Abstract
Background
The rapid rise in obesity rates among school children in Latin America and the Caribbean (LAC) could have a direct impact on the region’s physical and mental health, disability, and mortality. This review presents the available interventions likely to reduce, mitigate and/or prevent obesity among school children in LAC by modifying the food and built environments within and around schools.
Methods
Two independent reviewers searched five databases: MEDLINE, Web of Science, Cochrane Library, Scopus and Latin American and Caribbean Health Sciences Literature for peer-reviewed literature published from 1 January 2000 to September 2021; searching and screening prospective studies published in English, Spanish and Portuguese. This was followed by data extraction and quality assessment using the Cochrane risk-of-bias tool (RoB 2) and the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I), adopting also the PRISMA 2020 guidelines. Due to the heterogeneity of the intervention’s characteristics and obesity-related measurements across studies, a narrative synthesis was conducted.
Results
A total of 1342 research papers were screened, and 9 studies were included; 4 in Mexico, and 1 each in Argentina, Brazil, Chile, Colombia, and Ecuador. Four studies reported strategies for modifying food provision; four other targeted the built environment, (modifying school premises and providing materials for physical activity); a final study included both food and built environment intervention components. Overall, two studies reported that the intervention was significantly associated with a lower increase over time in BMI/obesity in the intervention against the control group. The remaining studies were non-significant.
Conclusions
Data suggest that school environmental interventions, complementing nutritional and physical education can contribute to reduce incremental childhood obesity trends. However, evidence of the extent to which food and built environment components factor into obesogenic environments, within and around school grounds is inconclusive. Insufficient data hindered any urban/rural comparisons. Further school environmental intervention studies to inform policies for preventing/reducing childhood obesity in LAC are needed.
Similar content being viewed by others
Introduction
Globally, childhood overweight and obesity rates has increased substantially over recent decades [1]. In Latin America and the Caribbean (LAC), three out of ten children aged 5–19 years are living with overweight or obesity [2]. The consequences of childhood obesity have been well studied and include detrimental health [3], cognitive development and educational attainment [4], and increased risk of developing cardiovascular diseases and obesity in adulthood [5, 6]. The rapid nutritional transition in the LAC region due to urbanisation, economic growth and transformation of broad food systems [7, 8], has had a direct effect on the rising childhood obesity rates. Dietary changes, including higher intakes of energy-dense and low-nutrient-density foods such as sugar-sweetened beverages (SSB) as well as the lower intakes of vegetables and legumes, and higher physical inactivity and sedentary behaviours (SB) among children and adolescents in LAC have contributed to the rapid increase in obesity and overweight among children and adolescents [9].
Obesogenic environments, defined as ‘the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations’ [10], have impacted children and adults across the world. Previous systematic reviews have focused primarily on assessing the association between the neighbourhood food and built environment (BE), and adiposity and/or weight status among children and adults [11,12,13,14]. However, as children spend much of their weekday time at schools, and a large proportion of their energy intake and expenditure occurs in this setting [15]; more information is needed about the role of schools in childhood obesity. This is the context for our LAC-focused systematic review that provides a valuable contribution, particularly given that several studies suggest that developing interventions at the school level can contribute to prevention and/or reduction in overweight and/or obesity among children and adolescents [16, 17].
School-based interventions have mostly focused on improving the nutritional education curriculum by delivering workshops and information (booklets, pamphlets, posters) for improving dietary behaviours, and increasing physical activity (PA) and/or reducing SB by modifying physical education (PE) sessions [18]. Several systematic reviews, including mostly high-income countries, have reported inconsistent results on the effectiveness of only educational interventions at preventing increases in body weight status [19,20,21], but some reductions in adiposity or body composition measurements have been reported [18, 22,23,24]. Interventions combining diet and PA components, targeting the school and home settings and with longer follow-up, tend to be more successful in preventing or managing weight gain, compared to single component or setting and with a shorter intervention length [19, 23, 25]. Most of the reviews assessing the effectiveness of school-based interventions do not analyse the results according to school level [22, 24]. A large review separated results between preschool and school-based (primary to secondary school) interventions, however, few studies were conducted among preschool settings to provide any conclusion [25]. Two reviews including mostly primary school-aged children found some positive evidence for educational interventions at reducing but not preventing childhood obesity [18, 23].
Systematic reviews focusing on school environments are more limited compared with those focusing only on educational components. A recent systematic review and meta-analysis assessed the effectiveness of the school food environment for preventing childhood obesity [26]. Results showed that interventions including a food environment component had a significant and meaningful effect on adiposity (body mass index (BMI) z-score). This review included worldwide intervention studies published in English, identifying only one conducted in a LAC country and used a broad definition of food environment, including social marketing and changes to the schools’ dietary guidelines, together with interventions targeting the food provision and the nutritional composition of food available at schools. A previous review assessing only isolated school food environment interventions (regulations and food provision) in the US and UK concluded that the two interventions included were successful in preventing increases in BMI in the treatment group [27].
The different definitions of school food environments provided by previous reviews included all food and drink available to students within the school [27], and all information influencing food choice and physical aspects of the food environment, such as availability and accessibility of food within spaces, infrastructure and conditions within or around schools [26]. Our review uses the International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support (INFORMAS) framework [28]. We also identified dimensions from the WHO School Policy Framework [29] to define the BE within and around the educational premises affecting PA and/or SB to prevent/reduce childhood overweight or obesity. Both frameworks provide a comprehensive and internationally agreed definition for understanding the influence of school environments on childhood obesity. Furthermore, interventions targeting specific aspects of school’s food and BE can provide low-cost and easily scaled-up strategies for tackling childhood obesity [27]. Making our review particularly relevant for policymakers looking to capitalise on evidence from already available intervention studies.
To this end, our aim is to systematically assess the effectiveness of interventions and policies targeting the school environments for preventing/reducing overweight or obesity among school children in LAC. In particular, we aim to answer the question: Are school environment interventions/policies effective in the reduction/prevention of obesity and/or overweight among school-age students from LAC? When available, effectiveness will be compared according to the environmental intervention type (food and/or BE), intervention length, and participant’s gender and age groups.
Methods
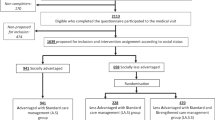
The protocol for this systematic review was registered in PROSPERO (CRD42021285247), and we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [30] (Fig. 1 and Supplementary Table 1).
Eligibility
Given our focus on LAC, peer-reviewed literature published in English, Spanish and Portuguese, from 1 January 2000 to September 2021 were eligible for inclusion. Prospective studies, including interventional study designs containing randomised/non-randomised controlled trials (RCTs and non-RCTs) and, cohort studies comparing changes in overweight and/or obesity measurements, after a school environment intervention/policy had been implemented, were included.
Search strategy
The team conducted searches in duplicate in five electronic databases: MEDLINE (via PubMed), Web of Science, Cochrane Library, Scopus and the Latin American and Caribbean Health Sciences Literature. Search terms and strategies for each database are in Supplementary Tables 2–7. Retrieved reports were stored in EPPI-Reviewer [31] and duplicates were identified and excluded. We hand-searched relevant systematic reviews’ references and included research papers to identify and incorporate relevant additional studies.
Screening, data extraction and quality assessment
MJV-S and AH-A, both fluent in English and Spanish as well as a good level of Portuguese, conducted title and abstract screening and full-text selection in duplicate. They also pilot tested the first 200 titles and abstracts, obtaining a moderate inter-rate agreement between reviewers (Kappa = 0.53) [32, 33]. Clarifications were made to the inclusion criteria with the whole team and the remaining title and abstract screening completed, obtaining an excellent agreement rate (Kappa = 0.74). All discrepancies and full texts in Portuguese were discussed with a third reviewer fluent in this language (RN).
Data extraction was performed independently (MJV-S and AH-A) in EPPI-Reviewer using a piloted coding tool and included the following data: publication details (authors, title, journal, year of publication), study details (study design, RCT characteristics (grouping, randomisation, allocation), sampling method, country, school setting, school area (urban/rural), data collection date (baseline and follow-up)), participant information (age, school level, gender/sex, ethnicity, and socioeconomic characteristics, number of participants at baseline and follow-up), intervention details (type of intervention, components, duration, theory), outcome data (measurement type, data collection tool, baseline and follow-up measurements), and effectiveness of intervention. Authors from five studies were contacted for clarifications and one sent the required information [34, 35]. When results were presented in plots only, the software Plot Digitizer was used for extracting data [36].
Study quality assessment was undertaken independently (MJV-S and AH-A) by using the Cochrane Risk of Bias tool for cluster RCT (RoB 2 C-RCT) [37, 38], and the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) [39] for non-randomised trials. Studies were graded as low, unclear or high risk of bias. For C-RCTs, six domains were assessed: randomisation, timing of identification and recruitment of participants, deviations from intended interventions, missing outcome data, measurement of outcomes and selection of the reported result. For non-RCTs, seven domains were assessed: confounding, selection of participants, classifications of interventions, deviations from intended interventions, missing data, measurement of outcomes and selection of the reported result. Risk of bias assessment by domains for each individual study is then presented in plots [40].
Types of interventions
All interventions, including the introduction of policies, and/or regulations aiming at modifying obesity/overweight by changing food and/or BE within and around the schools were included. Food environment dimensions were defined by the INFORMAS framework [28]: food composition, labelling, marketing, provision, retail, prices and, trade and investments. These dimensions can influence population health, diet and body weight, and can be modified by public and private sector policies. In addition, we used the WHO School Policy Framework [29] to define two dimensions of the BE: educational buildings and facilities, and walking and cycling infrastructure from and to the educational establishment. Studies assessing interventions in close proximity to schools were included if conducted within a one-mile radius around the perimeter of the educational establishment. Interventions regardless the length of follow-up were included. To avoid duplication of data analysis, only the most recent follow-up time including the population relevant to this review was included in the results.
Outcomes
All kinds of overweight and/or obesity measurements, including those derived from weight and height (e.g., BMI, standard deviation scores, Z-score, prevalence of overweight and obesity, ponderal index), waist circumference and body fat (e.g., body fat percentage, intra-abdominal fat, subcutaneous fat, visceral fat, skin-fold thickness), were included.
Data analysis
We performed a narrative synthesis containing the summary of findings over the effect of interventions on obesity-related measurements, reporting the effectiveness of interventions either as mean difference, risk ratio or odds ratio, accordingly to the type of measurement reported in each individual study. We summarised data according to the intervention components reported by each study, classifying it either as a food or, a built and physical environmental intervention. Due to the large heterogeneity in intervention components and multiple outcomes measured across studies, a meta-analysis was not feasible.
Results
Figure 1 shows the PRISMA 2020 flow diagram [30] used for the process of the study selection. The search strategies retrieved 1329 unique titles and abstracts, and 13 records were added from searching the reference list of relevant reviews and of the included research papers. In total, we assessed 40 full texts for eligibility and 9 studies were included. One study was conducted in 2005 [41], another in 2008 [42], and the remaining seven were conducted after 2010. Four studies were in Mexico, while individual studies were in Argentina, Brazil, Chile, Colombia, and Ecuador. Seven studies included girls and boys from primary education, and two included adolescents from lower secondary education [34, 43], classified according to the International Standard Classification of Education [44]. Sample sizes at baseline varied from 168 to 2682 children, and 120 to 1224 at follow-up.
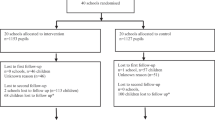
Seven studies used a C-RCT design, and another two a longitudinal quasi-experimental design (LQE). Clusters selected (schools) varied from 1 per intervention and 1 per control, to 30 schools in each group. All studies compared changes in control and treatment groups between baseline and follow-up. Follow-up measurements varied from ten weeks to three years. Table 1 summarises the study characteristics of the seven studies.
In terms of bias, six out of the seven C-RCT presented a low risk of bias, and one presented some concerns due to the reporting of outcomes. The two LQE studies presented serious concerns related to baseline and time-varying confounding. Figures 2 and 3 summarise the risk of bias assessment.
Overall, four studies reported intervention components for modifying the food environments and four studies, the BE (Table 2). Only one study reported components for both food and BE interventions [45]. Obesity-related outcomes were heterogeneous across the studies, including reports of BMI, BMI z-score and, overweight and/or obesity prevalence. The following sections present a detailed description of the design and results of included interventions targeting (a) the food environment (b) BEs, and (c) a combination of food and BEs.
Food environments
Four studies included intervention components targeting the food environments of the schools. Following the INFORMAS dimensions, four studies targeted food provision by increasing the availability of healthy products, while one limited the sales of high-energy and unhealthy foods [45]. Only the study by Ramírez-López et al. [41] assessed one component intervention, targeting the food composition of free school breakfasts (FSB), while the remaining three studies had several other intervention components, including strategies around nutritional and PE. Some studies reported more than one obesity-related measurement; BMI outcomes and BMI z-score were both reported together by two studies, body fat percentage and fat-free body mass were presented in one study, and overweight and obesity prevalence was reported by one study. One study was conducted in urban areas (Rosario), one in a rural setting (Metropolitan region of Santiago), one in a semi-rural (State of Mexico), and a final one comprising a large region (the State of Sonora) and including both rural and urban contexts.
The C-RCT by Alvirde-García [46] included students aged 9–10 years at baseline attending five semi-rural schools in the State of Mexico. The food provision component included a modification to the food items offered in school canteens by increasing the availability of fruits and vegetables and products low in saturated fat and sugar. In addition, the intervention included a nutritional and PA education component, delivering workshops with parents, school staff and school vendors, and booklets for students to complement their school curriculum. Results showed a similar (average) increase of BMI over time in the treatment group compared to the control group during the first 2 years, but a significantly lower rate of increase in (average) BMI among those in the treatment group, compared to the control group, for the third year of the intervention (1.6 ± 1.9 vs. 1.9 ± 1.7 kg/m2, p < 0.01). Despite both groups decreasing their energy intakes over time, in the third year this decrease was significantly higher among the intervention or treatment group compared with the control one (−756 kcal/d, p < 0.05).
The LQE study by González et al. [47] included preschool to 8th-grade students (4–15 years) from six schools located in rural areas of the Metropolitan region of Santiago, Chile. All students from five schools located in the same municipality received the year-long intervention, whereas students from one school in a different municipality were assigned to a control group. Students from the treatment group received fruits three times-per-week and a fruit basket was given to the family at the end of the year. This intervention also included workshops with nutritional education material for the students, their parents, and teachers. At the end of the year, results did not show any significant change in body weight status among participants in the control or treatment groups. However, the intervention was successful in increasing the frequency of daily intakes of fruits, vegetables, dairy products, pulses and fish, but was ineffective in reducing the consumption of unhealthy foods such as chips, hotdogs and pizza. Authors highlight the lack of increase in overweight or obesity status in treatment groups, considering the higher intake of healthy products that might contribute to increasing energy intakes.
The year-long quasi-experimental study by Ramírez-López et al. [41] included 1st- to 5th-grade students (6–10 years) from urban and rural areas in the state of Sonora, Mexico. The intervention assessed the effect of a national-and-state-funded FSB programme on obesity, body composition and cardiovascular risk, compared to non-beneficiaries’. This was the only study assessing one intervention component (i.e., provision of an FSB). Results showed that FSB beneficiaries did not differ in overweight or obesity prevalence, BMI, or body fat percentage, from those in the control group at the end of the 9-month intervention. Similarly, no major differences between groups were reported for total cholesterol, triglycerides, and glucose.
The C-RCT by Rausch Herscovici et al. [42] included students aged 9–11 years attending six schools in urban areas in Rosario, Argentina. The food provision intervention modified the school canteen options to include healthy food items (fruits, orange juice and low-sugar cereal). In addition, the intervention included three nutritional and PE workshops for children and one for parents. Results after 6 months showed no significant difference in BMI between the intervention and control groups. However, girls in the experimental group (not the boys) increased their consumption of some healthy foods targeted by the intervention (skim milk and orange juice), compared to their control group counterparts.
Built environments
Among the four interventions targeting the BE, one study intervened in the school playground, and three studies provided materials for promoting PA within the school premises. Studies could report more than one obesity-related measurement; BMI was reported in one study, BMI z-score was reported in three studies, and overweight and obesity prevalence was reported in another study. Four studies included schools located in urban areas (in the secondary cities of Cuenca and Fortaleza, and the capital city of Bogota), while only one study covered both rural and urban areas (State of Sonora).
The 3-year C-RCT by Andrade et al. [43] included 12- and 13-year-old adolescents attending 20 schools in urban areas of Cuenca, Ecuador, and involved a BE intervention with a walking trail drawn on the playground in the second year of the intervention. Other components included nutritional and PE materials (booklets and posters), workshops for adolescents and their parents, and the organisation of social events with famous athletes. After 3 years of intervention, no effects were reported for mean BMI z-score or prevalence of overweight between control and treatment groups. However, students in the treatment group showed a positive effect on physical fitness parameters (vertical jump and speed shuttle run) and a higher percentage met the PA recommendations (60 min of MVPA/day), compared to students allocated to the control groups (6 vs. 18 percentage points, p < 0.01).
The 4-month C-RCT by Barbosa Filho et al. [34, 35] involved 11- to 13-year-old adolescents in six schools in urban areas of Fortaleza, Brazil. The BE intervention offered space and PA equipment (balls, rackets, mini courts) to promote PA during free time. Other components involved health and PE training and materials (booklets, interactive media, posters) for teachers to include in the school curriculum and pamphlets for students and parents. After 4 months, no significant effects were reported for BMI, overweight or obesity prevalence. However, the intervention was successful in increasing MVPA time, number of PA, and time spent in PA games per week (control = −75.15, −0.25, −28.30; intervention = 127.92, 0.63, 92.01, respectively).
The C-RCT by Gutiérrez-Martínez et al. [48] included 10-year-old students in three schools (two treated and one control) from urban areas in Bogotá, Colombia. Both treatment groups received PA equipment (ribbons, balls, hoops, stairs, parachutes, and mats) to support PA during recess. In addition, a PE instructor delivered 30 standardised PA activities lasting 20’ each throughout the 10-week intervention period. In addition, participants in one of the treatment groups received daily SMS messages to promote extra-curricular PA and healthy nutrition. Results suggested there were no effects on BMI z-score or body fat percentage over the 10-week intervention period. Nevertheless, the intervention was successful in increasing MVPA and reducing SB minutes among participants in the treatment groups compared to those in the control one.
Finally, the 6-month C-RCT by Shamah Levy et al. [49] included 10- to 12-year-old students in six schools from both urban and rural areas in the State of Mexico. The treatment group received PA equipment (balls, ropes, and hoops) to support PA during recess over a 6-month intervention period. Other components included nutrition and PA education through workshops and materials (booklets, puppet show, advertising, banners) for students, parents, and school staff. Canteen personnel attended workshops aimed at promoting the daily sales of fruit, vegetables, and water. Results suggested a small but significant reduction in the probability of students in the treatment group to shift from the overweight to the obesity category after 6 months, compared to the ones in the control group (OR = 0.68; p = 0.01). However, no significant differences were reported for both groups (control and intervention) in the probabilities of shifting from the normal to overweight category after the intervention period. Overall, the intervention was relatively effective in maintaining BMI among children in the treatment group.
Food and built environments
The 18-month intervention reported by Safdie et al. [45] involved 4th- and 5th-grade children (9–10 years at baseline) attending 27 schools in urban areas of Mexico City. This study is the only one including food as well as BE strategies, among other intervention components. In addition, the strategy was implemented in two treatment groups, basic and plus, with the latter having all the same activities as the first, plus extra components implemented with additional financial investment and human resources. This C-RCT mixed different strategies, including the modification of the food provision in school canteens by limiting the availability of SSB and the sales of energy-dense foods at the school canteens during the 2 years for the plus group, and only during the second year for the basic one. It also included improvement of the school premises and provision of sports equipment for promoting the use of PA areas for two years in two different treatment groups (basic and plus). Games and sports courts were drawn on the ground, and each school received PA equipment (balls, ropes, nets, and elastic bands) to support PE classes and PA during recess and free time. Other components included promoting the availability of healthy food (fruits, vegetables, and non-fried dishes) and beverages (water) within school premises, reducing the number of eating opportunities, and providing nutritional and PA education by delivering workshops and pamphlets to students, parents, school staff and vendors. The intervention also included strategies for promoting PA during recess, among other activities. A small, yet non-significant reduction in the prevalence of overweight and obesity was reported for children from control and intervention groups (basic and plus) during the first year (19.5 vs 17; 11.9 vs 11.3; 12 vs 11.2%, respectively). Conversely, a slight increase in the prevalence was reported at the beginning of year 2 for control and basic treatment groups, but not for the plus group (17.9, 12.1, and 10.7%, respectively). Only children in the basic treatment groups reported a small but non-significant reduction in overweight and obesity prevalence during the second year (12.1 and 10.9%, respectively). In contrast, a small but significant BMI reduction was reported for control and plus groups in year 1 (19.9–18.4 and 20–18.5%, respectively). However, an inverse direction was reported for all in year 2, with small but non-significant increases in BMI across all groups (control = 18.9–19.1; basic = 20.1–20.4; plus = 18.7–19%). Therefore, the small-in-magnitude changes presented in overweight and obesity prevalence and BMI across the intervention period cannot be associated with the study intervention as similar changes were reported in control and intervention groups between baseline and follow-up periods. Yet, the intervention was effective at increasing intakes of recommended food and beverages and decreasing unhealthy ones, together with significant increases in PA (e.g., increases in steps taken by the students), among both treatment groups, compared to the control.
Discussion
Our review found only nine studies assessing school-based interventions including components for modifying the food and BE within and outside primary and secondary schools in LAC. From this pool, we are unable to conclude that children’s exposure to environmental interventions resulted in changes to obesity-related measurements. Albeit, two studies [46, 49] showed some results related to the prevention of obesity. Both were implemented in the State of Mexico, the first one in semi-rural areas [46] while the second one targeting both rural and urban areas [49]. It is not clear why this geographical concentration appears in our results; it could be speculated that the region has a higher obesity rate compared to other regions in our review, i.e., it already starts from a high rate of obesity and thus impact is easily detected. Notwithstanding, with such differences in the interventions’ design, this cannot be evidenced and therefore must remain a hypothesis for further studies.
The remaining seven studies did not present any significant changes in overweight or obesity-related measurements between control and treatment groups. However, all eight studies assessing intermediate outcomes contributing to prevent obesity in the long term reported some positive results, such as decreases in energy intakes [46] and in SB [48], increases in fruit and vegetable intake [47], healthy products [42, 45], physical fitness [43], MVPA minutes [34, 48], and steps taken [45]. Our findings are similar to previous intervention study reviews from the Global North, reporting improved dietary behaviours and increasing PA albeit inconclusive regarding the effects over obesity-related measures [50,51,52]. Notwithstanding, a recent review and meta-analysis including studies worldwide and using a wider definition of school food environments reported a meaningful effect of interventions to reduce adiposity (−0.12, 95% CI: 0.15–0.10) [26]. Overall, all but two studies were classified as showing a low risk of bias, with the remaining two as with moderate risk [41, 46], and all but three studies [43, 45, 46] had 1-year or shorter follow-up measurements, which could have weakened or biased our results. However, these studies are examples of relatively few number of studies assessing interventions in LAC, providing valuable information concerning the study design and methodological implications for future research teams.
In terms of scientific research and evidence mapping, our systematic review revealed the low number of peer-review articles assessing the effectiveness of food and BE interventions in schools for preventing/reducing childhood overweight and obesity in LAC. Previous reviews [53, 54] have primarily encountered interventions relying on educational components (e.g., nutritional education and modifications to PE sessions), and not environmental components. We also identified helpful methodological implications for future interventions in the region, for example, the need for a longer follow-up (beyond a 1-year horizon), and targeting both, the food and BEs. They should also assess mediating outcomes (changes in dietary and PA behaviours) and distal ones (obesity-related measures) when planning intervention strategies.
Our review has uncovered five studies targeting the BE, all within school boundaries, therefore not covering the 1-mile radius from the school as per our protocol. This is disappointing, particularly considering the positive impact that active commuting has in preventing obesity in schools [55,56,57]. Studies promoting BE interventions outside schools, such as active commuting, require organising multiple stakeholders (e.g., schools, councils, policymakers, and/or researchers), which might need more funding [58]. Considering the shortage of funding for research and development in LAC, with only 0.67% of its GPD allocated to it [59] and mostly from the public sector [60], interventions connecting different stakeholders and with a longer follow-up can face financial barriers. More research investment from governments and/or other funders could foster multi-stakeholder collaboration and design ambitious interventions, at the neighbourhood scale.
Moreover, most of the studies included here targeted urban areas, and even those targeting rural or semi-rural areas were in large metropolitan regions (Santiago de Chile and the State of Mexico). Considering that food provision in rural areas in LAC is generally more expensive than in urban locations (due to transport and logistics costs) [61], we hoped to find interventions conducted in more distinctive urban and rural settings. Expecting therefore to find contrasting results based on locations but the lack of published research on more typical rural landscapes has hampered any conclusive findings. However, this research gap does highlight the need for more interventions targeting the built and food environments in rural areas for preventing and reducing childhood obesity.
Our review has made a positive contribution to science and policymaking by updating the available evidence, even though included prospective studies only captured C-RCTs and LQE interventions excluding pre-and post-policy outcome evaluations related to childhood obesity. Only one LQE study in our pool assessed a state-wide school feeding programme, showing no difference between those receiving an FSB in any obesity-related measurement to those who did not [41]. It is in this area where our review also highlights a lack of policy evaluation studies reporting obesity-related outcomes. Indeed, 13 LAC countries have regulated the sale of food and beverages in schools [62], and four countries including Chile, Costa Rica, Ecuador and Uruguay, have implemented national policies aiming to restrict food marketing of unhealthy foods within school premises [63]. Only two countries, Chile and Mexico [62], have performed policy evaluations regarding restrictions on unhealthy product sales in schools, reporting positive results for reducing their availability in school kiosks in Chile [64] and for decreasing energy intake in children who only consumed food purchased at school in Mexico [65].
The case of Chile is a unique example within the region for implementing, in 2016, a mandatory and comprehensive policy for reducing the consumption of unhealthy products, and reducing and preventing obesity by including mandatory front-of-package warning labels, limiting advertising, and prohibiting school sales of products high in calories, sodium, sugar, or saturated fat [66]. Recent policy evaluations have reported positive outcomes for reducing the consumption and exposure to television advertising of unhealthy products among preschool children [67] and for households reducing purchases of unhealthy products [68]. However, no peer-reviewed policy evaluation in Chile has yet assessed the effect on obesity-related outcomes. A good example of a pre-and post-evaluation of an obesity prevention policy and its effectiveness in changing obesity-related measurements is the impact assessment of the SSB tax in Mexico and its role in decreasing overweight or obesity prevalence among adolescents [69]. Considering as stated above that research funding is scarce, future research should test the effectiveness of these policy-related interventions by conducting rigorous RCTs at a small scale; and use this evidence to decide whether scaling up is worthwhile. Scientists should exploit the opportunities presented by such policy changes and test their effect on changes in childhood obesity-related outcomes. The outcomes of such pre- and post-evaluations will take time but would at least inform governments if policy fixes are needed.
This lack of peer-reviewed policy evaluations suggests that there could be a disconnect between the scientific community and policymakers. A finding that can be attributed to a potential publication bias within our study is based on the exclusion of grey literature (e.g., technical reports). Notwithstanding, the question is, are scientists producing sufficient and adequate evidence for policymakers? Some evidence from studies reviewed here shows positive results in intermediate outcomes, such as reduction of SB and increase in fruit and vegetable intake as reported above. Yet, it seems peer-reviewed studies are not assessing changes in obesity-related measurements before/after policies are implemented and, therefore, policymakers do not seem to have the relevant evidence on the effectiveness of policies targeting childhood obesity in LAC. Decision-makers need evaluations of the short-term and long-term impact of childhood obesity prevention policies targeting school environments for reducing/preventing obesity, vis-à-vis the assessment of intermediate obesity determinants.
Considering that several countries in LAC are facing a double burden of obesity and undernutrition [70], this potential disconnect between the scientific community and policymakers is concerning, particularly considering the current COVID-19 pandemic. Indeed, the already large disparities in obesity rates and in behaviours contributing to obesity (diet, PA and SB) in LAC [71,72,73,74], predominantly affecting economically disadvantaged populations, have placed a disproportionate burden on these groups during the pandemic [75]. Due to disruptions in food supply chains, decreases in income and reductions in PA due to lockdowns [76, 77], it is expected that obesity rates across the continent will be impacted. Furthermore, the pandemic also has highlighted this science and policy disconnect, particularly considering the emergency response measures coming from some LAC governments at the start of the pandemic (such as Brazil and Mexico) [78, 79]. Despite the large and conclusive scientific evidence suggesting effective measures for mitigating contagion (e.g., use of facemasks and social distancing), some countries simply ignored the science. Academics working on other pressing issues such as climate change are already concluding that scientific evidence is more effective when academics and policymakers engage [80, 81]. LAC governments must take steps in bridging the science and policy gap, ensuring that policies are independently evaluated and peer-reviewed before upscaling.
Strengths and limitations
The main methodological limitations arise from the different sources of heterogeneity we encountered among the included studies. We list below the sources and their effect on our review or the studies themselves.
The first source is the high heterogeneity in reporting outcome measurements and measures of error. Studies reported different cut-off points and operationalisations for obesity-related outcomes (e.g., BMI, BMI z-score, overweight and/or obesity prevalence). Some presented results as mean differences; others reported averages or prevalence and others compared the frequency of these changes. In addition, only two reported straightforward measurements of variability for the effect changes (standard deviations, standard error, or confidence intervals). The second source is the high heterogeneity in study designs, age groups and types of intervention. A third source is the use of multiple intervention components used by the included studies, which might have influenced the lack of conclusive results. Together with modifications to the food and/or, BEs, interventions combined strategies by including nutrition and PA education, and/or changes to PE sessions. These components are delivered by different strategies, such as providing materials within the school curriculum, presenting workshops for students, parents and school staff, and the use of social marketing strategies (e.g., pamphlets and posters), among others. This multiplicity prevents us from clearly identifying if the intervention effects can be attributed to the inclusion of changes to the food or BEs in schools or to other types of intervention strategies. Only one study presented a food environmental strategy in isolation, and therefore, we cannot easily compare the effects of the different strategies. Altogether, these three sources of heterogeneity prevented us from quantitatively pooling data for a meta-analysis.
Likewise, the variable duration of interventions may have had an impact on the extent to which obesity-related measurements were affected. Six interventions lasted less than an academic year (<9 months), one lasted 2 years (18 months) and two lasted more than 3 years (28 months). Despite most of the interventions reporting positive results on some intermediate outcomes (diet, PA and SB), most failed to find any significant difference in measurements of obesity between intervention and control groups. Furthermore, all studies had small sample sizes (i.e., a reduced number of treated and non-treated schools). It is possible that some of these interventions might have been successful but that the effects might not have been large enough to be detected. Future interventions should consider a larger number of schools (based on power size calculations) and longer follow-up periods in their design, ensuring more conclusive findings on long-term obesity changes.
Conclusion
This review synthesised, for the first time, the effectiveness of interventions targeting the food and BEs in schools to prevent/reduce childhood obesity in LAC. Due to the high heterogeneity in study design and reporting outcomes, results were inconclusive. However, no study in our review reported a significant increase in BMI or obesity prevalence when interventions included modifications to the food and/or BEs.
In terms of evidence mapping, we revealed the low number of peer-review articles assessing the effectiveness of food and built and school environment interventions for preventing and reducing childhood overweight and obesity in LAC. Furthermore, we also have detected a complete absence of studies assessing the BE outside school buildings, for example, encouraging active school commutes.
Our conclusion is more concerning, as it points to a lack of policy evaluations from countries that have implemented policies, vis-à-vis a lack of adequate policy-informing evidence in countries where academics are active in obesity-related research, suggesting there is a potential disconnect between science and policymaking. With three out of ten children aged 5–19 years living with overweight or obesity in LAC countries, further funding to fund studies aiming to prevent and reduce childhood obesity in school settings in the region is needed. Notwithstanding, the production of evidence means little if science and policy operate in silos with little co-production of knowledge to better understand the food and BE factors that underpin LAC’s obesogenic environments where children learn, play and grow.
Data availability
Data collected and used in this review can be requested from the corresponding author.
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Fondo de las Naciones Unidas para la Infancia. El sobrepeso en la niñez: Un llamado para la prevención en América Latina y el Caribe. Ciudad de Panamá. 2021. www.unicef.org/lac. Accessed 27 Oct 2021.
Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82.
Segal AB, Huerta MC, Aurino E, Sassi F. The impact of childhood obesity on human capital in high-income countries: a systematic review. Obes Rev. 2021;22:e13104.
Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. 2012;13:985–1000.
Singh AS, Mulder C, Twisk JWR, Van Mechelen W, Chinapaw MJM. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88.
Popkin BM, Reardon T. Obesity and the food system transformation in Latin America. Obes Rev. 2018;19:1028–64.
Popkin BM, Gordon-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes. 2004;28:S2–9.
Corvalán C, Garmendia ML, Jones-Smith J, Lutter CK, Miranda JJ, Pedraza LS, et al. Nutrition status of children in Latin America. Obes Rev. 2017;18:7–18.
Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med (Baltim). 1999;29:563–70.
Townshend T, Lake A. Obesogenic environments: current evidence of the built and food environments: Perspect Public Health. 2017;137:38–44.
Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16:175–90.
Mackenbach JD, Rutter H, Compernolle S, Glonti K, Oppert JMM, Charreire H, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:1–15.
Li Y, Luo M, Wu X, Xiao Q, Luo J, Jia P. Grocery store access and childhood obesity: a systematic review and meta-analysis. Obes Rev. 2021;22:e12945.
Story M, Kaphingst KM, French S. The role of schools in obesity prevention. Futur Child. 2006;16:109–42.
Fondo de las Naciones Unidas para la Infancia (UNICEF). El rol de la escuela en la prevención del sobrepeso y la obesidad en estudiantes de América Latina y el Caribe. 2021. https://www.unicef.org/lac/media/29016/file/LACRO-El-rol-de-la-escuela-en-la-prevencion-del-sobrepeso.pdf. Accessed 29 Oct 2021.
Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794–802.
Sbruzzi G, Eibel B, Barbiero SM, Petkowicz RO, Ribeiro RA, Cesa CC, et al. Educational interventions in childhood obesity: a systematic review with meta-analysis of randomized clinical trials. Prev Med (Baltim). 2013;56:254–64.
Wang Y, Cai L, Wu Y, Wilson RF, Weston C, Fawole O, et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev. 2015;16:547–65.
Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity. 2008;16:1009–18.
Guerra PH, Cardoso da Silveira JA, Salvador EP. Physical activity and nutrition education at the school environment aimed at preventing childhood obesity: evidence from systematic reviews. J Pediatr (Rio J). 2016;92:15–23.
Lavelle HV, Mackay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Bangkok). 2012;34:360–9.
Liu Z, Xu HM, Wen LM, Peng YZ, Lin LZ, Zhou S, et al. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int J Behav Nutr Phys Act. 2019;16:1–12.
Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity. 2013;21:2422–8.
Bleich SN, Vercammen KA, Zatz LY, Frelier JM, Ebbeling CB, Peeters A. Interventions to prevent global childhood overweight and obesity: a systematic review. Lancet Diabetes Endocrinol. 2018;6:332–46.
Pineda E, Bascunan J, Sassi F. Improving the school food environment for the prevention of childhood obesity: what works and what doesn’t. Obes Rev. 2021;22:e13176.
Driessen CE, Cameron AJ, Thornton LE, Lai SK, Barnett LM. Effect of changes to the school food environment on eating behaviours and/or body weight in children: a systematic review. Obes Rev. 2014;15:968–82.
Swinburn B, Sacks G, Vandevijvere S, Kumanyika S, Lobstein T, Neal B, et al. INFORMAS (International Network for Food and Obesity/non-communicable diseases Research, Monitoring and Action Support): overview and key principles. Obes Rev. 2013;14:1–12.
World Health Organization. School policy framework: implementation of the WHO global strategy on diet, physical activity and health. 2008. https://apps.who.int/iris/handle/10665/43923. Accessed 4 Aug 2021.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Thomas J, Brunton J. EPPI-Reviewer: advanced software for systematic reviews, maps and evidence synthesis. London: EPPI-Centre Software, UCL Social Research Institute. 2020. https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=1913. Accessed 16 Nov 2021.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Report No.: 6.2. 2021. www.training.cochrane.org/handbook. Accessed 16 Nov 2021.
Orwin R. Evaluating coding decisions. In: Cooper H, Hedges L, editors. The handbook of research synthesis. New York, NY: Russell Sage Foundation; 1994.
Filho VCB, Da Silva KS, Mota J, Beck C, Da Silva Lopes A. A physical activity intervention for brazilian students from low human development index areas: a cluster-randomized controlled trial. J Phys Act Heal. 2016;13:1174–82.
Barbosa Filho VC, da Silva KS, Mota J, Vieira NFC, Gubert F, do A, et al. “For whom was it effective?” Moderators of the effect of a school-based intervention on potential physical activity determinants among Brazilian students. Prev Med (Baltim). 2017;97:80–5.
Cochrane Training. Extracting data from figures using software. 2016. https://training.cochrane.org/resource/extracting-data-figures-using-software-webinar. Accessed 15 Oct 2021.
Eldridge S, Campbell MK, Campbell MJ, Drahota AK, Giraudeau B, Reeves BC, et al. Revised Cochrane risk of bias tool for randomized trials (RoB 2) – additional considerations for cluster-randomized trials (RoB 2 CRT). 2021. https://drive.google.com/file/d/1yDQtDkrp68_8kJiIUdbongK99sx7RFI-/view. Accessed 26 Oct 2021.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12:55–61.
Ramírez-López E, Grijalva-Haro MI, Valencia ME, Ponce JA, Artalejo E. Impacto de un programa de desayunos escolares en la prevalencia de obesidad y factores de riesgo cardiovascular en niños sonorenses. Salud Publica Mex. 2005;47:126–33.
Rausch Herscovici C, Kovalskys I, Jose De Gregorio M. Gender differences and a school-based obesity prevention program in Argentina: a randomized trial. Rev Panam Salud Publica. 2013;34:75–82.
Andrade S, Lachat C, Ochoa-Aviles A, Verstraeten R, Huybregts L, Roberfroid D, et al. A school-based intervention improves physical fitness in Ecuadorian adolescents: a cluster-randomized controlled trial. Int J Behav Nutr Phys Act. 2014;11:1–17.
UNESCO Institute for Statistics. International Standard Classification of Education – ISCED 2011. Montreal, Canada; 2012. http://www.uis.unesco.org. Accessed 2 Dec 2021.
Safdie M, Jennings-Aburto N, Lévesque L, Janssen I, Campirano-Núñez F, López-Olmedo N, et al. Impact of a school-based intervention program on obesity risk factors in Mexican children. Salud Publica Mex. 2013;55(Suppl 3):374–87.
Alvirde-García U, Rodríguez-Guerrero AJ, Henao-Morán S, Gómez-Pérez FJ, Aguilar-Salinas CA. Resultados de un programa comunitario de intervención en el estilo de vida en niños. Salud Publica Mex. 2013;55(supl 3):S406–14.
González GCG, Zacarías HI, Domper RA, Fonseca ML, Lera ML, Vio del RF. Evaluación de un programa de entrega de frutas con educación nutricional en escuelas públicas rurales de la Región Metropolitana, Chile. Rev Chil Nutr. 2014;41:228–35.
Gutiérrez-Martínez L, Martínez RG, González SA, Bolívar MA, Estupiñan OV, Sarmiento OL. Effects of a strategy for the promotion of physical activity in students from Bogotá. Rev Saude Publica. 2018;52:79.
Shamah Levy T, Morales Ruán C, Amaya Castellanos C, Salazar Coronel A, Jiménez Aguilar A, Méndez Gómez Humarán I. Effectiveness of a diet and physical activity promotion strategy on the prevention of obesity in Mexican school children. BMC Public Heal. 2012;12:1–13.
Micha R, Karageorgou D, Bakogianni I, Trichia E, Whitsel LP, Story M, et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS One. 2018;13:e0194555.
Williams AJ, Wyatt KM, Hurst AJ, Williams CA. A systematic review of associations between the primary school built environment and childhood overweight and obesity. Health Place. 2012;18:504–14.
Davison KK, Lawson CT. Do attributes in the physical environment influence children’s physical activity? A review of the literature. Int J Behav Nutr Phys Act. 2006;3:1–17.
Lobelo F, Quevedo IG, de, Holub CK, Nagle BJ, Arredondo EM, Barquera S, et al. School-based programs aimed at the prevention and treatment of obesity: evidence-based interventions for youth in Latin America. J Sch Health. 2013;83:668–77.
Mancipe Navarrete JA, Garcia Villamil SS, Correa Bautista JE, Meneses-Echávez JF, González-Jiménez E, Schmidt-Riovalle J. Efectividad de las intervenciones educativas realizadas en América Latina para la prevención del sobrepeso y obesidad infantil en niños escolares de 6 a 17 años: una revisión sistemática. Nutr Hosp. 2015;31:102–14.
Lubans DR, Boreham CA, Kelly P, Foster CE. The relationship between active travel to school and health-related fitness in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2011;8:1–12.
Larouche R, Mammen G, Rowe DA, Faulkner G. Effectiveness of active school transport interventions: a systematic review and update. BMC Public Health. 2018;18:1–18.
Saunders LE, Green JM, Petticrew MP, Steinbach R, Roberts H. What are the health benefits of active travel? A systematic review of trials and cohort studies. PLoS One. 2013;8:e69912.
Daly-Smith A, Quarmby T, Archbold VSJ, Corrigan N, Wilson D, Resaland GK, et al. Using a multi-stakeholder experience-based design process to co-develop the Creating Active Schools Framework. Int J Behav Nutr Phys Act. 2020;17:1–12.
UNESCO. Research and development expenditure (% of GDP) – Latin America & Caribbean, European Union | Data. Data Bank, World Bank. 2018. https://data.worldbank.org/indicator/GB.XPD.RSDV.GD.ZS?locations=ZJ-EU. Accessed 20 Jun 2022.
ECLAC. Productive development in open economies. San Juan, Puerto Rico; 2004. https://repositorio.cepal.org/bitstream/handle/11362/13092/S2004056_en.pdf?sequence=1&isAllowed=y. Accessed 20 Jun 2022.
FAO, IFAD, PAHO, WFP, UNICEF. Regional overview of food security and nutrition in Latin America and the Caribbean 2020 – food security and nutrition for lagging territories. Santiago; 2021. https://www.fao.org/3/cb2242en/cb2242en.pdf. Accessed 24 Jun 2022.
Molina M, Anderson LN, Guindon GE, Tarride JE. A review of implementation and evaluation of Pan American Health Organization’s policies to prevent childhood obesity in Latin America. Obes Sci Pract. 2021;8:352–62.
Taillie LS, Busey E, Stoltze FM, Dillman, Carpentier FR. Governmental policies to reduce unhealthy food marketing to children. Nutr Rev. 2019;77:787–816.
Massri C, Sutherland S, Källestål C, Peña S. Impact of the food-labeling and advertising law banning competitive food and beverages in Chilean public schools, 2014–2016. Am J Public Health. 2019;109:1249–54.
López-Olmedo N, Jiménez-Aguilar A, Morales-Ruan M, del C, Hernández-Ávila M, Shamah-Levy T, et al. Consumption of foods and beverages in elementary schools: results of the implementation of the general guidelines for foods and beverages sales in elementary schools in Mexico, stages II and III. Eval Program Plann. 2018;66:1–6.
Rodríguez Osiac L, Cofré C, Pizarro T, Mansilla C, Herrera CA, Burrows J, et al. Using evidence-informed policies to tackle overweight and obesity in Chile. Rev Panam Salud Pública. 2017;41:1–5.
Jensen ML, Carpentier FD, Adair L, Corvalan C, Popkin BM, Taillie LS. Examining Chile’s unique food marketing policy: TV advertising and dietary intake in preschool children, a pre- and post- policy study. Pediatr Obes. 2021;16:e12735.
Taillie LS, Bercholz M, Popkin B, Reyes M, Colchero MA, Corvalán C. Changes in food purchases after the Chilean policies on food labelling, marketing, and sales in schools: a before and after study. Lancet Planet Heal. 2021;5:e526–33.
Gračner T, Marquez-Padilla F, Hernandez-Cortes D. Changes in weight-related outcomes among adolescents following consumer price increases of taxed sugar-sweetened beverages. JAMA Pediatr. 2022;176:150–8.
Corvalán C, Garmendia ML, Jones-Smith J, Lutter CK, Miranda JJ, Pedraza LS, et al. Nutrition status of children in Latin America. Obes Rev. 2017;18:7–18.
Vega-Salas MJ, Caro P, Johnson L, Papadaki A. Socioeconomic inequalities in dietary intake in Chile: a systematic review. Public Health Nutr. 2021;12:1–16.
Vega-Salas MJ, Caro P, Johnson L, Armstrong MEG, Papadaki A. Socioeconomic inequalities in physical activity and sedentary behaviour among the Chilean population: a systematic review of observational studies. Int J Environ Res Public Health. 2021;18:9722.
Mayén AL, Marques-Vidal P, Paccaud F, Bovet P, Stringhini S. Socioeconomic determinants of dietary patterns in low- and middle-income countries: a systematic review. Am J Clin Nutr. 2014;100:1520–31.
Mazariegos M, Auchincloss AH, Braverman-Bronstein A, Kroker-Lobos MF, Ramírez-Zea M, Hessel P, et al. Educational inequalities in obesity: a multilevel analysis of survey data from cities in Latin America. Public Health Nutr. 2021;25:1–9.
Halpern B, Louzada ML, da C, Aschner P, Gerchman F, Brajkovich I, et al. Obesity and COVID-19 in Latin America: a tragedy of two pandemics—official document of the Latin American Federation of Obesity Societies. Obes Rev. 2021;22:e13165.
Cortinez-O’Ryan A, Moran MR, Rios AP, Anza-Ramirez C, Slovic AD. Could severe mobility and park use restrictions during the COVID-19 pandemic aggravate health inequalities? Insights and challenges from Latin America. Cad Saude Publica. 2020;36:e00185820.
Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, Brun P, Ulloa N, Acevedo-Correa D, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during COVID-19 pandemic: an observational study. Nutrients. 2020;12:2289.
Garcia PJ, Alarcón A, Bayer A, Buss P, Guerra G, Ribeiro H, et al. COVID-19 response in Latin America. Am J Trop Med Hyg. 2020;103:1765–72.
Knaul F, Arreola-Ornelas H, Porteny T, Touchton M, Sánchez-Talanquer M, Méndez Ó, et al. Not far enough: public health policies to combat COVID-19 in Mexico’s states. PLoS One. 2021;16:e0251722.
Norström AV, Cvitanovic C, Löf MF, West S, Wyborn C, Balvanera P, et al. Principles for knowledge co-production in sustainability research. Nat Sustain. 2020;3:182–90.
Irwin EG, Culligan PJ, Fischer-Kowalski M, Law KL, Murtugudde R, Pfirman S. Bridging barriers to advance global sustainability. Nat Sustain. 2018;1:324–6.
Barlow SE. Expert Committee Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240.
WHO Multicentre Growth Reference Study Group de Onis M. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006;450:76–85.
Acknowledgements
We are grateful to all the authors who responded to our request for data for inclusion in our review.
Funding
This review was funded by PROCIENCIA (CONCYTEC/FONDECYT) grant number 030-2019, the British Embassy, the MRC grant (MR/S024778/1) and Newton Fund; and the Old Dart Foundation. The funders had no role in the design, collection, analysis, or interpretation of the present study, or in the decision to publish.
Author information
Authors and Affiliations
Contributions
CM, RN and KSV conceived the review. CM, RN, KSV and MJV-S designed the methodology for the systematic review. MJV-S led and conducted the literature search, screening, data extraction, risk of bias assessment, data analysis and interpretation, and writing of the first draft of the manuscript. AH-A was the second reviewer and contributed to searches, screening, data extraction, risk of bias assessment, and data analysis. RN was involved in resolving disagreements during screening processes. CM critically revised and edited the final draft of the manuscript. RN, AH-A, KC-Q, MEP, SC, JAL, AS, and KSV provided comments, revised the manuscript and approved the final version. MJV-S and CM confirm they had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vega-Salas, M.J., Murray, C., Nunes, R. et al. School environments and obesity: a systematic review of interventions and policies among school-age students in Latin America and the Caribbean. Int J Obes 47, 5–16 (2023). https://doi.org/10.1038/s41366-022-01226-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01226-9