Abstract
Bronchopulmonary dysplasia (BPD) remains the most common long-term morbidity of premature birth, and the incidence of BPD is not declining despite medical advancements. Infants with BPD are at high risk for postnatal growth failure and are often treated with therapies that suppress growth. Additionally, these infants may display excess weight gain relative to linear growth. Optimal growth and nutrition are needed to promote lung growth and repair, improve long-term pulmonary function, and improve neurodevelopmental outcomes. Linear growth in particular has been associated with favorable outcomes yet can be difficult to achieve in these patients. While there has been a significant clinical and research focus regarding BPD prevention and early preterm nutrition, there is a lack of literature regarding nutritional care of the infant with established BPD. There is even less information regarding how nutritional needs change as BPD evolves from an acute to chronic disease. This article reviews the current literature regarding nutritional challenges, enteral nutrition management, and monitoring for patients with established BPD. Additionally, this article provides a practical framework for interdisciplinary nutritional care based on our clinical experience at the Comprehensive Center for Bronchopulmonary Dysplasia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
Patel RM. Short- and long-term outcomes for extremely preterm infants. Am J Perinatol. 2016;33:318–28. https://doi.org/10.1055/s-0035-1571202.
Jensen EA, Edwards EM, Greenberg LT, Soll RF, Ehret DEY, Horbar JD. Severity of bronchopulmonary dysplasia among very preterm infants in the United States. Pediatrics. 2021;148:e2020030007 https://doi.org/10.1542/peds.2020-030007.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9. https://doi.org/10.1164/ajrccm.163.7.2011060.
Abman SH, Collaco JM, Shepherd EG, Keszler M, Cuevas-Guaman M, Welty SE, et al. Bronchopulmonary dysplasia collaborative. interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr. 2017;181:12–28.e1. https://doi.org/10.1016/j.jpeds.2016.10.082.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. an evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9. https://doi.org/10.1164/rccm.201812-2348OC.
Murthy K, Porta NFM, Lagatta JM, Zaniletti I, Truog WE, Grover TR, et al. Inter-center variation in death or tracheostomy placement in infants with severe bronchopulmonary dysplasia. J Perinatol. 2017;37:723–7. https://doi.org/10.1038/jp.2016.277.
Arigliani M, Spinelli AM, Liguoro I, Cogo P. Nutrition and lung growth. Nutrients. 2018;10:919 https://doi.org/10.3390/nu10070919.
Natarajan G, Johnson YR, Brozanski B, et al. Postnatal weight gain in preterm infants with severe bronchopulmonary dysplasia. Am J Perinatol. 2014;31:223–30. https://doi.org/10.1055/s-0033-1345264.
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. ESPGHAN Committee on Nutrition. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91. https://doi.org/10.1097/MPG.0b013e3181adaee0.
Dutta S, Singh B, Chessell L, Wilson J, Janes M, McDonald K, et al. Guidelines for feeding very low birth weight infants. Nutrients 2015;7:423–42. https://doi.org/10.3390/nu7010423.
Koletzko B, Cheah F-C, Domellof, M, Poindexter BB, Vain N, van Goudoever JB, editors. Nutritional care of preterm infants. Scientific basis and practical guidelines. World Review of Nutrition and Dietetics, vol 122. Basel: Karger; 2021. p. XII–XIV.
Skinner AM, Narchi H. Preterm nutrition and neurodevelopmental outcomes. World J Methodol. 2021;11:278–93. https://doi.org/10.5662/wjm.v11.i6.278.
Poindexter BB, Martin CR. Impact of nutrition on bronchopulmonary dysplasia. Clin Perinatol. 2015;42:797–806. https://doi.org/10.1016/j.clp.2015.08.007.
Piersigilli F, Van Grambezen B, Hocq C, Danhaive O. Nutrients and microbiota in lung diseases of prematurity: the placenta-gut-lung triangle. Nutrients. 2020;12:469 https://doi.org/10.3390/nu12020469.
Ma L, Zhou P, Neu J, Lin HC. Potential nutrients for preventing or treating bronchopulmonary dysplasia. Paediatr Respir Rev. 2017;22:83–88. https://doi.org/10.1016/j.prrv.2016.08.013.
Northway WH Jr, Moss RB, Carlisle KB, Parker BR, Popp RL, Pitlick PT, et al. Late pulmonary sequelae of bronchopulmonary dysplasia. N Engl J Med. 1990;323:1793–9. https://doi.org/10.1056/NEJM199012273232603.
Mataloun MM, Leone CR, Mascaretti RS, Dohlnikoff M, Rebello CM. Effect of postnatal malnutrition on hyperoxia-induced newborn lung development. Braz J Med Biol Res. 2009;42:606–13. https://doi.org/10.1590/s0100-879x2009000700004.
Frank L, Sosenko IR. Undernutrition as a major contributing factor in the pathogenesis of bronchopulmonary dysplasia. Am Rev Respir Dis. 1988;138:725–9. https://doi.org/10.1164/ajrccm/138.3.725.
Filbrun AG, Popova AP, Linn MJ, McIntosh NA, Hershenson MB. Longitudinal measures of lung function in infants with bronchopulmonary dysplasia. Pediatr Pulmonol. 2011;46:369–75. https://doi.org/10.1002/ppul.21378.
Bott L, Béghin L, Devos P, Pierrat V, Matran R, Gottrand F. Nutritional status at 2 years in former infants with bronchopulmonary dysplasia influences nutrition and pulmonary outcomes during childhood. Pediatr Res. 2006;60:340–4. https://doi.org/10.1203/01.pdr.0000232793.90186.ca.
Meyers JM, Tan S, Bell EF, Duncan AF, Guillet R, Stoll BJ, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental outcomes among extremely premature infants with linear growth restriction. J Perinatol. 2019;39:193–202. https://doi.org/10.1038/s41372-018-0259-8.
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 2006;117:1253–61. https://doi.org/10.1542/peds.2005-1368.
Pfister KM, Ramel SE. Linear growth and neurodevelopmental outcomes. Clin Perinatol. 2014;41:309–21. https://doi.org/10.1016/j.clp.2014.02.004.
Barrington KJ, Fortin-Pellerin E, Pennaforte T. Fluid restriction for treatment of preterm infants with chronic lung disease. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.cd005389.pub2.
Roberts K, Stepanovich G, Bhatt-Mehta V, Donn SM. New pharmacologic approaches to bronchopulmonary dysplasia. J Exp Pharmacol. 2021;13:377–96. https://doi.org/10.2147/JEP.S262350.
Rush MG, Engelhardt B, Parker RA, Hazinski TA. Double-blind, placebo-controlled trial of alternate-day furosemide therapy in infants with chronic bronchopulmonary dysplasia. J Pediatr. 1990 ;117:112–8. https://doi.org/10.1016/s0022-3476(05)82458-8.
Wassner SJ. Altered growth and protein turnover in rats fed sodium-deficient diets. Pediatr Res. 1989;26:608–13. https://doi.org/10.1203/00006450-198912000-00019.
Curtiss J, Zhang H, Griffiths P, Shepherd EG, Lynch S. Nutritional management of the infant with severe bronchopulmonary dysplasia. Neoreviews. 2015;16:e674–e679.
Bamat NA, Kirpalani H, Feudtner C, Jensen EA, Laughon MM, Zhang H, et al. Medication use in infants with severe bronchopulmonary dysplasia admitted to United States children’s hospitals. J Perinatol. 2019;39:1291–9. https://doi.org/10.1038/s41372-019-0415-9.
Kielt MJ, Logan JW, Backes CH, Conroy S, Reber KM, Shepherd EG, et al. Noninvasive respiratory severity indices predict adverse outcomes in bronchopulmonary dysplasia. J Pediatr. 2022;242:129–136.e2. https://doi.org/10.1016/j.jpeds.2021.11.015.
Lewis T, Truog W, Nelin L, Napolitano N, McKinney RL. Pharmacoepidemiology of drug exposure in intubated and non-intubated preterm infants with severe bronchopulmonary dysplasia. Front Pharmacol. 2021;12:695270 https://doi.org/10.3389/fphar.2021.695270.
Leitch CA, Ahlrichs J, Karn C, Denne SC. Energy expenditure and energy intake during dexamethasone therapy for chronic lung disease. Pediatr Res. 1999;46:109–13. https://doi.org/10.1203/00006450-199907000-00018.
Van Goudoever JB, Wattimena JD, Carnielli VP, Sulkers EJ, Degenhart HJ, Sauer PJ. Effect of dexamethasone on protein metabolism in infants with bronchopulmonary dysplasia. J Pediatr. 1994;124:112–8. https://doi.org/10.1016/s0022-3476(94)70265-9.
Appel B, Fried SK. Effects of insulin and dexamethasone on lipoprotein lipase in human adipose tissue. Am J Physiol. 1992;262:E695–9. https://doi.org/10.1152/ajpendo.1992.262.5.E695.
Hauner H, Schmid P, Pfeiffer EF. Glucocorticoids and insulin promote the differentiation of human adipocyte precursor cells into fat cells. J Clin Endocrinol Metab. 1987;64:832–5. https://doi.org/10.1210/jcem-64-4-832.
Bauer SE, Huff KA, Vanderpool CPB, Rose RS, Cristea AI. Growth and nutrition in children with established bronchopulmonary dysplasia: a review of the literature. Nutr Clin Pract. 2022;37:282–98. https://doi.org/10.1002/ncp.10841.
Wang LY, Luo HJ, Hsieh WS, Hsu CH, Hsu HC, Chen PS, et al. Severity of bronchopulmonary dysplasia and increased risk of feeding desaturation and growth delay in very low birth weight preterm infants. Pediatr Pulmonol. 2010;45:165–73. https://doi.org/10.1002/ppul.21171.
Malkar MB, Gardner W, Welty SE, Jadcherla SR. Antecedent predictors of feeding outcomes in premature infants with protracted mechanical ventilation. J Pediatr Gastroenterol Nutr. 2015;61:591–5. https://doi.org/10.1097/MPG.0000000000000867.
Hatch LD, Scott TA, Walsh WF, Goldin AB, Blakely ML, Patrick SW. National and regional trends in gastrostomy in very low birth weight infants in the USA: 2000-2012. J Perinatol. 2018;38:1270–6. https://doi.org/10.1038/s41372-018-0145-4.
Hansmann G, Sallmon H, Roehr CC, Kourembanas S, Austin ED, Koestenberger M. European Pediatric Pulmonary Vascular Disease Network (EPPVDN). Pulmonary hypertension in bronchopulmonary dysplasia. Pediatr Res. 2021;89:446–55. https://doi.org/10.1038/s41390-020-0993-4.
Rocha G, Guimarães H, Pereira-Da-Silva L. The role of nutrition in the prevention and management of bronchopulmonary dysplasia: a literature review and clinical approach. Int J Environ Res Public Health. 2021;18:6245 https://doi.org/10.3390/ijerph18126245.
Bozzetti V, De Angelis C, Tagliabue PE. Nutritional approach to preterm infants on noninvasive ventilation: an update. Nutrition. 2017;37:14–17. https://doi.org/10.1016/j.nut.2016.12.010.
Oh W. Fluid and electrolyte management of very low birth weight infants. Pediatr Neonatol. 2012;53:329–33. https://doi.org/10.1016/j.pedneo.2012.08.010.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, et al. European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology. 2019;115:432–50. https://doi.org/10.1159/000499361.
Biniwale MA, Ehrenkranz RA. The role of nutrition in the prevention and management of bronchopulmonary dysplasia. Semin Perinatol. 2006;30:200–8. https://doi.org/10.1053/j.semperi.2006.05.007.
Denne SC. Energy expenditure in infants with pulmonary insufficiency: is there evidence for increased energy needs? J Nutr. 2001;131:935S–937S. https://doi.org/10.1093/jn/131.3.935S.
De Meer K, Westerterp KR, Houwen RH, Brouwers HA, Berger R, Okken A. Total energy expenditure in infants with bronchopulmonary dysplasia is associated with respiratory status. Eur J Pediatr. 1997;156:299–304. https://doi.org/10.1007/s004310050605.
Kurzner SI, Garg M, Bautista DB, Bader D, Merritt RJ, Warburton D, et al. Growth failure in infants with bronchopulmonary dysplasia: nutrition and elevated resting metabolic expenditure. Pediatrics. 1988;81:379–84.
Groothuis JR, Makari D. Definition and outpatient management of the very low-birth-weight infant with bronchopulmonary dysplasia. Adv Ther. 2012;29:297–311. https://doi.org/10.1007/s12325-012-0015-y.
Fenton TR, Groh-Wargo S, Gura K, Martin CR, Taylor SN, Griffin IJ, et al. Effect of enteral protein amount on growth and health outcomes in very-low-birth-weight preterm infants: phase II of the pre-B project and an evidence analysis center systematic review. J Acad Nutr Diet. 2021;121:2287–2300.e12. https://doi.org/10.1016/j.jand.2020.11.002.
Brunton JA, Saigal S, Atkinson SA. Growth and body composition in infants with bronchopulmonary dysplasia up to 3 months corrected age: a randomized trial of a high-energy nutrient-enriched formula fed after hospital discharge. J Pediatr. 1998;133:340–5. https://doi.org/10.1016/s0022-3476(98)70266-5.
Giannì ML, Roggero P, Colnaghi MR, Piemontese P, Amato O, Orsi A, et al. The role of nutrition in promoting growth in pre-term infants with bronchopulmonary dysplasia: a prospective non-randomised interventional cohort study. BMC Pediatr. 2014;14:235 https://doi.org/10.1186/1471-2431-14-235.
Pereira GR, Baumgart S, Bennett MJ, Stallings VA, Georgieff MK, Hamosh M, et al. Use of high-fat formula for premature infants with bronchopulmonary dysplasia: metabolic, pulmonary, and nutritional studies. J Pediatr. 1994;124:605–11. https://doi.org/10.1016/s0022-3476(05)83143-9.
Eidelman AI. Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed Med. 2012;7:323–4. https://doi.org/10.1089/bfm.2012.0067.
Kim LY, McGrath-Morrow SA, Collaco JM. Impact of breast milk on respiratory outcomes in infants with bronchopulmonary dysplasia. Pediatr Pulmonol. 2019;54:313–8. https://doi.org/10.1002/ppul.24228.
Morgan JA, Young L, McCormick FM, McGuire W. Promoting growth for preterm infants following hospital discharge. Arch Dis Child Fetal Neonatal Ed. 2012;97:F295–8. https://doi.org/10.1136/adc.2009.170910.
Massaro D, Massaro GD. Retinoids, alveolus formation, and alveolar deficiency: clinical implications. Am J Respir Cell Mol Biol. 2003;28:271–4. https://doi.org/10.1165/rcmb.F263.
Mandell E, Seedorf G, Gien J, Abman SH. Vitamin D treatment improves survival and infant lung structure after intra-amniotic endotoxin exposure in rats: potential role for the prevention of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2014;306:L420–8. https://doi.org/10.1152/ajplung.00344.2013.
Mehta NM. Clinical guidelines: nutrition support of the critically ill child. J Parenter Enter Nutr. 2009;33:260–76. https://doi.org/10.1177/0148607109333114.
Bischoff AR, Tomlinson C, Belik J. Sodium intake requirements for preterm neonates: review and recommendations. J Pediatr Gastroenterol Nutr. 2016;63:e123–e129. https://doi.org/10.1097/MPG.0000000000001294.
Domellöf M, Georgieff MK. Postdischarge iron requirements of the preterm infant. J Pediatr. 2015;167:S31–5. https://doi.org/10.1016/j.jpeds.2015.07.018.
Terrin G, Berni Canani R, Di Chiara M, Pietravalle A, Aleandri V, Conte F, et al. Zinc in early life: a key element in the fetus and preterm neonate. Nutrients. 2015;7:10427–46. https://doi.org/10.3390/nu7125542.
Vázquez-Gomis R, Bosch-Gimenez V, Juste-Ruiz M, Vázquez-Gomis C, Izquierdo-Fos I, Pastor-Rosado J. Zinc concentration in preterm newborns at term age, a prospective observational study. BMJ Paediatr Open. 2019;3:e000527 https://doi.org/10.1136/bmjpo-2019-000527.
Shaikhkhalil AK, Curtiss J, Puthoff TD, Valentine CJ. Enteral zinc supplementation and growth in extremely-low-birth-weight infants with chronic lung disease. J Pediatr Gastroenterol Nutr. 2014;58:183–7. https://doi.org/10.1097/MPG.0000000000000145.
Cohen N, Golik A. Zinc balance and medications commonly used in the management of heart failure. Heart Fail Rev. 2006;11:19–24. https://doi.org/10.1007/s10741-006-9189-1.
Logan JW, Lynch SK, Curtiss J, Shepherd EG. Clinical phenotypes and management concepts for severe, established bronchopulmonary dysplasia. Paediatr Respir Rev. 2019;31:58–63. https://doi.org/10.1016/j.prrv.2018.10.004.
Underwood MA, Lakshminrusimha S, Steinhorn RH, Wedgwood S. Malnutrition, poor post-natal growth, intestinal dysbiosis and the developing lung. J Perinatol. 2021;41:1797–810. https://doi.org/10.1038/s41372-020-00858-x.
Ehrenkranz RA, Das A, Wrage LA, et al. Early nutrition mediates the influence of severity of illness on extremely LBW infants. Pediatr Res. 2011;69:522–9.
Jensen EA, Zhang H, Feng R, Dysart K, Nilan K, Munson DA, et al. Individualising care in severe bronchopulmonary dysplasia: a series of N-of-1 trials comparing transpyloric and gastric feeding. Arch Dis Child Fetal Neonatal Ed. 2020;105:399–404. https://doi.org/10.1136/archdischild-2019-317148.
Mehta NM. Energy expenditure: how much does it matter in infant and pediatric chronic disorders? Pediatr Res. 2015;77:168–72. https://doi.org/10.1038/pr.2014.180.
Institute of Medicine. Dietary reference intakes: the essential guide to nutrient requirements. Washington, DC: The National Academies Press; 2006. https://doi.org/10.17226/11537.
Corkins MR, Balint J, Plogsted S, Yaworski JA, editors. ASPEN Pediatric Nutrition Support Core Curriculum. 2nd ed., Ch. 32. ASPEN; 2018.
Kielt MJ, Logan JW, Backes CH, Reber KM, Nelin LD, Shepherd EG. In-hospital outcomes of late referrals for established bronchopulmonary dysplasia. J Perinatol. 2021;41:1972–82. https://doi.org/10.1038/s41372-021-01041-6.
Fenton TR, Anderson D, Groh-Wargo S, Hoyos A, Ehrenkranz RA, Senterre T. An attempt to standardize the calculation of growth velocity of preterm infants-evaluation of practical bedside methods. J Pediatr. 2018;196:77–83. https://doi.org/10.1016/j.jpeds.2017.10.005.
Pereira-da-Silva L, Virella D, Fusch C. Nutritional assessment in preterm infants: a practical approach in the NICU. Nutrients 2019;11:1999 https://doi.org/10.3390/nu11091999.
Madden J, Kobaly K, Minich NM, Schluchter M, Wilson-Costello D, Hack M. Improved weight attainment of extremely low-gestational-age infants with bronchopulmonary dysplasia. J Perinatol. 2010;30:103–11. https://doi.org/10.1038/jp.2009.142.
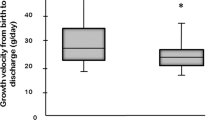
Miller AN, Moise AA, Cottrell L, Loomis K, Polak M, Gest A. Linear growth is associated with successful respiratory support weaning in infants with bronchopulmonary dysplasia. J Perinatol. 2022;42:544–5. https://doi.org/10.1038/s41372-022-01322-8.
Sanchez-Solis M, Perez-Fernandez V, Bosch-Gimenez V, Quesada JJ, Garcia-Marcos L. Lung function gain in preterm infants with and without bronchopulmonary dysplasia. Pediatr Pulmonol. 2016;51:936–42. https://doi.org/10.1002/ppul.23393.
Wood AJ, Raynes-Greenow CH, Carberry AE, Jeffery HE. Neonatal length inaccuracies in clinical practice and related percentile discrepancies detected by a simple length-board. J Paediatr Child Health. 2013;49:199–203. https://doi.org/10.1111/jpc.12119.
Nelin TD, Lorch S, Jensen EA, Alexiou S, Gibbs K, Napolitano N, et al. The association between diuretic class exposures and enteral electrolyte use in infants developing grade 2 or 3 bronchopulmonary dysplasia in United States children’s hospitals. J Perinatol. 2021;41:779–85. https://doi.org/10.1038/s41372-021-00924-y.
Bott L, Béghin L, Marichez C, Gottrand F. Comparison of resting energy expenditure in bronchopulmonary dysplasia to predicted equation. Eur J Clin Nutr. 2006;60:1323–9. https://doi.org/10.1038/sj.ejcn.1602463.
Sion-Sarid R, Cohen J, Houri Z, Singer P. Indirect calorimetry: a guide for optimizing nutritional support in the critically ill child. Nutrition. 2013;29:1094–9. https://doi.org/10.1016/j.nut.2013.03.013.
Gaio P, Verlato G, Daverio M, Cavicchiolo ME, Nardo D, Pasinato A, et al. Incidence of metabolic bone disease in preterm infants of birth weight <1250 g and in those suffering from bronchopulmonary dysplasia. Clin Nutr Espen. 2018;23:234–9. https://doi.org/10.1016/j.clnesp.2017.09.008.
Chen W, Zhang Z, Dai S, Xu L. Risk factors for metabolic bone disease among preterm infants less than 32 weeks gestation with Bronchopulmonary dysplasia. BMC Pediatr. 2021;21:235 https://doi.org/10.1186/s12887-021-02705-0.
Jensen EA, White AM, Liu P, Yee K, Waber B, Monk HM, et al. Determinants of severe metabolic bone disease in very low-birth-weight infants with severe bronchopulmonary dysplasia admitted to a tertiary referral center. Am J Perinatol. 2016;33:107–13. https://doi.org/10.1055/s-0035-1560043.
Chinoy A, Mughal MZ, Padidela R. Metabolic bone disease of prematurity: causes, recognition, prevention, treatment and long-term consequences. Arch Dis Child Fetal Neonatal Ed. 2019;104:F560–F566. https://doi.org/10.1136/archdischild-2018-316330.
Wood CL, Wood AM, Harker C, Embleton ND. Bone mineral density and osteoporosis after preterm birth: the role of early life factors and nutrition. Int J Endocrinol. 2013;2013:902513 https://doi.org/10.1155/2013/902513.
Pravia CI, Benny M. Long-term consequences of prematurity. Cleve Clin J Med. 2020;87:759–67. https://doi.org/10.3949/ccjm.87a.19108.
Abrams SA, Committee on Nutrition. Calcium and vitamin d requirements of enterally fed preterm infants. Pediatrics. 2013;131:e1676–83. https://doi.org/10.1542/peds.2013-0420.
Tkach EK, White AM, Dysart KC, Waber B, Nawab US, Zhang H, et al. Comparison of intact parathyroid hormone, alkaline phosphatase, phosphate levels for diagnosing severe metabolic bone disease in infants with severe bronchopulmonary dysplasia. Am J Perinatol. 2017;34:1199–204. https://doi.org/10.1055/s-0037-1602419.
Acknowledgements
This research was supported by the Ohio Perinatal Research Network (OPRN) at Nationwide Children’s Hospital. OPRN is supported by the Center for Perinatal Research at Nationwide Children’s Hospital. Funding is provided by the Abigail Wexner Research Institute at Nationwide Children’s Hospital. No funding was received for this review.
Author information
Authors and Affiliations
Contributions
AM and JC drafted the manuscript, table, and figures. AM, JC, ST, CB, and MK participated in review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miller, A.N., Curtiss, J., Taylor, S.N. et al. A review and guide to nutritional care of the infant with established bronchopulmonary dysplasia. J Perinatol 43, 402–410 (2023). https://doi.org/10.1038/s41372-022-01578-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01578-0