Abstract
Objective
To investigate whether individuals with an elevated BMI measurement, for whom a diagnosis of overweight or obesity (OW/OB) is not recorded, are less likely to be offered clinical care for obesity compared to those with a recorded diagnosis.
Subjects
A retrospective cohort study using the electronic medical record database of Maccabi Healthcare Services (MHS) in Israel. Included were 200,000 adults with BMI ≥ 25 kg/m2 measurement recorded during a primary care visit between 2014 and 2020, and no prior diagnosis of OW/OB or related co-morbidities.
Methods
The relationships between a recorded diagnosis of OW/OB and two composite outcomes: 1. A composite of referrals to screening tests for metabolic complications; 2. A composite of weight loss intervention and follow up, were analyzed using multivariate logistic regression models.
Results
In only 18% of individuals, a diagnosis of OW/OB was recorded. After adjusting for multiple potential confounding factors, individuals who received a recorded diagnosis were 18% more likely to be offered an evaluation for obesity-related metabolic complication, (OR 1.18, 95% CI 1.15–1.21, p < 0.001), and almost twice as likely to be offered intervention and follow up for their excess body weight (OR 1.84, 95% CI 1.76–1.94, p < 0.001) compared to individuals with missed diagnosis. These results persisted after adjusting for inter-physician variability. In addition, male sex, older age, and Arab sector were all associated with lower rates of weight loss intervention and follow up, while young individuals were less likely to be screened for metabolic complications.
Conclusion
Beyond BMI measurement, a recorded diagnosis of OW/OB is associated with statistically and clinically significant higher rates of performance of obesity care and intervention. Undiagnosed OW/OB presents a significant clinical opportunity, as recording a diagnosis of OW/OB would predict improved patient access to obesity healthcare and improved clinical outcomes.

Similar content being viewed by others
Introduction
Overweight and obesity have been recognized by numerous health organizations worldwide as chronic medical conditions associated with increased risk of morbidity and mortality. OW/OB are states of excess fat mass defined by BMI, with overweight defined as BMI 25–29.9 kg/m² and obesity as BMI ≥ 30 kg/m² [1].
In the The American College of Cardiology (ACC), the American Heart Association (AHA) and The Obesity Society (TOS) guideline for the management of OW/OB in adults [2] as in several other published guidelines, the primary care setting is viewed as a critical entry point to the health care of people with OW/OB. The primary care physician/provider (PCP) is uniquely positioned to diagnose, inform, periodically monitor body weight, screen for obesity-related co-morbidities and offer a stepwise management plan and follow-up. It is therefore predicted that management of OW/OB by the PCP at an early stage would be associated with early detection of adiposity-related complications, facilitation of weight loss, and prevention of further weight gain.
Specifically, recording a diagnosis of OW/OB is a crucial step in treating this medical condition. Placing a formal diagnosis of OW/OB indicates recognition of OW/OB as a chronic condition by the PCP, payer, and patient. In addition, recording a diagnosis by PCP indirectly indicates that the PCP has discussed with the patient his current body weight, which has been shown to increase the patient’s motivation to implement certain lifestyle modifications [3, 4]. The medical record is a legal document therefore recording a diagnosis may increase the PCP’s and other healthcare providers’ sense of obligation to perform the related clinical workup and continued OW/OB care. Moreover, people with OW/OB often expect their PCP to raise and discuss the issue of body weight and offer them appropriate care [5]. Unfortunately, OW/OB diagnosis rates are relatively low, as less than 50% of individuals with obesity have a diagnosis of obesity recorded in their medical file [6, 7].
There is limited data indicating the beneficial effect of placing a diagnosis of OW/OB on obesity care of individuals with excess body weight in the primary care setting.
The objective of this study was to explore the relationship between the recording of OW/OB diagnosis and the performance of obesity care in the primary care setting, using the electronic medical record database of Maccabi Healthcare Services (MHS). The study cohort included adult patients with an elevated BMI of 25 or more, without prior diagnosis of OW/OB or obesity-related metabolic comorbidities. First, we assessed the relationship between recording a diagnosis of OW/OB and offering a clinical assessment and screening for obesity-related comorbidities, in accordance with published professional guidelines. Second, we investigated the association between the recording of a diagnosis of OW/OB and the offering of clinical interventions and follow up in the primary care setting.
Research design and methods
Study design and population
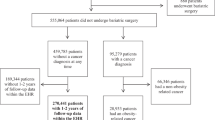
The Obesity Diagnosis Study (ODiS) is a retrospective observational study using the electronic medical record database of Maccabi Healthcare Services (MHS), the second largest HMO in Israel, serving over 1.6 million adults. Study population included adults, age ≥18 years, with a BMI ≥ 25 kg/m2 recorded during a primary care visit (the index event). Individuals who received a recorded diagnosis of OW/OB, had bariatric surgery and/or were prescribed anti-obesity medications prior to the index event were excluded from the study. Additionally, those with prior diagnoses of obesity-related complications were excluded from the study based on any one of the following: MHS’s registries of chronic diseases including cardiovascular disease, chronic kidney disease, hypertension and diabetes mellitus (the registries’ inclusion criteria are described in supplementary material S1); Coded diagnosis of either impaired fasting glucose, hyperlipidemia, or fatty liver disease; or prior diagnosis of obesity-associated cancer, such as breast, endometrial, esophageal cancers etc. [8] according to the Israeli national cancer registry (a list of obesity related cancers is presented in supplementary material S2). We excluded individuals who were filling prescriptions within 3 months prior to the index event for oral glucocorticoid [9] or second-generation antipsychotic medications [10], which are commonly prescribed medications known to cause weight gain (Table S3). Lastly, women who delivered a child within 9 months after or 6 months before the index event were excluded. Our cohort included 326,181 eligible individuals. Using the SQL function newid(), a random sample of 200,000 people was taken as the final cohort, per the institutional review board request. Data for the index date were collected between January 1st, 2014, and December 31st, 2020. Individuals were followed up until July 2021 (Fig. 1). The Maccabi Healthcare ethics committee approved the study protocol data collection and analysis, 0036-21-MHS.
The exposure variable
Recorded diagnosis of OW/OB was defined positive if either one of the following ICD10 codes was recorded by a PCP at or within seven days after the index event: E66, E66.0, E66.2, E66.3, E66.8, E66.9.
Outcome variables
Clinical assessment for OW/OB-related complications was defined as a composite outcome in accordance with clinical guidelines [2] and considered positive if all of the following occurred: (I) Blood pressure (BP) was recorded within three months of the index event; (II) fasting plasma glucose (FPG) or hemoglobin A1C (HbA1c), and (III) lipid profile were ordered, within three months after the index event.
Clinical management of obesity was defined positive if (both): (I) a referral to a dietitian, a bariatric surgery consultation, or a prescription for anti-obesity drug (Table S3) was issued within 3 months after the index event; (II) a second body weight recording between 9 to 15 months after the index event, indicating clinically relevant follow up in accordance with professional guidelines [2]. Of note, we aimed to assess parameters reflecting the PCP’s adherence to clinical guidelines, rather than patient adherence, therefore, the dependent variables correspond to drug prescription and referrals issued by the PCP, rather than the actual performance of blood tests, patient attendance at dietary consultations, or drug purchases. Of note, all Israeli citizens have medical insurance covered by the state. Primary healthcare is delivered by physicians. The number of visits with the PCP is not limited, and they are usually scheduled per patient request (i.e. annual visits are not mandatory). Periodic measurement of blood pressure and body weight are strongly advocated but not mandatory or reimbursed, neither does adding a diagnosis to the patient’s medical file. Dietary consultations are covered by medical insurance, but anti-obesity medications are not.
Covariates at baseline
Additional covariates included: sex, age, alcohol abuse, smoking status; calculated BMI, as recorded on regular clinic visits; patient sector was categorized into five categories according to their residential address at the time of the index event: Non-religious-Jewish, Jewish orthodox, Jewish-observant, Jewish-Russian immigrant, and Arab subjects; socioeconomic status (SES), based on residence at the time of the index event, coded on a 1 to 10 scale, as defined by the Israeli Bureau of Statistics [11]; Visitation to PCP during the year before the index visit; recording of an additional diagnosis at the index event other than OW/OB (i.e. reason for visit); the availability of a serum glucose test within 9 months prior to the index event; and a deidentified code assigned to each PCP at the index event.
Statistical analysis
Baseline characteristics and potential confounders distributions, according to the presence or absence of a recorded diagnosis of OW/OB, were presented as means and standard deviations for continuous variables and as frequencies and percentages for categorical variables. Chi-square tests and independent t tests were performed to compare the two groups for categorical and continuous variables, respectively. Univariate analysis of the distributions of the composite outcome variables and their components according to the presence or absence of a recorded diagnosis of OW/OB was conducted. Multivariate analysis to predict each of the two predefined composite outcomes was performed by logistic regression after adjusting for potential confounders. Adjusted odds ratios with 95% confidence intervals were calculated. The goodness of fit of the model was evaluated by the Hosmer-Lemeshow test. Data were analyzed with IBM SPSS statistics software version 28.0. (SPSS Inc. Headquarters, 233 S. Wacker Drive, 11th floor Chicago, Illinois 60606, USA). Level of significance was set at 0.05 and was two-tailed.
Results
Among 1,678,143 adult members of MHS, 977,326 had a BMI measurement of 25 or more during the study period. After excluding individuals who had a recorded diagnosis of OW/OB on their medical file before the index date, and those who had metabolic obesity-related comorbidities, or any one of the other exclusion criteria as described in methods, 326,181 people were eligible for the study, of which a random sample of 200,000 was analyzed (Fig. 1).
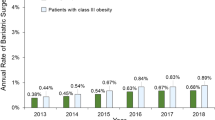
In this final cohort, the average age was 37.5, and average BMI was 28.8. 26% of the individuals had obesity, with BMI over 30, and 56.7% were male (Table 1). Within the study cohort only 18.0% of the subjects received a recorded diagnosis of OW/OB by their PCP at or immediately after the index event. Subjects with higher BMI were more likely to receive an OW/OB diagnosis: only 12.0% of the individuals with overweight, received a recorded diagnosis of OW/OB, compared to almost 50% of the people with obesity class III, BMI ≥ 40. People with a recorded OW/OB diagnosis were younger, more likely to be women, and had a higher BMI by 2.8 units on average, compared to people with OW/OB who did not receive a recorded diagnosis. Individuals with elevated BMI who had a recorded OW/OB diagnosis were less likely to visit their PCP during the year prior to the index event, and more likely to receive a new, non-OW/OB diagnosis at the index event, in contrast to those with missed diagnosis. In the study cohort, most subjects were non-religious Jewish adults, with less than 10% being Arab. There were minimal differences in socioeconomic status and sectorial representation between the two groups.
Overall, 56.8% of the subjects were issued referrals for fasting serum glucose levels, 48.8% were issued referrals for lipid profile blood tests, 75% of the subjects had their blood pressure taken at or immediately after the index event (Table 2). In the univariate analyses, people with OW/OB who received a recorded diagnosis of OW/OB vs those who did not, had a higher rate of the first composite outcome, 54.4% vs 45.9%. Surprisingly, individuals who received a recorded diagnosis of OW/OB were less likely to have their blood pressure taken. Overall, only 16.8% of the individuals in this cohort were issued referrals for a consultation with a nutritionist, 0.3% were issued a prescription for anti-obesity medication, 0.2% were referred to a consultation with a bariatric surgeon and 18.8% had a repeated weight measurement after a year. In the univariate analysis, individuals who had a recorded diagnosis of OW/OB had a higher rate of the second composite outcome event of obesity care, 9.4% vs. 3.3% in the control group. The event rate of each of the components of the second composite outcome was higher among individuals with a recorded diagnosis of OW/OB compared to the control group: they were more likely to be issued referrals for consultation with a nutritionist (31.0% vs. 13.7%), bariatric surgeon (0.5% vs. 0.1%), prescribed an anti-obesity medication (0.4% vs. 0.3%) or have a repeated body weight measurement after a year (26.4% vs. 17.1%).
After adjustment for potential confounders, there was a significant association between having a recorded diagnosis of OW/OB and the first composite outcome. In the multivariate analysis, people who were diagnosed with OW/OB by the PCP were 18% more likely to receive a clinical and biochemical evaluation for obesity-related metabolic complication, (OR 1.18, 95% CI 1.15–1.21, p value < 0.001). (Fig. 2, upper panel). Adjusting the model for two additional covariates, having an additional diagnosis recorded at the index event, and blood chemistry tests performed within 9 months prior to the index event, did not significantly affect this association (OR = 1.18, CI 1.15–1.21, p value < 0.001, table not shown). We also considered the possibility that clustering of patients within physician groups could potentially affect the study results. Therefore, we performed a sensitivity analysis with a generalized estimating equation to account for within-physician correlations, which did not affect the observed association (OR = 1.17, 95% CI 1.14–1.20, p value < 0.001, Table S4a). A subgroup analysis, including only individuals with obesity, BMI ≥ 30 kg/m2, showed similar results (OR 1.22, 95% CI 1.17–1.27, p value < 0.001, table not shown). According to our main model, BMI was a strong independent predictor of the first composite outcome, as with each increase of 1 unit of BMI there was a 6% increase in chances of being offered a clinical evaluation. In addition, older age, and male sex, were both associated with a higher likelihood, while having a visit with a PCP in the prior year was associated with lower likelihood of receiving a clinical assessment. Sector was another significant predictor of the composite outcome, as Orthodox- Jewish, observant-Jewish, and Arab individuals were less likely to be offered clinical and biochemical assessment compared to non-religious-Jewish individuals. The association between OW/OB diagnosis and the first composite outcome remained stable and statistically significant across different categories of age and BMI (Fig. S5).
Performance of clinical assessment of obesity-related complications, the first composite outcome (upper panel), and performance of obesity management and follow up, the second composite outcome (lower panel). *For every 5 years increase in age; †for every 1 unit increase in BMI measured at visit. OW/OB, overweight or obesity.
The association between OB/OW diagnosis and the second composite outcome of obesity care was analyzed in the multivariate regression model. After adjustment for multiple potential confounders, a recorded diagnosis of OW/OB was an independent predictor of the second composite outcome, with almost twofold increase in the performance rates of clinical weight management (OR 1.84, 95% CI 1.76–1.94, p value < 0.001) (Fig. 2, lower panel). A subgroup analysis, including only individuals with obesity, BMI ≥ 30 kg/m2, showed similar results (OR 1.66, 95% CI 1.56–1.77, p value < 0.001, table not shown). Adjusting the model for having a non-OW/OB diagnosis recorded at the index event did not significantly affect the results (OR = 1.84, 95% CI 1.75–1.93, p value < 0.001, table not shown). A sensitivity analysis was performed with a generalized estimating equation to account for within-physician correlations, which did not affect the observed association between OW/OB recorded diagnosis and obesity care (OR = 1.79, CI 1.70–1.89, p value < 0.001, Table S4b). The association between recorded OW/OB diagnosis and the second composite outcome remained stable and statistically significant across different categories of age and BMI (Fig. S6). The main model pointed out additional predictors: male sex compared to female was associated with a 53% reduction in the likelihood of the second composite outcome. Sector was another strong independent predictor, as Arab people with OW/OB were 44% less likely whereas Orthodox- Jewish people were 44% more likely to be offered clinical care and follow up for their excess body weight compared to the reference group of non-religious Jewish individuals. Lastly, younger age and higher BMI were both independent positive predictors for the second composite outcome.
Discussion
In this retrospective analysis of 200,000 individuals with excess body weight, those receiving a new recorded diagnosis of OW/OB were 18% more likely to be referred for screening tests for obesity-related metabolic complications, and almost twice as likely to be offered weight loss intervention and follow up compared to individuals who did not receive a recorded diagnosis. These results were highly significant and persisted also after adjustment for multiple potential confounders. In addition, male sex, older age, and Arab sector were all associated with lower rates of weight loss intervention and follow up, while young individuals were less likely to be screened for metabolic complications.
To the best of our knowledge, the current study is the first to show an association between the recording of OW/OB diagnosis and higher performance rates of clinical assessment of OW/OB- associated comorbidities. Compared to individuals with normal weight, people with obesity are at a higher risk for developing multi-morbidities across the BMI range even at the age of 30 [12]. Failure to timely diagnose OW/OB and screen for associated metabolic complications is a public health concern. Rapid weight gain is common among young adults [13], and is associated with increased risk for metabolic complications [14,15,16]. There are very limited data on the association between recorded diagnosis of OW/OB and performance of obesity care by medical staff. In a single-center retrospective report by Bardia et al., diagnosis of obesity was a strong predictor of formulation of an obesity treatment plan (OR = 2.39) [17]. In another small study by Banerjee et al., adding a diagnosis of obesity to the patient’s problem list was associated with increased likelihood of providers addressing obesity at future visits [18].
In this cohort of Israeli population with excess body weight, we report a relatively low rate of OW/OB diagnosis recording at or immediately after measuring an elevated BMI in alignment with previous studies, reporting low diagnosis rates especially among men [6, 17, 19, 20]. Recording a diagnosis may encourage the PCP and other healthcare providers to be proactive and offer additional workup and continued care.
This has been demonstrated in other chronic diseases. In a study by Gopalan et al. patients with type 2 diabetes, who received an ICD coded diagnosis of diabetes vs those who did not, were more likely to receive screening for vascular complications, foot care, and anti-diabetic pharmacotherapy [21]. According to ACC/TOS guidelines, screening for obesity-related comorbidities should be repeated annually, yet other professional guidelines suggest lower frequency of screening [22, 23]. In this study, adjusting the model for the availability of laboratory tests within 9 months prior to the index event did not affect the analysis result. We therefore conclude that higher rates of referrals to metabolic screening among patients with a recorded diagnosis of OW/OB cannot be attributed to lower availability of prior blood work. More than 60% of the subjects had a non-OW/OB diagnosis placed during the index event, which might suggest that the reason for most visits was non-weight-related and could partially explain the low rates that obesity care was offered. However, adjusting for this covariate did not considerably change the association. In this cohort, those who received a recorded diagnosis of OW/OB were less likely to have a visit with a PCP in previous year compared to the control group, despite having a higher BMI. This finding is somewhat surprising as previous studies reported BMI as a predictor of increased utilization of healthcare services, an association which was mostly driven by higher prevalence of chronic morbidity among people with elevated BMI [24, 25]. There are several possible explanations for this observation: Our cohort included only patients who did not have obesity-related comorbidities, and had a relatively low representation of people with severe obesity, class II and III; Patients who received a diagnosis were younger than the control group; Lastly, people with higher BMI could be prone to weight bias, which may negatively affect healthcare utilization, and postpone visits at the primary care clinic [26]. Their elevated BMI and lower healthcare utilization rates could also explain why those who received OW/OB diagnosis were more likely to have another diagnosis recorded at the index event compared to the control group. The reasons for primary healthcare utilization among patients with elevated BMI are beyond the scope of this work. Only 4.4% of the individuals were offered clinical care and follow-up in accordance with published guidelines. These low rates could be related to PCPs’ perceptions regarding their role in obesity care [27], and the reported ineffectiveness of obesity control efforts in the primary care setting [28, 29], which may lead to failure to recognize OW/OB and offer relevant clinical care. One could argue that recording a diagnosis is not by itself a trigger for management, and simply reflects the physician’s own bias, as some physicians are more interested than others in addressing obesity in their daily practice [30]. In the multivariate regression models, we noticed a differential effect of sex on the first and second outcomes: Male patients were more likely to receive clinical evaluation for obesity-related metabolic comorbidities, while female patients were more likely to have the second outcome of being offered weight loss intervention and follow up. These findings are consistent with other publications reporting higher rates of screening for cardiovascular risk factors in male patients [31, 32], while women are more likely to have their body weight measured [33] and to receive a prescription for anti-obesity drugs or referral to dietary consultation from their primary care provider [32, 34]. These sex differences could be related to physician bias as well as patient concern.
Adjusting our model for the PCP’s de-identified code allowed us to indirectly account for the inter-physician variability and did not affect the study results. To the best of our knowledge this is the first study to show the importance of recorded diagnosis irrespective of physician characteristics, in the management and care of people with OW/OB.
Ciemins et al. reported in a retrospective study that the recording of obesity diagnosis for patients with BMI of 30 or more was an independent predictor of achieving 5% weight loss after 1 year [6]. In their study, prescribing an anti-obesity medication, which reflects one of the aspects of obesity care offered by the physician, was a strong predictor of weight loss. After adjusting for anti-obesity drug prescription, obesity diagnosis was associated with a 30% increase in the likelihood of achieving a 5% weight loss or more. Their report suggests that both recorded diagnosis and physician performance increase the likelihood of weight loss. Taken together with the results of the current study, improving rates of OW/OB diagnosis recording in the primary care setting, for example by implementing automated dashboard notifications when elevated BMI is recorded [35], could increase PCP’s involvement and active role in obesity care and potentially lead to improved weight loss and metabolic outcomes.
Our study has several limitations. The analysis did not include data on free-text clinical notes, and therefore it is possible that OW/OB were verbally diagnosed or discussed during the visit, without placing a coded diagnosis, which might have led to underestimation of the association between OW/OB diagnosis and performance of obesity care by the PCP. Whether the concern of excess weight at the index event was raised by patient or physician, is a possible confounder, which this analysis did not account for. Of note, the study was conducted before the introduction and regulatory approval of new potent pharmacological interventions for obesity in clinical practice. It is possible that in coming years as effective pharmacological interventions will become widely accepted by both patient, PCP and provider, there will be an increase in the rate of OW/OB diagnosis and medical care. The goal of obesity care is to achieve weight loss and reduce future obesity related morbidity. The question whether a formal diagnosis of OW/OB by itself or performance of obesity care by the PCP leads to actual patient weight loss or prevention of obesity related complications, was not addressed in the current study, and will be the focus of our future work. Lastly, the study represents parameters of physician performance at the primary care setting in Israel, and therefore may not apply to other primary care settings around the world.
In conclusion, our study presents a strong association between the recording of OW/OB diagnosis and the offering of clinical screening and especially management for people with OW/OB in the primary care setting. Taken together, the high rates of undiagnosed OW/OB present a significant clinical opportunity, as recording a diagnosis of OW/OB would predict higher PCP’s engagement and obligation to offer obesity clinical care. Whether a recorded diagnosis of OW/OB is associated with weight control and prevention of OW/OB related complications warrants further investigation and will be the focus of our next studies.
Data availability
In accordance with the Israeli Ministry of Health regulations, individual-level data cannot be shared openly. Specific requests for remote access to de-identified community-level data should be directed to KSM, Maccabi Healthcare Services Research and Innovation Center.
References
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–66.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129:S102–38.
Dicker D, Alfadda AA, Coutinho W, Cuevas A, Halford JCG, Hughes CA, et al. Patient motivation to lose weight: importance of healthcare professional support, goals and self-efficacy. Eur J Intern Med. 2021;91:10–6.
Jackson SE, Wardle J, Johnson F, Finer N, Beeken RJ. The impact of a health professional recommendation on weight loss attempts in overweight and obese British adults: a cross-sectional analysis. BMJ open. 2013;3:e003693.
Dicker D, Kornboim B, Bachrach R, Shehadeh N, Potesman-Yona S, Segal-Lieberman G. ACTION-IO as a platform to understand differences in perceptions, attitudes, and behaviors of people with obesity and physicians across countries - the Israeli experience. Isr J health policy Res. 2020;9:56.
Ciemins EL, Joshi V, Cuddeback JK, Kushner RF, Horn DB, Garvey WT. DiagNosing Obesity As A First Step To Weight Loss: An Observational Study. Obes (Silver Spring, Md). 2020;28:2305–9.
Baer HJ, Karson AS, Soukup JR, Williams DH, Bates DW. Documentation and diagnosis of overweight and obesity in electronic health records of adult primary care patients. JAMA Intern Med. 2013;173:1648–52.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer-viewpoint of the IARC working group. N Engl J Med. 2016;375:794–8.
Morin C, Fardet L. Systemic glucocorticoid therapy: risk factors for reported adverse events and beliefs about the drug. A cross-sectional online survey of 820 patients. Clin Rheumatol. 2015;34:2119–26.
Bak M, Fransen A, Janssen J, van Os J, Drukker M. Almost all antipsychotics result in weight gain: a meta-analysis. PloS One. 2014;9:e94112.
Characterization and Classification of Geographical Units by the Socio-Economic Level of the Population 2017. In: Statistics CBo, editor. Jerusalem2020.
Kivimäki M, Strandberg T, Pentti J, Nyberg ST, Frank P, Jokela M, et al. Body-mass index and risk of obesity-related complex multimorbidity: an observational multicohort study. lancet Diabetes Endocrinol. 2022;10:253–63.
Malhotra R, Ostbye T, Riley CM, Finkelstein EA. Young adult weight trajectories through midlife by body mass category. Obes (Silver Spring, Md). 2013;21:1923–34.
Kodama S, Horikawa C, Fujihara K, Yoshizawa S, Yachi Y, Tanaka S, et al. Quantitative relationship between body weight gain in adulthood and incident type 2 diabetes: a meta-analysis. Obes Rev. 2014;15:202–14.
Jayedi A, Soltani S, Motlagh SZ, Emadi A, Shahinfar H, Moosavi H, et al. Anthropometric and adiposity indicators and risk of type 2 diabetes: systematic review and dose-response meta-analysis of cohort studies. BMJ (Clin Res ed). 2022;376:e067516.
Twig G, Afek A, Derazne E, Tzur D, Cukierman-Yaffe T, Gerstein HC, et al. Diabetes risk among overweight and obese metabolically healthy young adults. Diabetes care. 2014;37:2989–95.
Bardia A, Holtan SG, Slezak JM, Thompson WG. Diagnosis of obesity by primary care physicians and impact on obesity management. Mayo Clin Proc. 2007;82:927–32.
Banerjee ES, Gambler A, Fogleman C. Adding obesity to the problem list increases the rate of providers addressing obesity. Fam Med. 2013;45:629–33.
Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003-2008 Study. Int J Obes. 2011;35:1063–70.
Cyr PR, Haskins AE, Holt C, Hanifi J. Weighty problems: predictors of family physicians documenting overweight and obesity. Fam Med. 2016;48:217–21.
Gopalan A, Mishra P, Alexeeff SE, Blatchins MA, Kim E, Man AH, et al. Prevalence and predictors of delayed clinical diagnosis of Type 2 diabetes: a longitudinal cohort study. Diabet Med. 2018;35:1655–62.
Stegenga H, Haines A, Jones K, Wilding J. Identification, assessment, and management of overweight and obesity: summary of updated NICE guidance. BMJ (Clin Res ed). 2014;349:g6608.
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192:E875–e91.
Evans M, de Courcy J, de Laguiche E, Faurby M, Haase CL, Matthiessen KS, et al. Obesity-related complications, healthcare resource use and weight loss strategies in six European countries: the RESOURCE survey. Int J Obes. 2023;47:750–7.
Rimes-Dias KA, Costa JC, Canella DS. Obesity and health service utilization in Brazil: data from the National Health Survey. BMC public health. 2022;22:1474.
Alberga AS, Edache IY, Forhan M, Russell-Mayhew S. Weight bias and health care utilization: a scoping review. Prim Health Care Res Dev. 2019;20:e116.
McHale CT, Laidlaw AH, Cecil JE. Primary care patient and practitioner views of weight and weight-related discussion: a mixed-methods study. BMJ open. 2020;10:e034023.
Kaplan LM, Golden A, Jinnett K, Kolotkin RL, Kyle TK, Look M, et al. Perceptions of barriers to effective obesity care: results from the national ACTION Study. Obes (Silver Spring, Md). 2018;26:61–9.
Madigan CD, Graham HE, Sturgiss E, Kettle VE, Gokal K, Biddle G, et al. Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ (Clin Res ed). 2022;377:e069719.
Kraschnewski JL, Sciamanna CN, Pollak KI, Stuckey HL, Sherwood NE. The epidemiology of weight counseling for adults in the United States: a case of positive deviance. Int J Obes. 2013;37:751–3.
Krähenmann-Müller S, Virgini VS, Blum MR, da Costa BR, Collet TH, Martin Y, et al. Patient and physician gender concordance in preventive care in university primary care settings. Preventive Med. 2014;67:242–7.
Naicker K, Liddy C, Singh J, Taljaard M, Hogg W. Quality of cardiovascular disease care in Ontario’s primary care practices: a cross sectional study examining differences in guideline adherence by patient sex. BMC Fam Pract. 2014;15:123.
Nicholson BD, Aveyard P, Bankhead CR, Hamilton W, Hobbs FDR, Lay-Flurrie S. Determinants and extent of weight recording in UK primary care: an analysis of 5 million adults’ electronic health records from 2000 to 2017. BMC Med. 2019;17:222.
Patterson L, Kee F, Hughes C, O’Reilly D. The relationship between BMI and the prescription of anti-obesity medication according to social factors: a population cross sectional study. BMC public health. 2014;14:87.
Patel MS, Kurtzman GW, Kannan S, Small DS, Morris A, Honeywell S, et al. Effect of an automated patient dashboard using active choice and peer comparison performance feedback to physicians on statin prescribing: the PRESCRIBE cluster randomized clinical trial. JAMA Netw Open. 2018;1:e180818.
Acknowledgements
The ODiS study was supported by an independent grant from Novo Nordisk, LTD, funding the statistical analysis and the processing charges. The company did not take any part in study design, analysis interpretation of the data, or manuscript drafting.
Funding
Open access funding provided by Tel Aviv University.
Author information
Authors and Affiliations
Contributions
MKM contributed to study concept and design, analysis and interpretation of the data and manuscript drafting. SE contributed to study design, drafted manuscript figures and tables, reviewed, and edited the manuscript. TCY contributed to study design, discussion, reviewed, and edited the manuscript. DO contributed to study concept and design, researched data, contributed to discussion, reviewed, and edited the manuscript. All authors approved the final version of the manuscript, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
MKM reports receipt of speaker fees from Novo Nordisk, LTD, Eli Lilly; Sanofi and Boehringer Ingelheim. DO reports receipt of speaker fees from Novo Nordisk, LTD and Boehringer Ingelheim. SE reports no CI. TCY reports receipt of speaker fees from Novo Nordisk, LTD, Eli Lilly; Sanofi and Boehringer Ingelheim, Medtronic, Merck Sharp & Dhome and AstraZeneca.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kasher Meron, M., Eizenstein, S., Cukierman-Yaffe, T. et al. Missed diagnosis—a major barrier to patient access to obesity healthcare in the primary care setting. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01514-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41366-024-01514-6