human milk diet. Blood fatty acids were quantified at two time points. Comparisons were made using two-sample t-tests and Wilcoxon rank sum.
Results
Donor human milk-fed (n = 12) compared to mother’s own milk-fed infants (n = 18) from birth to after 28 days of life, had an increased interval change of linoleic to docosahexaenoic acid ratio (5.5 vs. −1.1 mole percent ratio, p = 0.034). Docosahexaenoic and eicosapentaenoic acid interval changes were similar between groups. The arachidonic acid change was similar between groups (−2.3 vs. −0.9 mole percent, p = 0.37), however, both experienced a negative change across time. At 36 weeks postmenstrual age, growth velocities were similar for groups.
Conclusion
An exclusive human milk diet maintains birth docosahexaenoic and eicosapentaenoic acid concentrations. However, the postnatal deficit in arachidonic acid was not prevented.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
If requested, I will provide the de-identified data used in this manuscript, the code book, and the analytic code to the editors.
References
Uauy R, Mena P, Wegher B, Nieto S, Salem NJ. Long chain polyunsaturated fatty acid formation in neonates: effect of gestational age and intrauterine growth. Pediatr Res. 2000;47:127–35.
Baack ML, Puumala SE, Messier SE, Pritchett DK, Harris WS. What is the relationship between gestational age and docosahexaenoic acid (DHA) and arachidonic acid (ARA) levels? Prostaglandins Leukot Ess Fat Acids. 2015;100:5–11.
Martin CR, Cheesman A, Brown J, Makda M, Kutner AJ, Da Silva D, et al. Factors determining optimal fatty acid absorption in preterm infants. J Pediatr Gastroenterol Nutr. 2016;62:130–6.
Carnielli VP, Simonato M, Verlato G, Luijendijk I, De Curtis M, Sauer PJJ, et al. Synthesis of long-chain polyunsaturated fatty acids in preterm newborns fed formula with long-chain polyunsaturated fatty acids. Am J Clin Nutr. 2007;86:1323–30.
Martin CR, Dasilva DA, Cluette-Brown JE, Dimonda C, Hamill A, Bhutta AQ, et al. Decreased postnatal docosahexaenoic and arachidonic acid blood levels in premature infants are associated with neonatal morbidities. J Pediatr. 2011;159:743–9.e2.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Marangoni F, Angeli MT, Colli S, Eligini S, Tremoli E, Sirtori CR, et al. Changes of N-3 and N-6 fatty acids in plasma and circulating cells of normal subjects, after prolonged administration of 20:5 (EPA) and 22:6 (DHA) ethyl esters and prolonged washout. Biochim Biophys Acta 1993;1210:55–62.
Stark KD, Aristizabal Henao JJ, Metherel AH, Pilote L. Translating plasma and whole blood fatty acid compositional data into the sum of eicosapentaenoic and docosahexaenoic acid in erythrocytes. Prostaglandins Leukot Ess Fat Acids. 2016;104:1–10.
Products N, Prolacta F. Nutrition information 100%. 2019. https://www.prolacta.com/Data/Sites/14/media/box.com/mkt-0627-rev-0_prolacta-product-nutrition-brochure-us_v18.pdf.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117:1253–61.
Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R. Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant. BMC Pediatr. 2013;13:1–10
Chou JH, Roumiantsev S, Singh R. PediTools electronic growth chart calculators: applications in clinical care, research, and quality improvement. J Med Internet Res. 2020;22. https://pubmed.ncbi.nlm.nih.gov/32012066/.
Patel AL, Engstrom JL, Meier PP, Jegier BJ, Kimura RE. Calculating postnatal growth velocity in very low birth weight (VLBW) premature infants. J Perinatol. 2009;29:618–22.
Richardson DK, Gray JE, McCormick MC, Workman K, Goldmann DA, et al. Score for neonatal acute physiology: a physiologic severity index for neonatal intensive care. Pediatrics. 1993;91:617–23.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr. 2001;138:92–100.
Gidrewicz DA, Fenton TR. A systematic review and meta-analysis of the nutrient content of preterm and term breast milk. BMC Pediatr. 2014;14:1–14.
Baack ML, Puumala SE, Messier SE, Pritchett DK, Harris WS. Daily enteral DHA supplementation alleviates deficiency in premature infants. Lipids. 2016;51:423–33.
Robinson DT, Martin CR. Fatty acid requirements for the preterm infant. Semin Fetal Neonatal Med. 2017;22:8–14.
Lu J, Jilling T, Li D, Caplan MS. Polyunsaturated fatty acid supplementation alters proinflammatory gene expression and reduces the incidence of necrotizing enterocolitis in a neonatal rat model. Pediatr Res. 2007;61:427–32.
Kitamura T, Kitamura Y, Hamano H, Shoji H, Shimizu T, Shimizu T. The ratio of docosahexaenoic acid and arachidonic acid in infant formula influences the fatty acid composition of the erythrocyte membrane in low-birth-weight infants. Ann Nutr Metab. 2016;68:103–12.
Koletzko B, Poindexter B, Uauy R. Nutritional care of preterm infants scientific basis and practical guidelines preface. 110th ed. Karger Publishers in Basel: Switzerland; 2014. p. XI–XII.
Fleig L, Unger J, Gollins L, Hagan J, Martin C, Hair A. An evaluation of docosahexaenoic acid (DHA) and arachidonic acid (AA) levels in preterm infants <1250 grams birth weight fed an exclusive human milk diet supplemented with human milk-based cream. Baltimore, Maryland.
Koletzko B, Bergmann K, Thomas BJ, Calder PC, Campoy C, Clandinin MT, et al. Should formula for infants provide arachidonic acid along with DHA? A position paper of the European Academy of Paediatrics and the Child Health Foundation. Am J Clin Nutr. 2020;111:10–6.
Fleith M, Clandinin MT. Dietary PUFA for preterm and term infants: review of clinical studies. Crit Rev Food Sci Nutr. 2005;45:205–29.
Gibson RA, Neumann MA, Makrides M. Effect of increasing breast milk docosahexaenoic acid on plasma and erythrocyte phospholipid fatty acids and neural indices of exclusively breastfed infants. Eur J Clin Nutr. 1997;51:578–84.
Lechner BE, Vohr BR. Neurodevelopmental outcomes of preterm infants fed human milk: a systematic review. Clin Perinatol. 2017;44:69–83.
Belfort MB, Ehrenkranz RA. Neurodevelopmental outcomes and nutritional strategies in very low birth weight infants. Semin Fetal Neonatal Med. 2017;22:42–8. https://doi.org/10.1016/j.siny.2016.09.001.
Rozé JC, Darmaun D, Boquien CY, Flamant C, Picaud JC, Savagner C, et al. The apparent breastfeeding paradox in very preterm infants: relationship between breast feeding, early weight gain and neurodevelopment based on results from two cohorts, EPIPAGE and LIFT. BMJ Open. 2012;2:1–9.
Abrams SA, Schanler RJ, Lee ML, Rechtman DJ. Greater mortality and morbidity in extremely preterm infants fed a diet containing cow milk protein products. Breastfeed Med. 2014;9:281–5.
O’Connor DL, Kiss A, Tomlinson C, Bando N, Bayliss A, Campbell DM, et al. Nutrient enrichment of human milk with human and bovine milk-based fortifiers for infants born weighing <1250 g: a randomized clinical trial. Am J Clin Nutr. 2018;108:108–16.
Hair AB, Peluso AM, Hawthorne KM, Perez J, Smith DP, Khan JY, et al. Beyond necrotizing enterocolitis prevention: improving outcomes with an exclusive human milk-based diet. Breastfeed Med. 2016;11:70–4.
Sullivan S, Schanler RJ, Kim JH, Patel JH, Trawöger R, Kiechl-Kohlendorfer U, et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr. 2010;156:562–7.
Cristofalo EA, Schanler RJ, Blanco CL, Sullivan S, Trawoeger R, Kiechl-Kohlendorfer U, et al. Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants. J Pediatr. 2013;163:1592–5.e1. https://doi.org/10.1016/j.jpeds.2013.07.011.
Osmanova M, Müller MJ, Habisch B, Hippe A, Seeliger S. Nutrition of infants with very low birth weight using human and bovine based milk fortifier: benefits and costs. Neonatal Pediatr Med. 2021;7.
Martin CR, Brown YF, Ehrenkranz RA, O’Shea TM, Allred EN, Belfort MB, et al. Nutritional practices and growth velocity in the first month of life in extremely premature infants. Pediatrics. 2009;124:649–57.
Friend LL, Perrin MT. Fat and protein variability in donor human milk and associations with milk banking processes. Breastfeed Med. 2020;15:370–5.
Acknowledgements
The authors thank the nursing staff of Texas Children’s Hospital neonatal intensive care unit and the parents of our preterm infants who were critical in ensuring the successful completion of this study. Supported by the Evie Whitlock Foundation Grant for fellows in Neonatal-Perinatal Medicine at Baylor College of Medicine. The authors would also like to thank the following people for their invaluable assistance with the project: Kristina Tucker, BSN, RNC-LRN, Nelly Zavala, Texas Children’s Hospital Neonatal Dietitians and Milk Bank Technicians.
Funding
LFH received research support from the Baylor College of Medicine Evangelina “Evie” Whitlock Fellowship Award in Neonatology, Houston, TX, and the Texas Children’s Hospital Clinical Research Center. She received no outside funding for this study. All other others did not contribute funding to this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: LFH, ABH and CRM; methodology: LFH, ABH and CRM; formal analysis: LFH, ABH and CRM; investigation: LFH, JPU, PG, HY, JEC-B, ABH and CRM; data curation: LFH, JPU, PG, HY and JEC-B; writing—original draft preparation: LFH; writing—review and editing: LFH, JPU, PG, HY, JEC-B, LAG, ABH and CRM; supervision: LFH, ABH and CRM; project administration: LFH, JPU and HY; funding acquisition: LFH.
Corresponding author
Ethics declarations
Competing interests
CRM serves on the advisory board of LactaLogics, Plakous Therapeutics, and Vitara Biomedical. All other authors declare no conflict of interest.
Ethical approval
All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work. The Institutional Review Board at Baylor College of Medicine, Texas Children’s Hospital in Houston, TX, approved this study (Protocol H-43075). Informed written consent was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Holzapfel, L.F., Unger, J.P., Gordon, P. et al. Fatty acid concentrations in preterm infants fed the exclusive human milk diet: a prospective cohort study. J Perinatol 44, 680–686 (2024). https://doi.org/10.1038/s41372-023-01841-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01841-y